Abstract
Wounds exhibit varied behaviour and types and each type has its own differential healing requirements. This realization has encouraged the development of various wound dressings, each with specific characteristics. In the present study, composite hydrogels composed of PVA/Pullulan/Poly-L-Lysine/Gelatin (P/Pu/L/G) were fabricated using the freeze-thawing method with the aim of achieving enhanced wound healing. The hydrogels were evaluated for their physicochemical and in vitro biological properties. The morphological evaluation using SEM revealed the porous three-dimensional structure exhibited by the P/Pu/L/G hydrogels. The wettability and chemical composition of the hydrogels was elucidated by contact angle and ATR-FTIR analysis respectively, where the contact angle measurements showed an increase in the hydrophilicity of P/Pu hydrogel upon the incorporation of Poly-L-lysine and Gelatin. The results of in vitro hemolysis assay showed better blood compatibility of the fabricated hydrogels while the protein adsorption study revealed a 2.3-fold increase in the protein adsorption on the P/Pu/L/G hydrogels as compared to PVA hydrogels. The composite P/Pu/L/G scaffolds exhibited a 2-fold increase in the cell viability on day 7, when compared to the control; while the results of the scratch assay where complementary to the cell viability assay, which affirmed improved cell migration and proliferation in the presence of P/Pu/L/G hydrogels. The overall results of physicochemical characterization and biological evaluation advocates the potential of the composite hydrogels of P/Pu/L/G for biomedical applications such as wound dressing.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A wound is a defect or break in the skin which may occur due to trauma, physiological or thermal damage [1, 2]. Wound dressings have been applied to open wounds since centuries to prevent further injury and protect the wound from microbial infections. They have been predominantly used to promote the various wound healing stages (haemostasis, inflammation, proliferation, and remodeling) and build appropriate healing environment [3, 4]. An ideal wound dressing should fulfill the following characteristics: maintain a local moist environment, remove excess exudates, and protect from infections and contaminations. Moreover, the material should be non-allergic, biocompatible, biodegradable, elastic with good mechanical properties, cost-effective, and comfortable to remove or replace [1,2,3]. Currently, the designs of the dressings have evolved towards exhibiting multi-functionality for better healing and control of infections.
Hydrogels are an appropriate candidate for wound dressing as a result of its peculiar properties: Hydrogels can swell and de-swell water in a reversible direction in response to specific physiological stimuli [5], they maintain the local moist environment at the wound site [1], and possess tissue-like structure and compatibility [1, 2]. Hydrogels may induce autolytic debriment that facilitates the elimination of dead tissue [2], they have high exudates carrying capacity, are nonadherent, flexible, and easily removable from the wound site. Moreover, hydrogels may accelerate wound healing, reduce pain and inflammation and are easy to develop and handle [1, 2]. Their tight mesh networks protect the wounds from infection and microbial attack [1]. Hydrogels can be fabricated using physical, radiation or chemical cross-linking methods [5]. Freeze-Thawing (F-T) method is one of the physical cross-linking methods used in the preparation of hydrogels, creating a strong and highly elastic gel. The hydrogels prepared using this method has advantages such as the nontoxicity, noncarcinogenity and the good biocompatibility [5, 6].
Polymeric hydrogels have attracted great attention and have been intensively used by biomaterial scientist for many years [1]. PVA is the widely explored water-soluble, synthetic polymer for wound dressing, wound management, drug delivery, tissue engineering scaffold and implantable devices [1, 3, 6,7,8,9,10,11] as a consequence of its favourable properties such as: biocompatibility, bio-adhesiveness, visco-elasticity, biodegradability, excellent film-forming ability, transparency and ease of processing [3, 5, 10, 12,13,14,15]. However, PVA has inadequate elasticity, stiff membrane and incomplete hydrophilic characteristics which limit its use alone as a wound dressing polymeric material [1]. To improve mechanical strength and the stability of PVA hydrogels, investigators have focused on modifying PVA by introducing molecules such as natural polysaccharides, proteins, and synthetic materials [1, 10, 16]. Hydrogels derived from both natural and synthetic sources may serve as dressing material during repair and have been employed clinically [17, 18]. Gelatin is one such natural protein, obtained by hydrolysis of collagen and is available abundantly [1, 5, 6, 19]. The properties of gelatin that make it a biomaterial favorable for wound healing include its high water holding property, gelling property, film-forming ability, ability to provide a moist environment and accelerate wound healing [5, 6, 20, 21]. Moreover, their ability to provide immediate haemostasis, prevent wound contracture and facilitate cell adhesion and proliferations must be highlighted [21]. The prime disadvantage associated with gelatin is their fast degradation rate, low thermo-stability, poor mechanical stability, less flexibility and brittle nature in the dry state [5, 21]. Also, due to its origin from a natural source, the physical and chemical properties of gelatin vary considerably [10]. Therefore, gelatin by itself is not used as a biomaterial and is combined with other compounds [20]. To a certain degree, gelatin combined with PVA can overcome the issues of mechanical stability; however, the hemostatic performance of such hydrogels is not very good [5].
