Abstract
Objective of the study was to explore factors associated with early childhood obesity and assess whether having a foreign born mother is protective against childhood obesity. Data sources include 9 months and 4 years parent interviews and direct assessments of possessive children’s weight and height (4 years) or length (9 months) from the Early Childhood Longitudinal Study-Birth Cohort. Subjects were children with anthropometric measures who lived with their mothers (n = 9,700 at 9 months and 8,200 at 4 years). Overweight is defined as a weight-for-length ratio at or above the 95th percentile at 9 months; obesity is defined as a body mass index at or above the 95th percentile at 4 years. The prevalence of overweight/obesity was 15.4% at 9 months and 18.0% at 4 years. After adjustment for potential confounders, having a foreign-born mother was not associated with the odds of overweight at 9 months or 4 years. At 9 months and 4 years, low birth weight, pre-pregnancy weight and weight gain during pregnancy were protective of overweight. In addition to these factors, at 4 years, excessive weight gain in the first 9 months was the strongest predictors for obesity. Living in a safe neighborhood and ever having breastfed were protective against obesity. Having a foreign born mother is not protective of early childhood obesity. A focus on health of women prior to conception and on women’s and infants’ health in the perinatal period are key to addressing childhood obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United States, obesity continues to be a major public health concern [1]. The prevalence of overweight among children increased dramatically during the last 30 years. This increase has been marked across all gender, racial and socioeconomic groups [2]. Data from the National Health and Nutrition Examination Surveys (NHANES) show that among pre-school children the prevalence of obesity increased from 5.0 to 13.9% between 1971–1974 and 2003–2004 [3]. Pooled NHANES data from 2003–2006 reveal that 24.4% of children ages 2–5 years in the United States were at or above the eighty-fifth percentile of the 2000 Centers for Disease Control and Prevention (CDC) body mass index (BMI)-for-age growth charts [4]. In 2005, data from the Early Childhood Longitudinal Study-Birth Cohort (ECLS-B) show the prevalence of obesity among 4 year old children alone was 18.4%. The higher percentages in the ECLS-B study were attributed largely to differences in weight assessment methods and older ages of the children relative to those in NHANES [5].
Early childhood obesity is likely to persist throughout the life span [6–8]. In addition to increasing the risk of obesity and its associated consequences in later life, childhood obesity also is associated with a wide spectrum of serious adverse outcomes including pediatric hypertension [9], type II diabetes mellitus [10], and coronary heart disease [11, 12]. Moreover, obese children experiences psychosocial difficulties such as mood disorders [13] and low self esteem [14].
The foreign-born population, currently representing 12% of the population, is a rapidly growing group in the United States [15]. The proportion of children living with at least one foreign-born parent increased from 12% in 1990 to 22% in 2007 [16, 17]. Immigrants have longer life expectancy, lower BMI, and lower risks of smoking, hypertension, and chronic conditions than the US-born population [18–20]. Immigrants also have better perinatal health; foreign-born women are less likely to have low birth weight babies (<2,500 g), as well as to experience preterm delivery and perinatal mortality [21, 22].
Researchers suggest several explanations for better health among the foreign-born. According to the notion of “healthy immigrant effects” or “positive immigrant selectivity,” people immigrating to the United States are thought to be a select group in that they are healthier than those who remain in their countries of origin [23–25]. The second explanation suggests that immigrants are more likely to possess norms and values that are protective of risky behaviors such as smoking, drinking, and unhealthy diets [26–28]. Third, immigrants may have stronger social and familial support and better social integration compared to the US-born population [29].
An acculturation process with regard to health is documented in some studies. Adult immigrants who have lived in the US for more than 10–15 years have health approaching that of native-born Americans [28, 30]. With greater length of residence in the U.S, immigrants are more likely to adopt the diets and lifestyles of residents in the host country, resulting in increasingly similar health outcomes. However, this process appears to differ by education and age at migration. For example, Kaushal and colleagues [31] found that immigrants with a bachelors degree or higher did not experience any change in the risk of obesity with increased duration of stay in the U.S; the risk of obesity, however, increased among those without a bachelors degree and with greater duration of stay. Age at arrival also affects the process of assimilation. Findings from a study by Roshania and colleagues [32] suggest that the relation between duration of residence and overweight or obesity prevalence varied by age at arrival; immigrants who arrive at a relatively young age are more likely to adopt the eating habits and lifestyles of the host country.
