Abstract
American Indian (AI) children have the highest rates of obesity among ethnic groups in the United States, and rates continue to increase. This study was designed to examine the effects of prenatal and early postnatal factors on AI children’s body mass index (BMI) trajectories, adiposity, and cardiovascular risk markers during early childhood. We screened 471 AI children (ages 5–8) from three Wisconsin tribes. Screenings included anthropometric and body fat measures and non-fasting lipid and glucose via fingerstick blood samples. Tribal records from Women Infants and Children (WIC) programs and clinic charts provided data on children’s BMI trajectories, maternal prenatal factors, and the early postnatal feeding environment. Forty-seven percent of children were overweight or obese. Analysis of growth trajectories showed that children’s BMI category was largely determined within the 1 year of life. Significant predictors of children’s BMI category at age 1 included macrosomia (OR 4.38), excess gestational weight gain (OR 1.64) and early termination of breastfeeding (OR 1.66). Children who were overweight/obese at age 1 had greater odds of being overweight (OR 3.42) or obese (OR 3.36), and having unhealthy levels of body fat (OR 2.95) and LDL cholesterol (OR 1.64) at ages 5–8. Children’s BMI category is determined in the early post-natal environment, within the 1 year of life, by factors including excess gestational weight gain and early termination of breastfeeding. In turn, children’s BMI category at age 1 predicts the emergence of cardiovascular risk markers in early childhood.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While obesity is a concern for all cultural groups in industrialized countries, minority ethnic groups in the U.S. have disproportionately high rates of obesity relative to European Americans [1]. Among all ethnic groups in the United States, American Indian (AI) children have the highest prevalence of obesity, and while rates of obesity have plateaued for most ethnic groups in the U.S., the prevalence of obesity among American Indian children continues to rise [2].
Research is accumulating to support the view that early development—particularly the prenatal period and first year of life—is especially important in determining children’s ultimate propensity for obesity. During this period, developmental plasticity is at its peak, and therefore small changes to the early environment are thought to induce phenotypic changes that have cascading effects across the lifespan [3–6].
Research to date has identified several risk factors in the prenatal and early postnatal environment that seem to predispose children to becoming overweight or obese. Maternal obesity [7–9] excess gestational weight gain [8, 10], gestational diabetes [7, 11], and maternal smoking during pregnancy [8, 11–14] all have been linked to increased risk of childhood obesity. Birth weight, at either very high or very low levels, also predicts later obesity [4–6, 8, 9, 15]. The early feeding environment is also important, with breastfeeding conferring a protective effect relative to formula feeding [16, 17].
Given the high prevalence of childhood obesity and its determinants among American Indians [18], we sought to examine predictors and consequences of early childhood body mass index (BMI) category in this understudied and high-risk population using data from the Wisconsin Nutrition and Growth Study (WINGS) [15, 16]. WINGS was designed to investigate the prevalence rates and contributing risk factors for obesity and its sequelae among children in three Wisconsin tribes (the Bad River Band of Lake Superior Chippewa Indians, the Menominee Tribe of Wisconsin, and the Lac du Flambeau Band of Lake Superior Chippewa Indians). The project took a community-based participatory approach to gather information about American Indian children’s early physical growth and environments in order to identify opportunities for intervention and prevention within the tribal communities. The current study examines the effects of prenatal and early postnatal factors on AI children’s BMI trajectories, adiposity, and cardiovascular risk markers during early childhood.
Methods
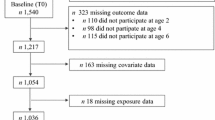
Participants
Data included in this analysis were from 471 American Indian children, the subset of the full WINGS cohort (n = 652) for whom we had both physiological data from a health screening conducted at age 5–8 and data from medical records of early growth from tribal Women Infants and Children (WIC) centers, Head Start, or tribal clinic chart records. The full WINGS cohort resulted from a 60 % response rate among those eligible. There was no indication that selection was biased relative to health measures. Specifically, distributions of height, weight, and BMI were comparable for the sample of WINGS participants as for the entire population of students in the schools/grades from which children were recruited [19, 20].