Lysine is a naturally occurring, alkaline amino acid with its structure similar to that of gelatin [10]. It has three reactive groups (α-carboxyl group, α-amino group, and ε-amino group) for chemical modifications [10, 22]. It is soluble in water and can be introduced in PVA hydrogel to promote cell adhesion, bioactivity, and biocompatibility [10]. However, PVA is found to be incompatible with lysine due to the absence of interactions between these two phases, and thus, cross-linkers are used to obtain a homogenous composite with excellent stability [10]. Pullulan, a non-ionic, linear exopolysaccharide is produced from starch by fungus Aurebasidium Pullulans [20, 23,24,25]. It is attractive as biomaterial because of its good mechanical properties, biocompatibility, film-forming ability and enzymatically mediated degradability [24,25,26,27]. It is a unique carbohydrate which is blood compatible, non-toxic, non-immunogenic and has good antioxidant property [17, 20, 25]. Pullulan possesses oxygen barrier property, good moisture retention and also may inhibit fungal growth [25]. Its multiple functional groups permit it to crosslink better and also form sponges with good absorbent capacity, thermal stability, and excellent mechanical properties [23, 25]. The properties of Pullulan can be attributed to the characteristic glycosidic linking, consisting of glucose units linked through α-1,6- and α-1,4- glycosidic bonds, with structural flexibility which can be further chemically modified [24, 25]. However, the poor bioactivity and limited cell adhesion ability on its surface hamper its biomedical applications as wound dressings and thus, is its blending or crosslinking with various biologically active polymers has been investigated [24, 25].
In the present study, with the aim of achieving wound dressing material with ideal properties, composite hydrogels composed of PVA/Pullulan/Poly-L-lysine/Gelatin were fabricated using freeze-thaw cycle method and characterized for their physicochemical properties using Scanning electron microscopy (SEM), Contact angle analysis, Attenuated Fourier Transformed Infrared Spectroscopy (ATR-FTIR), and water uptake potential. Further, biological evaluation of the hydrogels was carried out by performing hemolysis assay, protein adsorption assay, cell viability assay, and cell migration assay to validate the wound healing potential of the hydrogels.
Materials and method
Materials
PVA (Mw-31,000 – 50,000, 99% hydrolyzed), Poly-L-lysine hydrochloride (Mw- 15,000 – 30,000) were purchased from Sigma-Aldrich. Pullulan (Mw- 200,000) was purchased from Hayashibara laboratories, Japan. Gelatin type-B was procured from Loba-Chemie chemical. D-PBS, DMEM, TPVG, antibiotic solution was purchased from Himedia biosciences, India. All other chemicals unless specified were of analytical grade.
Fabrication of hydrogels
PVA solution was prepared by dissolving PVA (10% w/v) in milliQ water and continuously stirring for 1 h at 90 °C. The temperature of the PVA solution was cooled down to 60 °C, and Pullulan (10% w/w) was added to it followed by stirring for 1 h at 60 °C, in order to prepare PVA/Pullulan blend solution. Further, Poly-L-lysine (10% w/w) or Gelatin (10% w/w) were added to PVA/Pullulan solution followed by stirring for 1 h at 60 °C in order to prepare PVA/Pullulan/Poly-L-lysine and PVA/Pullulan/Gelatin solution respectively. Finally, PVA/Pullulan/Poly-L-lysine/Gelatin solution was prepared by adding both Poly-L-lysine (10% w/w) and Gelatin (10% w/w) to PVA/Pullulan solution followed by stirring for 1 h at 60 °C.
Hydrogels of PVA, PVA/Pullulan (P-Pu), PVA/Pullulan/Poly-L-lysine (P-Pu-L), PVA/Pullulan/Gelatin (P-Pu-G) and PVA/Pullulan/Poly-L-lysine/Gelatin (P-Pu-G-L) were fabricated by the freeze-thawing method. The respective solutions were poured in 35 mm cell culture dish, avoiding the formation of air bubbles. Subsequently, all samples were transferred to −20 °C for 12 h and later withdrawn for thawing at room temperature for 5 h. This cycle was repeated 7 times, and at the end of the fabrication process, the hydrogels were stored at 4 °C, until their use for further experiments.
Physicochemical characterization
Morphological analysis
The morphological analysis of the hydrogels in their dry state was carried out using scanning electron microscopy analysis (FE-SEM, Nova Nano SEM 450) at an accelerating voltage of 5 kV.
Contact angle analysis
The hydrophilicity of the hydrogels was evaluated using contact angle analysis carried out in a static mode using Kruss Drop shape analyzer. A drop of 3 μl of deionized water was placed on the hydrogel, and immediately the contact angle was measured by the sessile drop method using Advance software. The analysis was performed by placing water drop at different randomly selected locations of three independent samples, and the results were reported as mean ± SD.
ATR-FTIR analysis
Fourier Transform Infrared Spectroscopy analysis of the hydrogels was performed in Attenuated Total Reflectance mode using Bruker Alpha T spectroscopy. The samples were dried and pressed against the platinum crystal, and the spectra were obtained in the range of 400–4000 cm−1.
Water uptake capacity
Hydrogels of 1 cm2 (n = 3) were dried, and their dry weights were recorded. The hydrogels were soaked in milliQ water for 24 h at ambient temperature. The hydrogels were removed from the water, wiped with tissue paper and immediately their weights were recorded [28].
