Abstract
Psychiatric disorder prevalence has been shown demonstrably higher among justice-involved adolescents than youth in the general population. Yet, among arrested juveniles, little is known regarding racial/ethnic differences in disorder prevalence, the role of trauma exposure in the diagnosis of behavioral disorders, or subsequent psychiatric treatment provided to adolescents with such diagnoses. The current study examines racial/ethnic disparity in psychiatric diagnoses and treatment of behavioral disorders associated with delinquency, controlling for traumatic experiences, behavioral indicators, and prior offending among serious juvenile offenders. Logistic regression is employed to explore the racial/ethnic disproportionality in behavioral disorder diagnoses and psychiatric treatment provision among 8763 males (57.7 % Black, 11.8 % Hispanic) and 1,347 females (53.7 % Black, 7.6 % Hispanic) admitted to long-term juvenile justice residential placements in Florida. The results indicate Black males are 40 % more likely, and Black females 54 % more likely to be diagnosed with conduct disorder than Whites, even upon considerations of trauma, behavioral indicators, and criminal offending. Black and Hispanic males are approximately 40 % less likely to be diagnosed with ADHD than White males, with no racial/ethnic differences for females. Importantly, Black males are 32 % less likely to receive psychiatric treatment than White males, with no differences between White and Hispanic males, or any female subgroups. Traumatic exposures increased the odds of oppositional defiant disorder and ADHD, but not conduct disorder for males, though adverse childhood experiences were unrelated to behavioral disorder diagnoses among females.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In October 2015 the Federal Advisory Committee on Juvenile Justice (FACJJ) supported by the Office of Juvenile Justice and Delinquency Prevention (OJJDP), put forth policy and research recommendations to President Obama, Congress, and OJJDP Administrator Robert Listenbee calling for focused research on disproportionality in the diagnosis of youth where trauma exposure/symptomology is overlooked in favor of a behavioral disorder more closely associated with delinquency (FACJJ 2015). One question, which the current study seeks to address, is whether racial/ethnic disproportionality exists in the diagnoses of behaviorally defined mental health disorders associated with antisocial and delinquent behavior, irrespective of similar behavioral, offending, and traumatic exposure histories. Stated differently, do Black and/or Hispanic juvenile offenders receive behavioral diagnoses (such as conduct disorder) at greater rates than White youth, controlling for adverse childhood experiences, criminal offending and juvenile justice system placement history, individual risk factors, and other mental health risks? A second but equally important question we examine is the extent to which there are differences across racial/ethnic groups with respect to psychiatric treatment provision, including psychotropic medication prescription, net of those controls?
Examining whether such disproportionality exists has developmental significance as adolescents receiving differential diagnoses under similar individual and environmental contexts places youth on disparate pathways with regard to potential life chances and subsequent criminal offending. The correlates attributed to a youth’s antisocial behavior and the treatment of those suspected underlying causes has the potential to alter these trajectories positively (if accurate) or negatively (in instances of misdiagnoses, attributing behavior to conduct versus emotional problems, or internal attribution versus contextually-driven attribution to behavior). Further, the subsequent differences in (or no) psychiatric treatment stemming from differential diagnoses may further exacerbate developmental risk if they do not address the true underlying sources of antisocial behavior. If adolescent offenders who need treatment services are not afforded them, it stands to reason that they would be at heightened risk of experiencing additional adversity such as continued offending as well as diminished success in other key life domains, principally education and employment, that are critical for positive development and success over the life-course. In short, the psychiatric diagnoses ascribed to at-risk adolescents and the associated treatment has both short- and long-term ramifications for their development and affects the likelihood of actualizing future potential.
We examine these questions among a sample of serious offenders admitted to long-term juvenile justice residential commitment facilities. This population is particularly relevant as psychiatric disorder prevalence has been demonstrated highest among long-term incarcerated youth in comparison to general population youth—even when compared to offenders placed in short-term detention centers upon arrest (Karnik et al. 2009). Offenders with behavioral disorders are a policy-relevant subgroup as such disorders remain the most prevalent over time and are not limited to adolescence (Teplin et al. 2012). Additionally, conduct disorder is highlighted, as it is required prior to a diagnosis of adult antisocial personality disorder—no other adult personality disorder requires a childhood diagnosis (American Psychiatric Association 2013; see also Lahey et al. 2005).
Racial/Ethnic Disparities
Prior work has indicated racial/ethnic disparities in police arrest decisions (Kochel et al. 2011; Stevens and Morash 2015), prosecutorial charging practices (Wu 2016), and judicial sentencing practices (Mitchell 2005)—all of which point to Black and Hispanic disadvantage. Additionally, race has been shown to play a role in representation across stages/levels of juvenile justice system involvement, including secure facilities (Neighbors et al. 2003; Piquero 2008; Sickmund and Puzzanchera 2014). Black males have a 32 % chance of serving time in prison during their lives, in comparison to 17 % for Hispanic males, and only 6 % for White males (Vaughn et al. 2008). Bias in the diagnosis and treatment of Black youth has been implicated as a possible explanation for their disproportional involvement in both special education services for emotional and behavioral disturbance and juvenile justice settings (Gudiño et al. 2008; Losen and Orfield 2002).
In contrast to community samples, limited research has examined the overlap of psychiatric disorders and race/ethnicity among offending groups (Ricks and Louden 2016; but see Abram et al. 2003; Becker et al. 2012). Additionally, there is a scarcity of literature specific to the racial/ethnic disparities in mental health diagnosis in favor of behavioral disorders associated with delinquency among serious juvenile offenders while controlling for traumatic exposure histories, behavioral indicators, and official criminal history (El Sayed et al. 2015). With rare exceptions (cf. Dalton et al., 2009), prior work most often reports prevalence of mental health needs across race/ethnicity, with limited control for trauma exposure, offending, behavioral, and cognitive/attitudinal indicators, and few report on specific diagnoses rather than mental illness overall or counts of symptom expression (for exceptions see Teplin et al. 2002; Teplin et al. 2012; Wasserman et al. 2002).
Several prior studies have examined identification or receipt of mental health treatment services by race/ethnicity among adolescents in the juvenile justice system. In an analysis of 473 system-involved juveniles (predominately detention and probation cases), Rawal et al. (2004) found that while Black youth evidenced higher levels of mental health needs, they were provided lower rates of mental health services. This echoes other work finding racial disparities (Garland et al. 2005; Herz 2001), including findings that White youth needing treatment are approximately twice as likely to be detected as needing mental health services than Black youth needing treatment (Teplin et al. 2005). However, examining 33,000 juvenile court-referred youth, Breda (2003) found legal status and offense type had greater impact on treatment referrals than race. Dalton et al. (2009) analyzed 937 males in long-term secure juvenile justice facilities (more similar to the current study sample) finding White youth three to five times more likely to be designated with serious mental health status compared to Black youth, even after controlling for Massachusetts Youth Screening Instrument (MAYSI-II) indications for further assessment and prior mental health treatment history. Racial disparities in mental health service utilization were not attributable to ethnic differences in prevalence, severity of symptoms, or functional impairment among over 1,000 youth in the Patterns of Care study (Gudiño et al. 2008).
Prior work has promulgated two seemingly contradictory assumptions of racial/ethnic diagnostic differences (Neighbors et al. 1989). The first assumption is that members of different race/ethnic groups present similarly, and stereotypes held by clinicians are the primary reason for different diagnoses/prevalence of diagnoses. The second is that individuals of different race/ethnicities present different psychopathology but diagnosticians incorrectly assume they are the same. In this instance, clinicians are unaware of—or insensitive to—cultural differences in the manifestations of the same disorder displayed by different racial groups (see also Kunen et al. 2005). Several studies have shown prevalence of schizophrenia to be higher among Blacks than Whites (Neighbors et al. 1999, 2002, 2003; Pavkov et al. 1989), yet Blacks with bipolar disorder more often have symptoms of hallucinations and delusions, which are incorrectly assumed indicative of, and misdiagnosed as, schizophrenia resulting in “under-diagnosis” of affective disorders among Blacks, and an “over-diagnosis” of schizophrenia (Neighbors et al. 1989). Any racial differences in disorder expression contradicts the position that “mental disorders and their corresponding socially constructed diagnostic categories are discrete, distinguishable, and invariant across racial and ethnic groups” (Neighbors et al. 1999, p. 609).
The effects of racial stereotypes and attributions has been demonstrated where physicians’ assessment of patient intelligence, feelings of affiliation toward the patient, and physician beliefs regarding the patient’s likelihood of risky behavior and compliance with medical advice were associated with patient race (Van Ryn and Burke 2000). This line of research is similar to that of teacher ratings of Black students as less favorable on items measuring behavior, motivation to learn, classroom performance, as well as actually treating Black students worse than White students (Partenio and Taylor 1985; Plewis 1997; but see Chang and Sue 2003; Hosterman et al. 2008), and rating Black children higher on under-controlled and overall behavioral problems (Epstien et al. 1998; Reid et al. 1998). Clinician attributions regarding clients has been shown to influence whether misbehavior is construed as resulting from conduct problems or emotional disorders (Snowden 2003), and in other research in a sample of probation officers Bridges and Steen (1998) found officers’ reports more often included negative internal attributes to Black offenders and negative external attributions to White offenders. Psychiatrists and residents rating identical data on patients, with the exception of race, has shown that experts see Blacks as being less able to benefit from therapy based on stereotypes regarding their level of introspection and sophistication (Geller 1988; see also Dana 2012). Such stereotyping, or even cultural issues such as communication misunderstandings and subtleties, may lead to over-pathologizing of Blacks and Hispanics (Dana 2012; Neighbors et al. 2003; Whaley 2002). Additionally, the process that clinicians use to link symptom observations to diagnoses has been found to differ between Black and White patients; differences which could not be accounted for by racial differences in symptom rates (Neighbors et al. 2003). Consistent with this is the hypothesis offered by Dalton et al. (1999) where “providers attributed symptom expression to behavioral problems and not emotional problems more often” in Black than White youth (p. 204). Further, delinquent and criminal behavior among Blacks and Hispanics is more likely attributable to “innate characteristics or environments that are not amenable to treatment” (Mansion and Chassin 2016, p. 238; see also Fitzgerald 1996).
In total, these findings suggest that racial/ethnic disparities in psychiatric disorder diagnoses do exist and cannot simply be explained by differences in prevalence of such disorders. Yet, such disparities in both offending and specific disorder diagnoses may be influenced by factors outside the youth’s control, namely in their environment and the potentially adverse experiences that youth experience in such environments. How these adverse experiences relate to mental health are an important consideration, to which we now turn our attention.
The Link Between Adverse Childhood Experiences (ACE) and Mental Health
Juvenile justice-involved youth have demonstrated higher rates, and multiple exposures of childhood maltreatment, abuse, and neglect, as well as mental health problems than the general population of youth (Abram et al. 2004; Dierkhising et al. 2013). The negative repercussions of childhood maltreatment on health, education, and later-life outcomes, including crime and delinquency, are well documented (Godinet et al. 2014; Widom 1989a, b). Adverse abuse exposures and maltreatment are relevant to the current study as youth with physical and sexual abuse are at highest risk of psychiatric disturbance (Ackerman et al. 1998; see also Johnson et al. 1999). Further, prior research suggests that males with both physical and sexual abuse histories evidence the highest number of behavior disorders (Ackerman et al. 1998). Additionally, adolescents with more severe oppositional defiant disorder and conduct disorder tend to be reared in contexts including greater exposure to child abuse and neglect, domestic violence, parental substance abuse, and criminality, and separation and divorce (Boden et al. 2010; Lynskey et al. 1994; McCabe et al. 2005; Odgers et al. 2007).
