Abstract
The interplay between intrapersonal risk (low self-esteem, perfectionism and body dissatisfaction) and interpersonal protection (social support) appears relevant for delineating gender-specific pathways that lead to both depressive and eating psychopathology. The aims of this longitudinal study were to examine gender differences in the levels of depressive symptoms, disordered eating and the co-occurrence of both problems from preadolescence to mid-adolescence and to identify gender-specific risk and protective factors of depressive symptoms and disordered eating. A Spanish community-based sample initially comprising 942 early adolescents (49% females) was assessed at baseline (T1; X age = 10.8 years) and at 2 and 4-year follow-up (T2 and T3). Gender differences emerged at T2 for disordered eating and at T3 for depressive symptoms and for co-occurring depressive symptoms and disordered eating. Predictors of depressive symptoms were body dissatisfaction, low self-esteem and fear of getting fat, for girls, and body dissatisfaction and low self-esteem, for boys. Predictors of disordered eating were body dissatisfaction, depressive symptoms, BMI and perfectionism, for girls, and low social support and BMI, for boys. In addition, for boys only, social support moderated the effect of body dissatisfaction on depressive symptoms and the effect of depressive symptoms on disordered eating. The hypotheses of the study were partially supported. Clinical implications are derived regarding the components that should be included in programs for preventing depression and eating disorders in both girls and boys.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gender differences in both depression and eating disorders are well-known and have received considerable attention in past research. However, most studies generally have discussed either depression or eating disorders, with relatively few attempts to integrate results from both fields. The lack of integrative findings is even more pronounced regarding the subclinical manifestations of these disturbances. Nevertheless, the use of subthreshold measures of affective and eating psychopathology is justified for several reasons. Firstly, many questions have arisen in relation to whether current categories of depressive and eating disorders adequately reflect their respective spectrum of disturbances (Panagiotakopoulou and Kontaxaki 2007; Walsh and Sysko 2009). Secondly, subsyndromal manifestations of psychopathology are likely to evolve into full syndromes (Chamay-Weber et al. 2005; Fergusson et al. 2005). Lastly, many adolescents may not meet diagnostic criteria for a disorder but nonetheless experience the negative consequences of having such a disorder (Chamay-Weber et al. 2005; Lewinsohn et al. 1998). Consequently, it is worthwhile investigating the potential similarities underlying the gendered nature of depressive and eating disturbances by examining the subclinical levels of these forms of psychopathology.
Both depression and eating disorders are characterized by being overrepresented in females. Although the timing of gender differences varies depending on the outcome assessed, it is generally assumed that the gender disparity in the rates of internalizing symptoms and disorders first appears in adolescence (Hayward and Sanborn 2002). The transition from preadolescence to adolescence, therefore, represents a critical period in which to explore gender differences in mental health. For girls, the preponderance of depressive symptoms or depressed mood consistently emerges between the ages of 13 and 15 years (Ferreiro et al. 2011; Ge et al. 1994). Regarding disordered eating, no clear timeline for the development of gender differences has been established, although the gender gap in self-reported eating problems may arise just after the age of 10 or 11 years (Adams et al. 1993; Ohzeki et al. 1993). As far as the co-occurrence of affective and eating disturbances is concerned, there is strong evidence indicating high comorbidity rates between depression and eating disorders in females (Godart et al. 2007). However, little is known about the chronology of gender differences in the co-occurrence of the subsyndromal manifestations of depressive and eating psychopathology during adolescence.
Together with possible parallels in epidemiological features, it is also reasonable to postulate the existence of overlapping etiological mechanisms for affective and eating psychopathology. In fact, eating disturbances are supposed to cause affective problems (Stice et al. 2000), and vice versa (Beato-Fernández et al. 2007). There also may be many risk factors common to both types of disturbance (Bulik 2002; McCarthy 1990). Since the scope of this study is limited and taking into account that affective and eating problems are defined as internalizing difficulties, we will focus only on a subset of variables that appear to be particularly relevant in this field, namely, certain intrapersonal attributes with clear implications for the manner in which individuals perceive and judge themselves. This outlook is justified by a common observation; i.e., that negative self-evaluative processes appear to be a central component of both affective and eating problems. In this regard, it is well known that depressed individuals tend to feel worthless and guilty (American Psychiatric Association 2000). In fact, dysfunctional attitudes and inferences about the self play an essential role in some of the most widely accepted theories of depression (Abramson et al. 1989; Beck 1987). Likewise, disruptions in the sense of self appear in nearly all descriptions of patients with eating disorders (Ewell et al. 1996). As a result, a number of clinicians and researchers have implicated maladaptive self-representations as one of the key factors in the development of appearance-related disturbances (Bers et al. 2004; Cooper 1997; Strauman et al. 1991). Among all the constellation of variables reflecting self-perceptions and expectancies, we believe that three deserve special attention given their frequent appearance in the literature on both affective and eating problems: self-esteem, perfectionism and body dissatisfaction.
Intrapersonal Variables as Risk Factors
Self-esteem, conceptualized as a person’s overall appraisal of their own value, is undoubtedly one of the most important parts of an individual’s self-concept and identity. Moreover, self-esteem is widely recognized as central to psychological functioning and is related to many other variables, including general satisfaction with one’s life (Kim 2003). It is, therefore, not surprising that low self-esteem in adolescence predicts a variety of negative outcomes (e.g., Trzesniewski et al. 2006). In this respect, low self-esteem is thought to exert causal influence in the onset of depression. In fact, there is evidence that low self-esteem prospectively contributes to high levels of depression, whereas the reverse is not true (Orth et al. 2008). Low self-esteem also is related consistently to disordered eating. Indeed, low self-esteem has been suggested as a necessary prerequisite to the development of an eating disorder (Silverstone 1992). However, as posited in the review by Jacobi et al. (2004), most studies addressing the association between low self-esteem and eating psychopathology have not considered the precedence of low self-esteem to the eating-related outcome or any possible confounding effect of concurrent depressive symptomatology. In addition, the apparent strong relationship between low self-esteem and disordered eating may be partly due to the high correlation between low self-esteem and body dissatisfaction, as reported elsewhere (Chen et al. 2007; Gianini and Smith 2008). Consequently, low self-esteem may be a more salient predictor of depressive symptoms than of disordered eating.
Perfectionism—specifically self-oriented perfectionism—is also a fundamental construct for understanding the role of intrapersonal conditions in jeopardizing one’s emotional well-being. Although perfectionism includes both adaptive and maladaptive components (Hamachek 1978), it has usually been studied as a negative characteristic consisting of striving for unrealistically high standards. Perfectionism is supposed to confer risk for depression. In this regard, both self-oriented perfectionism (demanding perfection of oneself) and socially prescribed perfectionism (perceiving that others are demanding perfection of oneself) appear to be connected with depression (Hewitt and Flett 1991). There also appears to be a strong relationship between self-critical perfectionism and depression (Clara et al. 2007). Nevertheless, much previous research on the relationship between perfectionism and affective disturbances is cross-sectional. Considering the limited prospective research in this area, the data suggest that perfectionism may result in increased vulnerability to depressive symptoms following stressful life events, rather than leading by itself to such increased vulnerability (Enns and Cox 2005; Flett et al. 1995). In terms of eating psychopathology, it has been suggested that the core features of both anorexia nervosa and bulimia nervosa (e.g., the pursuit of a perfect body) are inherently perfectionistic (Goldner et al. 2002). Moreover, a recent review of personality and eating disorders has concluded that there is longitudinal evidence that perfectionism may be a predisposing factor for eating disorders (Lilenfeld et al. 2006). It is also interesting to note that self-oriented perfectionism has emerged as more specific to eating disorders than to depressive disorders (Castro-Fornieles et al. 2007). Thus, there is more consistent support for the role of perfectionism as a risk factor for disordered eating than as a risk factor for depressive symptoms.
