Abstract
Objectives We examined the association between religious involvement and health risk behaviors such as smoking, drinking, marijuana use, and having multiple sex partners among a multiethnic sample of pregnant and postpartum women. Methods Using data from the National Survey of Family Growth, we estimated multivariate logistic regression models to determine the association between various aspects of religious involvement (e.g., attendance, salience, and denomination) and certain behaviors known to be risky for pregnant women and their offspring. Results Frequent (more than once a week) and regular (once a week) attenders at religious services had 80% and 60% (respectively) lower odds of drinking alcohol compared to women who attended less than once a week. Similar patterns surfaced with regard to smoking tobacco with the odds of smoking roughly 85% lower (OR = 0.146, P < 0.001) among frequent attenders, and nearly 65% lower among regular attenders (OR = 0.369, P < 0.001). For smoking marijuana, religious attendance again emerges as a strong predictor. The odds of marijuana smoking are nearly 75% lower for women who attend services frequently (OR = 0.260, P < 0.05) and more than 65% lower for those who attend regularly (OR = 0.343, P < 0.01), as compared with their counterparts who attend services less often. Conclusions Religious attendance emerged as an important correlate of less-risky health behaviors among this nationwide sample of pregnant and postpartum women. Future research should include an examination of the links between religious involvement and other important lifestyle factors that may influence maternal and child health.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the contemporary United States, infants who are born with low birth weight are a major public health concern [1], and this problem has actually increased in recent years [2]. Babies born too small often spend several weeks or months in neonatal intensive care units, at an average cost of more than $1,000 per day. Consequently, low birth weight is responsible for 10% of all health care costs for children [3]. Moreover, low birth weight is also associated with subsequent morbidity and mortality [4, 5], and also exacts an emotional toll on parental well-being and marital quality [6]. For all of these reasons, the Healthy People 2010 campaign has established a goal of reducing the incidence of low birth weight infants (<2500 g) to 5% and very low birth weight infants (<1500 g) to <1% of all infants born in the US [1].
Among other factors, deleterious maternal practices can prevent the achievement of optimal fetal growth and development [7]. Among the most important and well-researched of these modifiable pregnancy health behaviors is smoking [8–11]. Other maternal behaviors during pregnancy, such as alcohol and drug use, have also been shown to adversely affect gestational length and birth weight [12–15]. Further, infections of the reproductive tract, which are often sexually transmitted, can lead to premature rupture of membranes and/or premature labor, resulting in low birth weight infants and increasing the risk of potentially life-threatening or debilitating infections in newborns [16, 17].
In light of such findings, researchers have devoted considerable attention to social factors that affect the risk of low birth weight and that can influence the health behaviors of pregnant women. For example, a number of studies have explored the influence of socioeconomic status (e.g., education, income, poverty level) [18, 19], race/ethnicity and nativity [20–22], and maternal age [23]. To date, however, despite a burgeoning literature on religion, spirituality, and health [24–26], few researchers have investigated the possible role of religious factors in maternal and child health [27, 28]. Our study addresses this gap in the literature by: (a) briefly reviewing relevant theory and research linking multiple dimensions of religious involvement with health behaviors; and (b) testing relevant hypotheses using data on pregnant and postpartum women from a major nationwide probability sample, the National Survey of Family Growth (NSFG).
Theoretical and Empirical Background
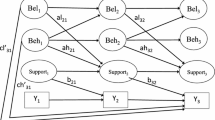
How and why might religious involvement be expected to shape the health risk behaviors of pregnant and postpartum women? Briefly, for several decades, social and behavioral scientists have recognized that religion is a multidimensional phenomenon [29, 30]. At a minimum, investigators routinely distinguish between organizational aspects of religiousness (e.g., attendance at services, participation in other congregational activities), non-organizational or subjective facets (e.g., frequency of devotional activities, salience of religious or spiritual identities), and affiliation (e.g., denominational differences based on theological, historical, or institutional specificity).
Organizational religiousness may be associated with health risk behaviors for several reasons. Prior theory and research indicate that engagement in a religious community, including regular participation in collective worship activities, may shape behavior via a number of mechanisms [31–33]. For example, organizational religious involvement may: (a) promote the internalization of religious norms concerning morality and personal contact, including teachings about the benefits of devotion, beliefs about divine punishment, and other potentially relevant doctrines; (b) provide positive role models and social reinforcement for adherence to behavioral standards; (c) foster coreligionist social networks and afford opportunities for wholesome social engagement; and (d) allow for informal (or even formal) sanctions—or the threat of sanctions—against persons who deviate from group standards. Many congregations also provide formal programs and other supports and resources that can discourage unwholesome lifestyle choices and promote positive health behaviors.
