Abstract
A combined measure of optimal antenatal care can provide more information on the role it plays in maternal health. Our objectives were to investigate the determinants of a measure of optimal antenatal care and the associated pregnancy outcomes. Data on 7,557 women taken from the 2004 Demographic and Health Survey in Cameroon were used to develop a new measurement of optimal antenatal care based on four indicators: at least four visits, first visit in first trimester, last visit in third trimester and a professional provider of antenatal care. We studied the relationship of this new variable with other related variables in a multivariate analysis, taking into account the complex study design. Almost sixty six percent of the women had optimal antenatal care. Secondary or higher education (OR 1.74; 95% CI 1.28–2.36), greater wealth (OR 2.31; 95% CI 1.73–3.1), urban residence (OR 1.42; 95% CI 1.12–1.82) and parity of 3–4 (OR 0.79; 95% CI 0.62–0.99) were independently associated with optimal antenatal care. Women with optimal antenatal care were more likely to deliver in a health unit (OR 2.91; 95% CI 2.42–3.49), to be assisted by a skilled health worker during delivery (OR 1.88; 95% CI 1.49–2.37) and to have a baby with a normal birthweight (OR 1.62; 95% CI 1.11–2.38). Obtaining and using a new measure for ANC is feasible. The association of optimal antenatal care to education, wealth and residence in this study, consistent with others, highlights the role of the country’s development in maternal health.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
More than 500,000 women die each year from pregnancy-related causes. Ninety-nine percent of these deaths occur in developing countries [1]. There are two main points at which we can intervene to prevent these maternal deaths and morbidity: antenatal care (ANC) and intrapartum care (during labor and delivery). Providing universal care during the more unpredictable and short period of labor and delivery is a more challenging task than in the longer and more stable antenatal period. Even though antenatal interventions may not address some of the major causes of maternal deaths, the use of ANC services is positively associated with the use of safe delivery [2]. The potential of ANC in improving maternal and fetal outcome has been recognized and voiced in many international conferences since 1990, and frequently surfaces as a cause for concern [3]. Universal access to reproductive health services (ANC and others) is one of the indicators of the fourth United Nations’ Millennium Development Goal (MDG), aimed at reducing maternal mortality [4].
The provision of ANC services depends mostly on organizational issues, but the determinants of its use are complex and multi-factorial. The use of ANC services is determined by personal and family factors (socio-demographics such as education, marital status, income, place of residence and the woman’s degree of autonomy), obstetric history (parity, gravidity), and organizational factors (availability of care, accessibility of care and quality of care) [3, 5–9].
The number of visits is used as an indicator for ANC coverage. The WHO recommends four goal-oriented visits during pregnancy [10]. Worldwide about 47% of pregnant women have at least four ANC visits and up to 97% in some developed countries. In sub-Saharan Africa the ANC coverage for at least four visit is 42%, and as low as 32% in the least developed countries [11]. In 2004, the ANC coverage for at least four visits in Cameroon was 60% [12].
Cameroon is a central African country with a population of about 18.5 million [11]. The total expenditure on health as a percentage of the Gross Domestic Product (GDP) is only 5.2% [13]. Government expenditures on health amount to only 28.1% of total health expenditures, implying that household expenditures are disproportionately high. There are 2.0 physicians and 16.0 nursing and midwifery personnel per 10,000 population [13]. The maternal mortality ratio (MMR) of 1,000/100,000 births is only a reflection of these health system constraints [11].
In recent years the importance of a more encompassing measure for ANC has been recognized. Other authors have used timing of first visit and provider of care to measure the utilization and access to ANC [5, 14]. The Kessner index measures the adequacy of ANC using the timing and number of visits. It’s more recent adaptation, the Adequacy of Prenatal Care Utilization (APNCU) index, incorporates the timing of initiation of pregnancy and the expected number of visits during the time the woman is actually in prenatal care [15]. These indices do not take into account the timing of the last visit, or the content of care provided. In regions where ANC coverage is low and there are marked human resource shortages, the provider of care may play a more important role than in countries where all providers are qualified; therefore information on the provider of care should be included in the assessment of ANC. If all the factors involved in ANC are not taken into account, information about the quality of care is omitted and its potential in improving maternal and fetal outcomes may be underestimated.