Body dissatisfaction refers to the negative evaluation of one’s body overall or of particular body parts. This variable has been established as a central aspect of self-worth and mental health across the lifespan (Harter 1990). However, the combination of adolescents’ changing physical appearance, their increasing capacity for introspection and their heightened interest in dating may render them particularly vulnerable to excessive preoccupation with their own attractiveness. In fact, satisfaction with one’s physical appearance is probably the most critical source for global self-esteem during adolescence (Harter 1999). Not surprisingly, body dissatisfaction has been most studied in relationship to eating disturbances. Nevertheless, nowadays, appearance-related factors also have come into prominence in several theories of depression (Hankin and Abramson 2001; Hyde et al. 2008; Stice et al. 2000). In this regard, a number of prospective studies with adolescents have found body dissatisfaction or negative body image as a significant predictor of both depressive mood (Holsen et al. 2001; Paxton et al. 2006) and disordered eating (Allen et al. 2008; Graber et al. 1994). Interestingly, it is subjective perceptions of one’s body rather than objective body size that appear to be relevant in predicting mental health problems (Al Mamun et al. 2007). Indeed, a review by Stice (2002) posits that body dissatisfaction is a robust risk factor for both negative affect and eating psychopathology. It, therefore, appears that body dissatisfaction may play a substantial role in predicting both depressive symptoms and disordered eating in adolescence.
The Protective Effect of the Interpersonal Context
According to the above evidence, low self-esteem, perfectionism and body dissatisfaction may operate as internal dispositions that increase the risk of developing both depressive and eating disturbances, with different levels of specificity for each problem in each case. A useful further step in understanding when these psychopathological mechanisms take place involves the exploration of factors that may moderate the deleterious effect of dysfunctional self-related attributes on mental health. In this regard, examining the interplay between intrapersonal characteristics and interpersonal provisions appears promising. Specifically, social support is assumed to be a salient environmental resource, as the experience that one is loved, cared for and valued by others is logically expected to protect against many undesirable outcomes. In fact, an inverse association between social support and both depressive symptoms (Galambos et al. 2004; Santos et al. 2007) and disordered eating (Santos et al. 2007; Stice et al. 2002) has been well-documented. Furthermore, social support appears to be especially effective in protecting us from ourselves, as it appears to buffer the effect of rumination on negative affect (Puterman et al. 2010) and to decrease the likelihood of making maladaptive inferences regardless of one’s stable cognitive vulnerability to depression (Panzarella et al. 2006). In addition, higher levels of social support are associated with a weaker relationship between eating disturbances and a variety of risk factors (Skomorovsky et al. 2006; Wonderlich-Tierney and Vander Wal 2010). Consequently, it can be assumed that social support may attenuate the risk incurred by negative internal dispositions for both depressive symptoms and disordered eating.
Gender Differences in the Influence of Risk and Protective Factors
An additional aspect that should be addressed for delineating the vulnerability to depressive symptoms and disordered eating alludes to gender differences in the influence of both risk and protective factors. Since both depressive and eating psychopathology are clearly gendered phenomena, it can be argued that the influence of etiological factors may vary by gender. This gender-related causation hypothesis appears to be true for the reciprocal relationship between depressive and eating disturbances. In this regard, a salient body of research indicates that eating-related factors may confer additional risk for depression in adolescent girls, but not in boys (Bearman and Stice 2008; Stice et al. 2000). In addition, longitudinal data support the existence of a female-specific pathway from negative affect to the development of eating disturbances (Beato-Fernández et al. 2007; Jackson and Chen 2008). With respect to self-related aspects, there is evidence that adolescent girls tend to be more self-conscious (Rankin et al. 2004) and ruminate more (Jose and Brown 2008) than their male counterparts. It also has been claimed that females may be better at identifying what they lack, in contrast to males, who may be better at identifying what they have (Garaigordobil and Durá 2006). Thus, low self-esteem, perfectionism and body dissatisfaction may be more detrimental for well-being in girls than in boys. In fact, there is some support for this assertion. According to several studies, low self-esteem may be a better risk factor for subsequent depression or depressive symptoms in girls than in boys (Ferreiro et al. 2011; Pelkonen et al. 2003). Likewise, there is cross-sectional (Muris et al. 2005; Santos et al. 2007) and longitudinal (Allen et al. 2008) evidence that the association between low self-esteem and disordered eating is only significant for adolescent females. It also has been reported that the different dimensions of perfectionism may relate to depressive symptoms in different ways in girls and boys (Rice et al. 2007). Moreover, perfectionism (Forbush et al. 2007), or at least self-oriented perfectionism (Bento et al. 2010), appears to be more consistently associated with disordered eating in females than in males. Body dissatisfaction also has proved to be associated both concurrently (Fung et al. 2010) and prospectively (Bearman and Stice 2008) with depression in girls, but not in boys. In addition, some data indicate that body dissatisfaction may predict extreme weight change behaviors (McCabe and Ricciardelli 2006) and abnormal eating behaviors (Beato-Fernandez and Rodriguez-Cano 2005) in adolescent females rather than in males. Finally, gender differences in the buffering effect of social support also may have been assumed. Gender-related issues in the interpersonal domain have been studied widely from different theoretical approaches. Briefly, it has been posited that females are socialized to display strong affiliative behavior and thus become more sensitive than males to what occurs in their social relationships (e.g., Cambron et al. 2009; Cyranowski et al. 2000; Rudolph 2002). From this perspective, girls should benefit more than boys from the protective effect of social support. Consistent with this, social support has been found to attenuate the impact of stressful circumstances on depressive symptoms to a greater extent in females than in males (Landman-Peeters et al. 2005). In contrast, to our knowledge, gender disparity in the protective effect of social support against eating disturbances has not previously been tested.
Overview
In summary, the evidence reviewed above highlights the need for further investigation of gender-sensitive features of both depressive and eating psychopathology. This interest takes diverse forms, from the examination of gender differences in the levels of depressive symptoms, disordered eating and the co-occurrence of both outcomes to the identification of unique etiologies in the development of each of these disturbances for girls versus boys. A prospective methodology is sorely needed in tackling these issues. Systematic exploration of the development of subsyndromal manifestations of both depressive and eating psychopathology across adolescence may be helpful for understanding the trajectories of each of these disturbances and their co-occurrence, as well as for elucidating the timing of gender differences in each case. Moreover, clarifying how risk and protective factors for depressive symptoms and disordered eating may overlap or differ across both types of psychopathology and both genders is a fundamental step in generating relevant knowledge for designing gender-specific prevention and treatment strategies for both of these problems. In this regard, the distinction between intrapersonal risk (low self-esteem, perfectionism and body dissatisfaction) an interpersonal protection (social support) provides a useful framework for delineating a causal mechanism underlying both affective and eating-related outcomes.
The Current Study
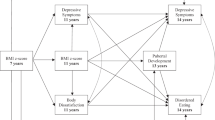
Taking into account the current status of this field of research, the present study was designed to address two main goals. The first goal was to explore gender differences in the levels of depressive symptoms, disordered eating and the co-occurrence of both problems from preadolescence to mid-adolescence. The second goal was to examine the risk and protective factors of depressive symptoms and disordered eating for each gender. A number of variables were explored as potential risk and protective factors for affective and eating disturbances. Firstly, disordered eating was examined as a potential risk factor for depressive symptoms, and vice versa. Secondly, three intrapersonal variables were considered as potential risk factors for both depressive and eating psychopathology: low self-esteem, perfectionism and body dissatisfaction. Thirdly, Body Mass Index also was included as a potential risk factor for these outcomes, in order to distinguish the effect of this objective variable from the effect of the subjective variable body dissatisfaction. Finally, one interpersonal factor was regarded as a potential protective factor against depressive and eating disturbances: social support.
As far as the first goal is concerned, we expected to find that the gender difference in depressive symptoms would emerge at between the ages of 13 and 15 years (between T2 and T3) and also that the gender difference in disordered eating would emerge at between the ages of 11 and 13 years (between T1 and T2). No specific hypotheses were offered concerning the emergence of gender differences in the co-occurrence of depressive symptoms and disordered eating because of the lack of empirical research on this topic.
With respect to the second goal, we formulated a number of hypotheses related to the comparison between disturbances and the comparison between genders. As regards the comparison between disturbances, it was hypothesized, first, that disordered eating would predict depressive symptoms, and vice versa. It also was assumed that the risk factors for depressive symptoms and disordered eating would overlap to a greater or lesser extent depending on each particular case. Specifically, the second hypothesis was that low self-esteem would be a better predictor of depressive symptoms than of disordered eating; the third hypothesis was that perfectionism would be a better predictor of disordered eating than of depressive symptoms; and the fourth hypothesis was that body dissatisfaction would have a large impact on both outcomes. Additionally, the fifth hypothesis was that body dissatisfaction, and not BMI, would predict both depressive symptoms and disordered eating. Finally, social support was expected to attenuate the effect of the intrapersonal risk factors on both depressive symptoms and disordered eating.
