Abstract
Recent research in religiousness and health suggests that epidemiological forces can have opposed effects. Here we examine two forms of religiousness and their association with disease. We performed a cross-sectional study of 23,864 people aged 50+ included in wave 1 (2004–2005) of the Survey of Health, Ageing and Retirement in Europe and a longitudinal study including people from wave 1, who were followed up during 11 years. Results suggested that taking part in a religious organization was associated with lower odds of heart attack (OR 0.74, 95% CI 0.60, 0.90), stroke (OR 0.68, 95% CI 0.50, 0.95), and diabetes (OR 0.72, 95% CI 0.58, 0.90) and longitudinally associated with lower odds of cancer (OR 0.78, 95% CI 0.60, 1.00). Conversely, praying was longitudinally associated with higher odds of heart attack (OR 1.27, 95% CI 1.10, 1.48) and high cholesterol (OR 1.12, 95% CI 1.00, 1.26). The most religious people had lower odds of stroke, diabetes, and cancer than other respondents, and in the longitudinal model, people who only prayed had higher odds of heart attack than non-religious people. Our findings lend support to the hypothesis that restful religiousness (praying, taking part in a religious organization, and being religiously educated) was associated with lower odds of some diseases, whereas little evidence was present that crisis religiousness (praying only) was associated with higher odds of disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Population aging is a major societal challenge in the twenty-first century (Borsch-Supan et al. 2013), and according to the World Health Organization (WHO), the impact of the major non-communicable diseases (diabetes, cardiovascular diseases, cancer, chronic respiratory diseases, and mental disorders) is alarming (WHO 2017). Work in the research field of religiousness/spirituality (R/S) and health has intensified in recent decades (Aldwin et al. 2014), the majority of which includes mental health (Koenig 2012). However, by positively affecting health behaviors, reducing stress and negative emotions and increasing social support, it is also indicated that religious involvement has an impact on a range of physical diseases (Koenig 2012)—albeit findings are mixed (Koenig et al. 2012).
A meta-analysis from 2009 found among 69 studies in healthy populations that R/S was associated with reduced all-cause mortality and cardiovascular disease (CVD) mortality (Chida et al. 2009). However, two recent longitudinal studies conducted in a large cohort of healthy, older women participating in the Women’s Health Initiative did not find a protective association between religious affiliation, religious service attendance, religious coping (Schnall et al. 2010), or private religious practice (Salmoirago-Blotcher et al. 2013) and CVD morbidity and mortality. Similar findings were reported in a prospective cohort study involving 5474 healthy men and women from the Multi-Ethnic Study of Atherosclerosis (Feinstein et al. 2010). In both cohorts, the results suggested a higher risk of CVD among the more religious people. In addition, a prospective study conducted among myocardial infarction (MI) survivors at risk for a second MI did not show associations between service attendance, private religious practice, or spiritual experiences and risk of recurrent MI (Blumenthal et al. 2007). Current evidence on R/S and cardiovascular mortality and morbidity remains inconclusive, and more research is needed across different subgroups and follow-up durations (Park et al. 2017).
Research focusing on the role of religion and spirituality on cancer outcomes has been sparse (Stefanek et al. 2005). In systematic reviews of R/S and cancer mortality or progression, there is inadequate evidence to support the hypothesis that R/S protects against cancer mortality and failure to support the hypothesis that R/S slows cancer progression (Powell et al. 2003). Koenig (2015) identified 29 studies, which investigated associations between R/S and the onset or the course of cancer. They found that 55% of the studies reported a lower risk of cancer or a better prognosis in individuals who were more religious, whereas two studies (7%) reported worse outcomes. However, there appears to be consensus that certain religious groups, such as Mormons and Seventh Day Adventists, have lower cancer rates than the general population (Thygesen et al. 2012), mainly because of healthy lifestyles (Hoff et al. 2008; Koenig et al. 2012).