Non-organizational aspects of religiousness may also be linked with health risk behaviors. The frequency of devotional activities (e.g., prayer, scriptural study) or religious salience may indicate a high level of commitment to religious doctrines and teachings, many of which discourage practices that can have negative health consequences (e.g., heavy drinking, risky sexual behavior) [34]. This may also involve the establishment of a close personal relationship with a (perceived) divine other (i.e., God), which can afford psychological security and comfort, as well as moral guidance [35, 36]. Individuals for whom religion is particularly salient are also prone to internalize religious norms and moral standards, making violations of these norms unlikely (and guilt-inducing) [32].
Specific religious subcultures may also shape and direct behaviors and lifestyle choices, including those germane to health. In particular, conservative (i.e., fundamentalist and evangelical) Protestant and sectarian groups typically have more restrictive moral codes than most other religious groups. These subcultures tend to discourage consumption of alcohol or illicit drugs, as well as having multiple sexual partners [31, 37, 38]. Although Catholics differ sharply from conservative Protestants and sectarians in attitudes toward alcohol, the Catholic Church traditionally emphasizes family solidarity and pronatalism, officially opposing all forms of birth control except for “natural” family planning methods, although lay contraceptive practices in the US are often at variance with the church position [39].
Although we are aware of no studies that explore religious influences on health risk behaviors among pregnant and postpartum women, a growing body of research documents religious variations in a number of relevant behaviors within the general population, and in samples of other specific subgroups [40, 41]. For example, a number of studies reveal inverse associations between religious practice (especially organizational participation), conservative affiliation, and alcohol consumption [31, 34, 42, 43]. Several studies also reveal inverse links between organizational religious involvement and adults’ smoking [44, 45]. Research on mostly adolescent and young adult samples has consistently shown inverse relationships between multiple dimensions of religiousness, as well as conservative denominational ties, and the use of illicit drugs, such as marijuana [33, 46]. Research linking religious factors and sexual behavior yields more complex findings, but even here there are inverse associations between organizational and non-organizational religiousness and the number of sexual partners, sexual infidelity among married persons, and other outcomes that are germane to this study [37, 47]. In addition, a growing literature now links religiousness—and chiefly organizational religious involvement, but occasionally religious salience as well—with a broad array of indicators of healthy lifestyle, including regular medical checkups and use of preventive health care, sleep quality, and regular exercise [40, 41, 48].
The foregoing review of relevant theory and research suggests several broad hypotheses that will guide the remainder of this study. First, we expect that pregnant and postpartum women who attend religious services at least once a week will be less likely to engage in potentially risky health behaviors—such as using alcohol, tobacco, or illicit drugs, having multiple sexual partners—than their counterparts who attend services less often, or not at all. Second, we anticipate that those women for whom religion has low or moderate salience, and those who report no religious preference at all, will be more likely to engage in these potentially risky health practices than women who report high levels of religious salience. Finally, we expect that conservative Protestant, and perhaps Catholic, women will be less prone to engage in problematic health behaviors than others.
Methods
Data
Data for this study are drawn from the NSFG, cycle 6, which was conducted by the National Center for Health Statistics. The NSFG was conducted in five previous cycles—1973, 1976, 1982, 1988, and 1995; the sixth cycle was conducted in 2002–03. Surveys were administered to a nationwide sample of women ages 18–44 in the civilian, non-institutionalized population of the United States. Data collection took place via personal (i.e., face-to-face) interviews conducted in the homes of respondents by trained female interviewers from the Survey Research Center at the University of Michigan. More than 7,000 female respondents completed the cycle 6 survey, which included oversamples of African-Americans and Hispanics. Of the women who self-identified as Hispanic, Black, or non-Hispanic White, 1,035 respondents indicated that they were pregnant at the time of the interview, or had been pregnant at some point during the 12-month period preceding the interview. These women composed the effective sample for our study. After adjustments for missing data on dependent variables, our analytic sample sizes range from 1,026 to 1,031 respondents.
Measures
Dependent Variables
Our study focuses on several specific health behaviors that have been associated with low birth weight or compromised maternal or infant health: alcohol consumption; tobacco use; marijuana use; having multiple sexual partners; and tests and/or treatment for sexually transmitted infections (STI). Respondents were asked: “During the past 12 months how often have you… (a) had beer, wine, hard liquor, or other alcoholic beverages? (b) smoked cigarettes? (c) smoked marijuana?” For each item, the original response categories were 1 = never, 2 = once or twice during the year, 3 = several times during the year, 4 = about once a month, 5 = about once a week, or 6 = about once a day. To create our dependent variables we recoded these responses into dummy variables. For alcohol consumption, we distinguished between women who rarely or never drank (categories 1–2, recoded as 0) vs. those who drank alcohol at least several times during the previous year (categories 3–6, recoded as 1). To create our measures of cigarette smoking and marijuana use, we distinguished between women who abstained (category 1, recoded as 0) vs. those who smoked cigarettes or marijuana at all (categories 2–6, recoded as 1). Respondents were also asked: “Thinking about the past 12 months, how many male sex partners have you had?” Answers were recoded to create a dummy variable, in which 0 denotes only one partner, and 1 denotes multiple partners. Finally, respondents were asked two questions concerning STI: “In the past 12 months, have you… (a) been tested by a doctor or other medical care provider for a sexually transmitted disease like gonorrhea, herpes, or syphilis? (b) been treated or received medication from a doctor or other medical care provider for a sexually transmitted disease like gonorrhea, herpes, or syphilis?” Answers to these items were recoded to create a single variable with ordered categories, where 1 denotes women who did not report an STI test, 2 denotes women who were tested but received no further treatment, and 3 denotes women who did receive medical care for an STI.