The children’s mean age at the health screening was 6.02 years (SD = 1.68). The sample was 49.7 % female. Approximately 45.2 % of participants were from the Menominee tribe; 38.4 % were from Lac du Flambeau; 16.3 % were from Bad River. The characteristics of the sample mirror those of the overall WINGS cohort [20].
Procedure
Kindergarten-2nd grade children (ages 5–8) were recruited for health screenings on three Wisconsin tribal reservations. Recruitment differed across the three tribal sites. Two tribes had schools located on their reservations, and those schools allowed us to conduct health screenings during the school day. In those two tribes, parent surveys and consent forms were sent home with all kindergarten through second grade students on two occasions prior to the health screenings. The caregiver survey asked about the home environment and the child’s activities. Consented children were asked for their assent then were screened at school over a period of 2–3 days. The health screening included anthropometric and body fat measures, non-fasting lipid panels and glucose via finger stick blood samples. The schools were compensated $10 for each child screened, and child participants received a t-shirt and other small prizes.
Because the third reservation did not have a tribal school, screenings took place at a series of community health fairs on the reservation. Advertisements for each health fair were posted in the tribal newspaper and at locations around the community. At the health fairs, parents completed the consent form and caregiver survey; then children gave their assent and were screened. Survey items and health screening procedures were identical to those used with the other two tribes. Caregivers received $10 cash for their participation, and children received a t-shirt and other small prizes.
Given the stable nature of the tribal communities, almost all child participants in the health screening had previously been participants in WIC or Head Start on their respective reservations. This provided us with a unique opportunity to obtain and review children’s medical records in order to learn about the children’s early growth, maternal prenatal risk factors, and early postnatal environments. With parent’s consent, members of the research team examined the records and recorded information about children’s birth status and early growth. Notably, some items from the WIC data were similar to those obtained from the parental surveys (e.g. birth weight, duration of breastfeeding). When compared, data from the two sources corresponded quite well. For example, for breastfeeding duration, r = 0.70 and for birth weight r = 0.92.
Measures
Data Collected at the Health Screening
Children’s heights were measured to the nearest .1 cm using a portable stadiometer. Impedance-based percentage of body fat was measured with a Tanita instrument (Model TBF-305; Tanita Corp, Chicago) which also provided weights to the nearest 1 kg. Hip and waist circumferences were measured to the nearest .1 cm with flexible plastic measuring tape. CDC syntax was used to convert children’s weights and heights into age- and gender- adjusted BMI and BMI z scores based on CDC growth charts [21]. Children who were above the 95th percentile were classified as obese. Children who were between the 85th and 95th percentiles were classified as overweight. Children between the 5th and 85th percentiles were classified as healthy weight. Children below the 5th percentile were classified as underweight.
Non-fasting glucose levels, total cholesterol (TC), and high-density lipoprotein (HDL) were measured from blood samples obtained by finger stick (Cholestech, LDX System, Hayward, CA). Blood pressures were measured by auscultation with a standard sphygmomanometer.
Trained tribal health professionals or academic research staff performed all measurements. Individual results for each child were sent to parents by letter, with recommended clinic follow-up for abnormal values.
Data Collected from WIC Records
Measures collected from the records included: birth order, birth weight, birth length, presence of gestational diabetes, duration of pregnancy, mother’s smoking habits before and during pregnancy, mother’s weight and height before pregnancy and at delivery, initiation and duration of breastfeeding, duration of formula feeding and age at which formula was started, age at which solid foods were started. Gestational weight gain was computed and classified according to IOM recommendations [22].
In addition, the height and weight of each child was recorded at each WIC visit, conducted approximately every 6 months from birth onward. These weights and heights were used to calculate age- and gender- specific BMI for each time point using CDC growth charts. Together, those measurements make it possible to track children’s growth trajectories across early childhood, leading up to the health screening.
