Abstract
Objective. The objective of this study was to evaluate changes in antenatal care (ANC) utilization among semi-nomadic Bedouin Arab women living in the Negev desert of Israel before and after the establishment of a local Maternal and Child Health (MCH) Clinic. Methods. Retrospective record review of ANC utilization by pregnant women in two successive pregnancies, one before and one after the establishment of a local MCH Clinic. The study population was comprised of all 85 women who registered their newborns for care at MCH Clinic A, regardless of whether or not they had registered at the clinic for ANC. Records of their care in previous pregnancies were obtained from other MCH Clinics previously utilized by the family. Results. There was a significant increase in the percent of women receiving ANC from 31.8% to 57.6% with the establishment of the local MCH Clinic (p = 0.004), increase in the percent of pregnant women who had at least one physician examination from 27% to 45% (p = 0.003), in the percent who had at least 3 nursing visits from 25% to 39% (p = 0.011) and in the compliance with screening tests. There was no significant change in birth week and birth weight between pregnancies before and after the establishment of Clinic A. Conclusions. The study demonstrated improvement in utilization of ANC in the study population. However, after the establishment of a local MCH clinic, over 40% of pregnant women still received no ANC. Non-geographic barriers to ANC are important and need to be addressed through community-based intervention programmes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Utilization of antenatal services has been shown to be an important factor, affecting outcome of pregnancies [1–5]. However, there are many populations of pregnant women who lack access to antenatal care (ANC) [6–8]. In addition, the provision of accessible services does not guarantee compliance with recommended antenatal screening tests and preventive services due to economic, cultural and sociological barriers to care [6–10].
The Bedouin Arab population of the southern desert region of Israel (the Negev desert) is a semi-nomadic population with a high general fertility rate of 9.2 and high infant mortality rate of 15.8 per 1000 [11]. The Bedouin of Israel's Negev region represent an ethnic minority within Israel – a culture in transition from a semi-nomadic to urban lifestyle. A population of 155,000 Bedouin live in the Negev, of whom 40% still live in spontaneous settlements and encampments of extended families and the remaining 60% live in towns with an urban character. The vast majority of the Bedouin, including those who reside in towns as well as those that live outside of towns in spontaneous settlements and encampments, live within a 40-kilometer radius from Beer-Sheva, the central city of the Negev.
The average socioeconomic level of the Bedouin community is very low with an unemployment rate among men of at least 25% [11]. The rate of illiteracy among women of reproductive age is 40% [12]. The society is patrilineal and patriarchal, and polygamy is practiced with a high level of consanguinity. Forty percent of Bedouin are married to their first cousins and an additional 17% to more distant relatives [12].
According to Bedouin tradition, women are not allowed to travel alone among strange men; therefore they are often dependant on family members for transportation to medical services. The majority of Bedouin extended families own cars, but very few women, mostly of the younger generation, hold driving licenses.
All Bedouin residents in Israel are citizens and have been entitled to national health insurance by law since 1995. Primary curative care is provided by Health Maintenance Organizations (HMO's) through a network of neighborhood clinics. Preventive Maternal and Child Health Care (MCH) care is provided through a network of neighborhood clinics run by the Ministry of Health according to national guidelines for ANC.
The primary practioner in MCH Clinics is a public health nurse, with medical back-up provided by an obstetrician and a pediatrician. The public health nurse is responsible for giving anticipatory guidance to the pregnant woman, providing health education regarding recommended health behavior during pregnancy (diet, exercise, rest, refrainment from smoking and alcohol), measuring weight, blood pressure and urine analysis for protein and sugar during each pre-natal visit as well as examination for edema of lower extremities. She is responsible for performing VDRL, blood type and Rh tests on women registered at the MCH clinic and referral of pregnant woman to other health care providers in order to obtain laboratory examinations that cannot be performed at the MCH Clinic. She is responsible for follow-up and out-reach to those women who do not comply with the recommendations, and referral of any woman with signs of complications of pregnancy to their local HMO for evaluation and treatment by specialists. The public health nurse also provides instruction about signs of labor. She has also been trained to be alert to signs of family dysfunction (family violence, problems of postpartum depression and/or problems of maternal-child interaction) in order to facilitate early intervention.