Independent Variables
Three distinct dimensions of religious involvement were considered in this study. First, respondents were asked their current religious or denominational affiliation. Following the coding scheme proposed by Steensland et al. [49], answers were recoded into a series of dummy variables: No religion (1=), Catholic (1=), Mainline Protestant (e.g., Episcopal, Methodist, Presbyterian; 1=), and non-Christian religion (e.g., Jewish, Muslim; 1=). In our analyses, each of these categories is compared to a reference category, consisting of members of conservative (i.e., fundamentalist or evangelical) Protestant groups (e.g., Southern Baptist, Assemblies of God, Pentecostal or Holiness, non-denominational conservative church). Second, respondents were asked: “About how often do you attend religious services?” Responses were recoded into two dummy variables, identifying women who attend more than once a week (1=) and those who attend once a week (1=); in our analyses, these categories of women are compared with respondents who reported attending less than once a week (0=). Finally, respondents were asked: “How important is religion in your daily life? Would you say it is very important, somewhat important, or not important?” Women who reported having no religious affiliation were not asked this item on religious salience. Responses to the salience item were recoded into dummy variables denoting low religious salience (1=) and moderate salience (1=); in our analyses, these women are compared with their counterparts who report a high degree of religious salience (0=). In addition, these analyses include another dummy variable to identify those women who reported having no religious affiliation, as indicated above (1=).
Control Variables
The multivariate analyses also control for a number of variables that are associated with religious involvement and/or health behaviors, and therefore might confound the relationships that are of central interest in this study. Control variables include the following: age (measured in years); race/ethnicity (recoded into dummy variables: 1 = Hispanic, interview conducted in Spanish; 1 = Hispanic, interview conducted in English; 1 = African-American; vs. 0 = non-Hispanic White); education (recoded into dummy variables: 1 = graduate degree; 1 = bachelor’s degree; 1 = associate’s degree or technical training; 1 = less than high school; vs. 0 = high school degree); poverty status (1 = living at or below the poverty line; 0 = living above the poverty line); relationship status (recoded into dummy variables: 1 = cohabiting; 1 = formerly married, i.e., divorced, separated, or widowed, and not cohabiting; 1 = never married and not cohabiting; vs. 0 = married); and urban residence (1 = living in metropolitan area, 0 = living in suburban or rural area).
Finally, in preliminary analyses we used information on the respondent’s pregnancy and pregnancy resolution to create a series of dummy variables, identifying women who had stopped being pregnant 9–12 months before the interview, 6–8 months before the interview, 3–5 months before the interview, or <3 months prior to the interview, as well as those who were pregnant at the time of the interview, and in their first trimester, second trimester, and third trimester of pregnancy, respectively. Our preliminary analyses (results not shown) revealed that only one of these dummy variables was significantly associated with self-reported health behaviors: the one identifying women who were currently pregnant, and in their third trimester at the interview. Therefore, we retain this dummy variable in the final models, comparing respondents who are in their third trimester of pregnancy (1=) vs. all other women who are pregnant or have been pregnant during the preceding year (0=).
Results
Descriptive Statistics
We begin by presenting descriptive statistics on all variables used in these analyses in Table 1. Of the all respondents—who were either pregnant at the time of the interview or at some point during the preceding year—39% answered that they drank alcohol more than several times a year. 25% and 14% of the sample responded positively for having used tobacco or marijuana during the past 12 months, respectively. To the question of having multiple sexual partners in the preceding year, 17% of respondents answered that they had more than one partner. Regarding STI tests and treatment, slightly more than half of the sample had no STI test (52%), while 42% of the sample was tested for an STI but did not have STI treatment, and 7% of the sample was treated for an STI.
The majority of respondents (66%) reported attending religious services less than once a week, slightly less than a quarter of respondents (24%) attended services once a week and 10% reported a higher level of church attendance (several times a week). Additionally, the respondents demonstrated a high religious salience level: more than half (51%) answered religion is very important; 30% answered religion is somewhat important; and only 4% of the sample responded that religion is not important in their daily lives. With regard to religious denominational affiliation, around 14% of the respondents reported that they were not affiliated with any religion, while 31% reported that they were Catholic. Conservative Protestants and Mainline Protestants represented 30% and 20% of the sample, respectively. Slightly <5% of the respondents reported their religion as non-Christian.