As regards the comparison between genders, we expected to find, first, that the reciprocal relationship between depressive symptoms and disordered eating would be stronger in females than in males. Second, it was assumed that the intrapersonal risk factors (low self-esteem, perfectionism and body dissatisfaction) would be better predictors of both depressive symptoms and disordered eating in girls than in boys. Third, social support was hypothesized to buffer the effect of the intrapersonal risk factors on depressive symptoms in girls but not in boys. Finally, no specific hypotheses were made about gender differences in the role of social support as a protective factor against disordered eating because of the absence of published studies on this particular issue.
For these purposes, we conducted a 4-year longitudinal study with a large community-based sample of adolescent girls and boys. Measurements were made across three waves, each 2 years apart (T1, T2 and T3), so that different critical ages between pre-adolescence and mid-adolescence were captured.
Method
Participants
To recruit the study sample, 12 public and state-assisted schools were randomly selected as representative of coastal and inland areas in the province of A Coruña (Spain). The sample at Time 1 (T1) comprised 942 pupils, 465 girls (M age = 10.84; SD = 0.74) and 477 boys (M age = 10.83; SD = 0.75). At Time 2 (T2), 93.6% of the students, 437 girls (M age = 12.84; SD = 0.77) and 445 boys (M age = 12.85; SD = 0.77), were re-evaluated. Finally, at Time 3 (T3), 84.8% of the initial sample, 376 girls (M age = 14.98; SD = 0.84) and 372 boys (M age = 14.99; SD = 0.85), completed further assessment. The response rate was 99% at T1, 97% at T2 and 98% at T3. The sample comprised 98.5 Caucasians, 1% Moroccans and 0.5% “others”. Participants covered all social and cultural backgrounds of the targeted population. Attrition analyses revealed no significant differences on either demographic or clinical variables between the participants who dropped out at T2 or T3 and those available at all assessment points.
Measures
Sociodemographic Data
All the participants provided data regarding gender, age, residence (rural or urban) and level of parents’ education (primary, secondary or higher).
Depressive Symptoms
The Children’s Depression Inventory (CDI; Kovacs 1992) was designed to evaluate depressive symptoms in children and adolescents. The Spanish version of the CDI used in this study has shown adequate internal consistency, test–retest reliability, and concurrent and convergent validity (del Barrio et al. 1999). As recommended by the author of the questionnaire, a cut-off point of 19 was applied. The alpha coefficient was .85 for girls and .84 for boys at T1, .85 for girls and .86 for boys at T2, and .86 for girls and .85 for boys at T3.
Disordered Eating
The Children’s Eating Attitudes Test (ChEAT; Maloney et al. 1988) was utilized to detect disordered eating. The Spanish version of the ChEAT used in this study has exhibited satisfactory internal consistency and concurrent validity (Senra et al. 2007). A score of 15 was considered the cut-off point, following the recommendations of Sancho et al. (2005). The responses to items 5, 15 and 25 were omitted at all three assessment points and the responses to items 9 and 26 were omitted at T1 because they were considered unsuitable for the age group studied (Senra et al. 2007).
As the ChEAT includes diverse items, a principal components analysis with varimax rotation was applied to explore the factor structure of the inventory. The analysis revealed four factors: (a) Fear of getting fat (α: T1 = .90 for girls and .86 for boys; T2 = .86 for both; T3 = .86 for girls and .83 for boys); (b) Dieting (α: T1 = .68 for both; T2 = .81 for girls and .80 for boys; T3 = .86 for girls and .77 for boys); (c) Bulimic symptoms (α: T1 = .77 for girls and .62 for boys; T2 = .55 for girls and .63 for boys; T3 = .74 for girls and .70 for boys); and (d) Social pressure to eat (α: T1 = .72 for both; T2 = .80 for girls and .79 for boys; T3 = .78 for both). For this research, only the first three factors were considered. The composition of the factors was similar to that reported in other studies (Sancho et al. 2005; Senra et al. 2007).
Self-Esteem
The Rosenberg Self-Esteem Scale (RSES; Rosenberg 1989) was designed to evaluate global self-esteem. The Spanish version of the RSES used in this study (Echeburúa 1995) has shown high internal consistency and test–retest reliability, and acceptable validity (Vázquez et al. 2004). Four of the 10 items of the original RSES were selected as the most suitable for the age at T1. The correlation between the short form and the standard form at T2 was .88, thus supporting the adequacy of the measure used at T1. The alpha coefficient was .85 for girls and .88 for boys at T1, and .85 for girls and .81 for boys at T2.
Perfectionism
The Perfectionism subscale of the EDI-2 (Garner 1991) evaluates the degree to which someone considers that they should excel in personal results. The Perfectionism subscale of the Spanish version of the EDI-2 has been found to be a reliable and valid measure (Corral et al. 1998). The alpha coefficient of the Perfectionism subscale was .78 for girls and .71 for boys at T1, and .68 for girls and .69 for boys at T2.
Body Dissatisfaction
The Body Dissatisfaction subscale of the Eating Disorder Inventory-2 (EDI-2; Garner 1991) measures overall body dissatisfaction and dissatisfaction with particular body parts. The Body dissatisfaction subscale of the Spanish version of the EDI-2 has shown adequate reliability and validity (Corral et al. 1998). The alpha coefficient of the Body Dissatisfaction subscale was .83 for girls and .79 for boys at T1, and .90 for girls and .86 for boys at T2.
Body Mass Index (BMI)
All the participants were weighed with an electronic precision balance and measured with a portable height measuring device. BMI was calculated from the formula: BMI = weight (kg)/height (m)2. BMI is a valid measure of adiposity (Garrow and Webster 1985).
Social Support
Perceived social support was assessed by three items (“Do you feel loved by your family?”, “Do you feel supported by your family?”, “Do you feel loved by your friends?”) scored on a Likert-type scale ranging from 1(not at all) to 4 (a lot). The alpha coefficient was .83 for girls and .82 for boys at T1, and .75 for girls and boys at T2.
Procedure
The research was approved by the Bioethics Committee at the University of Santiago de Compostela and the Regional Government (Xunta de Galicia). Permission to carry out the study was obtained from the head teachers of all schools. Informed consent was also obtained from the parents of the adolescents who took part in the study.
Self-report questionnaires were completed in classes of 20–25 students. Two research assistants remained in the classroom throughout the study session in order to answer any questions and prevent communication among the pupils. All adolescents were weighed and measured without footwear, under conditions of privacy and confidentiality.
Results
Preliminary Analyses
One-way analyses of variance (ANOVAs) were carried out to determine if there were age-related differences in the predictive variables at T1 (range 9–12 years) and T2 (range 11–14 years). The results only showed significant differences in the predictive variables at T2 for girls. Age was, therefore, introduced as a covariate in the multivariate analyses including these measures.
The correlations between criterion variables and predictive variables for each gender and the corresponding means and standard deviations are presented in Table 1. The results of t tests comparing girls and boys are also shown. Girls scored higher than boys in depressive symptoms at T3, disordered eating at T3, body dissatisfaction at T1 and T2 and fear of getting fat at T2, whereas boys scored higher than girls for self-esteem at T1, dieting at T1 and bulimic symptoms at T1 and T2.
Gender Differences in the Levels of Depressive Symptoms, Disordered Eating and the Co-Occurrence of Both Problems
The percentage of cases with depressive symptoms, disordered eating and the co-occurrence of both problems was calculated from the database for those participants available at all three assessment points (N = 718).
As regards depressive symptoms, 8.7% (T1), 11.2% (T2) and 16.8% (T3) of the girls and 9.1% (T1), 10.4% (T2) and 8.7% (T3) of the boys obtained scores equal to or above the cut-off point in the CDI. The female:male ratio was 0.9:1 at T1, 1.1:1 at T2 and 1.9:1 at T3. Gender differences were significant at T3 (χ2 = 9.71; p < .01), but not at T1 (χ2 = 0.02; ns) or T2 (χ2 = 0.11; ns). Change over time in the percentage of cases with depressive symptoms was calculated using McNemar’s test for each gender. For girls, there was a significant increase in depressive symptoms from T1 to T3 (p < .001) and from T2 to T3 (p < .05). For boys, there were no significant changes in depressive symptoms.