Although studies suggest that the prevalence of obesity is lower among immigrants compared with native-born adults, whether or not having a foreign born mother protects against childhood obesity remains unclear. The aim of our study was to explore factors associated with early childhood obesity and assess whether having a foreign born mother is protective for obesity in children.
Methods
Data sources and study sample
The data used in this study are from the Early Childhood Longitudinal Study- Birth Cohort (ECLS-B). ECLS-B is a nationally representative sample of about 10,700 children born in the U.S. in 2001 and followed prospectively. ECLS-B excludes children born to mothers less than 15 years of age and children who died or were adopted before 9 months. Data sources include birth certificates, direct child assessments at 9 months and 4 years, and computer assisted parent interviews at 9 months and 4 years. ECLS-B data also were collected when children were 2 years (range 16–39 months). However, data at 2 years were not used due to different measurements of attained size (length ≤24 months; height ≥24 months) and, accordingly, different reference populations [33]. Birth certificates provide data on prenatal and neonatal characteristics at the time of the child’s birth. Direct child assessments provide information regarding the child’s physical growth. Parents reported on family socio-demographic characteristics, maternal education and employment, feeding practices and children’s physical and sedentary activities at both times.
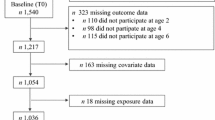
At 9 months and 4 years, we included children who had complete data on weight and length and whose biological mothers or other type of mother were interviewed. We also excluded outliers for z values for weight-for-length at 9 months (about 100), weight gain in the first 9 months (about 50), and weight gain after 2 years (about 50). About 9,700 and 8,150 children comprised the final analytic sample at 9 months and 4 years, respectively. The flow charts of the distribution of the samples are presented in Figs. 1 and 2.
Study variables
Dependent variables
Child’s weight and length/height were measured by certified interviewers during home visits. Child’s length at 9 months was measured with a Measure Mat [34], while height at 4 years was measured with a portable stadiometer [35]. The child’s weight was measured with a digital scale at both waves. At 9 months, the mother’s weight was subtracted from the combined weights of mother and child. At 4 years, weights for each child were measured directly (for example, the child stood on scale alone). Measurements were taken twice independently and recorded in the Child Assessment Booklet at 9 months and in the computer assisted data entry system at 4 years.
At 9 months, identifiable errors, such as a difference between repeat measurements greater than 5%, were reported to field supervisors who then would follow up with interviewers [33, 34]. Each physical measure was taken twice, and average scores used for differences <5%. For differences greater than 5%, the weight (length) closest to the weighted average weight (length) for the group of children in the sample of the same age and birthweight was used. At 4 years, a third measurement was obtained for differences ≥5%. The two length (height) and weight measurements were highly correlated (r = 0.81 for length and weight at 9 months; r = 0.99 for height and weight at 4 years).
Normalized (z-score) weight-for-length ratio at 9 months and body mass index (BMI) at 4 years were calculated. Overweight is defined as a weight-for-length ratio at or above the 95th percentile at 9 months; obesity is defined as a BMI at or above the 95th percentile at 4 years for age and sex using the 2000 Centers for Disease Control and Prevention growth charts for the United States.
Independent variables
Independent variables included family (household income, household food security, housing situation, language speak at home, perceived neighborhood safety), maternal (age, foreign-born status, education, employment, pre-pregnancy weight, weight gain during pregnancy, depressive symptoms, first born, plurality, exercise with rapid breathing and heartbeat) and child characteristics (birthweight, sex, race/ethnicity, weight gain during the first 9 months), feeding practices (ever breastfeed, to bed with bottle, >1 serving 100% juice daily, soda/sport/fruit drink daily, 3 daily vegetable servings, weekly fast food, days of eating dinner as a family, days of eating dinner at regular time) and physical activity (daily walk or play outside, organized athletic activity, >2 h daily TV, video and DVD on week days, TV rules/routines, computer use >3 times/week. Separate variables for household income, housing situation, and maternal education were used to assess the independent effects of different aspects of household socioeconomic status on child obesity.