The mean age of the respondents was approximately 28 years old (27.7) and the age range of pregnant women was between 18 and 44. More than half of the respondents (57%) were married and 14% were cohabiting. 21% of the respondents were never married at the time of the interview. The distribution of race/ethnicity was 21% African-Americans, 27% Hispanics in which 12% spoke Spanish and 15% spoke English as a primary language during the interview, and 52% were non-Hispanic Whites. Regarding the level of education, 32% of the respondents reported a high school degree, approximately 16% of the sample held a college degree, and slightly more than 6% of the respondents had a graduate degree. Those whose income was below poverty level represented nearly 30% of the sample and almost half of the sample (48%) lived in a metropolitan area. Finally, those who were pregnant in the third trimester represented 6% of the sample.
Multivariate Results
Next we turn to the multivariate models, selected findings from which are displayed in Table 2. Briefly, for each outcome we estimate five models: (a) an initial model that includes measures of religious attendance and sociodemographic covariates; (b) a second model in which attendance is replaced with religious salience; (c) a third model in which salience is replaced with a series of dummy variables tapping denominational affiliation; (d) a fourth model in which salience and attendance are included together; and (e) a fifth model in which denomination and attendance are considered together. This sequence of models allows us to gauge the relative importance of the various religious predictors; we do not display a full model with all religious predictors, because preliminary analyses revealed the potential for unstable estimates due to multicollinearity among religious variables. All models are estimated using dichotomous logistic regression techniques except for the models predicting testing and treatment for STI, which are estimated via ordered logistic regression.
To conserve space, our discussion focuses solely on the estimated net effects of religious variables, which are of central theoretical and substantive interest in this study.
Several notable patterns emerge from these results. First, we find strong and consistent protective effects of regular (i.e., weekly) and frequent (i.e., more than weekly) attendance at religious services on several of the outcomes examined here. For example, in model 1, the odds of drinking alcohol are more than 80% lower (OR = 0.190, P < 0.001) for frequent attenders, and more than 60% lower (OR = 0.374, P < 0.001) for regular attenders, as compared with pregnant or postpartum women who report attending religious services less than once per week. In models 4 and 5 (i.e., when salience and denomination are added to the model containing religious attendance), the magnitude of these strong attendance effects is only slightly reduced. Similar patterns surface with regard to smoking tobacco; the odds of smoking are roughly 82% lower (OR = 0.180, P < 0.001) among frequent attenders, and roughly 60% lower among regular attenders (OR = 0.408, P < 0.001). In models of smoking marijuana, religious attendance again emerges as a strong predictor. The odds of marijuana smoking are nearly 80% lower for women who attend services frequently (OR = 0.210, P < 0.01) and approximately 75% lower for those who attend regularly (OR = 0.254, P < 0.001), as compared with their counterparts who attend services less often. The estimated net effects of religious attendance on the other outcomes are less striking. Weekly attenders, but not frequent attenders, are somewhat less prone to report multiple sexual partners (OR = 0.597, P < 0.05), while frequent attendance, but not regular attendance, is inversely associated with testing and treatment for STI (OR = 0.594, P < 0.05). For these outcomes, too, attendance effects persist even when other dimensions of religious involvement (i.e., salience and denomination) are included in the models.
Second, the links between religious salience and health risk behaviors are weak and inconsistent, particularly once the confounding effects of religious attendance are taken into account. To be sure, pregnant and postpartum women who report low and/or moderate levels of religious salience are more prone to drink alcohol (OR = 2.844, P < 0.01 and OR = 2.008, P < 0.001, respectively) and to smoke marijuana (OR = 2.732, P < 0.05 and OR = 2.034, P < 0.01, respectively) when salience is the only religious variable included in the model (i.e., model 2). However, these associations disappear in the full models. Respondents who report no religion—and therefore were not asked the survey item on salience—are consistently more prone to drink alcohol, and to smoke tobacco and marijuana; this pattern persists for alcohol and marijuana even when the potentially confounding effects of regular religious attendance are held constant. None of the dummy variables tapping religious salience surface as significant predictors of multiple sexual partners or STI testing and/or treatment.
Third, we find only meager and inconsistent evidence of religious subgroup differences in these health risk behaviors, particularly when religious attendance variables are also included. As we noted above, even with other religious controls, women with no religious preference or affiliation are significantly more likely to report drinking alcohol and smoking marijuana, compared to women from conservative (i.e., fundamentalist or evangelical) Protestant backgrounds who constitute the reference category in the denominational models. For the other outcomes, however, women with no religion do not differ significantly in any model. Although Catholic women appear more likely to drink alcohol in model 3 (OR = 1.539, P < 0.05), this pattern is diminished by controls for attendance in model 5. When attendance differences are held constant, Catholic women are somewhat less likely than their evangelical Protestant counterparts to smoke tobacco (OR = 0.618, P < 0.10). However, neither Catholic nor mainline Protestant women are distinctive with respect to any of the other health risk behaviors examined in this study.