One measure of cumulative childhood traumatic stress exposure prominent in medical research (Felitti et al. 1998) and recently applied in criminological work (Baglivio et al. 2014) is the Adverse Childhood Experiences (ACE) score. The ACE score is a summation of ten specific binary trauma/abuse exposures, prior to 18 years of age, including: emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect, family violence, household substance abuse, household mental illness, parental separation or divorce, and household member incarceration (Centers for Disease Control and Prevention 2016). Research on over 15,000 adult health maintenance organization patients indicated that those with five or more adverse childhood experiences indicators evidenced three times the rate of psychotropic medication prescription as patients with an ACE score of four or less (Anda et al. 2007). The strong dose–response adverse childhood experiences-psychotropic medication link has implications for the need to understand the deleterious effects of trauma and early origins of the mental illness for which the medications are prescribed (Anda et al. 2007). Adverse childhood experiences such as parental criminality, substance abuse, mental illness, and family conflict, as well as child abuse and neglect have been found to increase the risk of conduct disorder (Kazdin 1997). Adverse childhood experiences contribute to deficits in attachment and regulation of mood and affect (Anda et al. 2006). Those with four or more adverse childhood experiences have been observed to be at increased risk of panic reactions, depression, anxiety, hallucinations, somatic disturbances, difficulty controlling anger, and a host of other health and behavioral outcomes (Anda et al. 2006).
Recent work examining ACE exposure among juvenile offenders demonstrates consistency with earlier studies on childhood maltreatment in that offenders evidence substantially more traumatic exposures than the general population (Baglivio et al. 2014; Cannon et al. 2016; Evans-Chase 2014; Grevstad 2010). Baglivio et al. (2014) analysis of over 64,000 juvenile offenders showed that the prevalence of each of the ten adverse childhood experience indicators was similar for males and females, with the exception of sexual abuse, where the female rate was 4.4 times higher (Cohen’s d = .92). However, although indicators had similar prevalence individually, only 1.8 % of the females reported no traumatic exposures compared to 3.1 % of the males, and 27.4 % of the males and 45.1 % of the females reported five or more adverse childhood experiences. Similar rates of exposure by sex to each of 19 different trauma types were found in prior studies of justice-involved adolescents, though females in those studies also evidenced higher rates of sexual abuse and sexual assault (Dierkhising et al. 2013; see also Cauffman et al. 1998). These sex differences in exposures, and more importantly in the extent of exposure to multiple trauma types, necessitates sex-specific analyses in examining trauma and mental health diagnoses and symptomology.
Mental health issues can have an effect on juvenile reoffending as well (Vermeiren et al. 2002; Wierson and Forehand 1995). For instance, a previous conduct disorder diagnosis, suicide attempt, or a previous diagnosis for attention-deficit hyperactivity disorder may influence reoffending among youth (Mallett et al. 2013). Additionally, psychopathy (Edens et al. 2007; Tengström et al. 2000), violent criminal history, and antisocial personality traits (Collins 2010) have been found to be among the most important predictors of violent reoffending patterns in several prior studies. Substance abuse and conduct disorder have been demonstrated to predict recidivism among White males, whereas ADHD, severity of the presenting offense, age at first conviction, and not having a depressive disorder predictive of Black male recidivism (Becker et al. 2012), illustrating the importance of racial subgroup analyses. Further, untreated oppositional defiant disorder may develop into conduct disorder, which, if left untreated, may lead to adult antisocial personality disorder (Kazdin 1997; Robbins 1978; Searight et al. 2001). Psychiatric disorders are likely to persist among juvenile offenders as they often lack substantial protective factors to ameliorate risks for disorders, such as childhood maltreatment, family dysfunction, criminality, substance abuse, and neurological deficits (Teplin et al. 2012). These factors make the provision of needed psychiatric treatment paramount; with racial/ethnic disparities in such treatment provision potentially confounding recidivism outcomes.
The role of context/environment in psychiatric disorders is also important. Prior work has found higher rates of externalizing behaviors among Black youth in comparison to White youth (Vaughn et al. 2008). However, such behavior represents pathology only when the behaviors in question are symptomatic of an underlying condition within the individual, but not when it is relative/reactionary to the environment in which the youth is an actor (APA 2013). If behaviors such as stealing, gang-involvement, and even weapon-carrying and aggression are common features of the youth’s context—and in some cases may be both normative and necessary for survival in particular contexts (Anderson 1999), one may question the appropriateness of psychiatric diagnoses (Hsieh and Kirk 2003; Richters and Cicchetti 1993). As Hsieh and Kirk (2003, p. 879) have noted, “A systemic failure to distinguish mental disorders from non-disordered problems-in-living would contribute to heterogeneity within the diagnostic category, thwart the progress of knowledge development, and compromise the validity of the psychiatric classification system.” This issue is to the detriment of Black and Hispanic youth who tend more often than not to reside in more disadvantaged contexts compared to Whites as diagnostically there is no valid/reliable way to differentiate disordered behavior from environmentally caused behavior (Brody et al. 2003; Hsieh and Kirk 2003). Some have argued that racism and poverty (and their combination) constitutes cumulative, pervasive stress akin to that endured by survivors of war or torture (Dana 2012). We argue that cumulative exposures to multiple trauma types (as per the ACE score) can itself be considered a type of disadvantaged context. Prior work has argued that post-traumatic stress disorder (PTSD) diagnosis is often missed as per the DSM criteria, which do not include repeated exposure to trauma. Those who have repeatedly been subjected to racism and oppression, repeated witnessing of violence or violent victimization, and even poverty, or trauma from immigration/refugee experiences may receive inappropriate treatment due to improper diagnosis (Worrell and Remer 2003; Velasquez et al. 1993).
Current Study
The current study examines disproportionality in psychiatric diagnoses across race/ethnicity in a sample of serious adolescent offenders admitted to long-term juvenile justice residential programs. Emphasis is placed on diagnoses in favor of behavioral disorders associated with delinquency while taking into account cumulative traumatic exposures. Additionally, the current study examines the provision of psychiatric treatment, which includes the prescription of psychotropic medications, across race/ethnicity, net of criminal history, individual, and mental health risk indicators. We hypothesize that a majority of youth will be diagnosed with conduct disorder, regardless of race/ethnicity, as they have committed serious illegal behaviors and have penetrated deep into the juvenile justice system (Frick 2006). However, we also hypothesize disparity, with Black and Hispanic youth having higher prevalence of the more serious conduct disorder diagnosis, while White youth will have higher rates of the less serious oppositional defiant disorder, as well as higher rates of non-behavioral disorders. Additionally, based on the extant literature, White youth are expected to receive higher rates of psychiatric treatment provision than Black and Hispanic youth.
In short, the importance of the current study emphasizes prior sentiments that “there is little argument that, independently, race and mental health are two of the most important issues in the juvenile justice system…yet, the relationship between them has not received much empirical scrutiny” (El Sayed et al. 2015, p. 3). In so doing, the study adds to the nascent research base on this issue using a sample of serious adolescent offenders who are at a critical juncture in their development where specific interventions and treatment may help them move away from a persistent offending trajectory and onto a prosocial one that offers opportunities for success across multiple life domains throughout the life course.
Methods
Data
To examine the linkages between race and mental health diagnoses, we use archival data records from the Florida Department of Juvenile Justice (FDJJ). This agency maintains a centralized database, the Juvenile Justice Information System, which contains complete demographic, offense, placement, and risk assessment history data for all youth referred for delinquency (equivalent to an adult arrest). The individual-level measures included in the current study were taken from the Community Positive Achievement Change Tool (C-PACT) risk/needs assessment administered to all youth prior to admission to a juvenile justice residential program, as well as the Residential Positive Achievement Change Tool (R-PACT) risk/needs assessment administered to each youth within 30 days of admission to a long-term residential program (both assessments are described below). Data for this study are inclusive of all youth within Florida admitted to a juvenile justice residential commitment program from December 1, 2011 to December 1, 2014 that were assessed with both the community version risk assessment (C-PACT) and the residential version risk assessment (R-PACT; n = 10,218). Of note, 20 youth were not assessed with the full community version risk assessment prior to placement, and 62 youth did not have records of a residential version risk assessment during residential placement, and were excluded. Additionally, 26 youth were classified as “other” race/ethnicity, and were excluded, resulting in a final sample of 10,110 serious offenders, representing 98.9 % of all youth admitted to residential programs in Florida during the study period.Footnote 1
The community version risk assessment (C-PACT) is the validated risk/needs assessment administered to all juveniles arrested in Florida (Baglivio 2009; Baglivio and Jackowski 2013). There is both a pre-screen and a full community version risk assessment that produce identical overall risk to re-offend scores (low, moderate, moderate-high, and high risk). The tools differ in that the full assessment contains approximately 80 additional items that do not contribute to the overall risk score, but do provide additional information for case planning. Only the full community version risk assessment contains the necessary information to create ACE scores (therefore youth receiving only a pre-screen PACT assessment were not included in the current study).Footnote 2 The full community version risk assessment administered just prior to residential placement was used in the current study to obtain adverse childhood experiences (ACE scores; described below).
Youth placed in juvenile residential commitment programs in Florida are assessed with a residential version risk assessment (the R-PACT). Initial assessment occurs within 30 days of admission to assist with individualized treatment/case plan development for each youth. Similar to the community version risk assessment described above, this residential youth risk/need assessment tool assesses youth for risk and protective factors across 12 domains (the same domains as the community tool described in endnote # 2). The initial residential version assessment was used to garner all mental health diagnosis and youth-level attributes other than the ACE scores. Both ACE scores (from the community version assessment) and youth-level attributes (from the residential version assessment) were taken from the assessments to be used as prominent risk factor controls in the examination of racial/ethnic differences in mental health diagnoses among youth in residential placement.Footnote 3
Measures
Mental Health Diagnoses
Every youth placed in a Florida juvenile justice residential program must first receive a comprehensive evaluation conducted by a licensed mental health practitioner. These providers are licensed (or clinically supervised by licensed) individuals contracted by the Florida Department of Juvenile Justice to conduct these services and are located throughout Florida. A comprehensive evaluation is the “gathering of information addressing physical health, mental health, substance abuse, academic, educational, or vocational problems of a youth for whom a residential commitment disposition is anticipated” (F.A.C. 63d-9 2016, p. 1). In addition to psychosocial histories, psychological testing results, and treatment and placement recommendations, the comprehensive evaluation providers include mental health diagnoses in their reports for each youth. These formal diagnoses are used to respond to a specific residential version risk assessment item in the mental health domain where the assessor indicates all diagnoses which apply. The following options are captured by that item and are examined in the current study: no diagnosis, adjustment disorder, anxiety disorder (including PTSD), attention deficit/hyperactivity (ADHD), conduct disorder, eating disorders, intermittent explosive disorder, mood disorder (including depression and bipolar), oppositional defiant disorder, personality disorder, and schizophrenia or psychotic disorder. Each diagnosis is dichotomous (either the youth has the formal diagnosis = 1 or does not = 0), with no indication of severity. To reiterate, the mental health diagnostic information used in the current study is based on the diagnoses made by the Florida Department of Juvenile Justice comprehensive evaluation providers, all licensed mental health providers, and captures those diagnoses made in the community prior to the youth’s admission to the residential program (and therefore are not manifestations of reactions to the placement setting).Footnote 4
While the current study reports prevalence by race/ethnicity for several diagnostic categories (mentioned above), the multivariate analysis focuses on conduct disorder, oppositional defiant disorder, and attention-deficit hyperactivity disorder. Both conduct disorder and oppositional defiant disorder are behavioral diagnoses closely associated with delinquency. Conduct disorder and oppositional defiant disorder can present similarly (see below), where a level of aggression and cruelty distinguishes the two from one another. Knowledge of racial disparities across those diagnoses among serious juvenile offenders, controlling for traumatic exposure, criminal offenses, inclination to physical aggression, and problem behaviors will advance our understanding of these relationships and, in turn, bear on policy/practice matters. Multivariate analyses elaborate on attention-deficit hyperactivity disorder as it was the second most prevalent diagnosis among the male offenders (after conduct disorder), and is associated with acting-out and delinquent behavior (Wasserman et al. 2000). These three psychiatric disorders are commonly considered as externalizing disorders in prior work (e.g., Gudiño et al. 2008), and the current study follows that precedent.