Data Analysis
Descriptive characteristics of the sample were examined using χ2 tests and one-way analysis of variance to compare healthy weight, overweight and obese children’s health and to compare the prevalence of prenatal and early postnatal risk factors for obesity across groups. Then, to examine children’s growth trajectories, children were classified according to BMI category at the health screening, and data from the children’s medical records were used to construct mean growth trajectories for each weight group from birth to age 5. Next, logistic regression was used to compute odds ratios for prenatal and early postnatal risk factors, predicting children’s BMI category at age 1 and age 5–8. Finally, odds ratios were computed to examine the association between children’s BMI category at age 1 and their cardiovascular risk markers at age 5–8.
Results
Prevalence of Childhood Overweight/Obesity at the Health Screening
The health screening revealed that approximately 54 % of children were normal weight, 18 % were overweight, and 27 % were obese. An additional 6 children (1 % of the sample) were underweight. Because the small size of the underweight group was unlikely to yield robust findings, we excluded them from further analyses.
Table 1 presents characteristics of the healthy weight, overweight, and obese children, from the health screening and accompanying parental survey. Results from one-way ANOVAs and χ2 tests showed that there were no differences among the groups in demographic factors, including age, gender distribution, parental educational attainment, or household size. However, there were significant differences among the groups, in the predicted directions, for almost every measure of physical health, including: hip and waist circumference, percentage body fat, total cholesterol, HDL cholesterol, and blood pressure, with obese children showing greatest risk for future cardiovascular problems.
Prevalence of Prenatal and Early Postnatal Risk Factors for Childhood Obesity
Table 2 shows the prevalence of prenatal and early postnatal risk factors within our sample. Overall, the rate of gestational diabetes was 13 %, and the rate of maternal smoking during pregnancy was 59 %. Maternal smoking was equally common across weight groups, but reports of gestational diabetes were significantly more common among mothers whose children were overweight or obese.
Low birth weight and very low birth weight were uncommon (3 % and <1 %, respectively), and rates did not differ by children’s BMI category at the health screening. High birth weight (macrosomia) was more common (5 %), and it was more frequent among overweight and obese children.
The rate of breastfeeding initiation was low (59 %) relative to formula use (97 %). Among mothers who initiated breastfeeding, the median duration was 13 weeks (range 1 day–5 years). The median time for introducing solid foods, was 22 weeks (range 5–65 weeks).
Self-reported heights and weights indicated that 72 % of mothers and 81 % of fathers were either overweight or obese at the time of the children’s health screening. Medical records showed that 60 % of mothers were overweight or obese before pregnancy. A majority of mothers (51 %) reported gestational weight gain in excess of IOM guidelines [22], and excess gestational weight gain was especially common among mothers whose children were overweight (54 %) or obese (60 %).
Growth Trajectories
The age- and gender- adjusted BMI growth trajectories of children who ultimately were healthy weight, overweight, and obese at the health screening are depicted in Fig. 1. There was no difference between the groups’ BMIs at birth, F (2, 377) = 0.29, p = 0.75. However, the groups’ growth trajectories quickly diverged during the first year of life, and the groups differed by age 1, F (2, 361) = 24.15, p < .001. The groups remained reliably different from age 1 onward (all ps < .001).
Predictors of Childhood Overweight and Obesity
Table 3 displays risk estimates for prenatal and early postnatal risk factors for childhood obesity, with each risk factor predicting BMI category at age 1 and age 5–8. The findings identify several determinants of children’s BMI category at age 1. Macrosomia (high birth weight), limited breastfeeding duration, and excess gestational weight gain all increased the odds that the child would be overweight or obese at age 1.
We conducted a parallel analysis to examine whether factors in the prenatal and early post-natal environment would also predict children’s BMI category at age 5–8 (the health screening). Those risk estimates are reported in Table 3, as well. Macrosomia, limited breastfeeding duration, and excess weight gain significantly all increased the odds that the child would be overweight or obese at age 5–8. Gestational diabetes was also associated with increased odds that the child would be overweight or obese by age 5–8.
To ensure that the effect of macrosomia was not solely a product of its co-occurrence with gestational diabetes, we conducted stratified analyses of those with a diabetic pregnancy and those without. Even when mothers had no diagnosis of gestational diabetes, macrosomia increased the odds that the child would be overweight/obese by age 1 (OR 2.53) and age 5–8 (OR 4.14).
