Abstract
While researchers are beginning to reach consensus around key psychological correlates of non-suicidal self-injury (NSSI), comparatively less work has been done investigating the role and influence of peers. Given evidence that engagement in this behavior may be susceptible to peer influence, especially during the early stages of its course, the current study prospectively explored whether knowing a friend who self-injures is associated with the onset, severity, and subsequent engagement in NSSI. The moderating roles of adverse life events, substance use and previous suicidal behavior in this relationship also were explored. Self-report data were collected from 1,973 school-based adolescents (aged 12–18 years; 72 % female) at two time points, 1 year apart. Knowing a friend who self-injured, negative life events, psychological distress and thoughts of NSSI differentiated those who self-injured from those who did not, and also predicted the onset of NSSI within the study period. Further, adverse life events and previous thoughts of NSSI moderated the relationship between exposure to NSSI in peers and engaging in NSSI at Time 2. However, the effect of having a friend who self-injures was not related to the severity of NSSI. Having a friend who self-injures appears to be a risk factor for self-injury among youth who are experiencing high levels of distress. Implications of these findings are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-suicidal self-injury (NSSI), the deliberate alteration or destruction of body tissue without conscious suicidal intent (International Society for the Study of Self-Injury 2007), is a growing public health concern. Particularly common in adolescents and young adults, it is associated with significant morbidity including anxiety, depression and later risk of suicide (Martin et al. 2010; Nock et al. 2006). Despite a growing foundational knowledge base regarding psychological correlates of NSSI (Brausch and Gutierrez 2010; Klonsky 2007; Nock 2010), relatively little is known about why young people start self-injuring and what factors may be associated with engagement in NSSI over time. Emerging research, however, has suggested that peer influence may aid understanding around these issues. This information is crucial for informing prevention and early intervention initiatives in this area, which are currently lacking.
Social cognitive theory suggests one way that behaviors are adopted is through the modelling of others; if a role model is respected and/or we identify with them, we are more likely to adopt their behavior (Bandura 1986). Such modelling of others’ behavior appears to be especially powerful during adolescence (Prinstein and Dodge 2008). Developmental researchers have hypothesised that peer behavior is of particular importance during this time, and may be adopted as a basis for identity formation within a social group, social bonding and acceptance, or as comparison when navigating through novel social situations (e.g., Harter et al. 1996; Hartup 1996; Hergovich et al. 2002). This research might help to explain why friends’ engagement in risk behaviors, such as substance use (Allen et al. 2012), delinquency (Gifford-Smith et al. 2005) and promiscuity (Dishion et al. 2012), is a strong predictor of adolescents’ later engagement in these behaviors. More recent research also has begun to suggest that NSSI is another risk behavior susceptible to peer influence. Research assessing the link between friends’ NSSI and individuals’ engagement in this behavior may aid understanding into why young people self-injure when distressed as opposed to engage in other functionally equivalent behaviors, such as substance use or disordered eating.
Anecdotal comments suggest some in the general community believe NSSI is “spread” among young people through exposing wounds and openly discussing the behavior. Evidence of a possible “contagion effect” of NSSI has been found within clinically-based studies, suggesting that exposure to NSSI within inpatient psychiatric facilities has led patients to start self-injuring (e.g., Taiminen et al. 1998). There is also mounting evidence to suggest that contagion of NSSI is present in community-based populations. For example, numerous studies have shown that young people reporting NSSI know more friends who self-injure relative to those not reporting this behavior (Claes et al. 2010) and were more likely to start self-injuring for social motives, including “angry at someone else” and “wanting to fit in with others” (Muehlenkamp et al. 2013). Further, research has shown that peers are frequently cited as providing the initial idea to self-injure (Heath et al. 2009; Deliberto and Nock 2008). Based on this research, it is difficult to untangle whether these individuals are emulating their friend’s behavior or whether apparent contagion effects may reflect associative relationships, whereby individuals with similar risk factors are more likely to become friends (Joiner 1999). Results from a longitudinal study examining peer influence on community-based adolescents’ subsequent engagement in NSSI have been interpreted to support the former explanation. Specifically, Prinstein et al. (2010) showed that, after accounting for depressive symptoms, best friend’s frequency of NSSI at baseline was associated with participant’s frequency of NSSI at follow-up but only among females and students in grade 6. This study represents a valuable contribution to the limited longitudinal evidence regarding the effect of peer influence on future NSSI. However, additional longitudinal research is sorely needed to understand how peers may influence this behavior, in terms of not only severity but also initiation as well as any future engagement. Such information could help to inform prevention and early intervention programs tailored for NSSI as well as help to alleviate the fear of contagion around this behavior, which has led to avoidance of open discussion on this topic in an effort to reduce risk of others self-injuring (McAllister et al. 2010).
While emerging research suggests a role for peer exposure in the development of NSSI among adolescents (Claes et al. 2010; Heilbron and Prinstein 2008; Prinstein et al. 2010), the awareness of NSSI among peers is unlikely to be sufficient to encourage NSSI in the individual. Rather, it is likely that this relationship is moderated (i.e., strengthened or weakened) by a number of factors. Susceptibility to peer influence may be moderated by factors such as age and gender, as shown by Prinstein et al. (2010), or the risk for NSSI may be amplified by psychosocial difficulties among those with friends who self-injure (Heilbron and Prinstein 2008; Prinstein 2007; Prinstein et al. 2001). Prinstein et al. (2001) noted that the relationship between suicidal behavior among friends and adolescents’ suicidal behavior was moderated by family dysfunction, social acceptance, and depression. While demographic factors allow the identification of youth most at risk of susceptibility to peer influence and psychosocial moderators might allow early intervention of modifiable factors, it is also likely that external and/or behavioral factors such as adverse life events and maladaptive coping behaviors cluster in a way that confers increased risk for some youth. Specifically, the relationship between NSSI among peers and an individual’s own NSSI may be amplified by an increased number of adverse life events, substance use and previous suicidal behavior.
Exposure to NSSI among peers may be more likely to encourage NSSI if the young person is already experiencing stressors or adverse life events. Given that NSSI is primarily engaged in as an emotion regulation strategy to cope with intense emotion (e.g., Klonsky 2009), an increased number of adverse life events, which arguably exacerbate negative emotion, may well prove a tipping point between exposure to NSSI among friends and individuals’ NSSI. Adverse life events are an independent predictor of NSSI (Zetterqvist et al. 2012), whereas stressors have been noted to be proximal risk factors (Hankin and Abela 2011). In contrast, Guerry and Prinstein (2009) noted that life events recorded at baseline did not directly predict later NSSI; however, life events did interact with attributional style to predict a worsening trajectory of NSSI over time. Young people who experience numerous adverse events and do not have effective coping strategies may gain the idea to self-injure to regulate emotion from friends who engage in the behavior.
