Abstract
To examine changes and equity in use of maternal care in different types of rural and urban areas in China from the early 1990s to early 2000s. Data were drawn from three National Health Household Interview Surveys conducted in 1993, 1998, and 2003. Analysis was based on married women aged between 15 and 49 who had live births within the 24 months prior to the survey. Nationally, the proportion of women receiving their first pre-natal visit within 12 weeks of gestation and the hospital delivery rate increased rapidly from 20.56 and 37.61% in the early 1990s to 52.60 and 74.02% in the early 2000s, respectively, while the proportion of women receiving at least one post-natal care visit dropped slightly from 56.46 to 54.12% in the same time period. There were large disparities in use of maternal care between urban and rural areas and among different sized cities and rural areas with different levels of socio-economic development. But the disparities narrowed over time, especially among different types of rural areas. The proportion of delivery out of hospital attended by trained staff in rural areas decreased considerably from 68.01% in 1991–1993 to 51.57% in 2001–2003. Maternal care utilization made remarkable progress in the study period, and the gap between rural and urban areas and among different classes of cities and rural areas significantly narrowed. This was probably due to both socio-economic development and targeted investments in improving health services. However, significant gaps remained, requiring attention.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent decades, China’s society and economy have undergone a profound reform process, which has achieved tremendous success in improving the income level and living standards of the majority of the population [1]. However, the transition from planned to market economy in China has had complex implications for the health sector in terms of the financing, organization and provision of health services [2–4]. Although health care as a whole has benefited from the economic reforms, there have been serious concerns about the equity impact of the early health sector reforms carried out from the mid 1980s [1]. The reforms were heavily market-oriented, including fiscal decentralization and effective part-privatization of public health facilities, and the collapse of the rural and urban co-operative health insurance schemes that provided most of the population with access to basic health care at low cost. A number of studies conducted during the 1990s demonstrated socio-economic and regional inequities in both health indicators and utilization of healthcare, related partly to the increasing un-affordability of healthcare and lack of financial protection mechanisms [5–8] Since the mid 1990s the Government of China has responded to this national and international evidence of the unintended consequences of the reforms and the economic burden of ill-health and has begun to develop new strategies aiming at better equity, efficiency and quality in health sector.
In the last few decades maternal health and healthcare have become an undisputed national and international priority. Internationally, the Millennium Development Goals (MDGs) call for a 75% reduction in maternal mortality between 1990 and 2015 [9], and in 2008, the countdown to 2015 initiative identified 68 priority countries including China for action on maternal, new born and child health [10]. Much attention has been paid to monitoring country-level progress in achieving high and equitable coverage with interventions effective in reducing the mortality of mothers, neonates and children under 5 years. In China, a series of laws and regulations aiming to improve maternal and child health were passed during the 1990s and early 2000s, including Guidelines for Chinese Women’s Development in 1995 and 2000, respectively, and the Maternal and Infant Health Care Law of the PRC in 1994. A Department of Maternal and Child Health Care and Community Health was established within the Ministry of Health in 1998, aiming to strength the management of reproductive health services [11].
To date, there have been few studies published in English examining the trends in maternal healthcare utilization during this significant period using nationally representative data for China, which has about one-fifth of the world’s population. This paper aims to contribute towards filling this gap by describing the levels and trends in use of maternal health care between and within urban and rural populations from 1991 to 2003. This examination of the pattern of trends in utilization and equity should contribute towards the international understanding of changes in healthcare access during economic and health system reforms.
Materials and Methods
Data were drawn from three National Household Surveys (NHHS) conducted in 1993, 1998, and 2003 under the supervision of Chinese Ministry of Health, covering both urban and rural populations in China. In NHHS a four-stage stratified random sampling procedure was used to select the households. The sampling method and sample size was almost the same for the three household surveys. In each survey, 95 counties/cities were taken as samples. 5 townships/streets were taken from each sample county or street. The total households selected were 57,000 (the population was 193,689 in the 2003 survey, 216,101 in the 1998 survey and 215,163 in the 1993 survey).The selected households represent 1 per 5,000 households of the country.