For mothers not born in the U.S., maternal duration in the U.S. was calculated by subtracting the age she moved to U.S from the current age. We constructed two different categorical variables for maternal foreign-born status. The first one included: (1) not foreign born; (2) foreign-born, U.S stay ≤5 years; (3) foreign-born, U.S stay >5 years & ≤10 years; (4) foreign-born, U.S stay >10 years & ≤15 years; and (5) foreign-born, U.S stay >15 years. The second one grouped maternal foreign born status into (a) not foreign born; (b) foreign-born, U.S stay ≤10 years; and (c) foreign-born, U.S stay >10 years. There was no significant difference when we used each variable in the respective analyses. Here we present results using the latter.
Using tertile cut-offs, pre-pregnancy weight and weight gain were categorized into three groups: high, middle, low. Weight gain in the first 9 months was calculated by subtracting weight at birth from weight at 9 months and grouped into 5 categories using quintile cut-offs.
Maternal depressive symptoms were measured by the12-item version of the Center for Epidemiological Studies Depression Scale (CES-D). The CES-D assesses depressive feelings and behaviors during the past week [36]. The CES-D generates a scale 0–36 which was categorized into four groups—no, mild, moderate, and severe depressive symptoms, using 5, 10 and 15 as cut points.
Statistical analyses
Analyses were conducted in Stata 10. Due to the complex sample design [37], sample weights were applied to account for stratification, clustering, and unit non response. In keeping with the restricted-use data license agreement, all unweighted numbers are rounded to the nearest 50.
Bivariate analyses of the relation between each independent variable and the outcomes were performed. Weighted two-way tabulations were conducted to explore associations between possible risk factors and overweight/obesity. To examine the significance of these associations, Pearson chi-square statistics were computed and corrected for the survey design using the second-order correction. Extension of the Wilcoxon rank-sum test [38] was performed to examine the trend across ordered groups. Weighted simple logistic regression models were fit to estimate the unadjusted OR’s for each independent variables and outcome. Variables with P-value <0.20 in bivariate analyses were selected for multivariate analyses. After stepwise selection, significant variables for either 9 months or 4 years (P < 0.05) and those conceptually relevant and supported in the literature were included in weighted models.
Missingness was not a significant issue. For continuous variables it contributed to less than 3% of the sample while for categorical variables only 1%. For continuous variables, we used medians to impute the missing value; while for categorical variables, ad hoc imputation methods were used [39].
Results
Prevalence of foreign born and overweight/obesity
Among the 26.2% of mothers who were foreign-born, the mean duration in the U.S. was 10.4 years at 9 months (SE = 0.18) (Table 1). At 4 years, among the 24.9% mothers who were foreign-born, the mean duration was 13.7 years (SE = 0.18) (Table 2).
The weighted prevalence of overweight was 15.4% at 9 months. There was no significant difference between children with native-born versus foreign-born mothers, regardless of duration in the U.S. At 4 years, the weighted prevalence of obesity was 18.0% for the full sample, 14.9% for children with native-born mothers, 17.5% for children with foreign-born mothers who had stayed in the U.S. 10 years or less, and 17.3% for children with foreign-born mothers who had stayed in the U.S. more than 10 years. The prevalence of obesity was higher among children with foreign-born rather than native-born mothers (P < 0.05); there was no difference in the prevalence of obesity related to duration of stay of foreign-born mothers in the U.S. (P > 0.05).
Bivariate analyses
At 9 months, among family characteristics, speaking Spanish at home was significantly associated with higher odds of overweight (Table 1). At 4 years, household income more than $25,000 and food security were protective of obesity; not owning a home, speaking Spanish at home and perception of living in a less safe neighborhood were related to a higher odds of obesity (Table 2).
At 9 months, high pre-pregnancy weight was related to higher odds of overweight. Severe maternal depressive symptoms and multiple births were associated with lower odds of overweight. At 4 years, except for having foreign-born mothers, high pre-pregnancy weight and high weight gain during the pregnancy were strong predictors for obesity. Trend tests suggested that there were positive linear relations between pre-pregnancy weight and weight gain during the pregnancy with the odds of obesity. Higher maternal education and multiple births were protective against obesity.