Similarly, substance use is often associated with NSSI (Andrews et al. 2012; Williams and Hasking 2010) although, results are not consistent (Klonsky 2011). While substance use is somewhat normalised among adolescents, heavier substance use tends to be associated with poor coping skills, suggesting that substance use is used as a means of coping (Dow and Kelly 2012). Early onset substance use is associated with increased risk-taking behavior generally (Wu et al. 2010), psychological morbidity, and increased risk of substance dependence (Lee et al. 2010). Concurrent substance use may disinhibit urges to self-injure once the individual has been exposed to NSSI, and/or reduce perception of pain, thus facilitating more severe NSSI, particularly when intoxicated (e.g., Sinclair and Green 2005). For youth who are engaging in heavy substance use, perhaps as a means of coping, exposure to NSSI among friends may provide them with an alternate coping strategy and thus facilitate NSSI. Consequently, substance use may moderate the relationship between peer exposure to NSSI and later NSSI, or may relate to an escalation of NSSI among those who self-injure.
While differentiated from suicidal behavior by definition, NSSI is associated with suicidal ideation and suicide attempts in some people (Brausch and Gutierrez 2010; Hamza et al. 2012; Martin et al. 2010; Zetterqvist et al. 2012). In a large population-based study, Martin et al. (2010) observed that those who had self-injured in the last 4 weeks were 41.6 times more likely to have attempted suicide within the last 12 months than those who did not self-injure. Increasingly, researchers are noting that individuals with a history of both NSSI and suicide attempts report greater psychopathology, more adverse life events and fewer protective factors than those who do not have a history of suicidal behavior (Brausch and Gutierrez 2010; Cloutier et al. 2010; Zetterqvist et al. 2012). Arguably, individuals with a history of suicidal ideation or attempts may be more likely to self-injure in an effort to prevent suicide (Klonsky 2007; Martin et al. 2010; Muehlenkamp and Gutierrez 2004). For youth exposed to NSSI among peers, the risk of subsequent NSSI may be elevated among those who have a history of suicidal behavior. That is, exposure to NSSI by friends may give a suicidal individual an alternative means of “escape” while not being lethal (Claes and Vandereycken 2007). Consequently, a previous history of suicidal ideation or attempts may also moderate the relationship between exposure to NSSI among peers and NSSI in the individual.
Similarly, a growing body of research also has begun to explore the relationship between thinking about NSSI and actually engaging in the behavior. Urges to self-injure typically precede self-injurious acts (Klonsky and Glenn 2008), with more severe and briefer thoughts more likely to precede NSSI (Nock et al. 2009). While exploring protective factors that facilitate resisting these urges (e.g., Klonsky and Glenn 2008; Martin et al. 2011; Washburn et al. 2010) is an important line of enquiry, it is also of interest to determine whether thoughts of NSSI can predict severity of NSSI across a longer time frame, or uniquely predict the onset of the behavior. If more distal thoughts of NSSI have predictive validity, then the first thoughts of NSSI could provide a valuable point for early intervention.
The Current Study
Longitudinal studies are urgently required to clarify the influence and interplay between factors associated with both the severity and onset of NSSI in adolescence. This would place us in a prime position to identify at-risk youth and to develop more effective education, early intervention, and prevention initiatives. As reviewed, peer influence of NSSI may help to explain why adolescents engage in this behavior. However, mechanisms underlying this relationship are not well understood with a lack of prospective studies investigating this topic. To address this gap in knowledge, the current longitudinal study aimed to explore the role of peer exposure to NSSI in predicting NSSI 1 year later, and determine whether adverse life events, substance use, and previous suicidal and nonsuicidal thoughts moderated this relationship, as well as which might predict onset of NSSI within the 1-year study period. In line with the reviewed literature, we hypothesized that knowing someone who self-injures would be related to later NSSI, but this relationship would be moderated by negative life events, substance use and previous suicidal behavior. Finally, we explored which variables were related to severity of NSSI among those who self-injured.
Method
Participants
Participants were surveyed annually at two time points, as part of a larger study on emotional problems in adolescence. At Time 1, 2,637 (12–18 years old; M = 13.9) secondary school students in their first 4 years of high school completed the questionnaire. At the second wave of data collection (Mean follow-up = 11.7 months), 1,973 students (560 males, 1,415 females; 13–19 years old; M = 14.9) participated again and were matched to their baseline data. The retention rate of 75 % is consistent with longitudinal studies examining suicidality (52–82 %; Boergers and Spirinto 2003). Reasons for attrition included transfer to another school (n = 96), school withdrew from the study (n = 114), parent/student withdrew from the study (n = 26), deceased (n = 1), or not present at second questionnaire administration (n = 428). Participants were recruited across five states in Australia from 40 schools (22 Catholic and 18 Non-Government). Majority of participants were in grades 9 (38.9 %) and 10 (31.1 %) at follow-up. Most were born in Australia (89.6 %). Comparisons with Australian Census data indicated females were over-represented in the sample due to participation of several girl-only schools, as were metropolitan areas and areas of higher socio-economic status (SES; Australian Bureau of Statistics, 2008).
Measures
NSSI and Suicidal Behavior
Suicidal behavior and NSSI were assessed with the Self-Harm Behavior Questionnaire (SHBQ; Gutierrez et al. 2001). Participants were asked whether they had ever hurt themselves on purpose, describe what they usually did, and report methods used, recency, frequency and severity (on a scale from not at all serious to life-threatening) of the behavior. As this measure may capture more general self-harm (e.g., overdosing) we examined methods used by participants and only indicated NSSI if external methods of injury were utilised. Participants were also asked whether they had thoughts of, or had ever tried to take their own life. An additional item asked participants if friends engaged in NSSI (Have any of your friends ever hurt themselves on purpose?), how they hurt themselves, and for what reason, in order to ensure methods used aligned with our definition of NSSI. Participants were asked whether they had ever seriously thought about hurting themselves (without actually acting on this thought). SHBQ has acceptable internal consistency across young adults and adolescents in community samples (.89–.96; Brausch and Gutierrez 2010; Gutierrez et al. 2001; Muehlenkamp and Gutierrez 2004) and differentiates between suicidal and non-suicidal young people (Muehlenkamp and Gutierrez 2004). In the current sample α = 0.88.