The surveys used standardized questionnaires including general demographic and socioeconomic information on sampled households and their members, perceived needs of and demands for health care, and use of and expenditure on health services. One section in the questionnaires focused on reproductive health and health care of married women aged between 15 and 49 years old and provided data about the history of women’s pregnancy-related activities. It is reasonable to infer that these data were comparable across years.
Ten indicators of socioeconomic development were used to categorize more than 2,400 cities and counties in China into seven strata (large, middle and small cities,Footnote 1 and four types of rural areas with different levels of socioeconomic development). The quality of the data collected from the surveys has been proved satisfactory in terms of representativeness of the sample and reliability of the data. For example, the structure of the study population sampled in the 1993 survey was very similar to that of the population data derived from the Chinese population census in 1990 [12, 13].
In this study, we selected those who had live births within the 24 months prior to the survey from all married women aged between 15 and 49 interviewed in each NHHS data collection round, and analyzed their maternal healthcare use with regard to their demographic characteristics and their place of residence. The women who gave birth from June 1991 to May 1993, January 1996 to December 1997, and September 2001 to August 2003 in selected households were interviewed. The number of women interviewed was 4,972 (825 from urban and 4,147 from rural areas), 3,910 (696 from urban and 3,214 from rural areas) and 3,289 (608 from urban and 2,681 from rural areas) in the three surveys, respectively. The total response rate for interview was 100%. If the selected household was not available for interview when visited, the next neighboring household was approached instead. Data on women who experienced still-births or maternal mortality is not available in the NHHS. The exclusion of these women should be considered a limitation of our study methodology since it places some limitations on the generalizability of our findings to the whole population of pregnant women.
The indicators of healthcare used in our analysis were: the proportion of first prenatal visits within 12 weeks of gestation; the proportion of prenatal care visit frequency meeting national MOH standards; the hospital delivery rate; the proportion of delivery out of hospital attended by trained staff in rural areas; and the proportion of postnatal visits. The Ministry of Health stipulates that pregnant women should: have at least 5 prenatal visits in rural areas and 8 visits in urban areas; have their first prenatal visit before 13 weeks of gestation; and have at least 3 postnatal visits (within 42 days of delivery) in both rural and urban areas. The Ministry of Health has also set standards for coverage levels for each criterion as follows [14]:
For large and medium-sized cities:
-
The proportion of pregnant women making their first prenatal visit within 12 weeks ≥75%
-
The proportion of pregnant women making at least 5 prenatal care visits ≥95%
-
The proportion of deliveries in hospital ≥98%
-
The proportion of post-partum women receiving at least postnatal visits ≥80%
For small cities and type 1–2 rural areas:
-
The proportion of pregnant women making their first prenatal visit within 12 weeks ≥50%
-
The proportion of pregnant women making at least 5 prenatal care visits ≥80–85%
-
The proportion of deliveries in hospital ≥50–88%
-
The proportion of post-partum women receiving at least postnatal visits >70%
For type 3–4 rural areas:
-
The proportion of pregnant women making their first prenatal visit within 12 weeks ≥40%
-
The proportion of pregnant women making at least 5 prenatal care visits >70%
-
The proportion of deliveries in hospital ≥30%
-
The proportion of post-partum women receiving at least postnatal visits >60%
The Chi-square test was used to analyze disparities in these indicators of the use of maternal care between and within urban and rural areas (as proxies of socio-economic development) and the trends across the years. Individuals were grouped according to the type of city/rural area they lived in and their utilization of services was compared. The proportion and odds ratios were all weighted in the analysis.