With respect to disordered eating, 14.6% (T1), 23.6% (T2) and 27.2% (T3) of the girls and 20.1% (T1), 17.5% (T2) and 8.4% (T3) of the boys obtained scores equal to or above the cut-off point in the ChEAT. The female:male ratio was 0.7:1 at T1, 1.3:1 at T2 and 3.2:1 at T3. Gender differences were significant at T2 (χ2 = 3.99; p < .05) and T3 (χ2 = 42.37; p < .001), but not at T1 (χ2 = 3.35; ns). McNemar’s test revealed that, for girls, there was a significant increase in disordered eating from T1 to T2 (p < .001) and from T1 to T3 (p < .001). For boys, there was a significant decrease in disordered eating from T1 to T3 (p < .001) and from T2 to T3 (p < .001).
Concerning the co-occurrence of depressive symptoms and disordered eating, 2.5% (T1), 5.1% (T2) and 9.8% (T3) of the girls and 3.1% (T1), 4.2% (T2) and 1.9% (T3) of the boys obtained scores equal to or above the cut-off point in both the CDI and the ChEAT. The female:male ratio was 0.8:1 at T1, 1.2:1 at T2, and 5.1:1 at T3. Gender differences were significant at T3 (χ2 = 19.50; p < .001), but not at T1 (χ2 = 0.39; ns) or T2 (χ2 = 0.26; ns). McNemar’s test revealed that, for girls, there was a significant increase in the co-occurrence from T1 to T3 (p < .001) and from T2 to T3 (p < .01). For boys, there were no significant changes in the co-occurrence.
Risk and Protective Factors of Depressive Symptoms and Disordered Eating
A series of hierarchical multiple regression analyses were performed to determine the contribution of the predictive variables at T1 and T2 to depressive symptoms and disordered eating at T3 and to examine whether social support moderated the effect of any of the predictive variables on any of the outcomes. Separate analyses were conducted for girls and boys, for depressive symptoms and disordered eating and for predictive variables at T1 and T2. Before carrying out the analyses, all the variables were centered to reduce multicollinearity between first-order terms and interaction terms (Holmbeck 1997). Moreover, the number of potential predictors in each regression was reduced by selecting only those variables significantly correlated with the corresponding outcome (see Table 1). In the first step, the baseline (T1 or T2) level of the outcome was entered as a covariate. In the second step, the predictive variables were entered as main effects. In the third step, the products between social support and each of the other predictive variables were added as interaction terms.
The significant effects for the prediction of depressive symptoms are summarized in Table 2. For girls, the variables at T1 that significantly contributed to depressive symptoms at T3 were the covariate, self-esteem and, marginally, fear of getting fat, whereas the significant predictors at T2 were the covariate and body dissatisfaction. No significant moderator effects of social support were found. For boys, the significant predictors at T1 of depressive symptoms at T3 were the covariate, body dissatisfaction, self-esteem and the interaction between social support and body dissatisfaction, whereas the significant predictors at T2 were the covariate and, marginally, body dissatisfaction. Post hoc tests of the interaction at T1 between social support and body dissatisfaction were carried out according to Holmbeck (2002). These tests revealed that there was a positive and significant association between body dissatisfaction and future depressive symptoms for boys with low social support (t = 4.36; p < .001), but not for boys with high social support (t = 0.43; ns).
The significant effects found for the prediction of disordered eating are summarized in Table 3. For girls, the variables at T1 that significantly contributed to disordered eating at T3 were the covariate, depressive symptoms, BMI and perfectionism, whereas the significant predictors at T2 were the covariate and body dissatisfaction. No significant moderator effects of social support were found. For boys, the significant predictors at T1 of disordered eating at T3 were the covariate, social support, BMI and the interaction between social support and depressive symptoms, whereas the significant predictors at T2 were the covariate and social support. Post hoc tests of the interaction at T1 between social support and depressive symptoms revealed that there was a positive and significant association between depressive symptoms and future disordered eating for boys with low social support (t = 2.03; p < .05), but not for boys with high social support (t = 0.55; ns).
Discussion
Although girls’ affective and eating problems have raised many questions regarding the possible interrelated nature of these forms of psychopathology (Ferreiro et al. 2011; Hayward and Sanborn 2002), no extensive research has been devoted to clarifying how the developmental trajectories of the subclinical manifestations of these two disturbances and their etiological factors may differ from each other and by gender. This longitudinal study was designed to address these shortcomings by examining the timing of gender differences in depressive symptoms, disordered eating and the co-occurrence of both outcomes from pre-adolescence to mid-adolescence and also the risk and protective factors for both disturbances in both girls and boys. Given the limited scope of the study, emphasis was placed on a number of intrapersonal attributes (low self-esteem, perfectionism and body dissatisfaction) that might confer risk for both outcomes, as well as on the role of a salient interpersonal factor (social support) that might moderate the relationships between internal dispositions and psychopathology. All the etiological mechanisms postulated were expected to be more relevant for females than for males. Our hypotheses were partially supported.
The first aim of this research was to analyze gender differences in the levels of depressive symptoms, disordered eating and the co-occurrence of both problems across the study time. In accordance with our hypotheses, a female preponderance in depressive symptoms emerged at some point between the ages of 13 and 15 years and clearly was established by the age of 15 years, when almost twice as many girls as boys were suffering depressive symptoms. This is consistent with prior longitudinal studies (Ferreiro et al. 2011; Ge et al. 1994). Moreover, in line with previous data (Ge et al. 1994; Twenge and Nolen-Hoeksema 2002), we found that girls, but not boys, were at greater risk for developing depressive symptoms as they grew older. Therefore, there is convincing evidence that adolescence is a critical period in which depressive psychopathology escalates distinctively in girls as compared to boys.
Also supporting our hypotheses, gender differences in disordered eating first appeared at the age of 13 years and became more pronounced at the age of 15 years, with girls being, respectively, around 1.5 and 3 times more likely than boys to display eating psychopathology. These findings reinforce cross-sectional evidence indicating that no gender differences in eating problems are noted before the age of 10 or 11 years (Adams et al. 1993; Ohzeki et al. 1993) and that the gender discrepancy in weight and eating concerns escalates with age (Richards et al. 1990). The proportion of cases with disordered eating increased over time for girls and decreased over time for boys. Other studies using the ChEAT or the EAT have not yielded conclusive results for girls, documenting either a rise in the risk with age (Ohzeki et al. 1993) or a steady trend (Halliwell and Harvey 2006). However, these divergent results are probably caused by the different age ranges investigated. In fact, when large spans from pre-adolescence to adolescence are considered, older girls do show more abnormal eating behavior than younger girls. Also in accordance with our results, there is strong support for a decline in the ChEAT or EAT scores of adolescent males as they grew older (Halliwell and Harvey 2006; Ohzeki et al. 1993). Nevertheless, as it has been suggested that the onset of eating disorders may occur somewhat later in males than in females (Muise et al. 2003), we think that the high proportion of boys with self-reported disordered eating at early ages may partly reflect an artifact indicating a tendency for males to overeat as they approach their growth spurt.
Gender differences in the co-occurrence of depressive symptoms and disordered eating did not arise until the age of 15 years, when the proportion of girls to boys with both types of symptoms was roughly 5:1. Although this topic needs further exploration, our findings clearly indicate mid-adolescence as a critical stage for females to engage in a significant level of interrelated affective and eating disturbances. Moreover, this converges with cross-sectional results showing a higher percentage of co-occurrence of depressive symptoms and disordered eating for females than for males by the age of 16 years (Santos et al. 2007). We also found a rise in the cases of co-occurrence over time in girls. Again, this is consistent with a previous report that the proportion of females with co-occurring depressive and eating problems increases from early adolescence to mid-adolescence (Graber and Brooks-Gunn 2001).