Psychological Distress
We used the General Health Questionnaire (GHQ-12; Goldberg and Williams 1988), a 12-item screen for anxiety and depression. It has been validated for use in Australian adolescents (Tait et al. 2003) and is a reliable indicator of psychological distress in this population. The measure exhibited good internal consistency in the current sample (α = 0.89).
Adverse Life Events
The Adolescent Life Events Scale (Hawton and Rodham 2006) was used to assess adverse life events. The 20-item checklist asks participants if a range of events has happened to them (e.g., parents fighting, having trouble with school work, getting in trouble with the police), and if so, whether the event occurred within the last 12 months (scored 2) or more than a year ago (scored 1; no occurrence was scored 0). Responses to all items were summated such that higher scores indicated more frequent and more recent negative life events. This allowed us to explore the effect of accumulation of events on NSSI.
Alcohol Use
The Consumption sub-scale of the Alcohol Use Disorders Identification Test (AUDIT; Babor et al. 2001) was used to assess alcohol use by participants. This 3-item subscale asked participants to indicate their usual frequency of consuming alcohol, the number of drinks consumed on a day when drinking alcohol and the frequency of consuming six or more drinks in a single drinking session. Scores range from 0 to 12 with higher scores indicating greater alcohol consumption. In the current sample α = 0.91.
Substance Use
Finally, substance use was assessed by asking a series of questions related to whether participants had ever smoked cigarettes, or tried any of a range of illicit drugs (e.g., marijuana, amphetamines, heroin) provided in a table. Participants were considered as having a history of substance use if they indicated they had tried at least one illicit drug in their lifetime.
Procedure
Ethical approval was obtained prior to the recruitment of participants, from two University Human Research Ethics Committee, and relevant Catholic Education archdioceses. With consent from school principals, an information sheet and consent form was sent home to parents (n = 14,841) of all students in relevant year levels. Students with parental consent (n = 4,119) and at school on the day of questionnaire administration were given their own information sheet and consent form (463 were not present on the day of questionnaire administration; the remainder declined participation). A researcher verbally explained these documents and reminded students that participation was voluntary, responses would remain confidential and they could withdraw at any time without penalty. Students completed the questionnaire during class time, without discussion, in one teaching period (40 min). A researcher was available during and after administration to address issues raised by participation. Students were given information packs about maintaining good mental health as well as contact numbers for any follow-up distress. This procedure was repeated at one-year follow-up, with all measures completed at both time points.
Data Analyses
The nature and extent of NSSI in this sample was explored through descriptive statistics, while gender differences and differences in peer exposure to NSSI were assessed with Chi square tests of independence. Logistic regression was performed to explore which variables could differentiate those who self-injured at follow-up or began NSSI over the study period from those who did not engage in NSSI and multiple regression explored which variables were related to severity of NSSI among those who self-injured. In this analysis, severity was based on the SHBQ score, including frequency, recency, and need for medical attention. In all analyses, predictor variables were those assessed at baseline, while criterion variables were those assessed at follow-up. In accordance with regression guidelines (Cohen et al. 2003), control variables (age, gender, psychological distress, and NSSI at baseline) were entered in the first step, followed by peer exposure. Potential moderators (cigarette smoking, alcohol use, and items related to suicidal behavior) were entered in the third step and all two-way interactions entered in the final step of the regression. The third block initially contained illicit drug use; however, large standard errors rendered the model unstable. As such, this variable was excluded from the logistic regression analyses. Adolescents ceasing NSSI within the study period were excluded from all analyses (n = 81). Multilevel modelling using a generalized mixed model was performed to assess the possible influence of clustering on models examining NSSI at T2, onset of NSSI and severity of NSSI. In all cases, we considered the effect of schools, nested within state, urbanicity (metropolitan or regional), and school denomination (Catholic or Independent).
Results
Preliminary Analyses
Attrition and Missing Data
A series of independent t-tests were used to determine whether there were significant differences between the longitudinal sample (n = 1,973) and the dropout sample (n = 667) using the first wave of data. Adolescents who dropped out at Time 2 (T2) were older (M = 14.11 vs. 13.89; t (2,524) = 4.75, p < .05), and had higher scores on the SHBQ (M = 1.61 vs. 1.02; t (2,466) = 3.42, p < .05) at Time 1 (T1). Expectation–maximization was used to impute <10 % of missing values on all continuous variables (Schafer and Olsen 1998).
Nature and Extent of NSSI
At baseline, 8.4 % (n = 166) adolescents reported a history of NSSI. This increased to 12 % (n = 236) at T2, 31.8 % of whom did not self-injure at baseline (new cases n = 75, 3.8 % of the total sample). Age of onset for those engaging in NSSI at follow-up ranged from 12 to 17 years (M = 14.41; SD = 1.10) with frequency ranging from 1 to 301 episodes (M = 10.82; SD = 32.42), 20.2 % engaging in one episode, 49.3 % 2–5 episodes, 9.0 % 6–10, 7.6 % 11–20 episodes, and 13.9 % 20+ episodes. The most common NSSI was cutting (71.4 %) followed by self-battery (12.0 %), scratching (10.3 %), burning (9.4 %), and other (e.g., biting, 3.8 %). Most NSSI episodes were considered by participants as “not at all serious” (45.9 %) or “needed first aid” (49.1 %) with 4.5 % “requiring medical attention”. One case was “life threatening”; (0.5 %). No gender differences were evident in NSSI at T1, χ2 (1, N = 1,973) = 1.22, p = .27, however females were more likely to self-injure at T2, χ2 (1, N = 1,973) = 11.09, p = .001 (males = 2.3 % of total sample, females = 9.6 % of total sample).
Peer Exposure to NSSI
Of the sample, 28.1 % reported knowing a friend who self-injures. Most knew between 1 and 5 people who self-injured (M = 1.96, SD = 1.86). Reasons provided for their friends’ NSSI primarily related to affect regulation (65.4 %). To influence others or seeking attention was also commonly thought to be the reason for NSSI (12.1 %), while 6.2 % of participants did not know why their friend/s self-injured.