Results
Trends in Use of Maternal Care
Prenatal Care
Proportion of Women Receiving First Pre-Natal Visit Within 12 Weeks
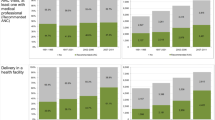
The proportion of women received their first prenatal visit within 12 weeks increased greatly from the early to mid 1990s in all areas except large cities. The increase was much larger in the rural areas, reducing the urban–rural difference from more than 4 times to about 1.4 times. The disparity decreased more remarkably among different types of rural areas than among cities of different size. The difference between the type 1 (richest) and the type 4 (poorest) rural areas was narrowed from 8.1 times to about 2.1 times while the difference between large cities and small cities only dropped from 1.6 times to 1.4 times (Table 1). Thereafter the rate continued to rise in poorer rural areas (Types 2–4) and large cities, but fell slightly in the Type 1 rural areas, small and medium cities by 2001–2003.
Frequency of Pre-Natal Visits Meeting MOH Standards
The proportion of women receiving antenatal care visits meeting the MOH standard (at least 8 times) slightly increased from 47% in 1991–1993 to 58% in 2001–2003 in urban areas, while in rural areas the proportion meeting the MOH standard (at least 5 times) increased sharply from 12% in 1991–1993 to 36% in 2001–2003. The speed of the proportional increase varied among different types of cities and different types of rural areas. The proportion remained almost unchanged in big cities but increased slightly in small and medium-sized cities with time. In rural areas, the proportional increase was much faster in less developed areas than in developed areas. The proportion increased by 4.2 times in type 4, 4.1 times in type 3, 3.6 times in type 2, and 2 times in type 4 rural areas from 1991–1992 to 2001–2002, respectively Table 2.
Delivery Care
Hospital Delivery Rate from 1991 to 2003
The hospital delivery rate increased from 37.61 to 74.02% in China during the study period. However, the change of the rate varied with the socio-economic status of different areas. The hospital delivery rate increased slightly from 89.70 to 94.36% in urban areas while the proportion increased from 27.25 to 69.44% in rural areas. The fastest change was found to be in type 4 rural areas, where the utilization quadrupled. The overall difference between rural and urban areas was substantially narrowed over the period (Table 3).
Proportion of Deliveries Out of Hospital Attended by Trained Staff in Rural Areas 1993 and 2003
Since very few urban women delivered out of hospital in urban areas in the three surveys, only the women in rural areas were covered in this section. The proportion of deliveries out of hospital attended by trained staff in rural areas dropped continually from 68.01% in the first period to 51.57% in the third period. The trend was significant in all except type 2 areas (Table 4).
Postnatal Care
Proportion of Women Receiving at Least One Post-Natal Care Visit
The proportion of women received at least one postnatal visit dropped slightly in both urban and rural areas. It decreased from 64.12 to 61.68% in urban areas, and fell slightly from 54.93% in 1993 to 52.41% in 2003 in rural areas with no statistical significance. The gap in the proportion of women receiving at least one postnatal visit between urban and rural areas and among rural areas was much smaller than that with the other variables concerning prenatal care and delivery care (Table 5).
Discussion
From 1991 to 2003, a complex picture emerged in terms of trends in equity of utilization of maternal health care in China, in that in general there were significant increases but the pace of increase varied over different periods and between different areas.
It is noteworthy that there was significant improvement in maternal care utilization, including prenatal care and delivery care in both rural and urban areas over the study periods, despite internal fluctuation and variations. Post-natal care was the exception in that it slightly decreased in all areas. Although the actual levels of utilization increased the most in absolute terms and remained higher in urban areas at the end of the period, the improvements in rural areas were significantly faster, especially in the poorest or second poorest rural areas, with the proportion of women making their first prenatal visit within 12 weeks of gestation increasing by more than 4 times, the proportion of women utilizing prenatal care meeting Chinese MOH standard by about 4 times, and the hospital delivery rate by more than twice.