Implications of Early BMI Category on Child Health
Table 4 shows that BMI category at age 1 is a reliable predictor of children’s’ BMI category at age 5–8. Children who were overweight/obese at age 1 had over 3 times the odds of being overweight or obese at age 5–8, relative to children who were at a healthy weight at age 1, whether measured by BMI or excess body fat.
Furthermore, odds ratios showed a pattern indicating that children who were overweight at age 1 were more likely to exhibit symptoms of cardiovascular risk and early metabolic syndrome during the health screening, including higher total cholesterol, lower HDL cholesterol, and higher non-fasting glucose. These effects were marginally significant.
Discussion
This study corroborates other studies showing that American Indian children are at high risk for overweight and obesity. Combined prevalence of overweight and obesity in this sample of kindgergarten-2nd graders was 45 %. Moreover, known risk factors for childhood obesity were unusually common. For example, 59 % of mothers were overweight or obese at the beginning of their pregnancy, 59 % of mothers reported smoking during pregnancy, and 76 % of mothers terminated breastfeeding within 4 months of the child’s birth. These rates are much higher than are typically seen in U.S. samples [12, 23, 24].
Not surprisingly, these common prenatal and early postnatal risk factors were associated with elevated risk for childhood overweight and obesity. Gestational weight gain in excess of the IOM’s 2009 guidelines increased the odds of having an overweight or obese child by 60 %, and a diabetic pregnancy increased the odds of having an overweight or obese child by almost 90 %. Children who weighed more than 4,500 g at birth had more than 4 times the odds of being overweight, compared to children who weighed less. These results are consistent with other studies that have linked fetal overnutrition to later obesity [6, 25]. Supporting a growing literature on the benefits of breastfeeding [16, 17], we found that breastfeeding for <4 months led to a 60 % increase in the odds of having an overweight or obese child.
Using current and historical data on children’s growth over time, we were able to examine the trajectories by which childhood overweight and obesity emerged. We found that children who ultimately would be overweight or obese at our health screening were, on average, already overweight by age one and their BMI category remained relatively stable thereafter. This adds to the body of work suggesting that children’s BMI category is largely determined during the 1 year of life [26]. Having a BMI greater than the 85th percentile at age 1 was also associated with cardiovascular risk markers at age 5–8.
These findings should all be interpreted in light of this study’s limitations. First, the population-based sample was not randomly selected. However, the high response rate, along with evidence that the WINGS children were representative of their school populations on relevant anthropomorphic factors, lead us to believe that our results can likely be generalized to other communities, especially other American Indian tribes. Second, our data analysis was limited by incomplete and imperfect data from the children’s historical WIC and clinic records. For example, not every child had height and weight data for every time point from birth to age 5. Our findings appear to be robust in spite of those missing data. Third, the sample is quite homogenous. This is a benefit in many ways, but it limits our ability to draw conclusions about the contributions of socioeconomic status and other community factors as predictors of childhood obesity. Despite these limitations, our findings provide support for the hypothesis that the prenatal and early postnatal environments play a major role in shaping long-term health outcomes related to obesity and its sequalae.
Conclusions
Children’s prenatal and early post-natal environments predict their BMI growth trajectories across early childhood and are associated with the emergence of cardiovascular risk markers. Therefore, community-research partnerships that address early determinants of obesity will be essential for understanding and combating childhood obesity and its sequalae.
In light of these results, each of the three tribes has undertaken projects to respond to the unique health needs of their communities. In addition, the current study helped inform a data-driven, culturally-tailored, family-based intervention to improve early childhood nutrition and physical activity in AI communities. That intervention, called Healthy Children, Strong Families, is ongoing [27, 28].
References
Ogden, C. L., Carroll, M. D., Curtin, L. R., McDowell, M. A., Tabak, C. J., & Flegal, K. M. (2006). Prevalence of overweight and obesity in the United States, 1999-2004. Journal of the American Medical Association, 295(13), 1549–1555. doi:10.1001/jama.295.13.1549.