Conduct disorder (CD) may be diagnosed when a youth has a repetitive and persistent pattern of behavior violating the rights of others or societal rule/law (American Psychiatric Association, APA 2013). CD is defined entirely by behavioral symptoms (Burke et al. 2002). The behavioral disturbances must cause clinically significant impairment in social, academic, or occupational functioning. Three or more of the DSM-5-identified behavior patterns in the past 12 months must be evident, with at least one evident in the past 6 months.
Oppositional defiant disorder (ODD) may be diagnosed if the child’s behavior problems do not meet criteria for CD, but involve a pattern of angry/hostile, defiant, irritable, or vindictive behavior(s). ODD-diagnosed youth may typically blame others rather than take/admit responsibility for their misbehavior. Similarly to CD, behavior must be a demonstrated pattern, lasting at least six months during which four or more of DSM-5-identified specific behaviors are present.
Youth with ODD present as thriving on deliberately annoying other people. As with CD, ODD is appropriately diagnosed only when behavioral patterns cause problems in social, academic, or occupational functioning. ODD and CD differ, primarily, in that the behavioral patterns of ODD will not evidence the level of cruelty present in those with CD, and, though argumentative, youth with ODD diagnoses do not evidence the physical aggression of youth with CD (Searight et al. 2001). Of note, and as required by the DSM, ODD and CD diagnoses are considered mutually exclusive.
Attention-deficit hyperactivity disorder (ADHD) may be diagnosed when symptoms of inattention and/or hyperactivity-impulsivity are present for more than six months and occur regularly in at least two different settings (such as home and school; APA 2013). Symptoms include: inability to sit still; listening problems; easily distracted; problems completing tasks; making careless mistakes; inability to follow instructions; organizational problems; forgetfulness; excessive talking; tendency to interrupt others; and impatience. Prior work suggests features of ADHD such as “disinhibition, inattention, and distractibility should be distinguished from lying, serious aggression and illegal behaviors” (Searight et al. 2001, p. 1582).
Psychiatric treatment
Whether the youth is receiving psychiatric treatment within the residential facility is captured by the residential version risk assessment (coded yes = 1, no = 0). This measure of receipt of psychiatric treatment allows us to examine racial/ethnic differences in youth receiving such treatment for the mental health diagnostic measures described above and includes the prescription of psychotropic medication. To reiterate, this measure is a simple yes/no indicator for the youth receiving treatment (which may include psychotropic medication) and does not include information related to the type, frequency, or duration of such treatment or medication. The measure does distinguish youth who are receiving treatment provided by a licensed psychiatrist, as opposed to a therapist, counselor, psychologist, or other credentialed mental health practitioner (youth receiving psychiatric treatment would also be receiving services from those other practitioners). Any youth receiving prescribed psychotropic medications would be considered an affirmative (yes response) under this measure. A youth receiving the Florida Department of Juvenile Justice-required therapy, mental health group treatment, individual counseling (with a therapist), and group counseling services within residential programs would not be included, unless that youth was also seen by a psychiatrist.
Key Independent Variables
The following individual-level attributes were included in the current study and grouped into domains to enable examination of the importance of each domain in distinguishing psychiatric diagnoses. We group measures into demographic, criminal history, individual risks, and mental health risks. Race/ethnicity is provided by the Florida Department of Juvenile Justice information system. All additional items (with the exception of the ACE score) were collected by the residential version risk/needs assessment administered within 30 days of residential admission. The ACE score was created from the full community version risk/needs assessment conducted prior to residential placement. Measures were selected based on use of similar metrics in prior work emphasizing race/ethnicity and psychiatric disorders among adolescents (e.g., Boden et al. 2010; Frick 2006; Teplin et al. 2012; Thomas et al. 1999), with an emphasis being placed on those including juvenile justice youth and behavioral disorders. Additionally, we include measures associated with both child-onset (such as dispositional and contextual risks) and adolescent-onset (such as peer associations) behavioral disorders (Dodge and Pettit 2003; Frick 2004, 2006).
Demographics
All analyses presented in the current study are sex-specific (male-only and female-only models). Race and ethnicity were included as demographic controls. Race/ethnicity was measured using a set of dichotomous variables that included Black (yes = 1, no = 0), Hispanic (yes = 1, no = 0), with White (non-Hispanic) being the reference group.Footnote 5
Criminal History Measures
All criminal history measures were taken from the residential version risk/needs assessment. The criminal history items are official measures of delinquency and are automated from the Florida Department of Juvenile Justice information system, meaning they are accurate and reliable indicators of system-involvement and not self-reported or dependent on youth recall or case file reviews. Criminal history items are essential for inclusion as early-onset, more extensive system placements, and more severe offending would arguably differentiate CD from ODD and ADHD diagnoses (APA 2013). Additionally, prior research has indicated juvenile justice placements may exacerbate traumatic stress symptoms, and that placements themselves could be considered as traumatic exposures (Ford et al. 2007; Hennessey et al. 2004), meaning the significance of placement indicators in prediction of diagnoses may be indicative of the significance of trauma in such diagnoses.
Age at First Offense
The age at which the youth was first arrested was captured as 12 and under, 13 to 14, 15, 16, and over 16 years of age (coded 1–5, respectively), where higher values indicate a later age of official criminal onset. The age at first arrest categories are those captured by the residential version risk/need assessment.
Prior Misdemeanors
The youth’s official misdemeanor arrest history was captured according to the residential version assessment categorizations as none or one, two, three or four, and five or more (coded 0–3), where higher values indicate a greater number of misdemeanors that resulted in diversion, adjudication withheld, adjudication, deferred prosecution, or referral to adult court.
Prior Felonies
The youth’s felony arrest history was captured as none, one, two, or three or more felonies (coded 0–3). Higher values indicate a more extensive history of felony arrests that resulted in diversion, adjudication withheld, adjudication, deferred prosecution, or referral to adult court.
Prior Against-Person Felony
The youth’s history of violent felony arrests was captured as none, one or two, or three or more against-person felony arrests (coded 0–2). Higher values indicate a greater extent of violent felony arrests that resulted in diversion, adjudication withheld, adjudication, deferred prosecution, or referral to adult court. Against-person felonies involve physical force or physical harm to another person and includes those offenses defined by the Florida Department of Law Enforcement (FDLE) as violent felonies.
Felony Sexual Offending
The total number of arrests for a felony sexual offense or involving sexual motivation including carnal knowledge, child molestation, communication with a minor for immoral purpose, incest, indecent exposure, indecent liberties, promoting pornography, rape, sexual misconduct, and voyeurism felonies were included. The youth’s extent of felony sexual offending was captured as none, one felony sexual offense, or two or more felony sexual offenses (coded 0–2, respectively), where higher values indicate a greater history of felony sexual offending arrests that resulted in diversion, adjudication withheld, adjudication, deferred prosecution, or referral to adult court.
Prior Detention Stays
The youth’s number of prior placements in juvenile detention centers where the youth was held for at least 48 h was captured by the residential version risk/needs assessment. Detention stay history is categorized as none, one, two, or three or more prior detention placements (coded 0–3), where higher values indicate a greater extent of detention placement history.
Residential Placement History
The youth’s history of disposition to a long-term juvenile justice residential commitment facility was captured as one, or two or more placements (coded 1–2). Higher values indicate the youth has more prior residential commitment placements. As all youth in the current study were currently placed in residential commitment programs (the study sample), no youth lack history of residential placement. Essentially, this measure differentiates those for whom the current residential commitment placement is their first commitment from those who have prior residential commitment placements.
Individual Risk Factors
The individual risk factors selected were based on each items relevance to a diagnosis of CD, ODD, or ADHD, or indication in prior work of individuals with such characteristics at increased likelihood for such diagnoses (as reviewed above; e.g., academic functioning deficits, social functioning impairments).
Behavioral Special Education Needs
Youth who have a history of being considered as “socially maladjusted” and having behavioral special education needs by an educational institution were coded 1 (else = 0). As the current study used the initial residential version risk/needs assessment, these needs must have been present in community school records to receive this designation (the classification was not made by the residential facility staff, but reflects prior school history).
Learning Special Education Needs
Youth with a prior history of designation by educational institutions as having a learning disorder or learning disability were classified as having learning special education needs (coded 1, else = 0). These youth typically have difficulties in listening, speaking, reading, writing, reasoning, or mathematical abilities. As with behavior special education needs described above, this classification reflected prior school history, and was not based on assessments made during residential placement.
Intellectual Disability
Youth with impaired intellectual and adaptive functioning were classified as having intellectual disability (coded 1, else = 0). These youth have a documented (by formal psychological evaluation) full scale intelligence quotient (IQ) under 70, whose level of cognitive impairment and related functional limitations impede their ability in daily living.
Previous School Suspensions/Expulsions
Whether the youth had ever been suspended or expelled from school, and the age at first suspension/expulsion were captured as 5–9 years old at first suspension/expulsion, 10–13 years of age, 14–15, 16–18, or never suspended (coded 1–5, respectively). Lower values indicate greater risk as these youth were suspended/expelled and at younger ages than youth with higher values on this measure.
School Conduct
The youth’s engagement in school prior to residential placement was captured as graduated/GED, enrolled full time, enrolled part time, suspended from school at the time of residential placement, dropped out of school, or expelled from school at the time of residential placement (coded 0–5). Higher values indicate a more negative school situation at the time of residential placement.
Alcohol Use
The youth’s prior alcohol use was captured as no prior use, prior use, or prior use which caused problems in specific life domains (coded 0–2). The life domains which alcohol use may have disrupted include: education, causing family conflict, interfering with maintaining pro-social friendships, causing health problems, contributing to criminal behavior, needing increasing amounts (tolerance), or experiencing withdrawal problems.
Drug Use
Similar to alcohol use, the youth’s drug use history was captured as no history of drug use, drug use, or drug use where the use caused problems in specific life domains (coded 0–2). The life domains potentially affected by drug use were the same as those for alcohol use.
Runaway History
The youth’s history of running away from home or being kicked out of the house where the youth did not voluntarily return within twenty-four hours was captured as no history, one to five instances, or over five instances (coded 0–2). Higher values indicate a greater extent of running away or getting kicked out of the home.
ACE Score
Although created to classify youth according to levels of risk to re-offend, the community version risk/needs assessment captures items related to adverse childhood experiences (ACE). These items were used to create ACE scores for each youth. The ACE score is a graded indicator of childhood traumatic stress exposure where higher values (more exposures) has been correlated with many of the leading causes of death (Felitti et al. 1998), internalizing and externalizing behavior (Duke et al. 2010), early onset juvenile offending and juvenile recidivism (Baglivio et al. 2015; Wolff et al. 2015), and serious, violent, and chronic juvenile offending (Fox et al. 2015). The exact community version risk/needs assessment items, responses, and coding used to create ACE scores have been reported elsewhere (Baglivio et al. 2014). Each exposure was binary (yes/no) and exposures were summed for a cumulative ACE score ranging from 0 (not exposed to any) to 10 (exposed to all ten categories). The following ten adverse childhood experiences are included (the same ten exposures noted by the CDC): emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect, family violence, household substance abuse, household mental illness, parental separation or divorce, and household member incarceration.
A brief description of each adverse childhood experience and responses indicating being exposed are: (1) Emotional abuse: Parents/caretakers were hostile, berating, and/or belittling to youth; (2) Physical abuse: The youth reported being a victim of physical abuse or was victimized or physically abused by a family member; (3) Sexual abuse: The youth reported being the victim of sexual abuse/rape; (4) Emotional neglect: The youth reported no support network, little or no willingness to support the youth by the family, or that youth does not feel close to any family member; (5) Physical neglect: The youth has a history of being a victim of neglect (includes a negligent or dangerous act or omission that constitutes a clear and present danger to the child’s health, welfare, or safety, such as: failure to provide food, shelter, clothing, nurturing, or health care); (6) Family violence: The level of conflict between parents included verbal intimidation, yelling, heated arguments, threats of physical abuse, domestic violence, or the youth has witnessed violence at home or in a foster/group home; (7) Household substance abuse: Problem history of parents and/or siblings in the household includes alcohol or drug problems; (8) Household mental illness: Problem history of parents and/or siblings in the household includes mental health problems; (9) Parental separation/divorce: Youth does not live with both mother and father; and (10) Incarceration of household member: There is a jail/prison history of members of the household. The ACE score was included as a primary focus of the current study is whether traumatic histories are being overlooked in favor of behavioral diagnoses (CD, ODD, ADHD).