The overall trend towards substantially increased utilization of most maternal healthcare services may be attributed to several major developments in China. First, the findings suggest that despite legitimate concerns about the negative impact of health sector reforms, general socio-economic development, including increases in income, living standards and educational levels may have played an important part in enabling increased utilization of services [15]. Second, external pressures through the global emphasis on MCH and the availability of financing from international organizations supported a substantial legislative, policy and programmatic effort by the Chinese government in the 1990s [16].
Significant legislative efforts included the establishment of the National Working Committee on Children and Women under the State Council in 1990, which was in charge of coordinating and promoting the framing and implementation of laws and regulations concerning women and children by different departments within the government, and the promulgation of the national Maternal and Infant Health Care Law in 1994. The Maternal and Infant Health Care Law covers pre-marital health, antenatal and perinatal health and includes guidelines on technical implementation, management and legal liability. The legislation is largely advocatory rather than mandatory, requiring the government at each level to develop a strategy to enhance the development of the MIH care system among others, and was supported by Implementation Regulations in June 2001. A small-scale case study evaluating the impact of the law in two counties in 2004 found that it had been successful in mobilizing resources to some extent, but that the overall proportion of funds allocated to MIHC remained low, and that its influence in influencing provider behaviour was limited in the context of high effective decentralization [17].The legislative framework was supported by national MOH regulations, including ‘Regulations about Systematic Healthcare Management for Pregnant Women in Rural China’, enacted by the MOH in 1989; and state programs such as the ‘Program for Chinese Women’s Development’ (1995–2000) and the national plan of action for the development of children: the ‘Outline of the Program for Chinese Children’s Development’ in the 1990s [11] .
A number of internationally supported programs provided financial investment and technical support for the development of rural health services, and in particular those targeted at maternal and child health. Most of these programs were implemented in poor rural areas. Details of the major programs conducted are given in Appendix. Activities conducted by the programs included: large scale skills training of grass-roots maternity and child health staff; construction of new facilities and refurbishment of old ones in the three-level health care system comprising county-level maternal and child hospitals/stations, township hospitals and village clinics; purchase of medical equipment; and since the re-establishment of the New Co-operative Medical Scheme (NCMS), support for poor pregnant women to participate in the scheme or to exempt them from payment for maternal healthcare, especially for hospital delivery care. For example in the ‘Health VIII’ program 1,107 township health centers were constructed or refurbished at a total cost of 273.81 million yuan. An evaluation of “Reinforcing Chinese MCH and Family Planning Services” (funded by UNICEF/UNFPA) (Project 1 in Appendix) found improvements in the maternal and child health working environment and service capacity in the 305 pilot counties. A number of evaluative studies have shown that the access to the use of maternal care increased markedly after the implementation of these programs [18–24].
The more rapid increases in utilization in rural than urban areas, and particularly in the poorest rural areas may be partly attributed to the focus of these development programmes on socio-economically less developed rural areas. However, it may also be due to the already relatively high utilization in urban areas, making further progress harder to achieve. In 2003, women in urban areas were 1.39 times more likely than rural women to receive their first antenatal care visit within 12 weeks of gestation, 1.36 times more likely to deliver in hospital, and 1.18 times more likely to receive a postnatal care visit, indicating that the rural–urban inequities had been decreased though not eliminated. However, the situation is more complex than this, as the proportion of women whose utilization of prenatal care met Chinese MOH standards varied substantially between types of city and rural areas, respectively. The distribution of hospital delivery rates was evidently in favour of the richest type of rural areas. In early 2000s women in the richest rural areas were 4.6 times more likely to utilize ante-natal care according to MOH standards than their counterparts in the poorest rural areas. Women in the richest rural areas were 2.8 times more likely to deliver in hospital, 1.81 times more likely to receive post-natal care and 2.87 times more likely to have assistance from trained staff than those in the poorest rural areas. It is also interesting to note that the utilization in type 1 rural areas was approaching the average level in urban areas.