The second aim of this study was to identify the risk and protective factors of depressive symptoms and disordered eating for each gender. Concerning this goal, mixed evidence was found in favor of our hypotheses. The most robust predictor of depressive symptoms in both girls and boys was the initial level of depressive symptoms, which clearly resembles the well-known statement that the best predictor of future behavior is past behavior. In addition, low self-esteem and fear of getting fat at T1 and body dissatisfaction at T2 predicted depressive symptoms in girls. Low self-esteem at T1 and body dissatisfaction at T1 and T2 predicted depressive symptoms in boys. Interestingly, social support moderated the impact of body dissatisfaction at T1 on depressive symptoms at T3, although only in boys. On the other hand, the most prominent predictor of disordered eating in both girls and boys also was disordered eating at previous assessments. Furthermore, depressive symptoms, BMI and perfectionism at T1 and body dissatisfaction at T2 predicted disordered eating in girls. Low social support at T1 and T2 and BMI at T1 were significant predictors of disordered eating in boys. A moderator effect of social support on the relationship between depressive symptoms at T1 and disordered eating at T3 was also found in boys. These results merit a number of comments in relation to their implications for understanding how certain etiological processes may differ depending on both the type of psychopathology and gender.
In reference to the comparison between disturbances, the findings supported our hypothesis that depressive symptoms and disordered eating would influence each other. In particular, pathways from the fear of getting fat to depressive symptoms and from depressive symptoms to disordered eating were identified. Thus, rather than a unidirectional association, affective and eating problems appear to be reciprocally related. We also found evidence that low self-esteem is somewhat specific to depressive symptoms, whereas perfectionism is more specific to disordered eating. Moreover, body dissatisfaction was confirmed as a relevant risk factor for both depressive and eating psychopathology. Together, these results suggest that negative attitudes about oneself predispose adolescents to both affective and eating disturbances. Nevertheless, the content of the self-related beliefs and feelings leading to each outcome may differ slightly. A poor sense of self-worth, implicit in low self-esteem, appears to be particularly salient for affective problems. Consistent with this, negative thoughts and inferences about oneself are central mechanisms involved in both the cognitive theory of depression (Beck 1987) and the hopelessness theory of depression (Abramson et al. 1989). In contrast, striving for excessively high self-standards appears to be particularly critical for entering into a spiral of disordered eating. This is not surprising, as anorexic patients have been described, since the first clinical reports in this field, as individuals who try to achieve perfection in every area of their lives (Bruch 1978). In a similar vein, Sawdon et al. (2007) found that the discrepancy between actual self and potential self distinguished eating disordered patients from those who were primarily depressed. It could, therefore, be stated that self-perceptions contributing to depression are based on who you are, whereas self-perceptions associated with eating disorders are focused on who you may become. On the other hand, the emergence of body dissatisfaction as an evaluative dimension linked to both types of psychopathology is quite revealing. In particular, this finding shows that negative self-perceptions related to body image may act as a common pathway toward depressive and eating problems, thereby supporting the role of appearance-related concerns as a highly motivationally significant domain in adolescents (Hankin and Abramson 2001). In other words, perceived physical attractiveness appears to be central to defining oneself as a person during adolescence, which may render adolescents who experience body dissatisfaction particularly vulnerable to developing different forms of psychopathology.
It should also be noted that, contrary to our expectations, BMI at T1 (and not body dissatisfaction) predicted disordered eating in both girls and boys. However, when examining the effects of predictive variables at T2, it was body dissatisfaction (and not BMI) that predicted disordered eating in girls. As a result, it appears that objective body size may act as a risk factor for disordered eating at early ages, whereas the subjective perception of one’s body may become the main predictor as youths grow older and gain introspective capacity. In the case of depressive symptoms, fear of getting fat and body dissatisfaction arose as significant predisposing factors, whereas BMI did not. It, therefore, appears that BMI itself does not increase the risk of developing depression, but concerns about weight and shape do compromise emotional well-being. Thus, this is coherent with previous findings underlining the importance of the perception of being overweight rather than measured overweight as a precursor of depression (Al Mamun et al. 2007).
Some noteworthy findings were obtained regarding social support. On the one hand, low social support by itself turned out to be a predictor of disordered eating. On the other hand, social support moderated the impact of certain risk factors on both depressive and eating psychopathology. As these results only appeared for boys, we will discuss their implications in further detail when examining gender differences in the risk and protective factors assessed. However, it could be posited that the effect of low social support on its own appears to be particularly detrimental as regards developing eating problems rather than affective problems, whereas social support appears to interact with several risk factors to predict both affective and eating difficulties. Specifically, social support buffered the effect of body dissatisfaction on depressive symptoms and the effect of depressive symptoms on disordered eating. Thus, as hypothesized, social support may be depicted as an interpersonal resource attenuating the effect of maladaptive internalizing conditions. In other words, social support appears to protect us from ourselves, as previously claimed (Puterman et al. 2010). In addition, our findings extend cross-sectional evidence on the role of social support as a safeguard against the impact of different risk factors on both negative affect (Puterman et al. 2010) and eating disturbances (Skomorovsky et al. 2006; Wonderlich-Tierney and Vander Wal 2010).
The results also allow us to make relevant comparisons by gender. As expected, the reciprocal relationship between depressive symptoms and disordered eating was more evident for females than for males. Specifically, only for girls, fear of getting fat at T1 predicted depressive symptoms and, in turn, depressive symptoms at T1 predicted disordered eating. This is, therefore, connected with a number of studies suggesting a stronger link between affective and eating problems for females than for males (Bearman and Stice 2008; Beato-Fernández et al. 2007). It should be noted that depressive symptoms also predisposed boys to disordered eating, but only in those with low social support. In contrast, the results only provided partial support for our hypothesis that the intrapersonal variables investigated would be better predictors of psychopathology in females than in males. In this regard, low self-esteem emerged as a predictor of depressive symptoms for both girls and boys. This finding contradicts previous evidence (Ferreiro et al. 2011; Pelkonen et al. 2003). This discrepancy may reflect differences in the age range studied or the analyses performed. However, Orth et al. (2008) found that the structural relation between self-esteem and depression was not affected by gender. Consequently, the relationship among self-esteem, depressive symptoms and gender requires further exploration. In contrast, perfectionism turned out to be a predictor of disordered eating only in girls. This finding converges with cross-sectional studies indicating that perfectionism or certain of its dimensions are more consistently associated with abnormal eating behaviors in females than in males (Bento et al. 2010; Forbush et al. 2007). As a result, it could be asserted that some traits traditionally attributed to girls with eating disorders may not be applicable to boys. On the other hand, body dissatisfaction predicted depressive symptoms in both girls and boys. Once again, this shows the relevance of appearance-related concerns in adolescence. Moreover, it may suggest that physical appearance no longer has a different meaning and importance in females and males, as suggested elsewhere (Seidah and Bouffard 2007). Nevertheless, body dissatisfaction did emerge as a female-specific risk factor for disordered eating. This is in accordance with prospective evidence that body dissatisfaction may be particularly detrimental for eating behavior in females (Beato-Fernandez and Rodriguez-Cano 2005; McCabe and Ricciardelli 2006). In this respect, it has been suggested that disordered eating in boys may be related to the desire for an athletic figure rather than a leaner shape and, as a consequence, male-specific body concerns may not be accurately captured by traditional measures of body dissatisfaction (Ricciardelli and McCabe 2004; Senra et al. 2007).
Gender differences were particularly remarkable concerning the role of social support. Low social support on its own turned out to be a male-specific predictor of disordered eating. To our knowledge, this is a new finding. However, it appears to extend cross-sectional evidence showing that males with eating disturbances tend to display more problems in social functioning than their female counterparts (Joiner et al. 2000). In fact, Joiner and colleagues posited that gender differences between bulimic females and males align along two dimensions: on the one hand, women are more preoccupied with their weight; on the other hand, men experience more interpersonal difficulties. It is, therefore, possible that eating psychopathology arises as an attempt to cope with different concerns in girls and boys. Furthermore, social support emerged as a protective factor against depressive symptoms and disordered eating in boys, but not in girls. In particular, social support moderated the association between body dissatisfaction at T1 and depressive symptoms at T3, as well as the association between depressive symptoms at T1 and disordered eating at T3. In other words, it was only boys with low social support for whom body dissatisfaction predicted depressive symptoms and for whom depressive symptoms predicted disordered eating. This result, therefore, not only contradicts the hypothesized higher female sensitivity to interpersonal relationships but also suggests that social context may do less to modify vulnerability to internalizing psychopathology in girls than in boys. Moreover, whereas the sole presence of body dissatisfaction or depressive symptoms appears sufficient to lead girls to negative outcomes, the additive effect of these factors and low social support appears necessary to compromise boys’ well-being. In this regard, the male-specific role of certain protective mechanisms may help explain the higher rates of depression and eating disorders in females.