Child Welfare History
The youth’s history of involvement with the child welfare system is captured as no history of court-ordered or child welfare voluntary out-of-home or shelter care placements exceeding 30 days, one such placement, two placements, or three or more placements (coded 0–3). Higher values indicate more extensive official child welfare system placement/exposure.
Family Member Killed as a Result of Violence
Whether the youth has had a family member killed as a result of violence is captured dichotomously (yes = 1, else = 0).
Gang Membership
Youth who self-report as gang members or who have documented gang membership (must be documented by law enforcement as per Florida Department of Law Enforcement standards) are classified as having a history of gang membership (=1, else = 0).
Living Arrangement Prior to Residential Placement
The youth’s living arrangements prior to residential placement were captured as living under adult supervision, living with peers and no adults, living alone, or being transient/homeless with no adult supervision (coded 0–3, respectively).
Mental Health Risks
Mental health risk factors were included as they should increase the likelihood of a youth receiving psychiatric treatment, and based on their relation to CD, ODD, and ADHD symptomology.
Suicide Ideation/Attempt History
The youth’s history of suicidal ideation and attempts was captured as never had serious thoughts about suicide, suicidal ideation history, or youth has attempted suicide (coded 0–2). Suicidal ideation is based on youth self-report as well as evidence of hospitalization for self-injurious behavior or articulation as evidenced in the comprehensive psychological evaluation (discussed above).
Self-mutilation
A history of self-mutilation behavior was captured dichotomously as youth has engaged in self-mutilation (= 1, else = 0).
Impulsivity
Impulsivity was measured as a single item capturing the extent to which the youth was impulsive/acts without thinking.Footnote 6 The item categorized youth as uses self-control/usually thinks before acting, some self-control, impulsive, or highly impulsive/usually acts before thinking (coded 0–3). Higher values indicate more impulsivity.
Accepts Responsibility for Actions
The extent to which the youth accepts responsibility for his/her antisocial behaviors is measured as accepts responsibility, minimizes/denies/justifies antisocial behavior, accepts antisocial behavior as okay, or is proud of antisocial behavior (coded 0–3).
Belief that verbal Aggression is Acceptable to Resolve Conflicts
The extent to which the youth believes verbal aggression is an appropriate means to resolve conflict was captured as believes verbal aggression is rarely appropriate, sometimes appropriate, or often appropriate (coded 0–2). Higher values indicate greater belief that verbal aggression is appropriate in conflict resolution.
Belief that Physical Aggression is Acceptable to Resolve Conflicts
The extent to which the youth believes fighting and physical aggression are appropriate means to resolve disagreements was captured as believes physical aggression is never appropriate, rarely appropriate, sometimes appropriate, or often appropriate (coded 0–3). Higher values indicate greater belief that physical aggression and fighting are appropriate in conflict resolution.
Analytic Strategy
Analyses were conducted to investigate whether a disproportionate number of Black and Hispanic youth involved in the juvenile justice system receive behavioral mental health disorder diagnoses while also being less likely to receive psychiatric treatment. Prior to any multivariate analyses, the disproportionality in clinical diagnoses across race and ethnicity were examined using an analysis of variance (ANOVA). Then, binary logistic regression was used to examine the effect of adverse traumatic exposures on CD, ODD, and ADHD across race/ethnic sex-specific subgroups. More comprehensive logistic regression analyses were then used to investigate whether Black and/or Hispanic youth were more or less likely to receive specific mental health diagnoses after controlling for childhood trauma and criminal history measures, as well as a multitude of mental health and individual risk factors. In order to examine the relative contribution of each domain, we use an iterative procedure to model the likelihood of receiving a particular diagnosis including several models for each outcome. Additionally, in light of differences in cumulative traumatic exposure in prior work (discussed above) male and female youth were examined separately in the analyses reported below.
Results
Bivariate Comparisons
Table 1 presents the results of the ANOVA examining the prevalence of mental health disorders among male and female youth by racial/ethnic subgroups. Panel A of Table 1 presents the results for male youth. As seen, Black and Hispanic males were significantly more likely to have a Conduct Disorder diagnosis (p < .01), with Blacks evidencing the highest rate. Results suggest that no differences in the diagnosis of ODD exist across the three groups (F = .37; p > .05). On the other hand, White youth were more likely to be diagnosed with ADHD, followed by Hispanics and Blacks (p < .01). Similarly, White males were significantly more likely to be diagnosed with Adjustment or Anxiety Disorder, Eating Disorder, Intermittent Explosive Disorder or Mood Disorder than Black males. White males were also more likely than Black or Hispanic males to receive psychiatric treatment.
The results of the ANOVAs for females are presented in panel B of Table 1. Although the number of significant differences that exist across groups is smaller than for males, Black females were significantly more likely to have received a Conduct Disorder diagnosis than Hispanic or White females (p < .01). Alternatively, White females and Hispanic females were both more likely to be diagnosed with a Mood Disorder than Black females (F = 3.12; p < .05). Overall, the results presented in Table 1 suggest that prior to controlling for any individual characteristics that may influence the likelihood of a particular diagnosis, Black and Hispanic youth are more likely to be diagnosed with Conduct Disorder, while White youth are more likely to receive an alternative diagnosis.
Effect of ACEs on Clinical Disorder Diagnoses by Race/Ethnicity
A primary focus of the current study was the examination of the effect of cumulative traumatic exposures (ACEs) on the likelihood of a disruptive behavior diagnosis (CD, ODD, and ADHD). Table 2 displays results of binary logistic regression models entering the ACE score as the sole predictor of CD, ODD, and ADHD (separately) across race/ethnic sex-specific subgroups. As shown, the ACE summary score is associated with a decreased likelihood of CD diagnosis for White and Black males. For each additional traumatic exposure White males have 4 % lower odds of a CD diagnosis (OR = .959, p < .05), and Black males 5 % lower odds of a CD diagnosis (OR = .951, p < .01). Greater ACE exposure increases the odds of ODD diagnosis for both Black males and White females. Additionally, higher ACE scores are associated with increased odds of an ADHD diagnosis for all race/ethnic sex subgroups, except Hispanic females. Each additional traumatic exposure increases the odds of an ADHD diagnosis between 12 and 19 %. The ACE score was relevant for distinguishing youth with at least one of the examined diagnosis (CD, ODD, or ADHD) from youth without such diagnosis for all race/ethnic subgroups except Hispanic females. The ACE score was most often relevant in distinguishing an ADHD diagnosis, where such exposure increased the odds of having such diagnosis at admission to residential placement.
Predicting Clinical Disorder Diagnosis
Means-difference tests (independent samples t-tests) were conducted to examine differences between males and females on all 28 covariates (results not shown for brevity). Significant differences were found on 21 of the 28, in demonstration of the need to conduct split-samples analyses predicting clinical disorders by sex as the two groups were widely dissimilar.Footnote 7 Tables 3 and 4 display the results from a series of logistic regression models for male and female youth, respectively, and include logistic odds-ratios and 95 % confidence intervals. In this portion of the analyses, three outcomes were explored. Specifically, the probability that a youth was diagnosed with one of three clinical disorders: (1) Conduct Disorder, (2) Oppositional Defiant Disorder, and (3) ADHD. For each of these three outcomes, four models are presented. In the first, only the race/ethnic categories are included. The second model contains several measures of criminal history in addition to the race/ethnicity variables. Model 3 includes all individual and mental health risk measures, and the fourth model contains all of the covariates included in the current study.
Results presented in Models 1–4 of Table 3 suggest that Black males involved in the juvenile justice system are significantly more likely to be diagnosed with Conduct Disorder than Whites, net of all measures considered. Once covariates beyond demographics are included, being Hispanic is not associated with a Conduct Disorder diagnosis. Criminal history items were particularly relevant for Conduct Disorder and ADHD diagnoses when included. Looking at the full model, Black males were more than 40 % more likely to be diagnosed with Conduct Disorder than Whites (OR = 1.408; p < .001). Also, youth with a greater number of prior offenses (both misdemeanor OR = 1.071 p < .01, and felony offenses OR = 1.221, p < .001) were more likely to have been diagnosed, as were gang members (OR = 1.198; p < .01). Male youth who committed a felony sex offense were less likely to have a conduct disorder diagnosis (OR = .526; p < .001) as were youth with history of a child welfare placement (OR = .869; p < .001). Interestingly, although the measure of childhood trauma (the ACE score) had a significant effect in Model 3, once the measures of criminal history were included, this effect was no longer statistically significant (OR = .976; p > .05).
The second set of models (5–8) examine the relationship between all considered covariates and the likelihood of an ODD diagnosis among male youth. In the case of ODD, there is little evidence that youth of a specific racial/ethnic group are significantly more or less likely to receive such a diagnosis. Of all the characteristics examined, results presented in Model 8 (full model) suggest male youth with a greater number of prior felonies as well as those with a history of self-mutilation were less likely to receive an ODD diagnosis (OR = .773 and OR = .427; p < .05, respectively), whereas youth who believe in the use of physical aggression were nearly 17 % more likely to be diagnosed with ODD (O.R. = 1.168; p < .05).
Turning to the series of results devoted to examining the correlates of an ADHD diagnosis, the results presented in models 9–12 indicate that several of the youth characteristics are significantly related to our outcome. Consistent with prior research, Black and Hispanic youth were significantly less likely to be diagnosed with ADHD compared to White youth. Of the criminal history variables, age at first offense, prior felony offenses, felonies against person, prior detention stays, and history of residential treatment were all significantly related to ADHD diagnoses. Youth with behavioral and learning educational needs were also more likely to have been diagnosed with ADHD. Youth who had experienced a greater number of adverse life events (OR = 1.061; p < .001) or who had a history of a child welfare placement (OR = 1.130; p < .001) were also more likely to have been diagnosed with ADHD. Male youth with a history of suicidal ideation or who had attempted suicide in the past were nearly 30 % more likely to have been diagnosed with ADHD (OR = 1.28; p < .001).
Table 4 displays the results of the female-specific logistic regression analyses. Similar to the male results presented above, four models are presented for each of the three outcomes. Interestingly, criminal history items have far less relevance for the three behaviorally-defined diagnoses for females than they did for males. Focusing on the findings most central to the current research, Black females were significantly more likely to have been diagnosed with Conduct Disorder (OR = 1.544; p < .001) compared to White females, while the difference between Hispanics and Whites was not significant (OR = 1.31; p > .05). Females with a history of suicidal ideation or who had attempted suicide in the past were also less likely to receive a diagnosis for Conduct Disorder (OR = .803; p < .01).
Very few of the predictors considered were able to distinguish female youth who had been diagnosed with ODD from those who had not. In fact, of all the variables considered, only the number of prior misdemeanors (OR = .802; p < .05) and beliefs regarding the use of verbal aggression (OR = .675; p < .05) were significantly related to this outcome among females, but both serve to lower the likelihood of ODD diagnosis. There was no evidence that race/ethnicity influenced the likelihood of receiving an ODD diagnosis. A similar story emerges when examining results related to ADHD. Race/ethnicity was not significantly related to the likelihood of an ADHD diagnosis among females, however, both learning educational needs (OR = 2.165; p < .001) and suicidal ideation or attempt history (OR = 1.401; p < .001) were related with an increased likelihood of such a diagnosis.
Predicting the Receipt of Psychiatric Treatment
The final set of regression models, presented in Table 5, examine the correlates of receiving psychiatric treatment (including psychotropic medications) among male and female youth. Results presented in model 4 of Table 4 indicate that Black male youth were 32 % less likely to receive psychiatric treatment net of all control variables considered than White male youth (OR = .680; p < .001). Once more comprehensive models are considered (model 3 and 4), being Hispanic is not related to receipt of psychiatric treatment for males. Male youth who committed felony sexual or against person offenses were more likely to receive treatment (OR = 1.764 and OR = 1.244; p < .01, respectively). Other covariates that were significantly related to an increased likelihood of receiving psychiatric treatment among male youth were learning needs (OR = 1.478, p < .001) and child welfare history (OR = 1.131, p < .05). Finally, male youth who had a history of suicidal ideation or who had attempted suicide were 60 % more likely to receive psychiatric treatment as part of their case plan (OR = 1.608, p < .001). Adverse childhood experiences were unrelated to psychiatric treatment provision.