Many of the recommended routine ANC screening tests cannot be performed in the MCH clinics. In order to perform these tests (e.g. complete blood count (CBC); urine culture, screening for glucose intolerance of pregnancy by glucose challenge test (GCT); ultrasound examination (US), alpha-fetal protein), the pregnant mother is referred to her local HMO and/or to a regional medical center.
Upon the registration of an infant at an MCH clinic, the public health nurse immediately clarifies with the mother the name of the clinic in which she and her other children previously received preventive MCH care. She then has the family's MCH records from MCH clinics previously utilized by the mother and her family transferred to the MCH clinic in which she and/or her children are currently receiving care. The records of ANC received by the mother in previous pregnancies in any MCH clinic in the country, together with the MCH record of the newborn infant, are filed together in a “family file,” allowing for easy record review of ANC in previous pregnancies.
Before the year 2000 there were 16 MCH Clinics serving the Bedouin population with 6039 live births [11], all of which were located in urban centers. Bedouin women living in semi-nomadic conditions in the desert had to travel a distance of up to 30 kilometers from their homes to urban centers in order to receive ANC in MCH Clinics.
In a study of 1,104 female residents of four Bedouin urban centers in Israel in 1994, 89% were found to have registered for ANC in a MCH clinic [12]. The Avicenne Initiative Study of post-partum Bedouin women in 1998 found that 91% of Bedouin women who were non-users of ANC lived in tribal units in spontaneous settlements and encampments while only 9% of non-users lived in established urban settlements [13]. They concluded that Bedouin women living in the desert outside of urban established settlements face geographical barriers to accessing ANC in MCH clinics.
As a result of this finding, the Ministry of Health of Israel began to establish in the year 2000 new local MCH Clinics in desert areas in which Bedouin extended families live in tribal units. The first MCH Clinic to be established outside of urban centers, Clinic A, serves a tribal unit, the majority of who live within 3 kilometers of the clinic. The clinic is accessible only by unpaved roads. The primary practioner in Clinic A is an Arabic-speaking Bedouin public health nurse.
The goal of this study was to evaluate changes in utilization of ANC care among Bedouin women before and after the establishment of a local MCH clinic in the desert in order to evaluate the extent to which removing geographic barriers to care can improve compliance with recommended ANC guidelines.
Methods
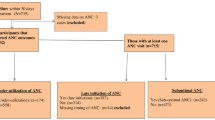
The present study was a retrospective record review of two successive pregnancies in women who gave birth both in the two year period preceeding the opening of Clinic A and in the two-year period after its establishment, regardless of whether or not they registered for ANC for either pregnancy. The study population was comprised of all 85 women who registered their newborn infants at Clinic A in the two-year period after the establishment of Clinic A and who gave birth both before and after its establishment in September 2000. The index pregnancy was defined as the first completed pregnancy after the establishment of local MCH Clinic A.
A record review was carried out in order to compare utilization of ANC care in the last two pregnancies of the same women - the pregnancy immediately before the establishment of Clinic A and the first pregnancy after the establishment of Clinic A. Demographic (independent) variables, which were extracted from MCH records, included birth order of the child of the index pregnancy, maternal age, consanguineous marriage, polygamy (women whose husband had more than one wife) and maternal and paternal education in years. In addition, data on presence or absence of genetic disease or congenital defects in previous pregnancies were collected.
ANC users were defined as women with at least one recorded visit to a MCH clinic during pregnancy. Gestational age at registration was determined by the week of pregnancy at the first antenatal visit, based on date of last menstrual period. Early initiation of care was defined as registration for ANC services at a MCH Clinic in the first trimester (≤13 weeks of gestation). Screening rates for three type of tests were evaluated: a test which is obtained locally at the MCH station by the MCH public health nurse (VDRL); a second group of tests (CBC and GCT) which are obtained at the local HMO Clinic (located adjacent to Clinic A) and a third test for which the pregnant mother has to travel at least ten kilometers (US).