This study also provides us with additional information about age-related differences regarding the prediction of both affective and eating disturbances. In this regard, it should be noted that the predictive power of the models was always higher at T2 than at T1, thus highlighting the stronger role of more proximal influences than more distal ones in predicting both depressive symptoms and disordered eating. In line with this, previous longitudinal studies have found that the impact of different risk factors on depressive and eating problems is generally greater when the span separating the predictors and the outcome is shorter (Gardner et al. 2000; Karevold et al. 2009). However, it appears that the length of the follow-up intervals determined the magnitude of the autoregressive parameters (from depressive symptoms at T1 and T2 to depressive symptoms at T3 and from disordered at T1 and T2 to disordered eating at T3), so that the shorter the time between one measurement and the other, the higher the test–retest correlation. Moreover, each point in time can be described as a sensitive period in which youths are vulnerable to different risk factors. The age of 11 years was found to be a period of unspecific risk wherein a variety of factors predicted depressive symptoms and disordered eating in both girls and boys. In contrast, as youths progressed through adolescence, body dissatisfaction (in both girls and boys) and low social support (in boys) became the most important predictors of the variables studied. In relation to this, physical appearance and social relationships are core features in the adolescent transition (Arnett 2010). In contrast, the moderator effects of social support on internalizing risk factors were only found at T1. It can, therefore, be speculated that social context may be more likely to interact with self-related perceptions and feeling at early ages, when youths have not yet achieved full autonomous thinking and self-regulatory processes.
Limitations and Future Directions
There were a number of limitations in the present study. Firstly, although we determined the proportion of high-scorers in the CDI and the ChEAT, these data cannot be considered equivalent to prevalence rates of depression and eating disorders. Secondly, by using a broad measure of disordered eating, the possible differences between anorexic and bulimic features may have been obscured. Thirdly, social support was assessed with a brief scale developed by the research team, so that the results may not be directly comparable to others. Fourthly, although most of the instruments utilized in this study are commonly used in research, several of them may be biased toward the aesthetic ideals and risky eating behaviors of girls. Consequently, the different nature of weight and eating attitudes in females and males might make it necessary to use gender-specific instruments for assessing these constructs. Finally, although a longitudinal design was used, a non-experimental design does not enable us to rule out the influence of extraneous variables. Therefore, causal inferences must be made with caution.
With regard to future directions, several suggestions can be made. Firstly, further research is needed to replicate our findings for different local conditions and ethnic backgrounds. Secondly, future studies also could incorporate other assessment methods such as multi-informant reports or diagnostic interviews. Thirdly, expansion of the investigation to consider a larger battery of biopsychosocial variables would be useful. Fourthly, recommendations also include the exploration of risk factors for depressive symptoms and disordered eating over longer intervals—from childhood to late adolescence or beyond. Finally, as risk factors may be interrelated, possible mediation mechanisms should be explored.
Conclusions
This study confirmed that, throughout adolescence, girls outnumber boys in depressive symptoms, disordered eating and the co-occurrence of both disturbances. Such a female preponderance appears to consolidate somewhat earlier for disordered eating (13 years) than for depressive symptoms and the co-occurrence of both types of psychopathology (15 years). Moreover, only for girls, increasing age was associated with increasing risk of endorsing depressive symptoms, disordered eating and both outcomes. On the other hand, both common and different intrapersonal variables arose as predictors of depressive symptoms and disordered eating. Moreover, some relevant gender differences were found as regards prediction of these outcomes. Reciprocal relationships between affective and eating problems were more evident for girls than for boys, whereas social support protected boys rather than girls from both affective and eating problems. Taken together, these findings may contribute to a better understanding of gender differences in the epidemiology and etiology of the subclinical manifestations of both depressive and eating disturbances in adolescence.
We believe that the study is notable for the multiwave, prospective design and the large community-based sample of adolescents. The results are also particularly valuable as replications of prior findings in the Spanish population, which clearly has been under-investigated in comparison with the North American population. Furthermore, the study produced some novel findings—such as the role of low social support in the predictive models for boys—which merit further exploration.
Several clinical implications may be derived from the results. Firstly, prevention programs for affective and eating psychopathology should begin before the surge in these disturbances in early to mid-adolescence. Secondly, targeted interventions should be aimed not only at girls but also at boys, particularly those lacking a protective social network. Thirdly, it appears necessary to intervene in body dissatisfaction, self-esteem, fear of getting fat and social support to reduce the incidence of depression, as well as to intervene in body dissatisfaction, depressive symptoms, obesity, perfectionism and social support to reduce the incidence of eating disorders. Fourthly, in the case of females, preventive strategies for depression may be effective in preventing eating disorders, and vice versa, as there appear to be reciprocal influences in both disturbances. Fifthly, in the case of males, reinforcing social support is assumed to be particularly useful in order to decrease the likelihood of both depression and eating disorders. Finally, prevention and intervention programs should be aimed at providing general skills at early ages (preadolescence) and then increasingly narrowed to focus on body-image concerns and social relationships (early to mid-adolescence). We hope that these guidelines will serve to enhance our ability to design gender-specific prevention and intervention strategies for depressive and eating psychopathology, so that the incidence and severity of such serious problems for adolescents can be effectively reduced in the future.
References
Abramson, L. Y., Metalsky, G. I., & Alloy, L. B. (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96, 358–372.
Adams, P. J., Katz, R. C., Beauchamp, K., Cohen, E., & Zavis, D. (1993). Body dissatisfaction, eating disorders, and depression: A developmental perspective. Journal of Child and Family Studies, 2, 37–46.
Al Mamun, A., Cramb, S., McDermott, B. M., O’Callaghan, M., Najman, J. M., & Williams, G. M. (2007). Adolescents’ perceived weight associated with depression in young adulthood: A longitudinal study. Obesity, 15, 3097–3105.
Allen, K. L., Byrne, S. M., McLean, N. J., & Davis, E. A. (2008). Overconcern with weight and shape is not the same as body dissatisfaction: Evidence from a prospective study of pre-adolescent boys and girls. Body Image, 5, 261–270.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: Author.
Arnett, J. J. (2010). Adolescence and emerging adulthood: A cultural approach (4th ed.). Upper Saddle River, NJ: Pearson.
Bearman, S. K., & Stice, E. (2008). Testing a gender additive model: The role of body image in adolescent depression. Journal of Abnormal Child Psychology, 36, 1251–1263.
Beato-Fernandez, L., & Rodriguez-Cano, T. (2005). Gender differences regarding psychopathological, family and social characteristics in adolescents with abnormal eating behavior. Eating Behaviors, 6, 337–344.
Beato-Fernández, L., Rodríguez-Cano, T., Pelayo-Delgado, E., & Calaf, M. (2007). Are there gender-specific pathways from early adolescence psychological distress symptoms toward the development of substance use and abnormal eating behavior? Child Psychiatry and Human Development, 37, 193–203.
Beck, A. T. (1987). Cognitive models of depression. Journal of Cognitive Psychotherapy, 1, 5–37.
Bento, C., Pereira, A. T., Maia, B., Marques, M., Soares, M. J., Bos, S., et al. (2010). Perfectionism and eating behaviour in Portuguese adolescents. European Eating Disorders Review, 18, 328–337.
Bers, S. A., Blatt, S. J., & Dolinsky, A. (2004). The sense of self in anorexia-nervosa patients: A psychoanalytically informed method for studying self-representation. The Psychoanalytic Study of the Child, 59, 294–315.
Bruch, H. (1978). The golden cage: The enigma of anorexia nervosa. Cambridge, MA: Harvard University Press.
Bulik, C. M. (2002). Anxiety, depression, and eating disorders. In C. G. Fairburn & K. D. Brownell (Eds.), Eating disorders and obesity: A comprehensive handbook (2nd ed., pp. 193–198). New York, NY: Guilford Press.
Cambron, M. J., Acitelli, L. K., & Pettit, J. W. (2009). Explaining gender differences in depression: An interpersonal contingent self-esteem perspective. Sex Roles, 61, 751–761.
Castro-Fornieles, J., Gual, P., Lahortiga, F., Gila, A., Casulà, V., Fuhrmann, C., et al. (2007). Self-oriented perfectionism in eating disorders. International Journal of Eating Disorders, 40, 562–568.