These disparities are hidden by the averages for both rural and urban areas, and indicate the continuing internal variations in socio-economic and health systems development across different regions of Chinese mainland. For instance, the economic development of rural areas of administration districts in the eastern coastal areas such as the Yangtze River and Pearl River Deltas is likely to approach and may even exceed that of small inland cities, especially those in the remote western provinces. Inter rural and inter-urban disparities therefore require attention in addition to the narrowing gap in average levels between urban and rural areas.
Despite the more rapid increase in utilization in rural areas, the absolute level of utilization of some services remained unacceptably low in rural areas in early 2000s. For instance, the hospital delivery rate in the poorest rural areas was only 33.20%, which was far below the target of 65% set in the Guideline of Chinese Women Development from 2000 to 2010. Another noteworthy phenomenon is that the proportion of delivery out of hospital attended by trained staff decreased continually. The reasons for this need further investigation, but it is likely that the policy focus on improving hospital delivery rates had been at the expense of ensuring trained assistance for those who deliver at home, to the detriment of care for some women who cannot or are reluctant to access hospital deliveries, such as women with ‘illegal’ pregnancies. In some counties birth certificates and healthcare cards are only issued for babies born in health facilities [25].
In addition, some indicators stagnated or even decreased in the second 5 year period; for instance, the proportion of first prenatal visits within 12 weeks of gestation in small and medium-sized cities decreased from 1997 to 2003; and the proportion of post-natal care visits decreased slightly in both urban and rural areas, though no statistical significance was found with the changes in the former. There was little improvement in the proportion of frequency of prenatal care visits meeting MOH standards in urban areas during the second half of the study period. Stagnation and decreases may have been due to: the effects of ongoing health sector reforms, including decentralization of the management of rural hospitals to local government leading to management problems and lack of attention to preventive care; and increases in out-of-pocket payments for healthcare and healthcare costs relative to income level [5, 6, 8, 25].
Conclusion
The rural–urban gap in service utilization on average was significantly narrowed in terms of maternal healthcare in China from 1991 to 2003. This demonstrates that significant achievements in reducing inequities can be made through a combination of socio-economic development and targeted investments in improving health services, including infrastructure, staff capacities, and subsidies to reduce the costs of service utilization for the poorest. However, the huge gap which still remained among cities of different size and within different types of rural areas indicated the need for further efforts to support the poorest areas. Equity analyses need to be nuanced enough to identify the remaining disparities between different types of rural and urban areas in addition to the broad rural–urban inequities. In addition, attention may be required to the potentially exclusionary effects of some policies for some groups such as women whose pregnancies were not approved by local family planning authorities or the poorest of the poor. The experience of stagnation in some areas also indicates that further improvement may be harder to achieve and may require new policy efforts to address those inequities exacerbated by health sector reforms.
Notes
The population of a large city was above 1 million, and a small city was categorized as less than 0.3 million. The size of a city tends to be indicative of a higher level of economic development and a greater allocation of healthcare resources.
References
Tang, S., Meng, Q., Chen, L., Bekedam, H., Evans, T., & Whitehead, M. (2008). Tackling the challenge to health equity in China. Lancet, 372, 1493–1501.
Feng, X., Tang, S., Bloom, G., Segall, M., & Gu, X. (1995). Cooperative medical schemes in rural China. Social Science and Medicine, 41, 1111–1118.
Liu, Y., Rao, K., & Fei, J. (1998). Economic transition and health transition: comparing China and Russia. Health Policy, 44, 103–122.
Ministry of Health. (2007). China health statistics yearbook 2007. Beijing: China Union Medical University Press.
Kaufman, J., & Jing, F. (2002). Privatization of health services and the reproductive health of rural Chinese women. Reproductive Health Matters, 10, 108–116.
Gao, J., Qian, J., Tang, S., Eriksson, B., & Blas, E. (2002). Health equity in transition from planned to market economy in China. Health policy and Planning, 17(Suppl 1), 20–29. Oxford University Press.