Birth weight was a strong predictor for overweight at 9 months in bivariate analysis. Being black was associated with higher risk of overweight compared with being white; while being Asian was suggested to be protective. Although there was no association between ever breastfed with overweight, being put to bed with a bottle was related to 20% increase in the odds of overweight at 9 months. At 4 years, in addition to birth weight and being black or Hispanic, weight gain during the first 9 months was a strong predictor for obesity; a trend test suggested a dose–response effect of weight gain during the first 9 months on the odds of obesity at 4 years old (P = 0.000). Having more than 1 serving of 100% juice daily, consuming soda/sport/fruit drinks daily and watching more than 2 h daily TV/video/DVD on week days were positively associated with obesity at 4 years. Ever breastfed, more days of eating dinner as a family, organized athletic activity, and having TV rules were protective against obesity at 4 years.
Multivariate analyses
After controlling for other covariates, maternal foreign born status was not significantly associated with overweight at 9 months or obesity at 4 years; while maternal pre-pregnancy weight, weight gain during pregnancy, birth weight and plurality were strong predictors for both (Table 3).
At 9 months, having a mother with severe depressive symptoms was associated with a 38% decrease in the odds of overweight, but this effect waned by 4 years. Black children had 33% higher odds of being overweight and Asian children a 34% lower odds than white children. Going to bed with a bottle was associated with a 20% increase in the odds of overweight.
At 4 years, after adjustment for other covariates, a perception of living in a less safe neighborhood was associated with a 20% increase in the odds of obesity. One of the strongest predictors for obesity was weight gain in the first 9 months. Compared with children whose weight gain in the first 9 months was in the first quintile, the odds ratios for those whose weight gain in the first 9 months was in the third, fourth and fifth quintiles were increased by 85, 160 and 350%. Family characteristics, including not owning a home and speaking Spanish at home remained associated with higher odds of obesity after controlling for other variables; however they were only marginally significant (Table 3). The adjusted OR for obesity at 4 years was 0.76 (95% CI: 0.63–0.92, P = 0.01) for ever breastfeeding. Each 1 unit increase in days of eating dinner as a family was associated with a 5% decrease in the odds of obesity (P = 0.03).
Discussion
Several studies have documented a lower risk of obesity among adult immigrants in the U.S. [40–42]. Our study, however, is the first to examine the risk of early childhood obesity among children of immigrants compared with children of native born Americans. In our study, the prevalence of obesity was compared between children with foreign-born mothers and those with native-born mothers, using a large, nationally representative sample. There was no evidence that having a foreign born parent is protective of early childhood overweight or obesity.
Prior research suggests that some immigrants experience better health than the U.S. born, possibly due to “positive immigrant selectivity,” healthier behaviors or better social support. These factors may not protect their children from obesity. Foreign born immigrants are more likely to have lower family income and to live in low SES neighborhoods [43, 44]. These environmental factors may correlate with increased intake of high-fat, energy-dense food and decreased physical activity among children.
Children’s food acceptance and early exposure to fruits and vegetables are shaped by parental behavior [45], and parents’ feeding behaviors are influenced by environmental factors. For example, some urban neighborhoods lack places where healthy foods can be purchased, such as supermarkets and outdoor produce stands. Instead, there may be convenience stores and fast food outlets in their neighborhoods, making it difficult for parents to purchase fresh, healthy, and affordable products for their children [46].
Physical activity is another important aspect in childhood obesity which also may be influenced by environmental factors; children who live in neighborhoods with good access to parks and playgrounds tend to have less sedentary activity and reduced risk for obesity [47, 48]. Our findings suggested that parents’ perception of less safe neighborhoods was significantly associated with a higher risk of obesity among their children. Similarly, a US study showed that parents living in the inner city were more likely to be concerned about neighborhood safety and have children who were less likely to engage in physical activity than their suburban peers [49]. The reason why children were less physically active may be due to parents’ fears for their children’s safety, the key concerns being road safety and harm from strangers [50].
Prior studies have noted disparities between parents’ perceptions and their children’s risk of obesity [51]. Some parents may not recognize that their children are at risk for increased weight or be convinced of the risks associated with their child being obese; they may believe that their child will shed the excess weight when s/he grows up [52]. Also, some low income mothers indicate a preference for chubbier children and believe that such children are healthier and happier than normal-weight children [53, 54]. Different perceptions of children’s size may increase the risk of childhood obesity among immigrants.