Adolescents who reported any previous history of NSSI in the follow-up questionnaire (i.e., including those who self-injured at baseline) were more likely to have at least one friend who self-injured at baseline (57.8 %, n = 89/155) relative to those never engaging in NSSI (23.5 %, n = 394/1,687), χ2 (1, 1,833) = 83.88, p < .001, and have more friends who self-injured (2.26 vs. 1.69, respectively, t (105.58) = 2.76, p < .01). Primary methods used by adolescents and their friends were largely consistent, χ2 (42, 227) = 70.90, p = .003. This was particularly true for participants who reported friends cutting (adjusted residual = 4.1) and scratching themselves (adjusted residual = 2.7) at baseline. Overall, the motives of friends and participants were not related, χ2 (48, 227) = 55.49, p = .21, although participants who self-injured for self-punishment were more likely to report their friends engaged in self-injury for self-punishment (adjusted residual = 4.1).
Adolescents beginning NSSI by the follow-up period were more likely to have at least one friend who self-injured at baseline (44.6 %; n = 33/75) relative to those who had never engaged in NSSI (23.5 %; n = 394/1,687), χ 2 (1, 1,753) = 16.04, p < .001. However, the number of friends who self-injured did not differ between adolescents reporting onset and adolescents without a history of NSSI (1.90 vs. 1.69, respectively, t (414) = 0.87, p = .38). Primary methods used by adolescents with onset of NSSI by follow-up were not related to methods reported by friends at baseline, χ2 (4, 69) = 1.49, p = .83. Motives for NSSI were also not related, χ2 (28, 70) = 13.49, p = .99.
Predicting Engagement in NSSI
After accounting for schools, nested within state, urbanicity (metropolitan or regional), and school denomination (Catholic or Independent) within a logistic regression model, similar parameter estimates for the factors of interest were found. Further, information criterion suggests that the logistic regression model was preferred over the equivalent logistic mixed models with three random intercepts. Specifically, the logistic regression model had a smaller Akaike Information Criterion (AIC) corrected values (435.76 < 8,553.69) and a smaller Bayesian Information Criterion (BIC) values (494.49 < 8,569.72). A likelihood ratio test also suggested that the logistic mixed model with three random intercepts did not significantly improve the original model, all c 2 (3) = 6.05, p = .10. This additional analysis suggests that the clustering of observations within these higher levels did not largely affect the results. The original logistic regression model is, therefore, reported.
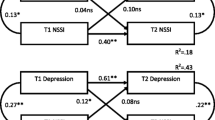
A logistic regression, including all predictors, successfully distinguished the two groups, χ2 (20, N = 1,887) = 356.00, p < .001, explaining between 17.4 % (Cox and Snell R2) and 40.0 % (Nagelkerke R2) of variance in NSSI (see Table 1). Those who self-injured at baseline were almost three times as likely to self-injure at follow-up, with girls more likely to self-injure than boys. Psychological distress and knowing a friend who self-injured increased the odds of reporting NSSI at follow-up. Adverse life events, and previous thoughts of NSSI both predicted NSSI at follow-up. Although the fourth step did not significantly distinguish the groups, two of the interactions successfully distinguished between those who self-injured and those who did not. Given the exploratory nature of this study, we analysed these interactions, although interpretations should be cautious. As seen in Fig. 1, the relationship between knowing a friend who self-injures and NSSI at follow-up was moderated by thoughts of NSSI and adverse life events. Knowing someone who self-injured only increased the likelihood of reporting NSSI at follow-up among those with more adverse life events. Having previously thought about NSSI appeared to decrease the likelihood of engaging in NSSI if participants had a friend who self-injured at baseline.
Onset of NSSI
As with engagement in NSSI at T2, the logistic regression model has smaller AIC values (433.74 < 8,213.02) and a smaller BIC values (486.72 < 8,228.92) than logistic mixed models with random intercepts. A likelihood ratio test also suggested that the logistic mixed model with three random intercepts did not significantly improve the original model, all χ 2 (3) = 5.98, p = .15. The original logistic regression model is, therefore, reported.
Of those who first commenced NSSI over the course of the study, 11.8 % smoked cigarettes, 45.3 % reported knowing a friend who self-injures, 52.0 % reported prior thoughts of NSSI, 30.3 % reported suicidal ideation. Only two participants reported a prior suicide attempt. This variable was subsequently not included in the analyses. When distinguishing those who began NSSI within the year from those with no history of NSSI, the final model successfully distinguished the groups, χ2 (19, N = 1,760) = 108.53, p < .001, explaining between 6.0 % (Cox and Snell R2) and 20.2 % (Nagelkerke R2) of variance. Girls were more likely to begin NSSI within the course of the study, as were those with more psychological distress and those who knew a friend who self-injured (see Table 1).
Predicting the Severity of NSSI
The original multiple regression (AIC = 6,817.75; BIC = 6,823.09) is again reported rather than a model including random intercepts (AIC = 6,823.78; BIC = 6,845.11), χ 2 (3) = 0.0001, p = .99. In bivariate correlations, the severity of NSSI was related to the majority of variables in the expected direction (see Table 2). As hypothesized, the severity of NSSI at baseline was related to NSSI at follow-up (see Table 3). Only smoking cigarettes was associated with NSSI.
Discussion
Although researchers are beginning to reach consensus around key psychological correlates of NSSI, comparatively fewer studies have investigated the role of peers in NSSI during adolescence. We explored whether knowing a friend who self-injured is related to NSSI onset 1 year later, and the moderating roles of adverse life events, substance use and previous suicidal behavior. Results generally supported our hypotheses. Notwithstanding some limitations to the interpretation of the results, knowing a friend who self-injured, life events, psychological distress and thoughts of NSSI differentiated those who self-injured at follow-up from those without a history of NSSI, and predicted the onset of this behavior within the study period. Adverse life events, and previous thoughts of NSSI, moderated the relationship between exposure to self-injuring peers and onset of NSSI at follow-up. However, the effect of having a friend self-injure was not related to the severity of NSSI and the methods and motives for NSSI were largely not related to the methods or motives of friends.