Where, W1 and W2 represent the weights before and after soaking in water and S represent the surface area of the hydrogels.
Hemolysis assay
The effect of hydrogels on the RBCs was evaluated by performing hemolysis assay [28,29,30,31]. Human blood (citrated) was obtained from Indian Serological Institute, Pune, India and used as received. The blood was centrifuged at 1200 rpm for 15 min to obtain the RBCs. The RBCs were washed and diluted using D-PBS in 1:20 (v/v) ratio of RBCs: D-PBS. The dried hydrogels (1 cm2, n = 3) were placed in 24 well plate and soaked in D-PBS at 37 °C for 1 h. D-PBS was replaced with 1 ml diluted RBCs and further incubated for 1 h at 37 °C. PBS diluted RBCs was taken as negative control whereas, positive control was 0.2% Triton X-100 diluted RBCs. Post incubation the plate was centrifuged at 3000 rpm for 15 min and the supernatant was transferred to a fresh 24 well plate. The absorbance of the hemoglobin released in the supernatant was recorded at 545 nm using a multi-plate reader (Eon Biotek, USA). Finally, the percentage of hemolysis was calculated using the formula:
Where, TS, NC, and PC are measured absorbance values of the test sample, negative control, and positive control at 545 nm, respectively [31].
Protein adsorption
The hydrogels (1 cm2, n = 3) were placed in a 24 well plate and soaked in D-PBS for 1 h. 1 ml Bovine serum albumin (1 mg/ml, BSA) was added per well and incubated for 2 h at 37 °C. Post incubation, the BSA solution was removed, and hydrogels were washed with D-PBS to remove unbound proteins. Further, 1 ml SDS (2% w/v) was added to each well and plates were kept for shaking at 200 rpm for 30 min followed by bath sonication for 10 min. BCA assay of the protein lysate solution was performed as per manufacturer’s protocol, and absorbance corresponding to the presence of protein was recorded at 562 nm [28, 30, 31].
In vitro cell viability assay
The cell viability of NIH/3 T3 on the hydrogels was evaluated for 7 days using MTT (3-(4,5-Dimethyl-2-thiazolyl)-2,5-diphenyltetrazolium bromide) assay. The hydrogels (1 cm2, n = 3) were placed in a 24 well-plate and UV sterilized for 2 h (each side). Further, the hydrogels were pre-wetted in the cell culture medium (DMEM) for 1 h followed by cell seeding at density of 1 × 104 cell /cm2 and incubated at 37 °C, 5% CO2. On achieving respective time-point (day 1, 3, and 7), 1 mg/ml MTT (300 μl) was added to each well followed by incubation for 4 h. Post incubation, the formazan crystals were dissolved by adding Dimethysulfoxide and the absorbance was recorded at 570 nm using multi-plate reader (Eon Biotek, USA) [32].
In vitro cell migration assay
Scratch assay test was performed to evaluate the cell migration of NIH3T3 cells in the presence of the hydrogels. Cells at a density of 2 × 105 cells/ml were seeded in 24 well culture plates and incubated to achieve a mono layer. A sharp scratch was gently scrapped in the monolayer using an autoclaved tooth-pick. The cell debris was removed, and the edges of the scratch were smoothened by washing the cells with 1 ml of the plain culture medium. The UV sterilized hydrogels (1 cm2, n = 3) were carefully placed in the wells, supplemented with the growth medium and incubated. At respective time-points, the cell migration towards the filling of gaps was visualized using phase contrast microscope, and images were captured. [29].
Statistical analysis
Results were reported as mean ± standard error of mean (SEM). Statistical analysis was performed using one-way analysis of variance and difference of P < 0.05 was considered as statistically significant. The significance level was defined as * P < 0.05, ** P < 0.01 and *** P < 0.001.
Results
Fabrication of hydrogels and its morphological analysis
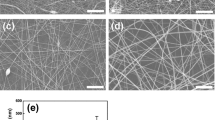
The hydrogels of PVA, P/Pu, P/Pu/L, P/Pu/G and P/Pu/L/G as shown in Fig. 1a were successfully fabricated using F-T method. The physical appearance of the PVA, P/Pu, P/Pu/L hydrogels was found to be transparent and clear; while the Gelatin containing P/Pu/G and P/Pu/L/G hydrogels exhibited opaque yellowish colour with a rough surface. The Fig. 1b represents the SEM micrographs of the hydrogels. The PVA hydrogels incorporated with bioactive compounds exhibited three-dimensional network structure with presence of porous architecture. The surface of the PVA hydrogels was observed to be smooth with no presence of pores, while the addition of bioactive compounds caused formation of rough surface with presence of micropores in case of the P/Pu and P/Pu/L hydrogels. The incorporation of gelatin to P/Pu and P/Pu/L hydrogels showed a highly interconnected network of hydrogel with the presence of micropores, mesopores and caves.