Qualitative research has shown that immigrants in the U.S. are more likely to report limited social support and feelings of isolation [55]. The lack of help from friends or other family members may limit their ability to provide healthy meals or allow their children to play outside. Also, lack of social support, as a possible stressor for the mother, may generate behavioral responses including unhealthy eating habits and reduced physical activity among their children, in turn leading to increased risk of obesity [56]. We explored the effect of social support on early childhood obesity in our analyses. However, there was limited information available, and none of the variables used as proxies to measure social support, such as sources of support excluding spouses and number of family members in the community, were related to the risk of obesity.
The results of this study suggested that maternal pre-pregnancy weight, weight gain during pregnancy and early weight gain of infants were strong predictors of early childhood obesity. During the past decade, there has been growing interest in applying a life-course approach in studies about the development of childhood obesity [57, 58]. This approach is well suited for the study of childhood obesity because it conceptualizes the development of chronic disease as a lifelong dynamic process which is caused by genetic, biological, social, and environmental factors [59, 60]. Our results are consistent with the earlier findings about the positive relations between maternal BMI and obesity risk in offspring [58, 61–63], rapid weight gain in infancy and higher rates of overweight and body fat deposition among children [64–66].
We acknowledge some limitations in this study. First, ‘foreign born’ mothers in this study were those who were born outside the United States, while the U.S. Census Bureau uses this term to refer to those who are not U.S. citizens at birth [67]. Second, ECLS was not designed for the study of obesity. There is limited information on children’s nutrition, feeding patterns or physical activity, or on mother’s BMI after birth of the child; however the large sample, relative to NHANES and other studies, permits more refined analyses focused on preschool children. Third, there is not sufficient statistical power to perform subgroup analysis of children by the country of origin of their foreign-born mothers. We explored the subgroup of children with foreign born mothers from Mexico, but found no significant association between most independent variables and the odds of obesity. Finally, there were some losses to follow up of respondents between the two waves of data collection reported here which may cause selection bias. Our analysis suggested that children who were overweight at 9 months were more likely to drop out of the study at 4 years.
Despite these limitations, this study has some inherent strengths. To our knowledge, few studies have explored the effect of having foreign born parents on early childhood obesity. Direct measurement of weight and height/length for children in ECLS, a large national data set, provides reliable data about overweight/obesity. ECLS also includes information for the family, child and parents, allowing us to adjust for these factors in our analyses.
Several policy and programmatic implications could be drawn from our findings. It is important to focus on the health of women before conception and in the perinatal period to address childhood obesity. Collaboration between community and health care providers is needed to identify missed opportunities to address childhood obesity. Finally, monitoring childhood obesity among various immigrant groups may provide valuable insights into the role of potentially modifiable social, behavioral, and environmental factors.
References
National Task Force on the Prevention and Treatment of Obesity. (2000). Overweight, obesity, and health risk. Archives of Internal Medicine, 160(7), 898–904.
National Center for Health Statistics. (2007). Health, United States, 2007 with chartbook on trends in the health of Americans. Hyattsville, MD: US Department of Health and Human Services.
National Center for Health Statistics. (2006). Prevalence of overweight among children and adolescents: United States, 2003–2004. Hyattsville, MD: US Department of Health and Human Services. Accessed October 6, 2009, from http://www.cdc.gov/nchs/products/pubs/pubd/hestats/overweight/overwght_child_03.htm
Ogden, C. L., Carroll, M. D., & Flegal, K. M. (2008). High body mass index for age among US children and adolescents, 2003–2006. JAMA, 299(20), 2401–2405.
Anderson, S. E., & Whitaker, R. C. (2009). Prevalence of obesity among US preschool children in different racial and ethnic groups. Archives of Pediatrics and Adolescent Medicine, 163(4), 344–348.
Mei, Z., Grummer-Strawn, L. M., & Scanlon, K. S. (2003). Does overweight in infancy persist through the preschool years? An analysis of CDC pediatric nutrition surveillance system data. Sozial- und Praventivmedizin, 48(3), 161–167.
Dubois, L., & Girard, M. (2006). Early determinants of overweight at 4.5 years in a population-based longitudinal study. International Journal of Obesity, 30(4), 610–617.