Peer Exposure
Previous research has shown that a substantial proportion of young people receive the initial idea to self-injure from their peers, suggesting that peer exposure to NSSI may contribute to onset of this behavior. The current findings support this assertion, showing that adolescents who started self-injuring at follow-up were more likely to know a friend who self-injured at baseline. Further, knowing a friend who self-injured was also found to increase the risk of onset. These findings build on work by Prinstein et al. (2010) to suggest that exposure to NSSI through friends may not only be related to the frequency of NSSI among adolescents but also the initiation of this behavior. However, the finding that adolescents in the onset group did not know more friends, overall, who self-injured relative to the control group challenges previous work by Claes et al. (2010) showing that those who self-injure have more friends who engage in this behavior. This might refute the notion of a dose–response relationship whereby greater exposure to the behavior infers increased risk. Rather, the quality of the relationship, and the nature of NSSI in a close friend, not the total number of people the individual is exposed to, may be the more salient determinant of future NSSI. Alternatively, a dose–response relationship might be unveiled within individual relationships. For example, the effect of severe and repeated NSSI in a close friend may confer risk beyond that conferred by milder NSSI performed by a more distant acquaintance.
In addition to onset, friends’ NSSI at baseline also was associated independently with any history of NSSI reported at follow-up. Again, this finding builds on previous work to suggest that peer exposure also may play a role in maintenance of NSSI among adolescents in the community. An interesting difference emerged in this group of adolescents relative to the onset group in that adolescents who self-injured over the study follow-up period knew, on average, more friends who self-injured, aligning with findings from Claes et al. (2010). Such a difference may reflect that those continuing to self-injure are more likely to form friendships with others who also self-injure (Joiner 1999), possibly reinforcing this behavior or, alternatively, individual’s engagement in this behavior may influence other friends to start self-injuring. Although further research is needed to elucidate the processes underlying peer exposure, these findings add preliminary insight into how the potential influence of friends’ NSSI may differ with regard to the development or maintenance of NSSI.
It is curious that friends’ NSSI was related to the onset as well as all recent engagement in NSSI, but methods and motives for this behavior were largely inconsistent. One would intuitively expect that the characteristics and functions of NSSI would be modelled in addition to the behavior itself. However, where methods differed with friends’, it appears that more superficial means of NSSI were used, namely scratching and self-battery among those who started NSSI. This finding makes sense in light of literature suggesting that NSSI may be initially mild and become more severe with continued engagement (e.g., Klonsky and Olino 2008). With regard to motives, it might be that adolescents perceived that friends use NSSI as a means of affect regulation. Such motives may have been expressed explicitly by these friends, especially given the stigma around using NSSI to gain attention from others (Crouch and Wright 2004). However, if friends’ engagement in NSSI does contribute to adolescents’ engagement in this behavior, as suggested in this study, then it is reasonable to assume that these individuals would have more social motives for self-injuring, such as influencing others. This interpretation is supported by Muehlenkamp et al. (2013) showing that initial engagement in NSSI among young adults was more likely to be socially motivated relative to motives centring on emotion regulation. Further, there is a myriad of evidence to suggest that social functions may be particularly salient to NSSI among young people in the community (Hilt et al. 2008; Klonsky and Olino 2008; Lloyd-Richardson et al. 2007; Muehlenkamp et al. 2013; Nock 2008), which may be reflected in these adolescents’ personal motives.
In contrast with the above results, peer exposure was not related to severity of NSSI at follow-up. This null association challenges findings from Prinstein et al. (2010) suggesting that best friend’s frequency of NSSI was related to adolescent’s frequency of NSSI at a 1-year follow-up. However, our measure of severity was computed based on not only frequency but also recency and seriousness of wounds. As a result, it might be that peer influence of NSSI may only extend to the frequency of this behavior. As mentioned previously, another explanation might be that the relationship between friend’s NSSI and adolescents’ own subsequent NSSI severity may be largely based on the quality of friendship. Prinstein et al. (2010) examined peer influence effects related to only one best friend, whereas the current study examined the effects of NSSI across adolescents’ broad friendship group with an absence of information regarding the quality of these relationships. It is also important to consider that null associations were found across key variables and NSSI severity. This pattern of results may suggest that these associations suffer from a ceiling effect, especially as this group recorded relatively high levels of psychological distress. However, variation was observed in the severity of NSSI within this group, and bivariate correlations were observed between most variables. The shared variance between NSSI severity at baseline and other variables of interest may preclude significant relationships once the severity of NSSI is controlled. Alternatively, exposure to peer NSSI may influence the decision to engage in NSSI, but is not related to severity. Future research would benefit from exploring the role of peers among those who already have begun to self-injure.
Moderators of Peer Exposure
The findings support previous work showing NSSI among family and friends is associated with NSSI in the individual (Claes et al. 2010; Muehlenhamp et al. 2008; Prinstein et al. 2010), but extends this work to suggest conditions under which this influence might be greatest. Our results appear to suggest that exposure alone is insufficient to encourage NSSI in the individual; however, youth experiencing adverse life events may be swayed by exposure to NSSI among peers, potentially using NSSI as a means of coping (Cawood and Huprich 2011; Hasking et al. 2010). Individuals who self-injure tend to experience elevated arousal in response to stressful events (Nock and Mendes 2008). Likewise, elevated levels of arousal and negative affect prior to NSSI, and resultant decreases after NSSI, have been observed in ecological momentary assessment studies (e.g., Armey et al. 2011; Nock et al. 2009). Arguably, an increased number of adverse life events provides repeated opportunities for young people to experience elevated distress, the cumulative effect of which may exacerbate negative affect and impede adaptive coping. Under such conditions, exposure to NSSI as a potential coping mechanism may appear more attractive to young people.
The apparent protective effect of previously thinking about NSSI seems counter-intuitive. Conceivably, although having considered NSSI, individuals who are close to other people who self-injure have a greater appreciation of the impact on family and friends. As such, they may be dissuaded from engaging in NSSI themselves. Previous research has demonstrated social support and social connectedness are protective against NSSI (Rotolone and Martin 2012). Although speculative, having a close circle of friends may protect against NSSI—regardless of friends’ engagement in NSSI.
Such an interpretation suggests that openly discussing NSSI with young people might be a means of preventing the behavior. Indeed, school based programs may improve knowledge and attitudes towards help-seeking without exerting iatrogenic effects (Muehlenkamp et al. 2010). However, thoughts of NSSI at baseline did directly and positively relate to NSSI at follow-up, and predicted onset of the behavior. These conflicting results suggest a variable in the model is a “suppressor” variable. Examining the bivariate correlations indicates a nonsignificant relationship between peer exposure and the severity of NSSI at follow-up for those who self-injure, which may indicate suppression. Further work exploring how peer exposure is related to NSSI is clearly needed to disentangle these effects.