Chamay-Weber, C., Narring, F., & Michaud, P.-A. (2005). Partial eating disorders among adolescents: A review. Journal of Adolescent Health, 37, 417–427.
Chen, Q., Fu, D., Chen, W., & Wang, J. (2007). Influence of self-esteem in eating disorders: The mediation effect of body dissatisfaction. Chinese Journal of Clinical Psychology, 15, 290–292.
Clara, I. P., Cox, B. J., & Enns, M. W. (2007). Assessing self-critical perfectionism in clinical depression. Journal of Personality Assessment, 88, 309–316.
Cooper, M. (1997). Cognitive theory in anorexia nervosa and bulimia nervosa: A review. Behavioural and Cognitive Psychotherapy, 25, 113–145.
Corral, S., González, M., Pereña, J., & Seisdedos, N. (1998). Adaptación española del Inventario de Trastornos de la Conducta Alimentaria EDI2. [Spanish adaptation of the Eating Disorder Inventory EDI2]. Madrid: TEA.
Cyranowski, J. M., Frank, E., Young, E., & Shear, M. K. (2000). Adolescent onset of the gender difference in lifetime rates of major depression: A theoretical model. Archives of General Psychiatry, 57, 21–27.
del Barrio, M. V., Moreno, C., & López, R. (1999). El children’s depression inventory (CDI; Kovacs, 1992). Su aplicación en población española. [The Children’s Depression Inventory (CDI; Kovacs, 1992) in a Spanish sample]. Clínica y Salud, 10, 393–416.
Echeburúa, E. (1995). Evaluación y tratamiento de la fobia social. [Assessment and treatment of social phobia]. Barcelona: Martínez Roca.
Enns, M. W., & Cox, B. J. (2005). Perfectionism, stressful life events, and the 1-year outcome of depression. Cognitive Therapy and Research, 29, 541–553.
Ewell, F., Smith, S., Karmel, M. P., & Hart, D. (1996). The sense of self and its development: A framework for understanding eating disorders. In L. Smolak, M. P. Levine, & R. Striegel-Moore (Eds.), The developmental psychopathology of eating disorders: Implications for research, prevention, and treatment (pp. 107–133). Mahwah, NJ: Lawrence Erlbaum Associates.
Fergusson, D. M., Horwood, L. J., Ridder, E. M., & Beautrais, A. L. (2005). Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry, 62, 66–72.
Ferreiro, F., Seoane, G., & Senra, C. (2011). A prospective study of risk factors for the development of depression and disordered eating in adolescents. Journal of Clinical Child and Adolescent Psychology, 40, 500–505.
Flett, G. L., Hewitt, P. L., Blankstein, K. R., & Mosher, S. W. (1995). Perfectionism, life events, and depressive symptoms: A test of a diathesis-stress model. Current Psychology, 14, 112–137.
Forbush, K., Heatherton, T. F., & Keel, P. K. (2007). Relationships between perfectionism and specific disordered eating behaviors. International Journal of Eating Disorders, 40, 37–41.
Fung, S. S. W., Stewart, S. M., Ho, S. Y., Wong, J. P. S., & Lam, T. H. (2010). Body dissatisfaction, maternal appraisal, and depressive symptoms in Hong Kong adolescents. International Journal of Psychology, 45, 453–460.
Galambos, N. L., Leadbeater, B. J., & Barker, E. T. (2004). Gender differences in and risk factors for depression in adolescence: A 4-year longitudinal study. International Journal of Behavioral Development, 28, 16–25.
Garaigordobil, M., & Durá, A. (2006). Relaciones del autoconcepto y la autoestima con la sociabilidad, estabilidad emocional y responsabilidad en adolescentes de 14 a 17 años. [Relationships of self-concept and self-esteem to sociability, emotional stability and responsibility in adolescents aged 14 through 17 years]. Análisis y Modificación de Conducta, 32, 37–64.
Gardner, R. M., Stark, K., Friedman, B. N., & Jackson, N. A. (2000). Predictors of eating disorder scores in children ages 6 through 14: A longitudinal study. Journal of Psychosomatic Research, 49, 199–205.
Garner, D. M. (1991). Eating disorder inventory-2: Professional manual. Odessa, FL: Psychological Assessment Resources.
Garrow, J. S., & Webster, J. (1985). Quetelet’s index (W/H2) as a measure of fatness. International Journal of Obesity, 9, 147–153.
Ge, X., Lorenz, F. O., Conger, R. D., Elder, G. H., Jr., & Simons, R. L. (1994). Trajectories of stressful life events and depressive symptoms during adolescence. Developmental Psychology, 30, 467–483.
Gianini, L. M., & Smith, J. E. (2008). Body dissatisfaction mediates the relationship between self-esteem and restrained eating in female undergraduates. International Journal of Behavioral Consultation and Therapy, 4, 48–60.
Godart, N. T., Perdereau, F., Rein, Z., Berthoz, S., Wallier, J., Jeammet, P., et al. (2007). Comorbidity studies of eating disorders and mood disorders. Critical review of the literature. Journal of Affective Disorders, 97, 37–49.
Goldner, E. M., Cockell, S. J., & Srikameswaran, S. (2002). Perfectionism and eating disorders. In G. L. Flett & P. L. Hewitt (Eds.), Perfectionism: Theory, research, and treatment (pp. 319–340). Washington, DC: American Psychological Association.
Graber, J. A., & Brooks-Gunn, J. (2001). Co-occurring eating and depressive problems: An 8-year study of adolescent girls. International Journal of Eating Disorders, 30, 37–47.
Graber, J. A., Brooks-Gunn, J., Paikoff, R. L., & Warren, M. P. (1994). Prediction of eating problems: An 8-year study of adolescent girls. Developmental Psychology, 30, 823–834.
Halliwell, E., & Harvey, M. (2006). Examination of a sociocultural model of disordered eating among male and female adolescents. British Journal of Health Psychology, 11, 235–248.
Hamachek, D. E. (1978). Psychodynamics of normal and neurotic perfectionism. Psychology, 15, 27–33.
Hankin, B. L., & Abramson, L. Y. (2001). Development of gender differences in depression: An elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin, 127, 773–796.
Harter, S. (1990). Developmental differences in the nature of self-representations: Implications for the understanding, assessment and treatment of maladaptive behavior. Cognitive Therapy and Research, 14, 113–142.
Harter, S. (1999). The construction of the self: A developmental perspective. New York, NJ: Guilford Press.
Hayward, C., & Sanborn, K. (2002). Puberty and the emergence of gender differences in psychopathology. Journal of Adolescent Health, 30, 49–58.
Hewitt, P. L., & Flett, G. L. (1991). Dimensions of perfectionism in unipolar depression. Journal of Abnormal Psychology, 100, 98–101.
Holmbeck, G. N. (1997). Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology, 65, 599–610.
Holmbeck, G. N. (2002). Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology, 27, 87–96.
Holsen, I., Kraft, P., & Røysamb, E. (2001). The relationship between body image and depressed mood in adolescence: A 5-year longitudinal panel study. Journal of Health Psychology, 6, 613–627.
Hyde, J. S., Mezulis, A. H., & Abramson, L. Y. (2008). The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychological Review, 115, 291–313.
Jackson, T., & Chen, H. (2008). Predicting changes in eating disorder symptoms among adolescents in China: An 18-month prospective study. Journal of Clinical Child and Adolescent Psychology, 37, 874–885.
Jacobi, C., Hayward, C., de Zwaan, M., Kraemer, H. C., & Agras, W. S. (2004). Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin, 130, 19–65.
Joiner, T. E., Jr., Katz, J., & Heatherton, T. F. (2000). Personality features differentiate late adolescent females and males with chronic bulimic symptoms. International Journal of Eating Disorders, 27, 191–197.
Jose, P. E., & Brown, I. (2008). When does the gender difference in rumination begin? Gender and age differences in the use of rumination by adolescents. Journal of Youth and Adolescence, 37, 180–192.
Karevold, E., Røysamb, E., Ystrom, E., & Mathiesen, K. S. (2009). Predictors and pathways from infancy to symptoms of anxiety and depression in early adolescence. Developmental Psychology, 45, 1051–1060.