Interestingly, the small cluster of pregnant and postpartum women from non-Christian faiths appear to be less prone to smoke tobacco, particularly when attendance differences are controlled (OR = 0.404, P < 0.05), but they are dramatically more likely to report having multiple sexual partners (OR = 5.607, P < 0.001), compared to conservative Protestant women with similar patterns of religious attendance. Unfortunately, additional details about this small and heterogeneous cluster of women are not available in the NSFG dataset.
Finally, in ancillary analyses (not shown, but available upon request), we investigated whether the protective effects of religious attendance—by far the strongest patterns observed here—vary according to other characteristics of these women. Specific potential moderators included race/ethnicity, age, socioeconomic status, and marital or relationship status. However, no compelling evidence of interactive or contingent effects was detected, suggesting that the associations between religious attendance and health risk behaviors in pregnant and postpartum women are robust across major population subgroups.
Discussion
These results clearly reveal that the self-reported frequency of attendance at religious services is an important correlate of several important health behaviors in this nationwide sample of pregnant and postpartum women. These patterns are especially pronounced with regard to drinking, smoking, marijuana use, and number of sexual partners, but are negligible with regard to use of prenatal care. The latter null finding is somewhat surprising, in light of other studies linking religious involvement—and specifically, frequency of attendance—with use of preventive health services (e.g., flu shot, mammograms, cholesterol screening, etc.) in the general population, and in samples of older adults [34, 50]. Moreover, ancillary analyses (not shown, but available upon request) turned up no clear or consistent evidence that the associations between religious attendance and the outcomes of interest vary according to age, race/ethnicity, SES, pregnancy vs. postpartum status, or relationship status. Thus, it appears that these patterns are robust across major subgroups of the population, as represented in the NSFG data.
To be sure, researchers have raised questions about the accuracy of self-reports of religious attendance, arguing that many individuals exaggerate the frequency with which they go to church or synagogue. According to these critics, survey items on attendance are likely to elicit socially desirable responses, which may also affect their associations with outcomes that are measured via self-reports [51, 52]. However, recent studies cast doubt on the role of such response biases in accounting for observed effects of religious involvement on sensitive personal behavior [38, 53]. Our findings add to the mounting evidence that self-reported attendance is a stronger predictor of behaviors than other survey items tapping religious involvement, including a variable tapping overall religious salience.
Of course, since the NSFG data are cross-sectional, it is impossible to establish the causal direction of the associations between attendance and personal behavior conclusively. Thus, these patterns could also reflect the influence of selectivity or reverse causality. For example, drinking or other negative or counter-normative behavior could lead individuals to abandon organized religion, or to reduce the frequency with which they attend services or participate in congregational activities. It is also conceivable that both regular attendance and avoidance of unhealthy behaviors could stem from unmeasured dispositional factors, such as risk aversion, conscientiousness, habit, or conformist tendencies. Nevertheless, although these possibilities warrant further investigation, our findings demonstrate that regular religious attendance is an important correlate of key health behaviors among pregnant or postpartum women.
Other aspects of religious involvement bear little relationship to these outcomes. Although our results confirm the tendency for members of conservative Protestant denominations to avoid alcohol use [31] and we also find that members of non-Christian faiths report more sexual partners, overall we find little evidence of denominational subcultures with respect to women’s health behaviors. The denominational patterns observed in some models were eliminated once individual variations in attendance were controlled. These findings are broadly consistent with arguments in the sociology of religion literature that brand loyalties, and especially intra-Protestant differences—have become less relevant for personal behavior, and indeed for much of American life, than variations in religious commitment or secularity [54].
Self-reported religious salience (i.e., how important is religion in your life?) has little direct bearing on the women’s health behaviors examined here. Although this item is frequently included on large-scale surveys, surprisingly few studies have found robust associations between these responses and other outcomes of interest. Given the discussion above, it is not clear what this generic salience item taps, over and above attendance at services. As is the case in other databases, responses to this item in the NSFG are significantly skewed in a positive direction. In lieu of an omnibus salience measure, researchers might profitably use items on domain-specific salience, i.e., asking about the relative importance of each respondent’s faith tradition and personal spiritual beliefs (if any) in shaping decisions in specific domains of activity (e.g., leisure pursuits, medical decisions, voting) relative to the influence of other possible influences (e.g., close friends, coworkers) [34].