Contact angle analysis
The surface hydrophilicity of the composite hydrogels was determined using contact angle analysis and depicted in Fig. 2. The contact angle was evaluated immediately after dropping a drop of water on the hydrogel surface. The PVA hydrogel showed a characteristic hydrophilic nature with the mean contact angle of 39.28°. Incorporation of Pullulan to P/Pu caused a comparative reduction in the hydrophilicity with the contact angle of 62.38°. Further, the incorporation of Poly-L-lysine, Gelatin, and Poly-L-lysine-Gelatine to P/Pu/L, P/Pu/G and P/Pu/L/G respectively increased the hydrophilicity of the hydrogels showing water contact angles of 52.08°, 44.0° and 40.01° respectively.
ATR-FTIR analysis
The spectra for ATR-FTIR analysis of the hydrogels is represented in Fig. 3. The PVA hydrogel showed characteristic –OH stretching peak at 3234.1 cm−1 along with the peak at 2909.57 cm−1 corresponding to the C-H stretching vibration of CH2 group. The strong peak at 1083.25 cm−1 indicates the presence of C-O. [33] The addition of Pullulan in P/Pu hydrogel showed additional peaks of α-glucopyranoside units at 841.6 cm−1. The band at 754 cm−1 represents the presence of α-(1, 4) glucosidic bonds and the band at 924.7 cm−1 represents the presence of α-(1, 6) glucosidic bond. The 1331.27 cm−1 bands attributed to CH/CH2 deformation vibration [33]. The peak at 1568.58 cm−1 in P/Pu/L and P/Pu/L/G corresponds to the amide II band. In case of P/Pu/G and P/Pu/L/G hydrogels, the bands at 3289.6 cm−1, 2933.7 cm−1, 1630.7 cm-1, and 1528.19 cm−1 are denoted as A, B, I and II amide bands respectively.
Water uptake capacity
The water uptake assay was performed to investigate the water retention property of the hydrogels and is represented in Fig. 4. It was observed that the hydrogels retained their general shape and did not disintegrate upon 24 h incubation in water (Fig. 1a). The water uptake for PVA hydrogel was found to be 91.7 mg/cm2, which was seen to reduce to 49.7 mg/cm2 for P/Pu hydrogel on the incorporation of Pullulan to PVA. Further, the incorporation of Poly-L-lysine, Gelatin, and Poly-L-lysine-Gelatine to P/Pu/L, P/Pu/G and P/Pu/L/G respectively gradually increased the water uptake to 67.7 mg/cm2, 89.3 mg/cm2, and 117.1 mg/cm2 respectively.
Hemolysis assay
The hemolysis ratio of the composite hydrogels is represented in Fig. 5. The positive reference was considered 100% hemolytic, and the negative reference was considered 0% hemolytic. The extent of hemolysis ratio for hydrogels of PVA, P/Pu, P/Pu/L, P/Pu/G, and P/Pu/L/G was found to be 0%, 0.5%, 0.7%, 3.3% and 1.3% respectively. Incorporation of gelatin within P/Pu/G or P/Pu/L/G caused increase in the hemolysis ratio of P/Pu and P/Pu/L hydrogels respectively.
Protein adsorption
The amount of BSA protein adsorbed on different hydrogels was determined using BCA assay and is represented in Fig. 6. The incorporation of Pullulan to PVA caused 36.2% reduction in the protein adsorption on P/Pu hydrogel. Further incorporation of Poly-L-lysine, caused the increase in protein adsorption on P/Pu/L hydrogels, however it was 32.4% lower as compared to PVA hydrogels. The incorporation of Gelatin to P/Pu and P/Pu/L hydrogel caused a dramatic increase in protein adsorption (1.7 and 2.3 fold respectively) as compared to PVA hydrogel.
In vitro cell viability assay
To determine the biocompatibility of the hydrogels, the NIH3T3 cell viability on the hydrogels was assessed over a period of 7 days and represented in Fig. 7. The cell viability for all the hydrogel types was seen to increase with the increasing incubation period from day 1 to day 7. At day 7 of the incubation, the cell viability on P/Pu, P/Pu/L, P/Pu/G, and P/Pu/L/G hydrogels was found to be 71.4%, 201.54%, 210.68%, and 277.86% higher as compared to the PVA hydrogel.
In vitro cell migration assay
To elucidate the effect of the hydrogels on the wound re-epithelialization, cellular proliferation and migration of fibroblasts were studied after 24 h and 48 h of incubation as shown in Fig. 8. The microscopic images post 24 h of incubation revealed significant cell proliferation and migration across the scratched area in the presence of the P/Pu/L, P/Pu/G and P/Pu/L/G hydrogels, while the gap closure was seen to be significant at 48 h post incubation as seen in Fig. 8. The hydrogels of P/Pu/L/G caused the highest number of cell migration in the denuded area, forming a confluent monolayer. The cells, however, showed lower cell proliferation and migration on the control (PVA) hydrogels as observed by scratch assay results. The results of cell migration assay thus confirm the enhancement in the wound healing property by the composite hydrogels.