Similar to results presented above, among the 1347 females analyzed, very few of the covariates considered were significantly related to the likelihood of psychiatric treatment. For females, those who used drugs or alcohol were significantly more likely to receive psychiatric treatment than youth without substance abuse problems. There was no evidence, among females, that race/ethnicity had a significant impact on the probability of receiving psychiatric treatment. Interestingly, none of the mental health risk factors considered were significantly associated with receiving psychiatric treatment among females involved in the juvenile justice system. Similarly to males, ACEs were unrelated to receipt of psychiatric treatment among the females.
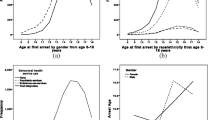
The predicted probabilities for each race/ethnic subgroup having a CD, or ADHD diagnosis, and for receiving psychiatric treatment are displayed for males (Fig. 1) and females (Fig. 2). These predicted probabilities are for the “average” youth of each race/ethnicity, holding all other variables included in the full models of Tables 2 and 3 at their means. As shown, for both males and females there is a stepwise progression in Conduct Disorder from White, to Hispanic, to Black youth, with White males having a 3 % lower probability than Hispanic males, and a 12.3 % lower probability than Black males, and White females a 12.9 % lower probability than Hispanic females and a 19 % lower probability than Black females. Furthermore, the “average” White male is only 7.8 % more likely than the “average” Hispanic male, but 30 % more likely than the “average” Black male to have received psychiatric treatment (predicted probability of .077 for White males and .054 for Black males; .077–0.054/.077 = .30). In comparison, there was a less than 3 %, non-significant, difference in psychiatric treatment provision across race/ethnicity for females.
Discussion
The high rates of psychiatric disorder among juvenile justice samples is well established (Karnik et al. 2009; Teplin et al. 2002; Wasserman et al. 2002), with detained youth up to three times as likely to have a psychiatric disorder than community youth (Cauffman et al. 2007). Yet the extent to which these results hold across race/ethnicity (and sex) remains an issue that has been relatively understudied. Even more noteworthy is the observation that the extent to which adolescents with particular diagnoses are provided adequate treatment in general and across race/ethnicity (and sex) is even less understood. The purpose of this study was to explore the racial/ethnic disproportionality in behavioral disorder diagnoses and the provision of psychiatric treatment among 8763 males and 1347 females admitted to long-term juvenile justice residential placements in Florida.
This study’s results confirmed the hypothesis that the majority of youth would be diagnosed with CD, except for White females who evidenced a 44.5 % prevalence. At the same time, our results differ from prior studies that found CD diagnosis higher among White youth than Black and Hispanic youth, though similar in that behavioral disorders were among the most prevalent psychiatric disorders in both males and females (Teplin et al. 2002). While Teplin and colleagues found White males and females to have higher rates of CD than Black males and females, and Hispanic females to have higher CD prevalence than Black females, our results show that Black juveniles evidence the highest CD prevalence, followed by Hispanics, then Whites (all group differences were statistically significant). Similar to prior work examining juveniles in residential placement (Vaughn et al. 2008), though not as disparate, and the Pathways to Desistance data (El Sayed et al. 2015), we found higher prevalence of ADHD among White youth compared to Hispanic and Black youth. Our findings also suggest that Black males were only 58–60 % as likely to receive psychiatric treatment, in spite of similar rates of not having any diagnosis (9.7 % of White males, 11.3 % of Black males), and net of controls. This echoes prior work finding racial disparities of Black youth being 39–52 % as likely to receive psychotropic medication among 5 through 14 year old, Medicaid insured community youth (Zito et al. 1998). Psychiatric treatment provision differences between White and Hispanic youth were not nearly as pronounced.
The results from the current study differ from a recent analysis of males in the Pathways to Desistance Study, which found no race/ethnicity differences in treatment provision among youth with substance abuse disorder diagnoses (Mansion and Chassin 2016). Our results may, therefore, be more troubling as the Pathways youth were incarcerated approximately 16 years ago, prior to recently touted juvenile justice reforms (Howell et al. 2014), whereas the current study examined residential admissions from the last five years in one large state. In comparison to a study of California youth in long-term residential juvenile placements (Karnik et al. 2009), Florida residential youth evidence much lower CD and ODD rates, but substantially higher ADHD prevalence across race/ethnicity and sex (with the exception of lower rates of ADHD for White females in Florida).
The hypothesis that Black youth would evidence lower rates of ODD and all other non-behavioral diagnoses than White youth was supported, with the exception of Black females having higher rates of ADHD than White females (although these differences were not statistically significant). Further, the hypothesis that White youth would have higher rates of psychiatric treatment provision than Black and Hispanic youth, net of controls, was observed only among males. No racial/ethnic disparities in the provision of psychiatric treatment for females were found.
With regard to trauma, as measured by the ACE score, when adverse childhood experiences are examined as the sole predictor of CD, ODD, and ADHD, significant results were found for ACEs decreasing the odds of CD for White males and Black males, increasing the odds of ODD for Black males and White females, and increasing the odds of ADHD for every subgroup except Hispanic females. These limited model results gave promise that cumulative traumatic exposure may be relevant in diagnostic decisions and race/ethnic diagnostic differences. In our comprehensive models with the inclusion of covariates, adverse childhood experiences decrease the likelihood of CD diagnoses for male youth but were rendered insignificant once criminal history indicators were included in the models, whereas more abuse exposures (higher ACE scores) increased the likelihood of ODD and ADHD diagnoses for males. For females, the ACE score was irrelevant across models. Overall, our results suggest that criminal history or other behavioral indicators may overshadow trauma symptomology in the diagnosis of externalizing behavioral disorders. Or, perhaps clinicians are following the behavioral indicators within diagnostic criteria and are not attending to the contextual realities in which youth were raised and currently reside. Contrary to expectations, the youth’s extent of exposure to multiple trauma types (the ACE score) was unrelated to whether the youth was receiving psychiatric treatment within the residential facility. It should be reiterated that prior research has indicated juvenile justice placements may exacerbate traumatic stress symptoms, and that arrests and placements themselves could be considered as traumatic exposures (Ford et al. 2007; Hennessey et al. 2004; Mahoney et al. 2004; Steinberg et al. 2004). In light of this interpretation, the significance of prior detention and residential placement indicators in the prediction of diagnoses may be indicative of the significance of trauma in such diagnoses. Prior detention placements increased the odds of ADHD among males, while prior residential placements increased the odds of ADHD among male and female youth.
The results from the current study should be tempered by the recognition of a few limitations. First, while the residential version risk/needs assessment was used for all youth in the current study, we have no knowledge of which assessments were used by the comprehensive evaluation clinicians to make the diagnoses which were indicated in the residential tool. Additionally, prior work has implicated that economic disadvantage may be related to a CD diagnoses, as those with lower socioeconomic status are found more likely to be diagnosed with CD (Lahey et al. 2005). Notably, as the current study did not include controls for the economic reality of the youth’s families, future work should collect this information. Also, it is likely the case that some unmeasured indicators that may have led to diagnostic differences were not present in the Florida data. However, the fact that the sample is exclusively of long-term residential juvenile justice admissions, and analyses controlled for traumatic exposures, prior offending, severity of offending, prior system placements, impulsivity, responsibility for actions, and peer associations, strengthens our position of disparity in CD diagnosis.
Moreover, the current study does not attend to the heterogeneity of youth with conduct disorder, either in terms of age of onset (childhood or adolescent onset), or with/without the callous-unemotional (CU) traits/limited prosocial emotions specifier. Recent work has highlighted this heterogeneity and the differences in risk factors, severity, etiology, aggressiveness, heritability, and “treatability” of the CD subgroups (Frick 2006; Frick et al. 2014; Scheepers et al. 2011; Van Damme et al. 2016; Viding et al. 2005; Viding et al. 2008; Waldman et al. 2011). While the DSM-5 contains a CU qualifier, the evidence in support of, or against, the specifier among juvenile justice-involved samples is rather limited (Colins and Andershed 2015; Colins and Vermeiren 2013; Lahey 2014; Van Damme et al. 2016), in contrast to more widespread support in community samples (Kahn et al. 2012; Pardini et al. 2012). Additionally, the current study captures admissions from 2011, prior to the DSM-5 (and therefore the CU specifier). Future work should examine racial/ethnic differences in the CU trait specifier for conduct disorder. This line of research examining subgroups of youth with CD is especially relevant in intervention outcome evaluations as the multisystemic and parent training interventions commonly employed with CD adolescents could be less effective with CD youth with CU traits, which is more biologically based and much less due to shared environment (Scheepers et al. 2011). The seemingly “un-treatability” of certain CD diagnosed youth may be more a function of the methods of treatment than true inability to improve functioning or outcomes. As CD increases risk of violence, weapon use, teenage pregnancy, substance abuse, and school dropout (Searight et al. 2001), and observing that 44–66 % of the youth (depending on race/ethnic and sex subgroup) had a diagnosis of CD in the current study, additional research is imperative. Such future research is particularly relevant, and related to the current study, as CU is associated with a history of maltreatment (Krischer and Sevecke 2008; Weiler and Widom 1996).
Additionally, the assessment instrument used in the current study did not specifically identify a PTSD diagnoses. A diagnosis of PTSD was included under the general anxiety disorder category. As such, the current study did not examine the implications of more extensive trauma exposure (higher ACE scores) on PTSD diagnoses. Future work should attend to important line of research, especially in light of suggestions that PTSD symptoms, and not simply traumatic exposure, may better explain the trauma-delinquency link, especially for females (Kerig et al. 2012). With respect to the psychiatric treatment dependent measure, future work should include more discrete measures of what treatment and or medication was actually provided, including dosages, frequencies, and durations. Furthermore, although the current study was focused on diagnostic disproportionality of residential youth, as only a judge can order a residential placement of a youth, future research should examine the extent to which placement decisions vary at the judicial level.
Conclusion
The current study examined racial/ethnic disparities in psychiatric behavioral diagnoses among serious juvenile offenders placed in long-term residential programs. Black males were more likely diagnosed with CD, and Black and Hispanic males less likely to have been diagnosed with ADHD, than White males, despite controlling for traumatic experiences, behavioral indicators, and prior offending. Black females were similarly more likely to have been diagnosed with CD than White females, even with the control measures included. Interestingly, in contrast to expectations, the extent of traumatic exposures experienced was unrelated to CD, ODD, or ADHD diagnoses for female adolescents, while adverse childhood experiences increased the likelihood of ODD and ADHD diagnoses for males. The results demonstrated that Black males were approximately 60 % as likely to receive psychiatric treatment as White males, in spite of similar rates of not having any diagnosis, while no race/ethnic differences in psychiatric treatment provision were found among female youth.
These results lend themselves well to both practice and policy implications. Clinical training may reduce ethnocentric biases through instruction on the appropriate application of Cultural Formulation tools within the DSM (Neighbors et al. 2003). Clinicians must be culturally knowledgeable with respect to how they ask questions, phrase terminology, and seek and process information, while making both within-group and between-group distinctions so as to not stereotype or “profile” youth (be culturally sensitive yet not assume all members of a racial/ethnic group are homogeneous; U.S. Department of Health and Human Services 2001; Neighbors et al. 2003). Additionally, prior work has shown more structured clinical assessments (which lessen discretion) reduce but do not eliminate racial bias in comparison to less structured diagnostic interviews (Neighbors et al. 1999). On the contrary, if there are cultural variations in how distress is communicated, diagnosticians would be better served attending to the influence of such factors in interpreting symptomology, meaning that more flexibility to incorporate cultural knowledge may be needed (Neighbors et al. 1999). While the current study did find differences in rates of disruptive behavior disorder diagnoses across racial/ethnic groups, the data do not permit attributing the disparities to profiling of diagnosticians, inadequacies in training, actual differences in mental health problems/symptomology across subgroups, or any other rationale.