Utilization of ANC was measured by several dependent variables: 1) ANC users (yes/no); 2) Early registration at MCH clinic at ≤13 weeks of gestational age (yes/no); 3) 3 or more ANC visits to public health nurse at MCH clinic (yes/no); 4) 1 or more ANC visits to obstetrician at MCH clinic (yes/no); 5) Compliance with screening tests (VDRL, CBC, GCT, US) (yes/no).
Dependent out-come variables included birth-weight and gestational age at birth as recorded on the newborn's MCH record on the basis of the newborn's discharge record from the hospital.
Comparisons of continuous and categorical variables between women who did and did not receive ANC after the establishment of Clinic A were performed using t-test for independent samples and chi-square test (Fisher's exact test when appropriate), respectively.
For comparison of utilization of ANC services and recommended ANC tests in successive pregnancies of women who were pregnant both before and after the establishment of Clinic A, paired t-test for continuous variables and McNemar's test for categorical variables were used. The software used for statistical analysis was SSPS 12.0.
Results
The demographic characteristics of the study population are presented in Table 1. The study population was characterized by low maternal educational level. Thirty five mothers (41.1%) had no formal education. Paternal educational level was significantly higher than maternal educational level (p < 0.001). Twenty (23.5%) mothers and 62 (72.9%) fathers had an educational level above 8 years. The study population was also characterized by high levels of polygamy (20%), a high rate of consanguinity (41.2% with first cousin marriages) and high birth order of the index pregnancy.
Forty nine women (57.6%) of the study population received ANC during the index pregnancy (after the establishment of local Clinic A), while 36 (42.3%) were non-users of ANC. We compared the demographic characteristics of ANC users and non-users in the index pregnancy (Table 2). With the exception of paternal education, no association was found between these variables and use of ANC services. An association was found between years of paternal schooling and use of ANC that approached marginal statistical significance (p = 0.053). We found no association between use of ANC services and history of having had a previous infant born with congenital defects or a genetic disease.
Comparison was made of the utilization of ANC services for the index pregnancy (after the establishment of local Clinic A) as compared with the last pregnancy in the same woman before the establishment of local Clinic A. There was a significant increase in the percent of pregnant women receiving ANC from 31.8% before to 57.6% after the establishment of Clinic A (p = 0.004). There were significant increases in the percent of pregnant women registering for care in the first trimester (at 13th week or earlier) from 3 (3.5%) to 6 (7.1%), in the percent of pregnant women who had at least one physician examination from 23 (27.1%) to 38 (44.7%) and an increase in the percent who had 3 or more nursing visits from 21 (24.7%) to 33 (38.8%) (Table 3). There was an increase in the percent of pregnant women performing recommended antenatal tests in the period after the establishment of local Clinic A compared with the period before its establishment (Table 3).
There was no significant change in gestational age at registration among ANC users between the last pregnancy before the opening of local Clinic A and the first pregnancy after its opening among women who registered for ANC at MCH clinic . Among those registered for ANC for the index pregnancy, the percent of women who complied with blood tests performed at the MCH clinic was higher than those who complied with recommended tests that have to be performed at locations other than MCH clinics. Among women who registered for ANC at MCH Clinic A, there was 100% compliance with the VDRL test, which is obtained at the clinic. This was significantly higher than the compliance with tests which had to be obtained at a HMO clinic (CBC, GCT) located a short distance from the MCH Clinic (92% for both) (p = 0.07). The compliance with US examination (90%), a test which is obtained at an urban center 10 kilometers away, was also significantly less than compliance with VDRL (p = 0.02).
We did not find a statistically significant change in gestational age at birth and mean birth weight between successive pregnancies in the same woman, before and after the establishment of Clinic A. Gestational age at birth before MCH Clinic A opened was 39.16 ± 0.20 weeks and 38.94 ± 0.25 weeks afterwards (p = 0.7). Mean birth weight of infants born before the new clinic was established was 3174 ± 52.7 gm and 3205 ± 63 gm after its establishment (p = 0.5).