Our understanding of the role of religion in shaping health behaviors among pregnant and postpartum women could be extended by several lines of investigation in the future. First, it would be useful to examine the links between religious involvement and other important lifestyle factors that may influence maternal and child health, including seat belt use (and car seat use for infants), sleep quality and quantity, exercise, dietary practices, and others. Although our analyses of drinking behavior have focused only on predicting which pregnant and postpartum women consumed alcohol more than once or twice during the preceding year, future work should also examine relationships between religious variables and more fine-grained measures of the frequency and quantity of alcohol consumption within this potentially vulnerable population. Second, religious involvement may also be associated with pronatalist values, family-centered attitudes, frequency of interaction with—and levels of support from—parents and in-laws, and pregnancy wantedness, any of which might mediate the association between religious attendance and health risk behaviors observed in this study. Third, although the latest cycle of the NSFG project contains only information on the female respondents’ religious affiliation, attendance, and salience, previous cycles also gathered parallel data on male partners. Do more religious males (or those from particular faith backgrounds) exert an influence on the health risk behaviors of their pregnant or postpartum partners? Are patterns of religious (dis)similarity among men and women associated with specific behavioral profiles? Given recent findings linking such (dis)similarity with various relationship characteristics (e.g., relationship conflict), more information is needed on this front [55].
Finally, work in the conceptualization and measurement of health-relevant dimensions of religiousness and spirituality has advanced well beyond the kinds of generic religious measures that are available in the NSFG. Recent developments have emphasized the value of more proximal, functional measures of these domains. Specific examples include congregational social and spiritual support processes [34, 56], religious coping practices [57], specific beliefs and meaning systems [58], formal support processes and programs, and informal support processes [56, 58]. Future research incorporating information on these factors will cast fresh light on the links between religion and maternal and child health.
References
U.S. Department of Health and Human Services. Healthy people 2010 (2nd ed.). Washington, DC: U.S. Government Printing Office; 2000 November. Report No.: DHHS Publication No. 017-01-00547-9.
Mattison, D. R., Damus, K., Fiore, E., Petrini, J., & Alter, C. (2001). Preterm delivery: A public health perspective. Paediatric and Perinatal Epidemiology, 15(Suppl. 2), 7–16. doi:10.1046/j.1365-3016.2001.00004.x.
March of Dimes. National perinatal statistics. 2008 March 22, 2008 [cited 2008 March 22, 2008]; Available from: http://www.marchofdimes.com/aboutus/680_2203.asp.
Collier, S. A., & Hogue, C. J. R. (2007). Modifiable risk factors for low birth weight and their effect on cerebral palsy and mental retardation. Maternal and Child Health Journal, 11, 65–71. doi:10.1007/s10995-006-0085-z.
Martin, J. A., Hamilton, B. E., Ventura, S. J., Menacker, F., & Park, M. M. (2002). Births: Final data for 2000. Hyattsville, Maryland: National Center for Health Statistics.
Swaminathan, S., Alexander, G. R., & Boulet, S. (2006). Delivering a very low birth weight infant and the subsequent risk of divorce or separation. Maternal and Child Health Journal, 10, 473–479. doi:10.1007/s10995-006-0146-3.
Reedy, N. J. (1997). Substance abuse. In H. Varney (Ed.), Varney’s midwifery (3rd ed., pp. 175–179). Sudbury, Massachusetts: Jones and Bartlett.
Ahern, J., Pickett, K. E., Selvin, S., & Abrams, B. (2003). Preterm birth among African American and white women: A multilevel analysis of socioeconomic characteristics and cigarette smoking. Journal of Epidemiology and Community Health, 57, 606–611. doi:10.1136/jech.57.8.606.
Sprauve, M. E., Lindsay, M. K., Drews-Botsch, C. D., & Graves, W. (1999). Racial patterns in the effects of tobacco use on fetal growth. American Journal of Obstetrics and Gynecology, 181, s22–s27. doi:10.1016/S0002-9378(99)70468-0.
Strobino, D., Nicholson, W., Misra, D., Hawkins, M., & Cassady, C. (1999). Issues in pregnancy care. In H. Grason, J. Hutchins, & G. Silver (Eds.), Charting a course for the future of women’s and perinatal health: Volume II-Reviews of key issues (pp. 103–136). Baltimore: Women’s and Children’s Health Policy Center, Johns Hopkins School of Public Health.
Bailey, B. A., & Byrom, A. R. (2007). Factors predicting birth weight in a low-risk sample: The role of modifiable pregnancy health behaviors. Maternal and Child Health Journal, 11, 173–179. doi:10.1007/s10995-006-0150-7.
Dew, P. C., Gullroy, V. J., Okah, F. A., Cal, J., & Hoff, G. L. (2007). The effect of health compromising behaviors on preterm births. Maternal and Child Health Journal, 11, 227–233. doi:10.1007/s10995-006-0164-1.
Peacock, J. L., Bland, J. M., & Anderson, H. R. (1995). Preterm delivery: Effects of socioeconomic factors, psychological stress, smoking, alcohol, and caffeine. British Medical Journal, 311, 531–535.
Sampson, P. D., Bookstein, F. L., Barr, H. M., & Streissguth, A. P. (1994). Prenatal alcohol exposure, birthweight, and measures of child size from birth to age 14 years. American Journal of Public Health, 84, 1421–1428.