While social cognitive theory suggests that young people might model NSSI, it is, as yet, not possible to disentangle the effects of associative relationships. Applying this theory to suicidality, Joiner (1999) suggests that shared characteristics of individuals lead to a process of pre-selection, such that individuals with similar risk factors are more likely to become friends. It is equally likely that shared stressors, and/or a shared inability to cope with stress, draw similar people together who then share NSSI as the method to address these pre-existing vulnerabilities. Supporting this, Claes et al. (2010) observed that adolescents who self-injured had more friends who self-injured, but also noted that having friends who self-injured was related to low self-esteem. They suggested that people with low self-esteem sought out self-injurers, or were more vulnerable to copying NSSI once exposed. Similarly, NSSI may be a means of bonding within friendship groups (Nock 2008).
Contrary to hypotheses, substance use was not related to future NSSI in this sample (although cross-sectional correlations were observed). Although commonly comorbid with NSSI (Andrews et al. 2012; Hasking et al. 2008; Martin et al. 2010; Williams and Hasking 2010), there is debate about the exact role. Both substance use and NSSI could be a means of coping with the same underlying issues, substance use may disinhibit the urge to self-injure, or the two behaviors could be distinct, yet be exhibited by the same individual. What is clear from the current study is that substance use is not necessarily an indicator of later NSSI.
Overall, results suggest that rather than seeking to limit exposure to NSSI, it is more important to identify vulnerable youth and help them develop more effective coping skills. Similarly, it is crucial that those often in contact with young people (e.g., teachers, mental health professionals) develop skills in discussing NSSI in such a way as to limit the attraction of NSSI as a coping strategy. Alternatively, it is possible that exposure to NSSI among friends may enlighten young people to negative effects that NSSI can have on individuals as well as those around them. Discussion of the repercussions for loved ones may serve a protective function.
Limitations and Suggestions for Future Research
Although the prospective design is a strength of this study, it is not possible to determine whether exposure to NSSI among peers is a unique risk factor for NSSI or whether individuals with shared pre-existing vulnerabilities are likely to become friends (Joiner 1999). Further longitudinal study will be invaluable in teasing out the observed effects and in establishing directional relationships between the variables. Similarly, our assessment of exposure to NSSI is a potential limitation of the study; future work should include more comprehensive assessments, including the duration and frequency of exposure and the nature of the friendship. Likewise, participants may not have accurately understood the reasons their friends engage in NSSI. However, it could be argued that the perception of the reasons a peer engages in NSSI is more compelling than the actual reason (Bauman and Fisher 1986). In the future, research in this area would be strengthened by obtaining reports both from individuals and their peers directly, to both improve the validity of responses and reduce artificially inflated relationships between the constructs (e.g., Prinstein et al. 2010). Another important avenue for future research is the social context of NSSI; while some individuals self-injure alone, others may do so in group settings. The reasons that individuals within friendship groups self-injure also requires additional research. Gender effects also could be explored in future research. The uneven gender distribution in our sample precluded an examination of whether boys or girls are more susceptible to socialisation effects, although previous research suggests that the relationship between NSSI among friends and an adolescents’ own NSSI may be stronger for girls (Prinstein et al. 2010). Finally, although previous studies have examined each event assessed by the Adolescent Life Events Scale individually, given our small sample for some analyses we chose instead to explore the total impact of cumulative events. Future work would benefit from an exploration of which specific life events may infer increased risk of self-injury.
Conclusion
While not the first study to show socialisation effects over time, our findings contribute to the limited literature supporting the influence of peer exposure to NSSI and later engagement in NSSI. The current findings extend on previous research to show a clear temporal relationship between friends’ NSSI and adolescents’ own engagement in this behavior. Overall, it appears that peer exposure is a risk factor for the onset of NSSI as well as overall subsequent engagement NSSI. Findings also provide preliminary evidence on wider behavioral and external factors that also may increase vulnerability to later NSSI, including adverse life events, psychological distress and thoughts of NSSI. Given the lack of longitudinal evidence on the course of NSSI, these findings provide valuable insight into mechanisms possibly underlying the development and maintenance of this behavior and should help to guide clinical and research efforts in this area. Findings further build on previous work to provide early understanding of the circumstances in which adolescents may be susceptible to peer influence regarding NSSI. Specifically, peer exposure was found to increase the risk of later NSSI among adolescents with more adverse life events, but was not related to the severity of NSSI once an individual begins to self-injure. Together, the findings help to further clarify the onset and maintenance of NSSI over time, adding to a foundational knowledge base that can be used to inform both prevention and early intervention initiatives.
References
Allen, J. P., Chango, J., Szwedo, D., Schad, M., & Marston, E. (2012). Predictors of susceptibility to peer influence regarding substance use in adolescence. Child Development, 83, 337–350. doi:10.1111/j.1467-8624.2011.01682.x.
Andrews, T., Martin, G., & Hasking, P. (2012). Differential and common correlates of non-suicidal self-injury and alcohol use among community-based adolescents. Advances in Mental Health, 11, 55–66.
Armey, M. F., Crowther, J. H., & Miller, I. W. (2011). Changes in ecolgoical momentary assessment reported affect associated with episodes of nonsuicidal self-injury. Behavior Therapy, 42, 579–588.
Australian Bureau of Statistics. (2008). An Introduction to Socio-Economic Indexes for Areas (SEIFA) 2006. Canberra: ABS. (ABS cat no. 2039.0).
Babor, T. F., Higgins-Biddle, J. C., Saunders, J. B., & Monteiro, M. G. (2001). The alcohol use disorders identification test: Guidelines for use in primary care. Geneva: World Health Organisation.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall.
Bauman, K. E., & Fisher, L. A. (1986). On the measurement of friend behavior in research on friend influence and selection: Findings from longitudinal studies of adolescent smoking and drinking. Journal of Youth and Adolescence, 15, 345–353.
Boergers, J., & Spirinto, A. (2003). Follow-up studies of child and adolescent suicide attempters. In R. A. King & A. Apter (Eds.), Suicide in children and adolescents. NY: Cambridge University Press.
Brausch, A. M., & Gutierrez, P. M. (2010). Differences in non-suicidal self-injury and suicide attempts in adolescents. Journal of Youth and Adolescence, 39, 233–242.