Early intervention is critical, especially in treating Conduct Disorder, as intervention effectiveness decreases significantly in older youth (Brestan and Eyberg 1998; Kazdin 1995) and CD is one of the most frequent referrals for children and adolescent treatment services, with poor prognosis, and transmission across generations (Kazdin 1997). Treatment (at least for CD without CU traits) is most effective when targeting multiple risk domains and involving multiple components (Frick 2006). Based on prior work finding similar risks for ODD and CD, similar treatments should be effective (Boden et al. 2010). As one example, the Florida Department of Juvenile Justice should consider scaling its provision of the Stop Now and Plan (SNAP) intervention, and target those youth clinically appropriate. Similar to other self-control type modification programs (Piquero et al. 2010, 2016a), SNAP includes both a child and parent training component for aggressive youth under the age of twelve designed to teach youth impulse control and ultimately reduce the incidence of antisocial behavior (Augimeri et al. 2011; Augimeri et al. 2014). Prior evaluations demonstrate that SNAP reduces anxiety, aggression, conduct problems, and improves emotional regulation (Burke and Loeber 2014; Burke and Loeber 2015). Additional interventions for older youth should include Multisystemic Therapy (MST), Functional Family Therapy (FFT), social skills training, and parent management training, behavior modification, and pharmacotherapy (see e.g., Piquero et al. 2009, 2016b; Dannerbeck and Yan 2009; Kazdin 1997). However, referral to, engagement, and treatment retention should be closely monitored across race/ethnicity and culturally responsive practitioners mindful of disparities.
Untreated diagnoses can affect both behavior during incarceration as well as reduce the likelihood of post-release success (Breda 2003; Frick 2006; Teplin 2001; Wasserman et al. 2002). In light of the high prevalence rates of psychiatric disorders examined here and in prior work (e.g., Abram et al. 2003), transition and re-entry planning for delinquent youth must include adequate referrals for services, including plans and services for continuation of psychotropic and other medications within the community.
With regard to the research recommendation posed by the Federal Advisory Committee on Juvenile Justice (FACJJ), it appears that racial/ethnic disparity exists in the diagnoses of behavioral disorders associated with delinquency in spite of trauma symptomology or exposure. Contrary to expectations, trauma exposure was unrelated to any behavioral disorder examined for females, and not related to Conduct Disorder in males, or indicative of increased likelihood for psychiatric treatment receipt among males or females. We hope that our results spur additional work but also help to inform both practice and policy with respect to race/ethnic differences in both diagnosis and especially the treatment of serious adolescent offenders, who represent a policy-relevant group (Mulvey et al. 2004). That we observe a large disparity among Black youth and their being neglected of treatment services is disconcerting. Additional attention to why this disparity exists and then taking steps to rectify it is critically important for all justice and social service systems to operate in a manner that is fair to all delinquent youth. Accomplishing this during mid-adolescence is especially critical because this is a period of the life course where youth are still more than amenable to appropriate intervention and treatment services as well as the stage in life where subsequent offending trajectories can shift in either direction.
Notes
10,218 youth were admitted to residential programs in Florida during the December 1, 2011 through December 1, 2014 study time frame. Eighty-two of the 10,218 youth (0.8 %) were not assessed with the full community version risk/needs assessment and residential version risk/needs assessment. Sixty-two of the 82 youth were not assessed with a residential version assessment because the residential version was not required as of the date of the end of the study period (December 1, 2014). Youth admitted to a residential program are required to be assessed within the first 30 days of admission; the 62 youth had not been at the residential program for 30 days by the end of the study period. The 20 youth not assessed with a full community version prior to placement were assessed with a pre-screen community version, which does not contain the required information to create an ACE score. The pre-screen assessment-only admissions were most likely violations of Florida Department of Juvenile Justice protocol by probation staff. As the current study focuses on racial/ethnic differences, the 26 “other” youth were excluded as sample sizes were too small for valid comparisons.
The full community version risk/needs assessment consists of 126 items across the following twelve domains: criminal history, school, leisure/free time, employment, relationships, family/living situation, alcohol/drug use, mental health, attitudes/behaviors, aggression, and social skills. Current Florida Department of Juvenile Justice policy requires each youth being considered for residential placement to receive a full community version risk/needs assessment prior to admission to such a program.
In Florida, only a judge can order placement of a youth in a Florida Department of Juvenile Justice residential program. All youth placed in such programs are administered the community version risk assessment described above and are also evaluated by a licensed mental health professional. The youth are placed at the residential programs for an indeterminate period of time, with release (approved by the judge) based on completion of an individualized performance/treatment plan, rather than a set length of stay. The performance/treatment plans contain goals that address the youth’s specific risk factors as per the risk assessment and the comprehensive evaluation conducted by the licensed mental health professional. All youth who have not obtained a high school or equivalent diploma must attend school 25 h per week, instructed by certified Florida teachers. Youth attend treatment groups and individual counseling sessions (provided by licensed or supervised therapists) based on their individualized needs. Group services predominantly include cognitive behavioral interventions (to address criminal thinking/thinking errors), skills training groups, substance abuse prevention or intervention (based on the youth’s substance use history and/or diagnoses), sex offender services (based primarily on offending history), mental health group services (such as healthy relationships, identifying internal and external triggers, anger management), and family therapy. All residential programs have a behavior management system (token economy) which requires level attainment for increased privileges.
Comprehensive mental health evaluations are governed by Florida Statute (F.S. 985.29) and must include the following components: identifying information; reason for evaluation; relevant background information (including home environment/family functioning; history of physical abuse, sexual abuse, neglect, witnessing violence and other forms of trauma; behavioral functioning; health [physical health, mental health and substance abuse] and educational functioning); behavioral observations/mental status examination; interview or procedures administered; discussion of findings; diagnostic impression/formulation; and recommendations. The current study does not include analyses of disparities across evaluator credentials (e.g., licensed social worker, licensed psychologist, etc.), or psychiatric diagnosis assessment methods, as the purpose was to examine differences in the diagnoses youth were labeled with upon admission to residential placement, and not the means by which such disparities arose. Future work would benefit from detailed examination across such evaluation and evaluator characteristics.
Of note, as per Florida Department of Juvenile Justice protocol, Hispanic ethnicity supersedes race, meaning the Black youth are non-Hispanic Blacks, and the White youth are non-Hispanic Whites.
While an anonymous reviewer questioned our use of impulsivity as a covariate in light of its association with one of the dependent measures (ADHD), we argue for its inclusion as: (1) impulsivity is only one component of ADHD; (2) our measure of impulsivity assesses such behavior within the past four weeks, while the ADHD diagnosis requires six months of such behavior; and (3) traumatic stress/exposure has been implicated in changes in brain functioning which alter the “fight or flight” response and increasing the propensity to perceive situations as overly threatening than reality suggests and act impulsively (Kerig and Becker 2010).
Specifically, males were significantly more likely than females to be Black or Hispanic, have more prior felonies, more likely to have sexual felony offenses, learning needs, self-report gang membership, and more likely to accept responsibility for actions. Males were less likely than females to have alcohol problems, had fewer prior misdemeanors, fewer prior detention stays, were younger at age of first suspension/expulsion from school, less likely to have extensive runaway history, had lower ACE scores and less likely to have child welfare history, less likely to have had a family member killed as a result of violence, less likely to be transient/homeless, less likely to have attempted suicide or engage in self-mutilation, less impulsive and less likely to espouse belief in the appropriateness of verbal or physical aggression.
References
Abram, K. M., Teplin, L. A., Charles, D. R., Longworth, S. L., McClelland, G. M., & Dulcan, M. K. (2004). Posttraumatic stress disorder and trauma in youth in juvenile detention. Archives of General Psychiatry, 61, 403–410.
Abram, K. M., Teplin, L. A., McClelland, G. M., & Dulcan, M. K. (2003). Comorbid psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry, 60, 1097–1108.
Ackerman, P. T., Newton, J. E. O., McPherson, W. B., Jones, J. G., & Dykman, R. A. (1998). Prevalence of post traumatic stress disorder and other psychiatric diagnoses in three groups of abused children (sexual, physical, and both). Child Abuse & Neglect, 22, 759–774.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. 5th ed. Arrlington, VA: American Psychiatric Publishing.
Anda, R. F., Brown, D. W., Felitti, V. J., Bremner, D., Dube, S. R., & Giles, W. H. (2007). Adverse childhood experiences and prescribed psychotropic medications in adults. American Journal of Preventive Medicine, 32, 389–394.
Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., Perry, B. D., Dube, S. R., & Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Clinical Neuroscience, 256, 174–186.
Anderson, E. (1999). Code of the street. New York, NY: Norton.
Augimeri, L. K., Walsh, M., Levene, K., Sewell, K., & Rajca, E. (2014). Stop now and plan (SNAP) model. Encyclopedia of criminology and criminal justice, (5053-5063). New York, NY: Springer Science – Business Media.
Augimeri, L. K., Walsh, M., & Slater, N. (2011). Rolling out SNAP® an evidence-based intervention: a summary of implementation, evaluation, and research. International Journal of Child, Youth and Family Studies, 2(2.1), 330–352.
Baglivio, M. T. (2009). The assessment of risk to recidivate among a juvenile offending population. Journal of Criminal Justice, 37(6), 596–607.
Baglivio, M. T., Epps, N., Swartz, K., Huq, M. S., Sheer, A., & Hardt, N. S. (2014). The prevalence of adverse childhood experiences (ACE) in the lives of juvenile offenders. Journal of Juvenile Justice, 3, 1–23.
Baglivio, M. T., & Jackowski, K. (2013). Examining the validity of a juvenile offending risk assessment instrument across gender and race/ethnicity. Youth Violence and Juvenile Justice, 11, 26–43.
Baglivio, M. T., Wolff, K. T., Piquero, A. R., & Epps, N. (2015). The relationship between adverse childhood experiences (ACE) and juvenile offending trajectories in a juvenile offender sample. Journal of Criminal Justice, 43, 229–241.
Becker, S. P., Kerig, P. K., Lim, J. -Y., & Ezechukwu, R. N. (2012). Predictors of recidivism among delinquent youth: Interrelations among ethnicity, gender, age, mental health problems, and posttraumatic stress. Journal of Child & Adolescent Trauma, 5, 145–160.
Boden, J. M., Fergusson, D. M., & Horwood, L. J. (2010). Risk factors for conduct disorder and oppositional/defiant disorder: Evidence from a New Zealand birth cohort. Journal of the American Academy of Child & Adolescent Psychiatry, 49, 1125–1133.
Breda, C. S. (2003). Offender ethnicity and mental health service referrals from juvenile courts. Criminal Justice and Behavior, 30, 644–667.
Brestan, E. V., & Eyberg, S. M. (1998). Effective psychological treatments for conduct disordered children and adolescents. Journal of Clinical Child Psychology, 27, 180–189.
Bridges, G., & Steen, S. (1998). Racial disparities in official assessments of juvenile offenders: Attribution stereotypes as mediating mechanisms. American Sociological Review, 63, 554–570.
Brody, G. H., Ge, X., Kim, S., Murry, V., Simons, R. L., Gibbons, F. X., Gerrard, M., & Conger, R. D. (2003). Neighborhood disadvantage moderates associations of parenting and older sibling problem attitudes and behavior with conduct disorders in African American children. Journal of Consulting and Clinical Psychology, 71, 211–222.
Burke, J. D., & Loeber, R. (2014). The effectiveness of the Stop Now and Plan (SNAP) Program for boys at risk for violence and delinquency. Prevention Science, 16, 242–253.
Burke, J. D., & Loeber, R. (2015). Mechanisms of behavioral and affective treatment outcomes in a cognitive behavioral intervention for boys. Journal of Abnormal Child Psychology, 44, 179–189.
Burke, J. D., Loeber, R., Mutchka, J. S., & Lahey, B. B. (2002). A question for DSM-V: Which better predicts persistent conduct disorder—delinquent acts or conduct symptoms? Criminal Behaviour and Mental Health, 12, 37–52.