Sprauve, M. E., Lindsay, M. K., Herbert, S., & Graves, W. (1997). Adverse perinatal outcome in parturients who use crack cocaine. Obstetrics and Gynecology, 89, 674–678. doi:10.1016/S0029-7844(97)00078-1.
Goldenberg, R. L., Andrews, W. W., Yuan, A. C., MacKay, H. T., & St. Louis, M. E. (1997). Sexually transmitted diseases and adverse outcomes of pregnancy. Clinics in Perinatology, 24, 23–41.
Winter, E. J. S. (2004). Sexual wellness and illness. In M. C. Condon (Ed.), Women’s health: Body, mind, spirit (pp. 445–462). Upper Saddle River: Prentice Hall.
Kramer, M. S., Goulet, L., Lydon, J., Seguin, L., McNamara, H., Dassa, C., et al. (2001). Socio-economic disparities in preterm birth: Causal pathways and mechanisms. Paediatric and Perinatal Epidemiology, 15 (Suppl. 2), 104–123. doi:10.1046/j.1365-3016.2001.00012.x.
Savitz, D. A., Kaufman, J. S., Dole, N., Siega-Riz, A. M., Thorp, J. M., & Kaczor, D. T. (2004). Poverty, education, race, and pregnancy outcome. Ethnicity & Disease, 14, 322–329.
Reichman, N. E., Hamilton, E. R., Hummer, R. A., & Padilla, Y. C. (2008). Racial and ethnic disparities in low birthweight among urban unmarried mothers. Maternal and Child Health Journal, 12, 204–215. doi:10.1007/s10995-007-0240-1.
Geronimus, A. (1996). Black/White differences in the relationship of maternal age to birthweight: A population-based test of the weathering hypothesis. Social Science and Medicine, 42, 589–597. doi:10.1016/0277-9536(95)00159-X.
Lu, M. C., & Halfon, N. (2003). Racial and ethnic disparities in birth outcomes: A life-course perspective. Maternal and Child Health Journal, 7, 13–30. doi:10.1023/A:1022537516969.
Khoshnood, B., Wall, S., & Lee, K. S. (2005). Risk of low birth weight associated with advanced maternal age among four ethnic groups in the United States. Maternal and Child Health Journal, 9, 3–9. doi:10.1007/s10995-005-2446-4.
Chatters, L. M. (2000). Religion and health: Public health research and practice. Annual Review of Public Health, 21, 335–367. doi:10.1146/annurev.publhealth.21.1.335.
Ellison, C. G., & Levin, J. S. (1998). The religion-health connection: Evidence, theory, and future directions. Health Education & Behavior, 25, 700–720. doi:10.1177/109019819802500603.
Koenig, H. G., McCullough, M. E., & Larson, D. B. (2001). Handbook of religion and health. New York: Oxford University Press.
Jesse, D. E., & Reed, P. G. (2004). Effects of spirituality and psychosocial well-being on health risk behaviors in Appalachian pregnant women. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 33, 739–747. doi:10.1177/0884217504270669.
Magana, A., & Clark, N. M. (1995). Examining a paradox: Does religiosity contribute to positive birth outcomes in Mexican American populations? Health Education Quarterly, 22, 96–109.
Levin, J. S., Taylor, R. J., & Chatters, L. M. (1995). A multidimensional measure of religious involvement for African Americans. The Sociological Quarterly, 36, 157–173. doi:10.1111/j.1533-8525.1995.tb02325.x.
Stark, R., & Glock, C. Y. (1968). American piety. Berkeley: University of California Press.
Cochran, J. K., Beeghley, L., & Bock, E. W. (1988). Religiosity and alcohol behavior: An exploration of reference group theory. Sociological Forum, 3, 256–276. doi:10.1007/BF01115293.
Grasmick, H. G., Bursik, R. J., & Cochran, J. K. (1991). “Render unto Caesar what is Caesar’s”: Religiosity and taxpayers’ inclinations to cheat. The Sociological Quarterly, 32, 251–266. doi:10.1111/j.1533-8525.1991.tb00356.x.
Hoffman, J. P., & Bahr, S. J. (2005). Crime/Deviance. In H. R. Ebaugh (Ed.), Handbook of religion and social institutions (pp. 241–263). New York: Springer.
Ellison, C.G., Bradshaw, M., Rote, S., Storch, J., & Trevino, M. (in press). Religion and alcohol use among college students: Exploring the role of domain-specific religious salience. Journal of Drug Issues.
Kirkpatrick, L. A. (2004). Attachment, evolution and the psychology of religion. New York: Guilford Press.
Pollner, M. L. (1989). Divine relations, social relations, and well-being. Journal of Health and Social Behavior, 30, 90–104. doi:10.2307/2136915.
Burdette, A. M., Ellison, C. G., Sherkat, D. E., & Gore, K. A. (2007). Are there religious variations in marital infidelity? Journal of Family Issues, 28, 1553–1581. doi:10.1177/0192513X07304269.