Discussion and conclusions
We found that the establishment of a fully equipped MCH clinic in a desert area serving a Bedouin Arab population living in a radius of 3 km from the clinic improved the percent of pregnant women receiving ANC from 31.8% to 57.6%, as well as the percent of pregnant women registering for care early in pregnancy, the percent with at least one physician visit, the percent with at least three nursing visits and the percent who obtained recommended antenatal screening tests. However, more than 40% of women who registered their newborn infants at the new local MCH clinic for well-baby care did not attend the clinic for their ANC. This result indicates that there are other barriers to care that must be addressed in order to ensure adequate use of ANC services.
Our study design controlled for financial barriers to ANC since all mothers had registered at local Clinic A for MCH care for their infant. The registration fee that mothers above the poverty line are requested to pay covers preventive MCH care for all family members, including ANC. Since our study population included only women who registered their families at MCH clinic, all ANC at MCH Clinic A was provided with no additional charge. In addition, language could not be a barrier to care since the primary caregiver in Clinic A was an Arabic-speaking Bedouin public health nurse.
We failed to find an association between maternal education and utilization of ANC even though maternal education has been found to be a major factor affecting utilization of ANC services in the Middle East. In the 1990 Jordan Population and Family Health Survey [14] and in the 1993 Turkey Demographic and Health Survey [15], mother's education level was found to be a factor affecting ANC utilization. In Saudi Arabia, in a sample of pregnant women attending health centers in Riyadh [16], higher educational level of mothers was found to be associated with earlier gestational age at registration and more antenatal visits. The reason for not detecting an association between mothers’ education and ANC utilization in our study was the lack of variance in maternal educational level in our population of semi-nomadic Bedouin Arab women in Israel, of whom almost all were illiterate or semi-literate with a mean reported educational level of only 4 years.
Father's education may have more immediate impact on the use of ANC services than women's education in this population. In the current study, higher paternal education was associated with increased use of ANC services, although the result did not reach statistical significance (p = 0.053). Similarly, in Saudi Arabia [16], as well as in previous studies among Bedouin in Israel [13], paternal educational level was found to be associated with registration for ANC early in pregnancy. Findings of the importance of the husband's role in wife's use of ANC have been found in Saudia Arabia [16, 18] and Afganistan [19], as well as in previous studies of the Bedouin population in Israel [12].
An important finding of our study was that the main factor affecting compliance with recommended antenatal screening tests was registration or non-registration at the MCH clinic, since over 90% of those registered obtained an US examination, although it requires a trip of over 10 kilometers to the nearest urban center. In several MCH Centers serving the Bedouin population in Israel [17], the addition of a local Bedouin woman liaison worker who was trained to provide individual and group instruction to mothers attending the clinics regarding the importance of early registration and compliance with recommended antenatal screening tests was found to be associated with earlier gestational age at registration in subsequent pregnancies. Such a trained Bedouin liason worker was employed at both the new MCH Clinic A and at the urban clinic where women previously received their ANC services. This may explain the high rate of compliance with recommended antenatal screening tests among women in our study population who chose to register for ANC at a MCH clinic.
We were not able to show impact of establishment of new clinic A on gestational age at birth and on birth weight. This fact may be related to a serious limitation of our study—small sample size. The strength of our study is a “before and after” design based on analysis of data on utilization of ANC services in successive pregnancies of the same women, one pregnancy before and one after the establishment of a local MCH clinic. This study design controlled for family and personal factors which may affect utilization of ANC services.