Cawood, C. D., & Huprich, S. K. (2011). Late adolescent nonsuicidal self-injury: The roles of coping style, self-esteem, and personality pathology. Journal of Personality Disorders, 25, 765–781.
Claes, L., Houben, A., Vandereycken, W., Bijttebier, P., & Muehlenkamp, J. (2010). Brief report: The association between non-suicidal self-injury, self-concept and acquaintance with self-injurious peers in a sample of adolescents. Journal of Adolescence, 33, 775–778.
Claes, L., & Vandereycken, W. (2007). Self-injurious behavior: Differential diagnosis and functional differentiation. Comprehensive Psychiatry, 48, 137–144.
Cloutier, P., Martin, J., Kennedy, A., Nixon, M. K., & Muehlenkamp, J. (2010). Characteristics and co-occurrence of adolescent non-suicidal self-injury and suicidal behaviors in pediatric emergency crisis sample. Journal of Youth and Adolescence, 39, 259–269.
Cohen, J., Cohen, P., West, S. G., & Aiken, L. S. (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). New Jersey: Lawrence Erlbaum Associates.
Crouch, W., & Wright, J. (2004). Deliberate self-harm at an adolescent unit: A qualitative investigation. Clinical Child Psychology and Psychiatry, 9, 185–204. doi:10.1177/1359104504041918.
Deliberto, T. L., & Nock, M. K. (2008). Exploratory study of the correlates, onset, and offset of non-suicidal self-injury. Archives of Suicide Research, 12, 219–231.
Dishion, T. J., Ha, T., & Véronneau, M. (2012). An ecological analysis of the effects of deviant peer clustering on sexual promiscuity, problem behavior, and childbearing from early adolescence to adulthood: An enhancement of the life history framework. Developmental Psychology, 48, 703–715. doi:10.1037/a0027304.
Dow, S. J., & Kelly, J. F. (2012). Listening to youth: Adolescents’ reasons for substance use as a predictor of treatment response and outcome. Psychology of Addictive Behaviors,. doi:10.1037/a0031065.
Gifford-Smith, M., Dodge, K., Dishion, T. J., & McCord, J. (2005). Peer influence in children and adolescents: Crossing the bridge from developmental to intervention science. Journal of Abnormal Child Psychology, 33, 225–265.
Goldberg, D., & Williams, P. (1988). A user’s guide to the general health questionnaire. Windor, UK: NFER-Nelson.
Guerry, J. D., & Prinstein, M. J. (2009). Longitudinal prediction of adolescent nonsuicidal self-injury: Examination of a cognitive vulnerability-stress model. Journal of Clinical Child and Adolescent Psychology, 39, 77–89.
Gutierrez, P. M., Osman, A., Barrios, F. X., & Kopper, B. A. (2001). Development and initial validation of the self-harm behavior questionnaire. Journal of Personality Assessment, 77, 475–490.
Hamza, C. A., Stewart, S. L., & Willoughby, T. (2012). Examining the link between non-suicidal self-injury and suicidal behavior: A review of the literature and an integrated model. Clinical Psychology Review, 32, 482–495.
Hankin, B. L., & Abela, J. R. Z. (2011). Nonsuicidal self-injury in adolescence: Prospective rates and risk factors in a 21/2 year longitudinal study. Psychiatry Research, 186, 65–70.
Harter, S., Stocker, C., & Robinson, N. S. (1996). The perceived directionality of the link between approval and self-worth: The liabilities of a looking glass self-orientation among young adolescents. Journal of Research on Adolescence, 6, 285–308.
Hartup, W. W. (1996). The company they keep: Friendships and their developmental significance. Child Development, 67, 1–13.
Hasking, P., Coric, S., Swannell, S., Martin, G., Thompson, H., & Frost, A. D. J. (2010). Brief report: Emotion regulation and coping as moderators in the relationship between personality and self injury. Journal of Adolescence, 33, 767–773.
Hasking, P., Momeni, R., Swannell, S., & Chia, S. (2008). The nature and extent of non-suicidal self-injury in non-clinical samples of young adults. Archives of Suicide Research, 12, 208–218.
Hawton, K., & Rodham, K. (2006). By their own young hand. Deliberate self-harm and suicidal ideas in adolescents. London: Jessica Kingsley.
Heath, N. L., Ross, S., Toste, J. R., Charlebois, A., & Nedecheva, T. (2009). Retrospective analysis of social factors and nonsuicidal self-injury among young adults. Canadian Journal of Behavioral Science, 41, 180–186.
Heilbron, N., & Prinstein, M. (2008). Peer influence and adolescent nonsuicidal self-injury: A theoretical review of mechanisms and moderators. Applied and Preventative Psychology, 12, 169–177.
Hergovich, A., Sirsch, U., & Felinger, M. (2002). Self-appraisals, actual appraisals and reflected appraisals of preadolescent children. Social Behavior and Personality, 30, 603–612.
Hilt, L. M., Nock, M. K., Lloyd-Richardson, E. E., & Prinstein, M. J. (2008). Longitudinal study of nonsuicidal self-injury among young adolescents: Rates, correlates, and preliminary test of an interpersonal model. Journal of Early Adolescence, 28, 455–469.
International Society for the Study of Self-Injury (2007). http://www.isssweb.org/aboutnssi.php 2007. Accessed 28 Sep 2012.
Joiner, T. (1999). The clustering and contagion of suicide. Current Directions in Psychological Science, 8, 89–92.
Klonsky, E. D. (2007). The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review, 27, 226–239.
Klonsky, E. D. (2009). The functions of non-suicidal self-injury in young adults who cut themselves: Clarifying the evidence for affect regulation. Psychiatry Research, 166, 260–268.
Klonsky, E.D. (2011). Non-suicidal self-injury in United States adults: Prevalence, sociodemographics, topography and functions. Psychological Medicine, 1–6. doi: 10.1017/S0033291710002497.
Klonsky, E. D., & Glenn, C. R. (2008). Resisting urges to self-injure. Behavioral and Cognitive Psychotherapy, 36, 211–220.
Klonsky, E. D., & Olino, T. M. (2008). Identifying clinically distinct subgroups of self-injurers among young adults: A latent class analysis. Journal of Consulting and Clinical Psychology, 76, 22–27.
Lee, C. S., Winters, K. C., & Wall, M. M. (2010). Trajectories of substance use disorders in youth: Identifying and predicting group memberships. Journal of Child and Adolescent Substance Abuse, 19, 135–157.