Discussion
Traditional wound dressing materials hardly play a role in case of infections or festering wounds [5]. A considerably high amount of water and fluid loss occurs from wounded skin as compared to normal skin [1]. Thus, the water permeability property of the dressings must maintain equilibrium between the dehydration and the excess accumulation of exudates at the wound site, without affecting the epithelialization or cell proliferation process [1]. It has been demonstrated that a wet dressing boosts the wound healing process as compared to dry dressings [1]. This may be ascribed to the healing and skin renewal without the formation of eschars or inflammation in case of the moist environment [1]. Moreover, wet dressings are considered to exhibit high water content and possess inherent permeability [1]. Thus, advanced dressings are designed to maintain a moist local environment at the wound site which allows the fluids to remain close to the wound while avoiding its spread to the unaffected healthy skin [2].
Hydrogels are widely used as de-bridging agents, moist dressings, and components of pastes for wound care [2]. They do not need further wound fluid to become gels and thus are suitable for dry wounds as well [2]. The mechanism of hydrogels as wound dressing materials can be ascribed to their ability to absorb and retain wound exudates, promoting cell migration and proliferation [1]. The structure of hydrogels is usually stabilized by cross-linking the hydrogel using chemical or physical interactions amongst the polymer chains [1]. The physical or the radiation based cross-linking methods are the most favoured over chemical cross-linking method because they eliminate the use of cross-linkers exhibiting inherent cytotoxicity [1, 3, 5, 6]. The F-T method is one of the physical crosslinking methods, creating a strong and highly elastic gel [3]. In the current study, PVA gels were prepared by F-T method, which induced crystallization of PVA [14]. PVA can crystallize upon cooling from the melt [3]. On a molecular level, the crystallites of PVA are a layered structure [3, 34]; upon cross-linking, the double layer of the molecules are held together by hydroxyl bonds, while the weaker van der wall forces operate between the double layer [3]. PVA contains many hydroxyl groups in its carbon chain and thus can form hydrogen bonding with another polymer on blending [10]. The change in the size of the hydrogel was seen to occur during the F-T procedure; with the hydrogel returns back to the original size before F-T step [20]. The morphological analysis of the hydrogels by SEM analysis showed the porous structure exhibited by the fabricated hydrogels. The materials with porous architecture are favored as wound dressings as they are permeable to water vapor and exudates from wounds. Moreover, such material may prevent bullae formation. The hydrophilic characteristics of the hydrogel were studies using contact angle analysis which showed highly hydrophilic nature of PVA with a reduction in its hydrophilicity on the addition of Pullulan and further gradual increase in the hydrophilicity on the incorporation of biological cues such as poly-L-lysine and gelatin.
The ATR-FTIR spectra gave the information related to the chemical composition and the interaction of the blended components in the composite. The amide II band in case of P/Pu/L and P/Pu/L/G could be related to the carbon-nitrogen (C-N) stretching vibration that can be implied to the characteristics of amino acids in lysine [10]. The amide A and B bands are mainly associated with the stretching vibration of N-H groups. The amide I is generated from the carbonyl (C=O) stretching coupled to N-H bending vibration. The amide II band is generated from the N-H bending vibration coupled to C-N stretching vibration [21]. The possible interactions in the composite could be hydrophobic bonds, electrostatic interactions and also hydrogen bonds [21]. The extent of polymer swelling and its swelling rate are essential properties of the hydrogel that affects its ability to allow diffusion of nutrients, the release of therapeutics and nutrients and the adsorption of exudates in case of wound healing [14, 20, 35,36,37]. It is directly correlated to the hydration ability and indirectly to the mechanical stiffness and structural properties of the hydrogel [38]. Swelling/ water uptake of a hydrogel ensures a moist environment, and adsorption of a small to medium amount of wound exudates, which is critical for wound healing [14, 38]. The water uptake of P/Pu was seen to reduce on addition of Pullulan; this might be due to the comparatively lower hydrophilicity of P/Pu hydrogels as compared to PVA hydrogels and also due to increases in the presence of higher bonds in hydrogel membrane which might limit the diffusion of water for swelling [14]. The remarkable increase in the swelling capacity was observed on addition of gelatin, which may be due to the presence of more hydrophilic groups in the network and because gelatin has higher water absorbing capacity and can hold about 5 to 10 times more fluid as compared to their own weight [5]. Similar results were reported by other research group in the past [14]. The water in hydrogels can be divided into: bound water, half-bound water, and free water. The quantity of bound water and half-bound water relates with the number of hydrophilic groups in the hydrogel, whereas, the three-dimensional structure and pore volume of hydrogel relates with the content of free water [21]. The high water adsorption capacity of the modified hydrogels reveals the presence of three-dimensional structures with a porous network which could be beneficial for cell adhesion and proliferation [21].