In this study, we aimed to investigate the determinants of ANC and the associated pregnancy outcomes using a new summary measure, optimal ANC, which includes the number of visits, timing of visits and provider of care.
Methods
This is a cross sectional retrolective and analytical study based on Demographic and Health Survey (DHS) data sets for 2004 in Cameroon. The DHS survey procedures were reviewed and cleared by the National Ethics Committee. In brief, the DHS is a nationwide household survey using a multistage cluster sample [12]. Data is collected on health, health related knowledge, attitudes and behaviors, maternal and child mortality, socioeconomic status and education. Details of the DHS methods are described elsewhere [16].
The target population for our analyses were women aged 15–49 residing in Cameroon. A total of 10,462 households were visited and 10,656 women were interviewed of which 7,557 had delivered in the last 5 years.
Variables
We analyzed variables which are likely to influence the use of maternal care services and pregnancy outcomes. A review of current literature provided a list of variables found to be associated with maternal care and pregnancy outcomes. We included socio-demographic variables (age, wealth, education, residence, marital status and religion), obstetric variables (parity, age at first birth and pregnancy terminations) and the women’s say in her health care. As outcome variables we included assistance during delivery, place of delivery and pregnancy outcomes (type of delivery and birth weight). Selected variables are defined in Table 1.
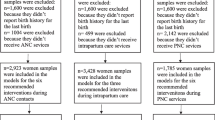
ANC was defined by a composite new variable denoting optimal ANC. To be classified as having optimal care, a woman must have had at least four visits, with the first in the first trimester, the last in the third trimester, and at least one visit from a skilled health provider. Only 2,450 women had sufficient data to be classified as having optimal care or not (Fig. 1).
Flow diagram of study population. Source: Data from the 2004 demographic and health survey in cameroon [12]
Data Analysis
Univariate analysis between socio-demographic variables, obstetric history, the woman’s decision making and optimal ANC were carried out using the Chi-square test with statistical significance defined at the alpha level of 0.05. Additionally, we analyzed the association between optimal ANC and birth weight, type of delivery, place of delivery and assistance during delivery. Multivariate logistic regression was carried out and ANC was dichotomized as: optimal ANC or suboptimal ANC. Only variables with statistically significant associations in the univariate analysis (α ≤ 0.05) were introduced into the model. Education, wealth and residence were entered as a block and the rest of the variables were forward introduced. Variables that included more than 25% missing data were excluded from the analysis. Odds Ratios (OR) and 95% Confidence Intervals (CI) are presented.
Data was analyzed using the Complex Samples Procedures program of the Predictive Analytic Software (PASW) Version 17.0 (SPSS, Inc., 2009, Chicago, IL, USA) which corrects for a complex sample design. In order to allow for these corrections, a plan file was created, including descriptions of the sample stages, strata, clusters and the weights of the individuals.
Due to a decrease of the sample size as a consequence of missing data, we compared the women with missing data on optimal ANC to the women with available data. There were statistically significant differences in age, residence, education, wealth and religion. The younger (15–19 years) and older (40–49 years) women, with secondary or higher education, residing in urban regions and who were single were more likely to have missing data. Equally, the wealthier women who were neither Christian nor Moslem, were more likely to have missing data (P < 0.001).
Results
Demographic Characteristics of Respondents
There were 7,557 women (70.9% of those interviewed) who had given birth in the last 5 years. Their socio-demographic characteristics are shown in Table 2. The mean age of our sample was 27.29 (± 0.11 standard error) and equal numbers resided in rural and urban areas. About one in five women and their partners had no education. More than a third were married and close to half fell into the two highest quintiles in the distribution of wealth. The majority were Christian.
Determinants of Optimal ANC
Two thirds (65.9%) of the 2,540 women with complete data had optimal ANC. In the univariate analysis, age, residence, education, wealth, final say in health care decisions and age at first delivery were positively associated with optimal ANC (data not shown).
In the multivariate analyses (Table 3), education, place of residence and wealth, remained associated with optimal ANC, but not the other socio-demographic variables. Among the obstetric variables, only parity was associated with optimal ANC. The woman’s final say in health care was no longer associated with optimal ANC.