Lloyd-Richardson, E., Perrine, N., Dierker, L., & Kelley, M. L. (2007). Characteristics and functions of non-suicidal self-injury in a community sample of adolescents. Psychological Medicine, 37, 1183–1192. doi:10.1017/S003329170700027X.
Martin, J., Bureau, J. F., Cloutier, P., & Lafontaine, M. F. (2011). A comparison of invalidating family environment characteristics between university students engaging in self-injurious thoughts and actions and non-self-injuring university students. Journal of Youth and Adolescence, 40, 1477–1488.
Martin, G., Swannell, S., Hazell, P., Harrison, J., & Taylor, A. (2010). Self-injury in Australia: A community survey. Medical Journal of Australia, 193, 506–510.
McAllister, M., Hasking, P., Estefan, A., McClenaghan, K., & Lowe, J. (2010). A strengths-based group program on self-harm: A feasibility study. Journal of School Nursing, 26, 289–300.
Muehlenhamp, J., Hoff, E., Licht, J., Azure, J., & Hasenzahl, S. (2008). Rates of non-suicidal self-injury: A cross-sectional analysis of exposure. Current Psychology, 27, 234–241.
Muehlenkamp, J., Brausch, A., Quigley, K., & Whitlock, J. (2013). Interpersonal features and functions of non-suicidal self-injury. Suicide and Life-Threatening Behavior, 43, 67–80.
Muehlenkamp, J., & Gutierrez, P. M. (2004). An investigation of differences between self-injurious behavior and suicide attempts in a sample of adolescents. Suicide and Life-Threatening Behavior, 34, 12–23.
Muehlenkamp, J., Walsh, B., & McDade, M. (2010). Preventing non-suicidal self-injury in adolescents: The signs of self-injury program. Journal of Youth and Adolescence, 39, 306–314.
Nock, M. (2008). Actions speak louder than words: An elaborated theoretical model of the social functions of self-injury and other harmful behaviors. Applied and Preventative Psychology, 12, 159–168.
Nock, M. (2010). Self-injury. Annual Review of Clinical Psychology, 6, 339–363.
Nock, M., Joiner, T., Gordon, K., Lloyd-Richardson, E., & Prinstein, M. (2006). Non-suicidal self-injury among adolescents: Diagnostic correlates and relation to suicide. Psychiatry Research, 144, 65–72.
Nock, M. K., & Mendes, W. B. (2008). Physiological arousal, distress tolerance, and social problem-solving deficits among adolescent self-injurers. Journal of Consulting and Clinical Psychology, 76, 28–38.
Nock, M. K., Prinstein, M. J., & Sterba, S. K. (2009). Revealing the form and function of self-injurious thoughts and behaviors: Real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology, 118, 816–827.
Prinstein, M. J. (2007). Moderators of peer contagion: A longitudinal examination of depression socialisation between adolescents and their best friends. Journal of Clinical Child and Adolescent Psychology, 36, 159–170.
Prinstein, M. J., Boergers, J., & Spirito, A. (2001). Adolescents’ and their friends’ health-risk behaviors: Factors that alter or add to peer influence. Journal of Paediatric Psychology, 26, 287–298.
Prinstein, M. J., & Dodge, K. A. (2008). Peer influence processes among youth. New York: Guilford.
Prinstein, M. J., Heilbron, N., Guerry, J. D., Franklin, J. C., Rancourt, D., Simon, V., et al. (2010). Peer influence and non-suicidal self-injury: Longitudinal results in community and clinically-referred adolescent samples. Journal of Abnormal Child Psychology, 38, 669–682.
Rotolone, C., & Martin, G. (2012). Giving up self-injury: A comparison of everyday social and personal resources in past versus current self-injurers. Archives of Suicide Research, 16, 147–158.
Schafer, J. L., & Olsen, M. K. (1998). Multiple imputation for multivariate missing-data problems: A data analyst’s perspective. Multivariate Behavioral Research, 33, 545–571.
Sinclair, J., & Green, J. (2005). Understanding resolution of deliberate self harm: Qualitative interview study of patients experiences. British Medical Journal, 330, 1112.
Taiminen, T. J., Kallio-Soukainen, K., Nokso-Koivisto, H., Kaljonen, A., & Kelenius, H. (1998). Contagion of deliberate self-harm among adolescent inpatients. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 211–217.
Tait, R. J., French, D. J., & Hulse, G. K. (2003). Validity and psychometric properties of the general health questionnaire-12 in young Australian adolescents. Australian and New Zealand Journal of Psychiatry, 37, 374–381.
Washburn, J. J., Juzwin, K. R., Styer, D. M., & Aldridge, D. (2010). Measuring the urge to self-injure: Preliminary data from a clinical sample. Psychiatry Research, 178, 540–544.
Williams, F., & Hasking, P. A. (2010). Emotion regulation, coping and alcohol use as moderators in the relationship between self-injury and psychological distress. Prevention Science, 11, 33–41.
Wu, J., Witkiewitz, K., McMahon, R. J., & Dodge, K. A. (2010). A parallel process growth mixture model of conduct problems and substance use with risky sexual behavior. Drug and Alcohol Dependence, 111, 207–214.
Zetterqvist, M., Lundh, L., & Svedin, C. G. (2012). A comparison of adolescents engaging in self-injurious behaviors with and without suicidal intent: Self-reported experiences of adverse life events and trauma symptoms. Journal of Youth and Adolescence. doi:10.1007/s10964-012-9872-6.
Acknowledgments
This study was funded by the Australian Research Council. We would like to acknowledge the work of research staff Sophie Aitken, Emily Berger and Grace Skrzypiec (all Monash University) and Lauren Friend (University of Queensland), and research students Teryn Callaway, Megan Wisewould and Alicia Tanner (all Monash University) who assisted with data collection and entry.
Author contributions
PH and TA conceptualised the study, TA performed statistical analyses, PH wrote the majority of the manuscript, GM and PH designed the study, GM assisted with preparation of the manuscript for publication. All authors have read the manuscript and approve it for submission.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hasking, P., Andrews, T. & Martin, G. The Role of Exposure to Self-Injury Among Peers in Predicting Later Self-Injury. J Youth Adolescence 42, 1543–1556 (2013). https://doi.org/10.1007/s10964-013-9931-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10964-013-9931-7