The majority of the research on religiousness and health comes from the USA, whereas studies in other regions are sparser. Evidence from Europe suggests associations between various forms of religious participation and better self-rated health, lower depression, and lower mortality (VanderWeele 2017b). A population-based cross-sectional study from Norway of 35,964 participants found that religious attendance was associated with lower blood pressure (Sorensen et al. 2011). Recent cross-sectional evidence from the Survey of Health, Ageing and Retirement in Europe (SHARE) (Linardakis et al. 2015) found that praying and being religiously educated were associated with fewer multiple behavioral risk factors for chronic diseases. Our recent longitudinal study (Ahrenfeldt et al. 2017) examining associations on religiousness and health in various European countries showed that participating in a religious organization had the most consistent associations with health, whereas little evidence was found that prayer, when considered on its own, was associated with health outcomes; however, evidence was present that people who prayed had higher odds of depressive symptoms than non-religious people.
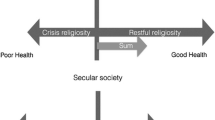
Recent research has conceptualized two tendencies in religion and health as opposite epidemiological forces (Hvidt et al. 2016). In every population, there are people that are religious in the sense that they rest intrinsically in their faith and have a longstanding reliance on religion marked by restfulness (“restful religiousness”). The opposite is provoked by stress or group pressure and comes across as increased reliance on religion during crisis (“crisis religiousness”). Restful religiousness is mostly marked by a combination of religious upbringing, religious practice, and personal prayer. The opposite tendency is when religiousness is provoked by stress or group pressure and increasingly functions as a coping mechanism during crisis (Ryan et al. 1993). Other theorists have delineated similar dichotomies, such as Ross–Allport’s distinction between intrinsic and extrinsic religiosity, suggesting differences between those who live their religion, and those who use their religion (Allport and Ross 1967). This was later updated with the concept of quest toward a fuller presentation of motivation in religiosity (Batson et al. 1993) to which other researchers have proposed updates (Neyrinck et al. 2010).
Building upon previous research (Ahrenfeldt et al. 2017; Hvidt et al. 2016), the aim of the present study is to investigate the associations between religiousness and various somatic diseases in Europeans aged 50 and over and to examine how each of the two forms of religiousness is associated with diseases. We hypothesize that restful religiousness (identified by praying, taking part in a religious organization, and being religiously educated) lowers the odds of disease, whereas such effects may be much weaker or even reversed for the less religious individuals (identified by praying without other religious activities) if prayer arise from a state of crisis.
Materials and Methods
Setting and Study Population
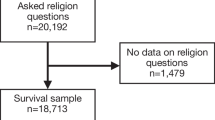
The present study includes respondents from 10 European countries in SHARE (Borsch-Supan et al. 2013). SHARE is a multinational survey including information on health, socioeconomic status, and social factors designed to be representative of non-institutionalized Europeans aged 50+. The data collection was drawn at the household level, and the participants were interviewed at home by trained interviewers according to strict quality standards. In addition to the main interview, a self-administrated questionnaire was given to participants after the interview (Borsch-Supan et al. 2013). The household response rate differed by country and wave varying between 44.0% in Switzerland and 67.1% in Denmark in wave 1 (Bergmann et al. 2017). Calibrated individual weights are provided by SHARE to handle unit non-response and sample attrition (Borsch-Supan et al. 2013).
The cross-sectional study includes people aged 50 and above from SHARE wave 1, who were interviewed in 2004–2005. The longitudinal study was based on people from wave 1 who were followed up in waves 2 (2006–2007), 4 (2011), and 6 (2015). Ten European countries were included; however, Greece was not a part of wave 4, and the Netherlands did not participate in wave 6. France was not included, because the French questionnaire did not include questions about religiousness.
Religiosity Measures
Information about religiousness was available in wave 1. Praying was assessed by the question: “Thinking about the present, about how often do you pray?” and was dichotomized into praying and not praying. Taking part in a religious organization was investigated by the question: “Have you done any of these activities in the last month?” which had seven possible answers, one of them being “taken part in a religious organization (church, synagogue, mosque, etc.)”, with the possible answers “yes” or “no.” Religious education was measured by the question: “Have you been educated religiously by your parents?” answered by “yes” or “no.” Information about religious attendance came from the personal interview, whereas information about praying and religious education was based on the self-administered questionnaire.