Taveras, E. M., Rifas-Shiman, S. L., Belfort, M. B., Kleinman, K. P., Oken, E., & Gillman, M. W. (2009). Weight status in the first 6 months of life and obesity at 3 years of age. Pediatrics, 123(4), 1177–1183.
Belfort, M. B., Rifas-Shiman, S. L., Rich-Edwards, J., Kleinman, K. P., & Gillman, M. W. (2007). Size at birth, infant growth, and blood pressure at three years of age. Journal of Pediatrics, 151(6), 670–674.
Steinberger, J., Moran, A., Hong, C. P., Jacobs, D. R., Jr., & Sinaiko, A. R. (2001). Adiposity in childhood predicts obesity and insulin resistance in young adulthood. Journal of Pediatrics, 138(4), 469–473.
Field, A. E., Cook, N. R., & Gillman, M. W. (2005). Weight status in childhood as a predictor of becoming overweight or hypertensive in early adulthood. Obesity Research, 13(1), 163–169.
Burke, V., Beilin, L. J., Dunbar, D., & Kevan, M. (2004). Associations between blood pressure and overweight defined by new standards for body mass index in childhood. Preventive Medicine, 38(5), 558–564.
Britz, B., Siegfried, W., Ziegler, A., Lamertz, C., Herpertz-Dahlmann, B. M., Remschmidt, H., et al. (2000). Rates of psychiatric disorders in a clinical study group of adolescents with extreme obesity and in obese adolescents ascertained via a population based study. International Journal of Obesity and Related Metabolic Disorders, 24(12), 1707–1714.
Wang, F., Wild, T. C., Kipp, W., Kuhle, S., & Veugelers, P. J. (2009). The influence of childhood obesity on the development of self-esteem. Health Reports, 20(2), 21–27.
Martin, P., & Midgley, E. (2006). Immigration: Shaping and reshaping America. Population Bulletin, 61(4), 3–28.
Johnson, J. O., Kominski, R., Smith, K., & Tillman, P. (2005). Changes in the lives of US children, 1990–2000. Washington, DC: US Census Bureau. [cited 2009 June 15]. 71 pp. US Census Bureau Population Division Working Paper No. 78. Accessed October 6, 2009, from http://www.hwcli.com/documents/news/280.pdf
Federal Interagency Forum on Child and Family Statistics. (2008). America’s children: Key national indicators of wellbeing (23 pp). Washington, DC: US Government Printing Office. Accessed October 6, 2009, from http://www.childstats.gov/pdf/ac2008/ac_08.pdf
Singh, G. K., & Miller, B. A. (2004). Health, life expectancy, and mortality patterns among immigrant populations in the United States. Canadian Journal of Public Health, 95(3), 14–21.
Frisbie, W. P., Cho, Y., & Hummer, R. A. (2001). Immigration and the health of asian and pacific islander adults in the United States. American Journal of Epidemiology, 153(4), 372–380.
Sanchez-Vaznaugh, E. V., Kawachi, I., Subramanian, S. V., Sa′nchez, B. N., & Acevedo-Garcia, D. (2008). Differential effect of birthplace and length of residence on body mass index (BMI) by education, gender and race/ethnicity. Social Science & Medicine, 67(8), 1300–1310.
Kelaher, M., & Jessop, D. J. (2002). Differences in low-birthweight among documented and undocumented foreign-born and US born latinas. Social Science and Medicine, 55(12), 2171–2175.
Forna, F., Jamieson, D. J., Sanders, D., & Lindsay, M. K. (2003). Pregnancy outcomes in foreign-born and US-born women. International Journal of Gynecology and Obstetrics, 83(3), 257–265.
Marmot, M. G., Adelstein, A. M., & Bulusu, L. (1984). Lessons from the study of immigrant mortality. Lancet, 1(8392), 1455–1457.
Hummer, R. A., Rogers, R. G., Nam, C. B., & LeClere, F. B. (1999). Race/ethnicity, nativity and US adult mortality. Social Science Quarterly, 80(1), 136–153.
Jasso, G., Douglas, M., Rosenzweig, M., & Smith, J. P. (2005). Immigration, health, and New York city: Early results based on the US new immigrant cohort of 2003. FRBNY Economic Policy Review, 11, 127–151.
Perez, C. E. (2002). Health status and health behavior among immigrants. Health Reports, 13(Suppl), 1–12.