Centers for Disease Control and Prevention. (2009). Obesity prevalence among low-income, preschool-aged children—United States, 1998-2008. MMWR: Morbidity and Mortality Weekly Report, 58(28), 769–773.
Anzman, S. L., Rollins, B. Y., & Birch, L. L. (2010). Parental influence on children’s early eating environments and obesity risk: Implications for prevention. International Journal of Obesity, 34(7), 1116–1124. doi:10.1038/ijo.2010.43.
Hanson, M. A., & Gluckman, P. D. (2008). Developmental origins of health and disease: New insights. Basic and Clinical Pharmacology and Toxicology, 102(2), 90–93. doi:10.1111/j.1742-7843.2007.00186.x.
Armitage, J. A., Poston, L., & Taylor, P. D. (2008). Developmental origins of obesity and the metabolic syndrome: The role of maternal obesity. Frontiers of Hormone Research, 36, 73–84.
Tamashiro, K. L. K., & Moran, T. H. (2010). Perinatal environment and its influences on metabolic programming of offspring. Physiology and Behavior, 100(5), 560–566. doi:10.1016/j.physbeh.2010.04.008.
Pirkola, J., Pouta, A., Bloigu, A., Hartikainen, A. L., Laitinen, J., Jarvelin, M. R., et al. (2010). Risks of overweight and abdominal obesity at age 16 years associated with prenatal exposures to maternal prepregnancy overweight and gestational diabetes mellitus. Diabetes care, 33(5), 1115–1121. doi:10.2337/dc09-1871. Epub 2010/04/30.
Olson, C. M., Strawderman, M. S., & Dennison, B. A. (2009). Maternal weight gain during pregnancy and child weight at age 3 years. Maternal and Child Health Journal, 13(6), 839–846. doi:10.1007/s10995-008-0413-6.
Rooney, B., Mathiason, M., & Schauberger, C. (2010). Predictors of obesity in childhood, adolescence, and adulthood in a birth cohort. Maternal and Child Health Journal, 15(8), 1166–1175. doi:10.1007/s10995-010-0689-1.
Schack-Nielsen, L., Michaelsen, K. F., Gamborg, M., Mortensen, E. L., & Sorensen, T. I. A. (2009). Gestational weight gain in relation to offspring body mass index and obesity from infancy through adulthood. International Journal of Obesity, 34(1), 67–74. doi:10.1038/ijo.2009.206.
Huang, J. S., Lee, T. A., & Lu, M. C. (2007). Prenatal programming of childhood overweight and obesity. Maternal and Child Health Journal, 11(5), 461–473. doi:10.1007/s10995-006-0141-8.
Ino, T. (2010). Maternal smoking during pregnancy and offspring obesity: Meta-analysis. Pediatrics International, 52(1), 94–99. doi:10.1111/j.1442-200X.2009.02883.x.
Adams, A. K., Harvey, H. E., & Prince, R. J. (2005). Association of maternal smoking with overweight at age 3 y in American Indian children. The American Journal of Clinical Nutrition, 82(2), 393–398.
Gorog, K., Pattenden, S., Antova, T., Niciu, E., Rudnai, P., Scholtens, S., et al. (2009). Maternal smoking during pregnancy and childhood obesity: Results from the CESAR Study. Maternal and Child Health Journal, 15(7), 985–992. doi:10.1007/s10995-009-0543-5.
De Lucia Rolfe, E., Loos, R. J., Druet, C., Stolk, R. P., Ekelund, U., Griffin, S. J., et al. (2010). Association between birth weight and visceral fat in adults. The American Journal of Clinical Nutrition, 92(2), 347–352. doi:10.3945/ajcn.2010.29247.
Owen, C. G., Martin, R. M., Whincup, P. H., Smith, G. D., & Cook, D. G. (2004). Effect of infant feeding on the risk of obesity across the life course: A quantitative review of published evidence. Pediatrics., 115(5), 1367–1377. doi:10.1542/peds.2004-1176. Epub 2005/05/04.