Kim, Y. -H. (2003). Correlation of mental health problems with psychological constructs in adolescence: Final results from a 2-year study. International Journal of Nursing Studies, 40, 115–124.
Kovacs, M. (1992). The children’s depression inventory (CDI). Manual. Toronto, Ontario: Multi Health Systems.
Landman-Peeters, K. M. C., Hartman, C. A., van der Pompe, G., den Boer, J. A., Minderaa, R. B., & Ormel, J. (2005). Gender differences in the relation between social support, problems in parent-offspring communication, and depression and anxiety. Social Science and Medicine, 60, 2549–2559.
Lewinsohn, P. M., Rohde, P., & Seeley, J. R. (1998). Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clinical Psychology Review, 18, 765–794.
Lilenfeld, L. R. R., Wonderlich, S., Riso, L. P., Crosby, R., & Mitchell, J. (2006). Eating disorders and personality: A methodological and empirical review. Clinical Psychology Review, 26, 299–320.
Maloney, M. J., McGuire, J. B., & Daniels, S. R. (1988). Reliability testing of a children’s version of the eating attitude test. Journal of the American Academy of Child and Adolescent Psychiatry, 27, 541–543.
McCabe, M. P., & Ricciardelli, L. A. (2006). A prospective study of extreme weight change behaviors among adolescent boys and girls. Journal of Youth and Adolescence, 35, 425–434.
McCarthy, M. (1990). The thin ideal, depression and eating disorders in women. Behaviour Research and Therapy, 28, 205–215.
Muise, A. M., Stein, D. G., & Arbess, G. (2003). Eating disorders in adolescent boys: A review of the adolescent and young adult literature. Journal of Adolescent Health, 33, 427–435.
Muris, P., Meesters, C., van de Blom, W., & Mayer, B. (2005). Biological, psychological, and sociocultural correlates of body change strategies and eating problems in adolescent boys and girls. Eating Behaviors, 6, 11–22.
Ohzeki, T., Otahara, H., Hanaki, K., Motozumi, H., & Shiraki, K. (1993). Eating attitudes test in boys and girls aged 6–18 years: Decrease in concerns with eating in boys and the increase in girls with their ages. Psychopathology, 26, 117–121.
Orth, U., Robins, R. W., & Roberts, B. W. (2008). Low self-esteem prospectively predicts depression in adolescence and young adulthood. Journal of Personality and Social Psychology, 95, 695–708.
Panagiotakopoulou, A., & Kontaxaki, M.-I. (2007). Continuum and spectrum hypotheses of depressive disorders. Psychiatriki, 18, 239–250.
Panzarella, C., Alloy, L. B., & Whitehouse, W. G. (2006). Expanded hopelessness theory of depression: On the mechanisms by which social support protects against depression. Cognitive Therapy and Research, 30, 307–333.
Paxton, S. J., Neumark-Sztainer, D., Hannan, P. J., & Eisenberg, M. E. (2006). Body dissatisfaction prospectively predicts depressive mood and low self-esteem in adolescent girls and boys. Journal of Clinical Child and Adolescent Psychology, 35, 539–549.
Pelkonen, M., Marttunen, M., & Aro, H. (2003). Risk for depression: A 6-year follow-up of Finnish adolescents. Journal of Affective Disorders, 77, 41–51.
Puterman, E., DeLongis, A., & Pomaki, G. (2010). Protecting us from ourselves: Social support as a buffer of trait and state rumination. Journal of Social and Clinical Psychology, 29, 797–820.
Rankin, J. L., Lane, D. J., Gibbons, F. X., & Gerrard, M. (2004). Adolescent self-consciousness: Longitudinal age changes and gender differences in two cohorts. Journal of Research on Adolescence, 14, 1–21.
Ricciardelli, L. A., & McCabe, M. P. (2004). A biopsychosocial model of disordered eating and the pursuit of muscularity in adolescent boys. Psychollogical Bulletin, 130, 179–205.
Rice, K. G., Leever, B. A., Noggle, C. A., & Lapsley, D. K. (2007). Perfectionism and depressive symptoms in early adolescence. Psychology in the Schools, 44, 139–156.
Richards, M. H., Casper, R. C., & Larson, R. W. (1990). Weight and eating concerns among pre- and young adolescent boys and girls. Journal of Adolescent Health Care, 11, 203–209.
Rosenberg, M. (1989). Society and the adolescent self-image (rev. ed.). Middeltown, CT: Wesleyan University Press.
Rudolph, K. D. (2002). Gender differences in emotional responses to interpersonal stress during adolescence. Journal of Adolescent Health, 30, 3–13.
Sancho, C., Asorey, O., Arija, V., & Canals, J. (2005). Psychometric characteristics of the children’s eating attitudes test in a Spanish sample. European Eating Disorders Review, 13, 338–343.
Santos, M., Richards, C. S., & Bleckley, M. K. (2007). Comorbidity between depression and disordered eating in adolescents. Eating Behaviors, 8, 440–449.
Sawdon, A. M., Cooper, M., & Seabrook, R. (2007). The relationship between self-discrepancies, eating disorder and depressive symptoms in women. European Eating Disorders Review, 15, 207–212.
Seidah, A., & Bouffard, T. (2007). Being proud of oneself as a person or being proud of one’s physical appearance: What matters for feeling well in adolescence? Social Behavior and Personality, 35, 255–268.
Senra, C., Seoane, G., Vilas, V., & Sánchez-Cao, E. (2007). Comparison of 10- to 12-year-old boys and girls using a Spanish version of the children’s eating attitudes test. Personality and Individual Differences, 42, 947–957.
Silverstone, P. H. (1992). Is chronic low self-esteem the cause of eating disorders? Medical Hypotheses, 39, 311–315.
Skomorovsky, A., Matheson, K., & Anisman, H. (2006). The buffering role of social support perceptions in relation to eating disturbances among women in abusive dating relationships. Sex Roles, 54, 627–638.
Stice, E. (2002). Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological Bulletin, 128, 825–848.
Stice, E., Hayward, C., Cameron, R. P., Killen, J. D., & Taylor, C. B. (2000). Body-image and eating disturbances predict onset of depression among female adolescents: A longitudinal study. Journal of Abnormal Psychology, 109, 438–444.
Stice, E., Presnell, K., & Spangler, D. (2002). Risk factors for binge eating onset in adolescent girls: A 2-year prospective investigation. Health Psychology, 21, 131–138.
Strauman, T. J., Vookles, J., Berenstein, V., Chaiken, S., & Higgins, E. T. (1991). Self-discrepancies and vulnerability to body dissatisfaction and disordered eating. Journal of Personality and Social Psychology, 61, 946–956.
Trzesniewski, K. H., Donnellan, M. B., Moffitt, T. E., Robins, R. W., Poulton, R., & Caspi, A. (2006). Low self-esteem during adolescence predicts poor health, criminal behavior, and limited economic prospects during adulthood. Developmental Psychology, 42, 381–390.
Twenge, J. M., & Nolen-Hoeksema, S. (2002). Age, gender, race, socioeconomic status, and birth cohort difference on the children’s depression inventory: A meta-analysis. Journal of Abnormal Psychology, 111, 578–588.
Vázquez, A. J., Jiménez, R., & Vázquez-Morejón, R. (2004). Escala de autoestima de Rosenberg: Fiabilidad y validez en población clínica española. [Rosenberg Self-Esteem Scale: Reliability and validity in a Spanish clinical population]. Apuntes de Psicología, 22, 247–255.
Walsh, B. T., & Sysko, R. (2009). Broad categories for the diagnosis of eating disorders (BCD-ED): An alternative system for classification. International Journal of Eating Disorders, 42, 754–764.
Wonderlich-Tierney, A. L., & Vander Wal, J. S. (2010). The effects of social support and coping on the relationship between social anxiety and eating disorders. Eating Behaviors, 11, 85–91.
Acknowledgments
This study was supported by the Ministry of Education (AP2008-01526) and the Ministry of Science and Innovation (PSI2010-19793) of the Spanish Government.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferreiro, F., Seoane, G. & Senra, C. Gender-related Risk and Protective Factors for Depressive Symptoms and Disordered Eating in Adolescence: A 4-year Longitudinal Study. J Youth Adolescence 41, 607–622 (2012). https://doi.org/10.1007/s10964-011-9718-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10964-011-9718-7