Singh, G. K., & Siahpush, M. (2001). All-cause and cause-specific mortality of immigrants and native-born in the United States. American Journal of Public Health, 91(3), 392–399.
Goel, M. S., McCarthy, E. P., Phillips, R. S., & Wee, C. C. (2004). Obesity among US immigrant subgroups by duration of residence. JAMA, 292(23), 2860–2867.
Singh, G. K., & Hiatt, R. A. (2006). Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979–2003. International Journal of Epidemiology, 35(4), 903–919.
Kaplan, M. S., Huguet, N., Newsom, J. T., & McFarland, B. H. (2004). The association between length of residence and obesity among Hispanic immigrants. American Journal of Preventive Medicine, 27(4), 323–326.
Kaushal, N. (2009). Adversities of acculturation? Prevalence of obesity among immigrants. Health Economics, 18(3), 291–303.
Roshania, R., Narayan, K. M. V., & Oza-Frank, R. (2008). Age at arrival and risk of obesity among US immigrants. Obesity, 16(12), 2669–2675.
Center for Disease Control and Prevention. (2009). Overweight and obesity [Internet]. Atlanta, GA: Centers for Disease Control and Prevention. Accessed October 6, 2009, from http://www.cdc.gov/nccdphp/dnpa/obesity/index.htm
Nord, C., Edwards, B., Hilpert, R., Branden, L., Andreassen, C., & Elmore A. (2004). Early childhood longitudinal study, birth cohort (ECLS-B): User’s manual for the ECLS-B nine-month restricted-use data file and electronic code book (NCES 2004-092). Washington, DC: US Department of Education, Institute of Education Sciences, National Center for Education Statistics.
Snow, K., Thalji, L., Derecho, A., Wheeless, S., Lennon, J., Kinsey, S., Rogers, J., & Raspa, M. (2007). Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), Preschool Year Data File User’s Manual, 2005–2006 (NCES 2008-024). Washington, DC: US Department of Education, Institute of Education Sciences, National Center for Education Statistics.
Radloff, L. S. (1977). The CES-D: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Bethel, J., Green, J. L., Nord, C., & Kalton, G. (2005). Early childhood longitudinal study, birth cohort (ECLS-B), sampling. Volume 2 of the ECLS-B methodology report for the 9-month data collection, 2001–2002 (NCES 2005-147). Washington, DC: US Department of Education, Institute of Education Sciences, National Center for Education Statistics.
Cuzick, J. (1985). A Wilcoxon-type test for trend. Statistics in Medicine, 14(4), 87–89.
Sande, I. G. (1982). Imputation in surveys: Coping with reality. The American Statistician, 36(3), 145–152.
Antecol, H., & Bedard, K. (2006). Unhealthy assimilation: Why do immigrants converge to American health status levels? Demography, 43(2), 337–360.
Lauderdale, D. S., & Rathouz, P. J. (2000). Body mass index in a US national sample of Asian Americans: Effects of nativity, years since immigration and socioeconomic status. International Journal of Obesity and Related Metabolic Disorders, 24(9), 1188–1194.
Sundquist, J., & Winkleby, M. (2000). Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. International Journal of Epidemiology, 29(3), 470–477.
Gordon-Larsena, P., Harrisa, K. M., Wardb, D. S., & Popkin, B. M. (2003). National longitudinal study of adolescent health. acculturation and overweight-related behaviors among hispanic immigrants to the US: The national longitudinal study of adolescent health. Social Science and Medicine, 57(11), 2023–2034.
Fortuny, K., Capps, R., Simms, M., & Chaudry, A. (2009). Children of immigrants: National and state characteristics. The urban institute. 9. Accessed December 21, 2009, from http://www.urban.org/UploadedPDF/411939_childrenofimmigrants.pdf
Hill, A. J. (2002). Developmental issues in attitudes to food and diet. Proceedings of the Nutrition Society, 61(2), 259–266.
Wieting, J. M. (2008). Cause and effect in childhood obesity: Solutions for a national epidemic. The Journal of the American Osteopathic Association, 108(10), 545–552.
Cohen, D. A., McKenzie, T. L., Sehgal, A., Williamson, S., Golineli, D., & Lurie, N. (2007). Contribution of public parks to physical activity. American Journal of Public Health, 97(3), 509–514.