Regnerus, M. D., & Uecker, J. (2007). Religious influences on sensitive self-reported behaviors: The product of social desirability, deceit, or embarrassment? Sociology of Religion, 68, 145–163.
Brewster, K. L., Cooksey, E. C., Guilkey, D., & Rindfuss, R. R. (1998). The changing impact of religion on sexual and contraceptive behavior of adolescent women in the U. S. Journal of Marriage and the Family, 60, 493–504. doi:10.2307/353864.
Hill, T. D., Burdette, A. M., Ellison, C. G., & Musick, M. A. (2006). Religious attendance and health behaviors of Texas adults. Preventive Medicine, 42, 309–312. doi:10.1016/j.ypmed.2005.12.005.
Hill, T. D., Ellison, C. G., Burdette, A. M., & Musick, M. A. (2007). Religious involvement and healthy lifestyles: Evidence from the Survey of Texas Adults. Annals of Behavioral Medicine, 34, 217–222. doi:10.1007/BF02872676.
Hill, T. D., & McCullough, M. E. (in press). Religious involvement and the frequency of intoxication among low-income urban women. Journal of Drug Issues.
Koenig, H. G., George, L. K., Meador, K., Blazer, D. G., & Ford, S. M. (1994). The relationship between religion and alcoholism in a sample of community-dwelling adults. Hospital & Community Psychiatry, 45, 586–596.
Gillum, R. F. (2005). Frequency of attendance at religious services and cigarette smoking in American women and men: The Third National Health and Nutrition Examination Survey. Preventive Medicine, 41, 607–613. doi:10.1016/j.ypmed.2004.12.006.
Koenig, H. G., George, L. K., Cohen, H. J., Hays, J. C., Blazer, D. G., & Larson, D. B. (1998). The relationship between religious activities and cigarette smoking in older adults. Journal of Gerontology: Medical Sciences, 53A, 426–434.
Bartkowski, J. P., & Xu, X. (2007). Religiosity and teen drug use reconsidered: A social capital perspective. American Journal of Preventive Medicine, 32, s182–s194. doi:10.1016/j.amepre.2007.03.001.
Regnerus, M. D. (2007). Forbidden fruit: Sex and religion in the lives of American teenagers. New York: Oxford University Press.
Wallace, J. M., Jr., & Forman, T. A. (1998). Religion’s role in promoting health and reducing risk among American youth. Health Education & Behavior, 25, 721–741. doi:10.1177/109019819802500604.
Steensland, B., Park, J. Z., Regnerus, M. D., Robinson, L. D., Wilcox, W. B., & Woodberry, R. D. (2000). The measure of American religion: Toward improving the state of the art. Social Forces, 79, 291–318. doi:10.2307/2675572.
Benjamins, M. R., & Brown, C. (2004). Religion and preventative health care utilization among the elderly. Social Science and Medicine, 58, 109–118. doi:10.1016/S0277-9536(03)00152-7.
Hadaway, C. K., Marler, P. L., & Chaves, M. (1993). What the polls don’t show: A closer look at U. S. church attendance. American Sociological Review, 58, 741–752. doi:10.2307/2095948.
Presser, S., & Stinson, L. (1998). Data collection mode and social desirability bias in self-reported religious attendance. American Sociological Review, 63, 137–145. doi:10.2307/2657486.
Regnerus, M. D., & Smith, C. (2005). Selection effects in studies of religious influence. Review of Religious Research, 47, 23–50. doi:10.2307/4148279.
Alwin, D. F. (1986). Religion and child-rearing orientations: Evidence of a Catholic-Protestant convergence. American Journal of Sociology, 92, 412–440. doi:10.1086/228506.
Curtis, K. T., & Ellison, C. G. (2002). Religious heterogamy and marital conflict: Findings from the National Survey of Families and Households. Journal of Family Issues, 23, 551–576. doi:10.1177/0192513X02023004005.
Krause, N. (2002). Exploring race differences in a comprehensive battery of church-based social support measures. Review of Religious Research, 44, 126–149. doi:10.2307/3512512.
Pargament, K. I., Smith, B. N., Koenig, H. G., & Perez, L. (2000). The many methods of religious coping: Development and validation of the brief RCOPE. Journal of Clinical Psychology, 56, 519–543. doi :10.1002/(SICI)1097-4679(200004)56:4≤519::AID-JCLP6≥3.0.CO;2-1.
Idler, E. L., Musick, M. A., Ellison, C. G., George, L. K., Krause, N. M., Levin, J. S., et al. (2003). Measuring multiple dimensions of religion and spirituality for health research: Conceptual background and findings from the 1998 General Social Survey. Research on Aging, 25, 327–366. doi:10.1177/0164027503025004001.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Page, R.L., Ellison, C.G. & Lee, J. Does Religiosity Affect Health Risk Behaviors in Pregnant and Postpartum Women?. Matern Child Health J 13, 621–632 (2009). https://doi.org/10.1007/s10995-008-0394-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-008-0394-5