Gu, X., Tang, S., & Gao, S. (1995). The financing and organization of health services in poor rural China: A case study in Donglan County. International Journal of Health Planning and Management, 10, 265–282.
Tang, S., & Bloom, G. (2000). Decentralizing rural health services: A case study in China. International Journal of Health Planning and Management., 15, 189–200.
The MDG Africa Steering Group. (2008). Achieving the millennium development goals in Africa: Recommendations of the MDG Africa steering group.
Countdown Coverage Writing Group. (2008). Countdown to 2015 for maternal, newborn, and child survival: the 2008 report on tracking coverage of interventions. Lancet, 371, 1247–1258.
Guo, Y., Zakus, D., & Liang, H. (2008). China: Policy and practice of MCH since 1990 s. Maternal and Child Health Journal, 12, 138–148.
Tang, S., Li, X., & Wu, Z. (2006). Rising cesarean delivery rate in primiparous women in urban China: Evidence from three nationwide household health surveys. American Journal of Obstetrics and Gynecology, 195, 1527–1532.
Center for Health Statistics and Information, MOH. (2004). An analysis report of national health services survey in 2003. Xiehe Medical University Press.
Ministry of Health. Guideline on quality of maternal care for both urban and rual areas. http://www.people.com.cn/item/flfgk/gwyfg/1985/407104198502.html.
Anson, O. (2004). Utilization of maternal care in rural Hebei province, the People’s Republic of China: Individual and structural characteristics. Health Policy, 70, 197–206.
Liu, Y., & Liu, G. (2007). Summary report of strengthening China Basic Health Services Project. China: Political and Financial Press.
Tolhurst, R., Zhang, T., Yang, H., Gao, J., & Tang, S. (2004). Factors affecting the implementation of health legislation and its impact on the rural poor in China: A case study of implementation of the Maternal and Infant Health care Law in two poor counties. International Journal of Health Planning and Management, 19, 247–265.
Park, R. (1996). China’s great achievement in strengthening MCH/FP at grassroots level program. Maternal and Child Health Care of China, 11(6), 21.
Wang, F. L. (1996). Push MCH by making great effort to do cooperative health projects. Maternal and Child Health Care of China, 11(6), 2–10.
Wang, Y. Z. (2004). An investigation on public health issues in western China. Review of Economics Research 54, 2–8, 33.
Chen, H., et al. (2004). Evaluation on maternal health of Health VI project at village level. Maternal and Child Health Care of China, 18(9), 524–526.
Peng, Y. (2000). Fulfill the goals set in the “Women and Children Development planning” by careful implementing the project “Reduce the maternal mortality and eliminate the incidence of tetanus infection of newborn babies”. Maternal and Child Health Care of China, 15(2), 68–72.
MOH. (2003). A summary of the project of “Decrease the maternal mortality and annual newborn infant tetanus”. http://www.MOH.gov.cn.
Yan, G., Zhuochun, W., Huijing, S., et al. (2007). Effects of health VIII project on maternal health service utilization. Chinese Primary Health Care, 21(12), 8–10.
Tao F. B., Huang K., Long X., Tolhurst R., & Raven J. (2010). Low postnatal care rates in two rural counties in Anhui province China: Perceptions of key stakeholders, Midwifery (forthcoming).
Acknowledgments
This document is an output from the project “Structural hinders to and promoters of good maternal care in rural China—CHIMACA (015396)”, funded by the European Commission INCO Program and co-ordinated by the National Institute for Health and Welfare, Helsinki, Finland.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 6.
Rights and permissions
About this article
Cite this article
Wu, Z., Lei, P., Hemminki, E. et al. Changes and Equity in Use of Maternal Health Care in China: from 1991 to 2003. Matern Child Health J 16, 501–509 (2012). https://doi.org/10.1007/s10995-011-0773-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-011-0773-1