Gordon-Larsen, P., Nelson, M. C., Page, P., & Popkin, B. M. (2006). Inequalities in the built environment underlies key health disparities in physical activity and obesity. Pediatrics, 117(2), 417–424.
Weir, L. A., Etelson, D., & Brand, D. A. (2006). Parents’ perceptions of neighborhood safety and children’s physical activity. Preventive Medicine, 43(3), 212–217.
Carver, A., Timperio, A., & Crawford, D. (2008). Playing it safe: The influence of neighbourhood safety on children’s physical activity. A review. Health Place, 14(2):217–227.
Etelson, D., Brand, D. A., Patrick, P. A., & Shirali, A. (2003). Childhood obesity: Do parents recognize this health risk? Obesity Research, 11(11), 1362–1368.
Jain, A., Sherman, S. N., Chamberlin, L. A., Carter, Y., Powers, S. W., & Whitaker, R. C. (2001). Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics, 107(5), 1138–1146.
Rich, S. S., DiMarco, N. M., Huettig, C., Essery, E. V., Andersson, E., & Sanborn, C. F. (2005). Perceptions of health status and play activities in parents of overweight hispanic toddlers and preschoolers. Family & community health, 28(2), 130–141.
Brewis, A. (2003). Biocultural aspects of obesity in young Mexican schoolchildren. American Journal of Human Biology, 15(3), 446–460.
Lindsay, A. C., Sussner, K. M., Greaney, M. L., & Peterson, K. E. (2009). Influence of social context on eating, physical activity, and sedentary behaviors of Latina mothers and their preschool-age children. Health Education & Behavior, 36(1), 81–96.
Lohman, B. J., Stewart, S., Gundersen, C., Garasky, S., & Eisenmann, J. C. (2009). Adolescent overweight and obesity: Links to food insecurity and individual, maternal, and family stressors. Journal of Adolescent Health, 45(3), 230–237.
Oken, E., & Gillman, M. W. (2003). Fetal origins of obesity. Obesity Research, 11(4), 496–506.
Lawlor, D. A., & Chaturvedi, N. (2006). Treatment and prevention of obesity—are there critical periods for intervention? International Journal of Epidemiology, 35(1), 3–9.
Ben-Shlomo, Y., & Kuh, D. (2002). A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology, 31(2), 285–293.
Langenberg, C., Hardy, R., Kuh, D., Brunner, E., & Wadsworth, M. (2003). Central and total obesity in middle aged men and women in relation to lifetime socioeconomic status: Evidence from a national birth cohort. Journal of Epidemiology and Community Health, 57(10), 816–822.
Whitaker, R. C. (2004). Predicting preschooler obesity at birth: The role of maternal obesity in early pregnancy. Pediatrics, 114(1), e29–e36.
Salsberry, P. J., & Reagan, P. B. (2005). Dynamics of early childhood overweight. Pediatrics, 116(6), 1329–1338.
Li, C., Goran, M. I., Kaur, H., Nollen, N., & Ahluwalia, J. S. (2007). Developmental trajectories of overweight during childhood: Role of early life factors. Obesity, 15(3), 760–771.
Stettler, N., Zemel, B. S., Kumanyika, S., & Stallings, V. A. (2002). Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics, 109(2), 194–199.
Toschke, A. M., Grote, V., Koletzko, B., & von Kries, R. (2004). Identifying children at high risk for overweight at school entry by weight gain during the first 2 years. Archives of Pediatrics and Adolescent Medicine, 158(5), 449–452.
Singhal, A., & Lanigan, J. (2007). Breastfeeding, early growth and later obesity. Obes Rev, 8(sup1):51–54.
Larsen, L. J. (2004). The foreign-born population in the United States: 2003 (9 pp). Washington, DC: US Census Bureau. Current Population Reports: P20–P551.
Acknowledgments
This study was supported by grant R40 MC 08951 from the Maternal and Child Health Bureau (Title V, Social Security Act), Health Resources and Services Administration, Department of Health and Human Services.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, N., Strobino, D., Ahmed, S. et al. Is There a Healthy Foreign Born Effect for Childhood Obesity in the United States?. Matern Child Health J 15, 310–323 (2011). https://doi.org/10.1007/s10995-010-0588-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-010-0588-5