Harder, T., Bergmann, R., Kallischnigg, G., & Plagemann, A. (2005). Duration of breastfeeding and risk of overweight: A meta-analysis. American journal of epidemiology, 162(5), 397–403. doi:10.1093/aje/kwi222. Epub 2005/08/04.
Jernigan, V. B. B., Duran, B., Ahn, D., & Winkleby, M. (2010). Changing patterns in health behaviors and risk factors related to cardiovascular disease among American Indians and Alaska Natives. American Journal of Public Health, 100(4), 677–683. doi:10.2105/ajph.2009.164285.
Adams, A. K., Miller-Korth, N., & Brown, D. (2004). Learning to work together: Developing academic and community research partnerships. Wisconsin Medical Journal, 103(2), 15–19.
Adams, A. K., Quinn, R. A., & Prince, R. J. (2005). Low recognition of childhood overweight and disease risk among native-American caregivers. Obesity, 13(1), 146–152. doi:10.1038/oby.2005.19.
Kuczmarski, R. J., Ogden, C. L., Guo, S. S., Grummer-Strawn, L. M., Flegal, K. M., Mei, Z., et al. (2002). 2000 CDC growth charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Statistics, 11(246).
Institute of Medicine (IOM). (2009). Weight gain during pregnancy: Reexamining the guidelines. In K. M. Rasmussen & A. Yaktine (Eds.), Washington, D.C.: National Academy Press.
Li, R., Darling, N., Maurice, E., Barker, L., & Grummer-Strawn, L. M. (2005). Breastfeeding rates in the United States by characteristics of the child, mother, or family: The 2002 National Immunization Survey. Pediatrics, 115(1), e31–e37. doi:10.1542/peds.2004-0481. Epub 2004/12/08.
Bombard, J., Dietz, P., Galavotti, C., England, L., Tong, V., Hayes, D., et al. (2010). Chronic diseases and related risk factors among low-income mothers. Maternal and Child Health Journal, 16(1), 60–71. doi:10.1007/s10995-010-0717-1.
Whitaker, R. C., & Dietz, W. H. (1998). Role of the prenatal environment in the development of obesity. The Journal of pediatrics, 132(5), 768–776. doi:10.1016/S0022-3476(98)70302-6.
Monteiro, P. O. A., & Victora, C. G. (2005). Rapid growth in infancy and childhood and obesity in later life—a systematic review. Obesity Reviews, 6(2), 143–154. doi:10.1111/j.1467-789X.2005.00183.x.
LaRowe, T. L., Wubben, D. P., Cronin, K. A., Vannatter, S. M., & Adams, A. K. (2007). Development of a culturally appropriate, home-based nutrition and physical activity curriculum for Wisconsin American Indian families. Preventing Chronic Disease, 4(4), A109.
LaRowe, T. L., Adams, A. K., Jobe, J. B., Cronin, K. A., Vannatter, S. M., & Prince, R. J. (2010). Dietary intakes and physical activity among preschool-aged children living in rural American Indian communities before a family-based healthy lifestyle intervention. Journal of the American Dietetic Association, 110(7), 1049–1057. doi:10.1016/j.jada.2010.04.009.
Acknowledgments
The project described is supported by grants from the Eunice Kennedy Schriver National Institute of Child Health and Human Development (T32 HD049302 to Lindberg), the Great Lakes Native American Research Centers for Health with funding from IHS/NIGMS (U269400014-01 to Adams), the Wisconsin Department of Health and Family Services with funding from the CDC for Cardiovascular Health Research (DHHS 22236646/155069 to Adams), and a NIH/NHLBI Career Development grant (K23 HL068827 to Adams). This manuscript's content is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations. The authors thank the Wellness staff who assisted in gathering data from Bad River, Menominee, and Lac du Flambeau. We also thank the children and families participating in WINGS.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lindberg, S.M., Adams, A.K. & Prince, R.J. Early Predictors of Obesity and Cardiovascular Risk Among American Indian Children. Matern Child Health J 16, 1879–1886 (2012). https://doi.org/10.1007/s10995-012-1024-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-012-1024-9