Our study shows that it is possible to increase utilization of ANC services in hard-to-reach nomadic and semi-nomadic populations with high rates of illiteracy by the establishment of a local MCH Clinic. However, over 40% of the study population did not utilize the services offered. In this population of semi-nomadic Bedouin Arabs, the establishment of local MCH services needs to be complemented by programmes to encourage adequate utilization of the services provided. Such programmes should include not only promotion of maternal literacy, but also intervention programmes directed towards increasing the understanding of husbands of the importance of ANC for their wives. In addition, it is important to encourage grass-roots community involvement in order to increase awareness of the importance of ANC and to allow the community to organize a culturally and socially appropriate way to provide child-care and transportation for mothers attending antenatal care services.
References
Blondel B, Marshall B. Poor antenatal care in 20 French districts: risk factors and pregnancy outcome. J Epidemiol Community Health 1998;52:501–6.
Insler, V et al. The impact of prenatal care on the outcome of pregnancy. Eur J Obstet Gynecol Reprod Biol 1986;23:211–23.
Baldo M. The antenatal care debate. East Mediterr Health J 2001;7:1046–55.
Younis M et al. A study of the biosocial factors affecting perinatal mortality in an Egyptian maternity hospital. Popul Sci 1981;2:71–90.
El-Kak F et al. Patterns of antenatal care in low-versus high-risk pregnancies in Lebanon. East Mediterr Health J 2004;10:268–76.
Zanconato et al. Antenatal care in developing countries: the need for a tailored model. Semin Fetal Neonatal Med 2006;11:15–20.
Cindoglu D, Sirkeci I. Variables that explain variation in prenatal care in Turkey; social class, education and ethnicity re-visited. J Biosoc Sci 2001;33:261–70.
Navaneetham K, Dharmalingam A. Utilization of maternal health care services in Southern India. Soc Sci Med 2002;55:1849–69.
Lewando-Hundt G et al. Knowledge, action and resistance: the selective use of pre-natal screening among Bedouin women of the Negev, Israel. Soc Sci Med 2001;52:561–9.
York R et al. A review of problems of universal access to prenatal care. Nurs Clin North Am 1996;31:279–92.
Statistical Abstracts of Israel No 51, 2000, Jerusalem.
Weitzman D et al. Factors affecting the use of prenatal testing for fetal anomalies in a traditional society. Community Genetics 2000;3:61–70.
Lewando-Hundt G. Final report on CT93AV12-031, Evaluation and improvement of maternal and child preventive health services to for Palestinian in Gaza and Bedouin in the Negev. Negev. European commission, DGXII, 1999.
Shakhatreh F, Abbas A, Issa A. Determinants of infant mortality and the use of maternity services in Jordan. Dirasat Med Biol Sci 1996;23:59–69.
Celik Y, Hotchkiss D. The socio-economic determinants of maternal health care utilization in Turkey. Soc Sci Med 2000;50:1797–806.
Al-Shammari S, Khoja T, Jarallah J. The pattern of antenatal visits with emphasis on gestational age at booking in Riyadh Health Centers. J R Soc Health 1994;114:62–6.
Weitzman D. Consanguinity and utilization of prenatal tests to detect fetal malformations and hereditary diseases among the settled Bedouins of the Negev: evaluation of community interventions among pregnant women. PhD thesis, Beer-Sheva, Israel, 2003.
Nigenda G et al. Women's opinions on antenatal care in developing countries: results of a study in Cuba, Thailand, Saudi Arabia and Argentina. BMC Public Health 2003;20:3–17.
van Egmond K et al. Reproductive health in Afghanistan: results of a knowledge, attitudes and practices survey among Afghan women in Kabul. Disasters 2004;28:269–82.
Acknowledgements
We would like to thank Dr. Marina Rebchinsky for her contribution to the project.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Conflict of interest statement: The authors have no conflicts of interest regarding this research or paper
Rights and permissions
About this article
Cite this article
Bilenko, N., Hammel, R. & Belmaker, I. Utilization of Antenatal Care Services by a Semi-Nomadic Bedouin Arab Population: Evaluation of the Impact of a Local Maternal and Child Health Clinic. Matern Child Health J 11, 425–430 (2007). https://doi.org/10.1007/s10995-007-0193-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-007-0193-4