ANC and Outcomes of Pregnancy
Women with optimal ANC were two times more likely to have had a Caesarean section (OR 2.52; 95% CI 1.21–5.23). After adjustment for the effects of parity, education, age, residence, wealth, and the woman’s final say in health care the association between optimal ANC and Caesarean sections disappeared (OR 1.51; 95% CI 0.67–3.26). Only education (OR 2.57; 95% CI 0.83–7.79) and wealth (OR 2.9; 1.00–8.18) remained associated with Caesarean deliveries.
Women with optimal ANC were more likely to have had a baby with a normal birthweight before and after adjustment (OR 1.76; 95% CI 1.21–2.56; Table 4).
ANC, Place of Delivery and Assistance During Delivery
Women who had optimal ANC were almost three times more likely (OR 2.9; 95% CI 2.42–3.49) to deliver in a health unit and almost two times more likely (OR 1.88; 95% CI 1.49–2.38) to be assisted by a skilled worker during delivery.
Discussion
We found that education, wealth, residence and parity affect a woman’s chances of having optimal ANC. Women who had better ANC had higher chances of delivering in a health unit, being assisted by a skilled health worker during delivery, and having a baby with normal birthweight.
Since our study was a secondary analysis of data from the 2004 DHS survey in Cameroon, we advise caution in the interpretation and generalization of these findings due to large amounts of missing data (Fig. 1). However, the comparison between women with missing data and women with available data indicates that mostly the educated, urban and wealthy women had missing data.
Measuring ANC
Access to ANC and use of ANC are two concepts which arise frequently in the measurement of ANC. They are meant to express the organizational aspects of provision of ANC services and the personal factors associated with seeking ANC.
We composed the variable optimal ANC, to provide a unique measure of multiple aspects of ANC, using four related variables: adequate number of visits, timing of first and last visits, and provider of care, as an expression of appropriately spaced out use, and the health workforce. These variables were chosen because they measure both use and availability of services. The consistency of our findings in regards to the determinants and outcomes associated with better ANC used in other studies provides additional weight for its use as a more comprehensive variable for the analysis of ANC [2, 3, 6, 17, 18].
Putting these variables together entails more requirements to classify as having good ANC, as it would require that women go for at least four visits, to a skilled health provider starting in the first trimester and ending in the third trimester. It also combines aspects of ANC for which there are known socio-demographic differences, conditions of delivery and pregnancy outcomes. Several studies found that a greater number of visits, earlier visits and having a skilled provider of ANC were all independently associated with wealth, education, residence, more use of skilled assistance at birth and better birth weights [2, 3, 5, 6, 17].
Unfortunately, this measure doesn’t take into account the duration of gestation. Women who did not make it to the third trimester would therefore be counted as having either an insufficient number of visits or poorly spaced out visits.
Predictors of Optimal ANC
Wealth, residence, education and parity all contributed independently to the association with optimal ANC. These variables are known factors associated with a greater number of visits in pregnant women worldwide [3, 11, 19]. Studies in Nigeria and Kenya found higher education to be associated with earlier first visits and a greater number of visits [5, 20]. An early first visit may leave more time for more visits before confinement, and the qualified providers of care may actively encourage women to come for more visits. Another study reported that wealthier and more educated women were more likely to seek care from a medically trained person [14]. Urban–rural differences in timing of first visits, provider of care and number of visits have been described in other observational studies and a systematic review [6, 14]. These findings consistently demonstrate large inequalities in the use of ANC services by residence, wealth and education.
Final say in health care was associated with optimal ANC in the univariate analyses. These women had fewer visits, late first visits and early last visits. This association disappeared in the multivariate analyses when we controlled for other factors. A similar variable, woman’s autonomy, has been shown by others to have an influence on the use of ANC services [6]. Other factors like marital status and desirability of the pregnancy may play a significant role. These findings suggest that final say in health care does not directly influence a woman’s chances of having optimal ANC. Since final say in health care was measured by just one variable in this study, it might have been insufficient to address the complexity of the social dynamics involved in the decision making process.
The relationship with parity was in favor of the women with smaller [1, 2] and larger (5+) parities. Clinically, the primiparae (one delivery) and the grand multiparae (five or more deliveries) are those most likely to elicit concern from health workers and more emphasis may be laid on providing more care for them. However, some authors have described a negative association between parity and the use of ANC, [3, 19] owing to overconfidence from the multiparae [19].