Cannon, Y., Davis, G., Hsi, A., & Bochte, A. (2016). Adverse childhood experiences in the New Mexico juvenile justice population. Albuquerque, NM: New Mexico Sentencing Commission.
Cauffman, E., Feldman, S., Waterman, J., & Steiner, H. (1998). Posttraumatic stress disorder among female juvenile offenders. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 1209–1216.
Cauffman, E., Lexcen, F. J., Goldweber, A., Shulman, E. P., & Grisso, T. (2007). Gender differences in mental health symptoms among delinquent and community youth. Youth Violence and Juvenile Justice, 5, 287–307.
Centers for Disease Control and Prevention. (2016). Injury prevention and control: Adverse childhood experiences (ACE) study. Available online: http://www.cdc.gov/violenceprevention/acestudy/. Accessed May 15, 2016.
Chang, D. F., & Sue, S. (2003). The effects of race and problem type on teachers’ assessments of student behavior. Journal of Consulting and Clinical Psychology, 71, 235–242.
Collins, R. E. (2010). The effect of gender on violent and nonviolent recidivism: A meta-analysis. Journal of Criminal Justice, 38, 675–684.
Colins, O. F., & Andershed, H. (2015). The DSM-5 with limited prosocial emotions specifier for conduct disorder among detained girls. Law and Human Behavior, 39, 198–207.
Colins, O. F., & Vermeiren, R. (2013). The usefulness of DSM-IV and DSM-5 conduct disorder subtyping in detained adolescents. Journal of Nervous and Mental Disease, 201, 736–743.
Dalton, R. F., Evans, L. J., Cruise, K. R., Feinstein, R. A., & Kendrick, R. F. (2009). Race differences in mental health service access in a secure male juvenile justice facility. Journal of Offender Rehabilitation, 48(3), 194–209.
Dana, R. H. (2012). Mental health services for African Americans: A cultural/racial perspective. Journal of Human Growth & Development, 9, 63–73.
Dannerbeck, A., & Yan, J. (2009). Exploring patterns of court-ordered mental health services for juvenile offenders: Is there evidence of systemic bias? Criminal Justice and Behavior, 36, 402–419.
Dierkhising, C. B., Ko, S. J., Woods-Jaeger, B., Briggs, E. C., Lee, R., & Pynoos, R. S. (2013). Trauma histories among justice-involved youth: Findings from the national child traumatic stress network. European Journal of Psychotraumatology, 4, 1–12. doi:10.3402/ejpt.v4i0.20274.
Dodge, K. A., & Pettit, G. S. (2003). A biopsychosocial model of the development of chronic conduct problems in adolescence. Developmental Psychology, 39, 349–371.
Duke, N. N., Pettingell, S. L., McMorris, B. J., & Borowsky, I. W. (2010). Adolescent violence perpetration: Associations with multiple types of adverse childhood experiences. Pediatrics, 125, 778–786.
Edens, J. F., Campbell, J. S., & Weir, J. M. (2007). Youth psychopathy and criminal recidivism: A meta-analysis of the psychopathy checklist measures. Law and Human Behavior, 31, 53–75.
El Sayed, S., Piquero, A. R. Schubert, C. A., Mulvey, E. P., Pitzer, L., & Piquero, N. L. (2015). Assessing the mental health/offending relationship across race/ethnicity in a sample of serious adolescent offenders. Criminal Justice Policy Review, doi:10.1177/0887403415575145.
Epstien, J. N., March, J. S., Conners, C. K., & Jackson, D. L. (1998). Racial differences on the Conners teacher rating scale. Journal of Abnormal Child Psychology, 26, 109–118.
Evans-Chase, M. (2014). Addressing trauma and psychosocial development in juvenile justice-involved youth: A synthesis of the developmental neuroscience, juvenile justice and trauma literature. Laws, 3, 744–758.
Federal Advisory Committee on Juvenile Justice (FACJJ). (2015). Recommendations to the President, Congress, and OJJDP Administrator. Available at: http://www.facjj.org/annualreports/FACJJ_2015_Cover_letter_and_recommendations_FINAL.pdf?ed2f26df2d9c416fbddddd2330a778c6=oxvooxixv-oanpoana.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., & Marks, J. S. (1998). Relationship of childhood abuse and dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine, 14, 245–258.
Fitzgerald, W. A. (1996). Stories of child outlaws: On child heroism and adult power in juvenile justice. Wisconsin Law Review, 1996, 495–538.
Florida Administrative Code. (2016). Rule chapter 63d-9: Assessment. Available from: https://www.flrules.org/gateway/ChapterHome.asp?Chapter=63D-9
Ford, J. D., Chapman, J. F., Hawke, J., & Albert, D. (2007). Trauma among youth in the juvenile justice system: Critical issues and new directions. National Center for Mental Health and Juvenile Justice, 1-8.
Fox, B. H., Perez, N., Cass, E., Baglivio, M. T., & Epps, N. (2015). Trauma changes everything: Examining the relationship between adverse childhood experiences and serious, violent and chronic juvenile offenders. Child Abuse & Neglect, 46, 163–173.
Frick, P. J. (2004). Developmental pathways to conduct disorder: Implications for serving youth who show severe aggressive and antisocial behavior. Psychology in the Schools, 41, 823–834.
Frick, P. J. (2006). Developmental pathways to conduct disorder. Child and Adolescent Psychiatric Clinics of North America, 15, 311–331.
Frick, P. J., Ray, J. V., Thonton, L. C., & Kahn, R. E. (2014). Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. Psychological Bulletin, 140, 1–57.
Garland, A., Lau, A., Yeh, M., McCabe, K., Hough, R., & Landsverk, J. (2005). Racial and ethnic differences in utilization of mental health services among high-risk youths. American Journal of Psychiatry, 162, 1336–1343.
Geller, J. D. (1988). Racial bias in the evaluation of patients for psychotherapy. In L. D. Comas-Díaz & E. E. H. Griffith (Eds.). Clinical guidelines in cross-cultural mental health (pp. 112–134). New York, NY: Wiley.
Godinet, M. T., Li, F., & Berg, T. (2014). Early childhood maltreatment and trajectories of behavioral problems: Exploring gender and racial differences. Child Abuse and Neglect, 38, 544–556.
Grevstad, J. A. (2010). Adverse childhood experiences and juvenile justice. PowerPoint delivered to Washington State Family Policy Council June 8, 2010.
Gudiño, O. G., Lau, A. S., Yeh, M., McCabe, K. M., & Hough, R. L. (2008). Understanding racial/ethnic disparities in youth mental health services: Do disparities vary by problem type? Journal of Emotional and Behavioral Disorders, advance online publication, doi:10.1177/1063426608317710.
Hennessey, M., Ford, J. D., Mahoney, K., Ko, S. J., & Siegfried, C. B. (2004). Trauma among girls in the juvenile justice system. Los Angeles, CA and Durham, NC: National Child Traumatic Stress Network.
Herz, D. C. (2001). Understanding the use of mental health placements by the juvenile justice system. Journal of Emotional and Behavioral Disorders, 9, 172–181.
Hosterman, S. J., DuPaul, G. J., & Jitendra, A. K. (2008). Teacher ratings of ADHD symptoms in ethnic minority students: Bias or behavioral difference? School Psychology Quarterly, 23, 418–435.
Howell, J. C., Lipsey, M. W., & Wilson, J. J. (2014). A handbook of evidence-based juvenile justice systems. Lanham, MD: Lexington Books.
Hsieh, D. K., & Kirk, S. A. (2003). The effect of social context on psychiatrists’ judgments of adolescent antisocial behavior. Journal of Child Psychology and Psychiatry, 44, 877–887.
Johnson, J. G., Cohen, P., Brown, J., Smailes, E. M., & Bernstein, D. P. (1999). Childhood maltreatment increases risk for personality disorders during early adulthood. JAMA Psychiatry, 56, 600–606.
Kahn, R. E., Frick, P. J., Youngstrom, E., Findling, R. L., & Youngstrom, J. K. (2012). The effects on including a callous-unemotional specifier for the diagnosis of conduct disorder. The Journal of Child Psychology and Psychiatry, 53, 271–282.
Karnik, N. S., Soller, M., Redlich, A., Silverman, M., Kraemer, H. C., Haapanen, R., & Steiner, H. (2009). Prevalence of and gender differences in psychiatric disorders among juvenile delinquents incarcerated for nine months. Psychiatric Services, 60, 838–841.
Kazdin, A. E. (1995). Conduct disorders in childhood and adolescence. 2nd ed. Thousand Oaks, CA: Sage.
Kazdin, A. E. (1997). Practitioner review: Psychological treatments for conduct disorder in children. Journal of Child Psychology and Psychiatry, 38, 161–178.
Kerig, P. K., & Becker, S. P. (2010). From internalizing to externalizing: Theoretical models of the processes linking PTSD to juvenile delinquency. In Sylvia J. Egan (Ed.), Post-traumatic stress disorder (PTSD): Causes, symptoms and treatment (pp. 33–78). Hauppauge, NY: Nova Science Publishers.
Kerig, P. K., Vanderzee, K. L., Becker, S. P., & Ward, R. M. (2012). Deconstructing PTSD: Traumatic experiences, posttraumatic symptom clusters, and mental health problems among delinquent youth. Journal of Child & Adolescent Trauma, 5, 129–144.
Kochel, T. R., Wilson, D. B., & Matrofski, S. D. (2011). Effect of suspect race on officers’ arrest decisions. Criminology, 24, 460–495.
Krischer, M. K., & Sevecke, K. (2008). Early traumatization and psychopathy in female and male juvenile offenders. International Journal of Law and Psychiatry, 31, 253–262.
Kunen, S., Smith, P., Niederhauser, R., Morris, J., & Marx, B. (2005). Race disparities in psychiatric rates in emergency departments. Journal of Consulting and Clinical Psychology, 73, 116–126.
Lahey, B. B. (2014). What we need to know about callous-unemotional traits: Comment on Frick, Ray, Thornton, and Kahn (2014). Psychological Bulletin, 140, 58–63.
Lahey, B. B., Loeber, R., Burke, J. D., & Applegate, B. (2005). Predicting future antisocial personality disorder in males from a clinical assessment in childhood. Journal of Consulting and Clinical Psychology, 73, 389–399.
Losen, D. J., & Orfield, G. (2002). Racial inequity in special education. Cambridge, MA: Harvard Education Publishing Group.
Lynskey, M. T., Fergusson, D. M., & Horwood, L. J. (1994). The effect of parental alcohol problems on rates of adolescent psychiatric disorders. Addition, 89, 1277–1286.
Mahoney, K., Ford, J. D., Ko, S. J., & Siegfried, C. B. (2004). Trauma-focused interventions for youth in the juvenile justice system. Los Angeles, CA: National Child Traumatic Stress Network.
Mallett, C. A., Fukushima, M., Stoddard-dare, P., & Quinn, L. (2013). Factors related to recidivism for youthful offenders. Criminal Justice Studies, 26, 84–98.
Mansion, A. D., & Chassin, L. (2016). The effect of race/ethnicity on the relation between substance use disorder diagnosis and substance use treatment receipt among male serious adolescent offenders. Children and Youth Services Review, 61, 237–244.
McCabe, K. M., Lucchini, S. E., Hough, R. L., Yeh, M., & Hazen, A. (2005). The relation between violence exposure and conduct problems among adolescents: A prospective study. American Journal of Orthopsychiatry, 75, 575–584.
Mitchell, O. (2005). A meta-analysis of race and sentencing research: Explaining the inconsistencies. Journal of Quantitative Research, 21, 439–466.
Mulvey, E. P., Steinberg, L., Fagan, J., Cauffman, E., Piquero, A. R., Chassin, L., & Losoya, S. H. (2004). Theory and research on desistance from antisocial activity among serious adolescent offenders. Youth Violence and Juvenile Justice, 2, 213–236.