The blood compatibility of the hydrogels was evaluated in vitro by measuring the RBCs lysis on their contact with the hydrogels. The hemolysis assay represents the extent of fracture and dissolution of RBCs caused by the material’s contact with the blood [21]. Therefore, a material must exhibit lower hemolysis ratio to be blood compatible. As per the ASTM standards, a material to be used for the medical application must exhibit hemolysis ratio not more than 5%. The result of our hemolysis assay confirms the blood compatibility of the composite hydrogels with their hemolysis ratios below 4%. It was observed that the hemolysis ratio of P/Pu and P/Pu/L composites increased on addition of Gelatin, which may be due to the presence of an active group (-NH2) in gelatin [21]. The interaction of cells with the material starts with protein adsorption which directly affects cell adhesion and proliferation making the phenomenon of protein adsorption a crucial factor. A material with high protein adsorption property is preferred because; adsorption of serum proteins could result in platelet adhesion, activation and initiation of wound healing process [3, 39]. The mechanism of protein adsorption on a surface is owing to the various type of interacting forces between the protein molecules and the membrane surfaces, such as weak bonds (van der wall forces, hydrophobic interactions, ionic bonds, and hydrogen bonds), and covalent bonds present in chemically surface modified membranes [3, 40]. In our study, the higher protein adsorption was observed on the addition of gelatin to P/Pu and P/Pu/L hydrogels. This increased adhesion might be due to the higher hydrophilic interactions as a result of the addition of gelatin. Our results are in accordance with the previous studies by [3] wherein; they observed increased protein adsorption with increasing hydrophilicity of the surface. Similar results were reported by kim, et al. [41], and Hwang et al. [42].
The in vitro biocompatibility is of principle importance for the success of any biomaterial [3]. The structured aqueous nature of the hydrogels provides an ideal environment for cellular growth and sustainability [17]. The fibroblasts and the keratinocytes are the predominant cells found in the skin which makes up most of the dermal layer and epidermal layer respectively [3]. PVA hydrogels are intrinsically resistant to protein adsorption, and thus cell material interactions are limited on its surface. In order to stimulate cell adhesion and proliferation on the PVA based hydrogels, we incorporated biological cues such as Poly-L-lysine and gelatin which are known to stimulate cellular adhesion and proliferation processes. The results of the MTT assay showed a dramatic increase in the percent (%) cell viability on the P/Pu/L/G hydrogels upon the incorporation of poly-L-lysine and gelatin. Poly-L-lysine promotes the non-specific attachment of cells to solid substrates by enhancing electrostatic interaction between negatively charged ions of the cell membrane and the material surface. The cell viability results of day 1 highlight the beneficial role of poly-L-lysine in case of P/Pu/L and/Pu/L/G hydrogels, whereby its presence caused higher initial cell attachment and thus viability on the hydrogel surface. Moreover, the presence of gelatin improved the performance of the hydrogel with respects to cell viability; this may be attributed to the integrin binding sites (such as RGD tri-peptide) in gelatin which positively influences the cell-specific attachment and growth through RGD–integrin conjugation thus, promoting cell proliferation. The other possible factors influencing the increased cell viability could be attributed to the improved hydrophilicity and protein adsorption on the developed hydrogels. The trypan blue exclusion assay was performed to confirm the results of cell viability obtained by MTT assay, the results of which verified that enhanced biocompatibility of the modified hydrogels (data not incorporated). Cell migration is a complex multi-step process and involves the migration of cells which plays a vital role in wound repair [36]. The wound scratch model is a two-dimensional assay to evaluate wound healing in vitro [36]. The wound healing hydrogels showing improved wound gap closure ability in vitro have also been known to exhibit remarkable wound healing ability in vivo [36]. The data thus advocate the efficiency of the of P/Pu/L/G hydrogel which could potentiate re-epithelialization of the wounded site. The results of this study provide evidence that the P/Pu/L/G hydrogels promote cell proliferation and migration and thus could be potential materials to facilitate the wound healing and repair process.
Conclusion
The current study reports the engineering of biomimetic PVA/Pu hydrogels with biological cues such as Lysine and Gelatin and there physicochemical and biological evaluation as wound dressing material in vitro. Our results indicated that the biomimetic P/Pu/L/G hydrogels were effective biomaterials with respect to properties such higher hydrophilicity and water absorption capacity which could be advantageous in an application such as wound dressing since they can absorb wound exudates and provide a moist environment as a virtue of good swelling properties. The incorporation of bioactive components to PVA lead to the formation of hydrogel with a porous architecture. The hydrogels were found to be blood compatible and exhibited higher protein adsorption. Further, the developed hydrogel displayed improved initial cell adhesion and enhanced cell viability as a result of the use of bioactive compounds Poly-L-lysine and Gelatin respectively. The data from scratch assay highlights the efficiency of the of P/Pu/L/G hydrogel which could potentiate re-epithelialization of the wounded site. However, the hydrogels must be further evaluated for their mechanical properties in the dry and wet state and further studies at in vivo level must be conducted for their clinical translation.