Optimal ANC and Pregnancy Outcomes
The association between optimal ANC and Caesarean sections in the univariate analysis disappeared when we controlled for other factors. Some of these socio-demographic and obstetric factors like age and parity were included in the model, but had no effect. Higher education and increased wealth were associated with higher chances of having a Caesarean section. There are clinical factors like duration of labor, fetal health and eclampsia that will influence the decision of the physician to perform a Caesarean section. The DHS data set doesn’t include information on clinical conditions. In Cameroon, health care is purchased individually, by out-of pocket payments; therefore wealth can influence a woman’s chances of having a Caesarean section. This and other factors around the delivery period have a stronger influence than optimal care on whether a woman would have a Caesarean section. Since wealth is associated with optimal ANC, it would play a double role in ensuring optimal ANC on one hand and financing for a Caesarean section on the other hand.
Optimal ANC remained a strong predictor for normal birthweight even after controlling for confounders. Brown et al. found that two ANC visits were associated with normal birthweights and the association remained the same with even more visits [20]. Other studies have reported a strong association between number of visits and birthweights [17, 21]. Showstack et al. found that the strength of the association was reduced when only the timing of first visit was used to define ANC as being adequate [17]. Kotelchuk also demonstrated a positive association between birthweight and ANC, using the APNCU index [18]. Birthweight is an outcome that depends on many factors, some of which can be influenced by ANC.
Optimal ANC, Place of Delivery and Assistance During Delivery
Women who had optimal ANC were more likely to deliver in a health unit and to have skilled assistance during delivery. These two variables go together as it would be improbable to find a health unit without a skilled health worker. A systematic review reported more use of skilled assistance during delivery in women who had better ANC, higher education, more wealth and who lived in urban regions [19]. Place of delivery and assistance during delivery have been described as reasons for better outcomes in women who use more ANC [20]. Other studies have documented greater use of skilled assistance during delivery with increasing number of visits [2, 3]. This relationship is the mainstay of the efficacy of ANC in reducing maternal mortality, and its absence in any research would be a cause for concern.
Limitations of the Study
This study was based on a large representative national data set. However, there are some limitations. Being a secondary analysis, we had little influence over the variables in the data set. There was also a considerable amount of missing data. Information bias can be expected as the women’s recall may not be accurate after 5 years and they may over-report practices that are thought to be desirable e.g. number of ANC visits leading to an overestimation of the proportions of women with these attributes.
Using only one variable for ANC (at least four visits), the 2004 DHS reported a coverage of 60%. We found that 65.9% of the women had optimal ANC. This apparent contradiction arises from the fact that optimal ANC is a more stringent measure and that fewer women had sufficient data to be classified for ANC.
Conclusions
A more encompassing indicator of ANC is feasible to obtain. Maternal education, greater wealth and urban residence stand out as the main factors associated with optimal ANC care in Cameroon. The overall picture of ANC usage and consequently maternal mortality in Cameroon can be improved by addressing developmental issues. The achievement of the fifth MDG aimed at improving maternal health requires not only an improvement in access to and use of health care, but also an improvement in female education and socioeconomic status. The improvement of maternal health is thus strongly tied with the first MDG (eradicate extreme poverty and hunger) and the second (universal primary education). Optimal ANC is associated with better pregnancy outcomes such as birth weight. It is also associated with deliveries in a health unit and with skilled assistance at delivery, both of which contribute to better pregnancy outcomes.
References
Nawal, M. N. (2008). An introduction to maternal mortality. Reviews in Obstetrics and Gynecology, 1, 77–81.
Bloom, S., Lippeveld, T., & Wypij, D. (1999). Does antenatal care make a difference to safe delivery? A study in urban Uttar Pradesh, India. Health Policy Plan, 14, 38–48.
Abou-Zahr, C., Wardlaw, T. (1990–2001). Antenatal care in developing countries: Promises, achievements and missed opportunities: An analysis of trends, levels and differentials. http://www.childinfo.org/files/antenatal_care.pdf.
United Nations’ Millennium Development Goals. http://www.un.org/millenniumgoals/.
Adekanle, D. A., Isawumi, A. I. (2008). Late antenatal care booking and its predictors among pregnant women in south western Nigeria. Online Journal of Health and Allied Sciences, 7(1), 4. http://www.ojhas.org/issue25/2008-1-4.htm.