Neighbors, H. W., Ford, B., Trierweiler, S. J., & Stillman, P. (2002). African American mental health disparities: Prevalence, utilization, diagnosis, and treatment. In J. Berry, D. Baldwin, & P. Marshall (Eds.), Eliminating disparities in the treatment of African Americans with mental health and substance abuse disorders. Rockville, MD: Substance Abuse & Mental Health Services Administration.
Neighbors, H. W., Jackson, J. S., Campbell, L., & Williams, D. (1989). The influence of racial factors on psychiatric diagnosis: A review and suggestions for research. Community Mental Health Journal, 25, 301–311.
Neighbors, H., Trierweiler, S., Ford, B., & Murorff, J. (2003). Racial differences in DSM diagnoses using a semi-structured instrument: The importance of clinical judgment in the diagnosis of African Americans. Journal of Health and Social Behavior, 43, 237–256.
Neighbors, H. W., Trierweiler, S. J., Munday, C., Thompson, E. E., Jackson, J. S., Binion, V. J., & Gomez, J. (1999). Psychiatric diagnosis of African Americans: Diagnostic divergence in clinical structured and semi structured interviewing conditions. JAMA, 91, 601–612.
Odgers, C. L., Milne, B. J., Caspi, A., Crump, R., Poulton, R., & Moffitt, T. E. (2007). Predicting prognosis for the conduct-problem boy: Can family history help? Journal of the American Academy of Child & Adolescent Psychiatry, 46, 1240–1249.
Pardini, D., Stepp, S., Hipwell, A., Stouthamer-Loeber, M., & Loeber, R. (2012). The clinical utility of the proposed DSM-5 callous-unemotional subtype of conduct disorder in young girls. Journal of the American Academy of Child & Adolescent Psychiatry, 51, 62–73.
Partenio, I., & Taylor, R. (1985). The relationship of teacher ratings and IQ: A question of bias? School Psychology Review, 14, 79–83.
Pavkov, T. W., Lewis, D. A., & Lynons, J. S. (1989). Psychiatric diagnosis and racial bias: an empirical investigation. Professional Psychology: Research and Practice, 20, 364–368.
Piquero, A. R. (2008). Disproportionate minority contact. The Future of Children, 18, 59–79.
Piquero, A. R., Jennings, W., & Farrington, D. P. (2010). On the malleability of self-control: Theoretical and policy implications regarding a General Theory of Crime. Justice Quarterly, 27, 803–834.
Piquero, A. R., Jennings, W., Farrington, D. P., Diamond, B., & Reingle Gonzalez, J. M. (2016a). A meta-analysis update on the effectiveness of early self-control improvement programs to improve self-control and reduce delinquency. Journal of Experimental Criminology, 12, 249–264.
Piquero, A. R., Farrington, D. P., Welsh, B. C., Tremblay, R., & Jennings, W. (2009). Effects of early family/parent training programs on antisocial behavior and delinquency. Journal of Experimental Criminology, 5(2), 83–120.
Piquero, A. R., Jennings, W., Farrington, D. P., Diamond, B., Farrington, D. P., Tremblay, R. E., Welsh, B. C., & Reingle Gonzalez, J. M. (2016b). A meta-analysis update on the effects of early family/parent training programs on antisocial behavior and delinquency. Journal of Experimental Criminology, 12, 229–248.
Plewis, I. (1997). Inferences about teacher expectations from national assessment at Key Stage One. British Journal of Educational Psychology, 67, 235–247.
Rawal, P., Romansky, B., Jenuwine, M., & Lyons, J. (2004). Racial differences in the mental health needs and service utilization of youth in the juvenile justice system. Journal of Behavioral Health Services and Research, 31, 242–254.
Reid, R., DuPaul, G. J., Power, T. J., Anastopoulos, A. D., Rogers-Adkinson, D., Noll, M. B., & Riccio, C. (1998). Assessing culturally different students for attention deficit hyperactivity disorder using behavior rating scales. Journal of Abnormal Child Psychology, 26, 187–198.
Richters, J., & Cicchetti, D. (1993). Mark Twain meets DSM-III-R: Conduct disorder, development, and the concept of harmful dysfunction. Development and Psychopathology, 5, 5–29.
Ricks, E. P., & Louden, J. E. (2016). Slipping through the cracks: Is mental illness appropriately identified among Latino offenders? Criminal Justice and Behavior, 43, 525–538.
Robbins, L. N. (1978). Sturdy childhood predictors of adult antisocial behavior: Replications from longitudinal studies. Psychological Medicine, 8, 611–622.
Scheepers, F. E., Buitelaar, J. K., & Matthys, W. (2011). Conduct disorder and the specifier callous and unemotional traits in the DSM-5. European Child and Adolescent Psychiatry, 20, 89–93.
Searight, H. R., Rottnek, F., & Abby, S. L. (2001). Conduct disorder: Diagnosis and treatment in primary care. American Family Physician, 63, 1579–1588.
Sickmund, M., & Puzzanchera C. (Eds.) (2014). Juvenile offenders and victims: 2014 national report. Washington DC: National Center for Juvenile Justice.
Snowden, L. (2003). Bias in mental health assessment and intervention: Theory and evidence. American Journal of Public Health, 93, 239–243.
Steinberg, L., Chung, H. L., & Little, M. (2004). Reentry of young offenders from the justice system: A developmental perspective. Youth Violence and Juvenile Justice, 2, 21–38.
Stevens, T., & Morash, M. (2015). Racial/ethnic disparities in boys’ Probability of Arrest and Court Actions in 1980 and 2000: The disproportionate impact of “Getting Tough” on Crime. Youth Violence and Juvenile Justice, 13, 77–95.
Tengström, A., Grann, M., Långström, N., & Kullgren, G. (2000). Psychopathy (PCL-R) as a predictor of violent recidivism among criminal offenders with schizophrenia. Law and Human Behavior, 24, 45–58.
Teplin, L. A. (2001). Assessing alcohol, drug, and mental disorders in juvenile detainees. Washington, DC: U.S. Department of Justice. (OJJDP Fact Sheet No. 2)
Teplin, L. A., Abram, K. M., McClelland, G. M., Dulcan, M. K., & Mericle, A. A. (2002). Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry, 59, 1133–1143.
Teplin, L. A., Abram, K. M., McClelland, G. M., Washburn, J. J., & Pikus, A. K. (2005). Detected mental disorder in juvenile detainees: Who receives services? American Journal of Public Health, 95, 1773–1980.
Teplin, L. A., Welty, L. J., Abram, K. M., Dulcan, M. K., & Washburn, J. J. (2012). Prevalence and persistence of psychiatric disorders in youth after detention. Archives of General Psychiatry, 69, 1031–1043.
Thomas, W. J., Stubbe, D. E., & Pearson, G. (1999). Race, juvenile justice, and mental health: New dimensions in measuring pervasive bias. The Journal of Criminal Law & Criminology, 89, 615–670.
U.S. Department of Health and Human Services. (2001). Mental health: Culture, race, and ethnicity- A supplement to mental health: A report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services.
Van Damme, L., Colins, O. F., & Vanderplasschen, W. (2016). The limited prosocial emotions specifier for conduct disorder among detained girls: A multi-informant approach. Criminal Justice and Behavior, 43, 778–792.
Van Ryn, M., & Burke, J. (2000). The effect of patient race and socio-economic status on physicians’ perceptions of patients. Social Science & Medicine, 50, 813–828.
Vaughn, M. G., Wallace, J. M., Davis, L. E., Fernandes, G. T., & Howard, M. O. (2008). Variations in mental health problems, substance use, and delinquency between African American and Caucasian juvenile offenders. International Journal of Offender Therapy and Comparative Criminology, 52, 311–329.
Velasquez, R. J., Johnson, R., & Brown-Cheatham, M. (1993). Teaching counselors to use the DSM-II-R with ethnic minority clients: A paradigm. Counselor Education and Supervision, 32, 323–331.
Vermeiren, R., Schwab-Stone, M., & Ruchkin, V., et al. (2002). Predicting recidivism in delinquent adolescents from psychological and psychiatric assessment. Comprehensive Psychiatry, 43, 142–149.
Viding, E., Blair, J. R., Moffitt, T. E., & Plomin, R. (2005). Evidence for substantial genetic risk for psychopathy in 7-year-olds. Journal of Child Psychology and Psychiatry, 46, 592–597.
Viding, E., Jones, A., Frick, P., Moffitt, T. E., & Plomin, R. (2008). Heritability of antisocial behavior at age nine: Do callous-unemotional traits matter? Developmental Science, 11, 17–22.
Waldman, I. D., Tackett, J. L., Van Hulle, C. A., Applegate, B., Pardini, D., Frick, P. J., & Lahey, B. B. (2011). Child and adolescent conduct disorder substantially shares genetic influences with three socioemotional dispositions. Journal of Abnormal Psychology, 120, 57–70.
Wasserman, G. A., McReynolds, L. S., Lucas, C. P., Fisher, P., & Santos, L. (2002). The Voice DISC-IV with incarcerated male youths: Prevalence of Disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 41, 314–321.
Wasserman, G. A., Miller, L. S., & Cothern, L. (2000). Prevention of serious and violent juvenile offending. Juvenile Justice Bulletin, Office of Justice Programs: Office of Juvenile Justice and Delinquency Prevention.
Weiler, B. L., & Widom, C. S. (1996). Psychopathy and violent behaviour in abused and neglected young adults. Criminal Behaviour and Mental Health, 6, 253–271.
Wierson, M., & Forehand, R. (1995). Predicting recidivism in juvenile delinquents: The role of mental health diagnoses and the qualification of conclusions by race. Behavioral Research and Therapy, 33, 63–67.
Whaley, A. (2002). Ethnicity/race, paranoia, and psychiatric diagnosis: Clinician bias versus sociocultural differences. Journal of Psychopathology and Behavioral Assessment, 19, 1–20.
Widom, C. S. (1989a). The cycle of violence. Science, 244(4901), 160–166.
Widom, C. S. (1989b). Child abuse, neglect, and adult behavior: Research design and findings on criminality, violence, and child abuse. American Journal of Orthopsychiatry, 59, 355–367.
Wolff, K. T., Baglivio, M. T., & Piquero, A. R. (2015). The relationship between adverse childhood experiences and recidivism in a sample of juvenile offenders in community-based treatment. International Journal of Offender Therapy and Comparative Criminology, advance online publication, doi:10.1177/0306624X15613992.
Worrell, J., & Remer, P. (2003). Feminist perspectives in therapy: Empowering diverse women. New York, NY: Wiley.
Wu, J. (2016). Racial/ethnic discrimination and prosecution. Criminal Justice and Behavior, 43, 437–458.
Zito, J. M., Safer, D. J., Dosreis, S., & Riddle, M. A. (1998). Racial disparity in psychotropic medications prescribed for youths with Medicaid insurance in Maryland. Journal of the American Academy of Child & Adolescent Psychiatry, 37, 179–184.
Author Contributions
MB conceived of the project and its design, drafted a majority of the manuscript, participated in the design of study methodology, and participated in cleaning the data and creating appropriate measures. KW drafted a significant portion of the manuscript, participated in the design of study methodology, and performed the vast majority of statistical analyses. AP drafted significant portions of the manuscript, participated in the design of study methodology, consulted on statistical analysis, and coordinated editing of manuscript drafting. MG provided both assistance with drafting of the manuscript, editorial support, and insight into the juvenile justice system, procured the data, obtained approval for use of the data, and provided input into appropriate analysis of the data. NE conceived of the project, cleaned the data, was integral in the policy implications of the study, and provided editorial support. All authors read, edited, and approved the final manuscript.
Funding
The authors received no funding for the completion of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict interests.
Ethical Approval
Approval for this project was acquired from the Florida Department of Juvenile Justice Institutional Review Board.
Rights and permissions
About this article
Cite this article
Baglivio, M.T., Wolff, K.T., Piquero, A.R. et al. Racial/Ethnic Disproportionality in Psychiatric Diagnoses and Treatment in a Sample of Serious Juvenile Offenders. J Youth Adolescence 46, 1424–1451 (2017). https://doi.org/10.1007/s10964-016-0573-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10964-016-0573-4