References
Kamoun EA, Kenawy ES, Chen X (2017) A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J Adv Res 8:217–233
Calo E, Khutoryanskiy VV (2015) Biomedical applications of hydrogels: a review of patents and commercial products. Eur Polym J 65:252–267
Fahmy A, Kamoun EA, Eisawy RE, El-Fakharany EM, Taha TH, El-Damhougya BK, Abdelh F (2015) Poly(vinyl alcohol)-hyaluronic acid membranes for wound dressing applications: synthesis and in vitro bio-evaluations. J Braz Chem Soc 26:1466–1474
Kaolaor A, Phunpee S, Ruktanonchai UR, Suwantong O (2019) Effects of β-cyclodextrin complexation of curcumin and quaternization of chitosan on the properties of the blend films for use as wound dressings. J Polym Res 26:43–54
Fan L, Yang H, Yang J, Peng M, Hu J (2016) Preparation and characterization of chitosan/gelatin/PVA hydrogel forwound dressings. Carbohydr Polym 146:427–434
Jaiswal M, Gupta A, Agrawal AK, Jassal M, Dinda AK, Koul V (2013) Bi-layer composite dressing of gelatin Nanofibrous mat and poly vinyl alcohol hydrogel for drug delivery and wound healing application: in-vitro and in-vivo studies. J Biomed Nanotechnol 9:1495–1508
Chen DH, Leu JC, Huang TC (1994) Transport and hydrolysis of urea in a reactor-separator combining an anion-exchange membrane immobilized urease. J Chem Tech Biotechnol 61:351–357
Hyon SH, Cha W, Ikada Y, Kita M, Ogura Y, Honda Y (1994) Poly(vinyl alcohol) hydrogels as soft contact lens material. J Biomater Sci Polym Ed 5:397–406
Smith TJ, Kennedy JE, Higginbotham CL (2009) The rheological and thermal characteristics of freeze-thawed hydrogels containing hydrogen peroxide for potential wound healing applications. J Mech Behav Biomed Mater 2:264–271
Zhou G, Ruhan A, Ge H, Wang L, Liu M, Wang B, Su H, Yan M, Xi Y, Fan Y (2014) Research on a novel poly (vinyl alcohol)/lysine/ vanillin wound dressing: biocompatibility, bioactivity and antimicrobial activity. Burns 40:1668–1678
Hassan CM, Peppas NA (1999) Structure and application of poly(vinyl alcohol) hydrogels produced by conventional crosslinkingor by freeze thawing methods. Adv Polym Sci 153:38–62
Yoshiia F, Zhanshanb Y, Isobec K, Shinozakic K, Makuuchi K (1999) Electron beam crosslinked PEO and PEO/PVA hydrogels for wound dressing. Radiat Phys Chem 55:133–138
Kamoun EA, Chen X, Mohy Eldin MS, Kenawy ES (2014) Crosslinked poly(vinyl alcohol) hydrogel for wound dressing applications: a review of remarkably blended polymers. Arab J Chem 8:1–14. https://doi.org/10.1016/j.arabjc.2014.07.005
Baghaie S, Khorasani MT, Zarrabi A, Moshtaghian J (2017) Wound healing properties of PVA/ starch /chitosan hydrogel membranes with nano zinc oxide as antibacterial wound dressing material. J Biomater Sci Polym Ed 28:2220–2241. https://doi.org/10.1080/09205063.2017.1390383
Lian Z, Ye L (2015) Synthesis and properties of carboxylated poly (vinyl alcohol) hydrogels for wound dressings. J Polym Res 22:72–83
Miranda LFD, Cunha KLG, Barbosa ITF, Masson TJ, Munhoz AH (2018) Obtaining hydrogels based on PVP/PVAL/Chitosa containing Pseudoboehmite nanoparticles for application in drugs. Intech Open, Hydrogels. https://doi.org/10.5772/intechopen.72007
Wong VW, Rustad KC, Galvez MG, Neofytou E, Glotzbach JP, Januszyk M, Major MR, Sorkin M, Longaker MT, Rajadas J, Gurtner GC (2011) Engineered pullulan–collagen composite dermal hydrogels improve early cutaneous wound healing. Tissue Eng A 17:5–6
Annabi N, Mithieux SM, Weiss AS, Dehghani F (2009) The fabrication of elastin-based hydrogels using high pressure CO2. Biomaterials 30:1–7
Shafagh N, Sabzi M, Afshari MJ (2018) Development of pH-sensitive and antibacterial gelatin/citric acid/ag nanocomposite hydrogels with potential for biomedical applications. J Polym Res 25:259–266
Nicholas MN, Jeschke MG, Amini-Nik S (2016) Cellularized bilayer pullulan-gelatin hydrogel for skin regeneration. Tissue Eng A 22:9–10
Lia D, Yea Y, Li D, Li X, Mu C (2016) Biological properties of dialdehyde carboxymethyl cellulosecrosslinked gelatin–PEG composite hydrogel fibers for wound dressings. Carbohydr Polym 137:508–514
Kołodziejska I, Kaczorowski K, Piotrowska B, Sadowska M (2004) Modification of the properties of gelatin from skins of Baltic cod (Gadus morhua) with transglutaminase. Food Chem 86:203–209
Wang X, Zhang D, Wang J, Tang R, Wei B, Jiang Q (2016) Succinyl pullulan-crosslinked Carboxymethyl chitosan sponges for potential wound dressing. Int J Polym Mater Polym Biomater 66:61–70. https://doi.org/10.1080/00914037.2016.1182912
Autissier A, Letourneur D, Visage CL (2006) Pullulan-based hydrogel for smooth muscle cell culture. Wiley InterScience 82A:336–342. https://doi.org/10.1002/jbm.a.30998