Say, L., & Raine, R. (2007). A systematic review of inequalities in the use of maternal health care in developing countries: Examining the scale of the problem and the importance of context. Bulletin of the World Health Organization, 85, 812–819.
Lavender, T., Downe, S., Finnlayson, K., Walsh, D. Access to antenatal care: A systematic Review. http://www.cemach.org.uk/getattachment/dbeebce9-4625-4bbe-bfcd-fec2be076ccc/Access-to-antenatal-care-(Literature-review).aspx.
Downe, S., Finlayson, K., Walsh, D., & Lavender, T. (2009). Weighing up and balancing out: A meta-synthesis of barriers to antenatal care for marginalised women in high-income countries. BJOG, 116, 518–529.
Simkhada, B., Teijlingen, E. R., Porter, M., & Simkhada, P. (2008). Factors affecting the utilization of antenatal care in developing countries: Systematic review of the literature. Journal of Advanced Nursing, 61, 244–260.
Villar, J., Bakketeig, L., Donner, A., Al-Mazrou, Y., Ba’aqeel, H., Belizán, J. M., Carroli, G., Farnot, U., Lumbiganon, P., Piaggio, G., Berendes, H. (1998). The WHO antenatal care randomised controlled trial: Rationale and study design. Paediatric and Perinatal Epidemiology, 12(suppl 2), 27–58.
UNICEF. (2009). State of the world’s children. Maternal and newborn health. http://www.unicef.org/sowc09/report/report.php.
Institut National de la Statistique (INS) et ORC Macro. (2004). Enquête Démographique et de Santé du Cameroun [Cited 2010 July 28]. Available from: http://www.measuredhs.com/aboutsurveys/search/metadata.cfm?surv_id=232&ctry_id=4&SrvyTp=.
WHO Statistical Information System [Online]. (2008). [Cited 2009 July 28]. Available from: http://apps.who.int/whosis/data/Search.jsp?Indicators=[Indicator].[HSR].Members.
Rahman, M., Islam, R., Islam, A. Z. (2008). Rural-urban differentials of utilization of ante-natal health-care services in Bangladesh. Health Policy and Development, 6, 117–125. http://www.bioline.org.br/request?hp08015.
Kotelchuk, M. (1994). An evaluation of the kessner adequacy of prenatal care index and a proposed adequacy of prenatal care utilization index. American Journal of Public Health, 84, 1414–1420.
Measure, D. H. S. (2009). Demographic and health surveys. Survey Methodology. [Online]. [Cited 2009 July 29] Available from: http://www.measuredhs.com/aboutsurveys/methodology/process.cfm.
Showstack, J. A., Budetti, P. P., & Minkler, D. (1984). Factors associated with birthweight: an exploration of the roles of prenatal care and length of gestation. American Journal of Public Health, 74, 1003–1008.
Kotelchuk, M. (1994). The adequacy of prenatal care utilization index: Its US distribution and association with low birthweight. American Journal of Public Health, 84, 1486–1489.
Jimoh, A. A. G. (2003). Utilisation of antenatal services at the provincial hospital, Mongomo, Guinea Equatoria. African Journal of Reproductive Health, 7, 49–54.
Brown, A. C., Sohani, B. S., Khan, K., Lilford, R., & Mukhwana, W. (2008). Antenatal care and perinatal outcomes in Kwale district, Kenya. BMC Pregnancy Childbirth, 8, 2.
Siza, J. E. (2008). Risk factors associated with low birth weight of neonates among pregnant women attending a referral hospital in northern Tanzania. Tanzania Journal of Health Research, 10, 1–8.
Acknowledgements
We are grateful to the Legacy Heritage International Master of Public Health Program and the Hebrew University-Hadassah, Braun School of Public Health and Community Medicine. This work is based on the MPH thesis of Lawrence Mbuagbaw tutored by Rosa Gofin. We are also grateful to Measure DHS for providing us with the 2004 Cameroon DHS data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mbuagbaw, L.C.E., Gofin, R. A New Measurement for Optimal Antenatal Care: Determinants and Outcomes in Cameroon. Matern Child Health J 15, 1427–1434 (2011). https://doi.org/10.1007/s10995-010-0707-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-010-0707-3