Rekha MR, Sharma CP (2007) Pullulan as a promising biomaterial for biomedical applications: a perspective. Trends Biomater Artif Organs 20:116–121
Chaouat M, Visagea CL, Autissiera A, Chaubet F, Letourneur D (2006) The evaluation of a small-diameter polysaccharide-based arterial graft in rats. Biomaterials 27:5546–5553
Shingel KI (2004) Current knowledge on biosynthesis, biological activity, and chemical modification of the exo-polysaccharide, pullulan. Carbohydr Res 339:447–460
Shitole AA, Raut PW, Sharma N, Giram P, Khandwekar AP, Garnaik B (2019) Electrospun polycaprolactone/hydroxyapatite/ZnO nanofibers as potential biomaterials for bone tissue regeneration. J Mater Sci Mater Med 30:51–68
Giram PS, Shitole A, Nande SS, Sharma N, Garnaik B (2018) Fast dissolving moxifloxacin hydrochloride antibiotic drug from electrospun Eudragit L-100 nonwoven nanofibrous Mats. Mater Sci Eng C 92:526–539
Shitole AA, Giram PS, Raut PW, Rade PP, Khandwekar AP, Sharma N, Garnaik B (2019) Clopidogrel eluting electrospun polyurethane/polyethylene glycol thromboresistant, hemocompatible nanofibrous scaffolds. J Biomater Appl 18:1–21
Raut PW, Shitole AA, Khandwekar A, Sharma N (2019) Engineering biomimetic polyurethane using polyethylene glycol and gelatin for blood-contacting applications. J Mater Sci 54:10457–10472
Shinde DB, Koratkar SS, Sharma NE, Shitole AA (2016) Antioxidant activity and antiproliferative action of methanolic extract of liquorice (Glycyrrhiza glabra) in HepG2 cell line. Int J Pharm Pharm Sci 8:293–298
Qian Y, Qi M, Zheng L, King MW, Lv L, Ye F (2016) Incorporation of Rutin in electrospun pullulan/PVA nanofibers for novel UV-resistant properties. Materials 9:504
Chandy T, Sharma CP (1990) Chitosan - as a biomaterial. Biohat., art. Cells. Art Org 18:1–24
Pan JF, Liu NH, Sun H, Xu F (2014) Preparation and characterization of electrospun PLCL/ Poloxamer nanofibers and dextran/gelatin hydrogels for skin tissue engineering. PLoS One 9:e112885
Ninan N, Forget A, Shastri VP, Voelcker NH, Blencowe A (2016) Anti-bacterial and anti-inflammatory pH-responsive tannic acidcarboxylated agarose composite hydrogels for wound healing. ACS Appl Mater Interfaces 8:28511–28521. https://doi.org/10.1021/acsami.6b10491
Ninan N, Muthiah M, Park IK, Elain A, Thomas S, Grohens Y (2013) Pectin/carboxymethyl cellulose/microfibrillated cellulose composite scaffolds for tissue engineering. Carbohydr Polym 98:877–885
Liu J, Carrasco GC, Cheng F, Xu W, Willfor S, Syverud K, Xu C (2016) Hemicellulose-reinforced nanocellulose hydrogels for wound healing application. Cellulose 23:3129–3143
Burkatovskaya M, Tegos GP, Swietlik E, Demidova TN, Castano AP, Hamblin MR (2006) Use of chitosan bandage to prevent fatal infections developing from highly contaminated wounds in mice. Biomaterials 27:4157–4164
Kenawy ER, Kamoun EA, Mohy Eldin MS, El-Meligy MA (2013) Physically crosslinked poly(vinyl alcohol)-hydroxyethyl starch blend hydrogel membranes: synthesis and characterization for biomedical applications. Arab J Chem 7:372–380. https://doi.org/10.1016/j.arabjc.2013.05.026
Kim JO, Park JK, Kim JH, Jin SG, Yong CS, Li DX, Choi JY, Woo JS, Yoo BK, Lyoo WS, Kim JA, Choi HG (2008) Development of polyvinyl alcohol–sodium alginate gel-matrix-based wound dressing system containing nitrofurazone. Int J Pharm 359:79–86
Hwang MR, Kim JO, Lee JH, Kim Y, Kim JH, Chang SW, Jin SG, Kim JA, Lyoo WS, Han SS, Ku SK, Yong CS, Choi HG (2010) Gentamicin-loaded wound dressing with polyvinyl alcohol/dextran hydrogel: gel characterization and in vivo healing evaluation. AAPS PharmSciTech 11:1092–1102
Acknowledgements
The authors would sincerely like to thank Symbiosis School of Biological Sciences (SSBS) and Symbiosis Center for Research and Innovation (SCRI), Symbiosis International (Deemed University) (SIU), Lavale, Pune, India for providing the research grants. The authors would like to thank Dr. Vinaykumar Rale (Director, SSBS) for providing Pullulan for the current research work. Ajinkya A. Shitole and Meghna Baruah kindly acknowledge SCRI, SIU for providing the Senior Research fellowship.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there are no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shitole, A.A., Raut, P.W., Khandwekar, A. et al. Design and engineering of polyvinyl alcohol based biomimetic hydrogels for wound healing and repair. J Polym Res 26, 201 (2019). https://doi.org/10.1007/s10965-019-1874-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10965-019-1874-6