We classified religiousness into three categories: The more religious—people who pray, take part in a religious organization, and are religiously educated; the less religious—people who pray, without taking part in a religious organization, or being religiously educated; and the non-religious—people who answered “no” to praying, taking part in a religious organization, and being religiously educated. Moreover, three comparisons were constructed: Comparison 1—the more religious versus all other respondents; comparison 2—the more religious versus the less religious; and comparison 3—the less religious versus the non-religious.
Chronic Diseases
Diseases were recorded by the following questions which were all part of the personal interview: “Has a doctor ever told you that you had any of the conditions on this card?” (wave 1). In the subsequent waves, respondents were asked: “Has a doctor ever told you that you had/do currently have any of the conditions on this card? [With this we mean that a doctor has told you that you have this condition, and that you are either currently being treated for or bothered by this condition]”. We excluded diseases that were not asked about in the same way in all waves (asthma, arthritis, and osteoporosis). Furthermore, Parkinson’s disease was excluded because of low number of cases. The following diseases were included: “Heart attack including myocardial infarction or coronary thrombosis or any other heart problem including congestive heart failure,” “High blood pressure or hypertension,” “High blood cholesterol,” “Stroke or cerebral vascular disease,” “Diabetes or high blood sugar,” “Chronic lung disease such as chronic bronchitis or emphysema,” “Cancer or malignant tumor, including leukemia or lymphoma, but excluding minor skin cancers,” and “Stomach or duodenal ulcer, peptic ulcer,” Moreover, we investigated multiple diseases, dichotomized into none or one vs. two or more chronic diseases.
Socio-demographic Characteristics
European regions, gender, age at interview (continuous), educational level, marital status, and employment were included as covariates in the models. We grouped the European countries into three regions: Northern Europe (Denmark and Sweden), Southern Europe (Italy, Spain, and Greece), and Western Europe (Austria, Belgium, Germany, Switzerland, and the Netherlands). Further details are provided in Table 1 and by Ahrenfeldt et al. (2017).
Statistical Analyses
Associations between religiousness and diseases were analyzed using logistic regression models with robust standard errors, estimating odds ratios (ORs) and 95% confidence intervals (CIs) in a longitudinal setting of participants in wave 1 who were followed up in at least one of waves 2, 4, and 6. For each outcome, people with the specific disease in wave 1 were excluded. In the overall model, we included all waves, taking repeated observations from the same individual into account by clustering (Huber 1967) and adjusting for wave and the covariates. Furthermore, we fitted an interaction model, additionally including terms for interaction between wave and religiosity measures. The overall analysis was repeated, examining possible interactions between religiosity measures and European region and between religiosity measures and gender, respectively. Further, we investigated the associations between religiousness and diseases in a cross-sectional design using data from wave 1 only. The main analyses were corrected for multiple testing using the Holm–Bonferroni method via R version 3.3.1. Stata version 14.2 was used for all other analyses.
Results
In Table 1, we report descriptive statistics of demographic, socioeconomic, and religious variables as well as disease prevalence for people in wave 1 who were followed up in waves 2, 4 and 6, respectively. On average, 69.5% reported praying, 12.9% took part in a religious organization, and 76.6% were religiously educated.
In the overall model (Fig. 1a), praying was associated with higher odds of heart attack (OR 1.27, 95% CI 1.10, 1.48), with ORs ranging between 1.23 and 1.32 in the interaction model (Supplementary Table 1). Praying was associated with higher odds of high cholesterol, both overall (OR 1.12, 95% CI 1.00, 1.26) and in the interaction model (wave 6). Conversely, lower odds of cancer were indicated overall (OR 0.83, 95% CI 0.68, 1.01) and in waves 2 and 6.
Associations between religiosity measures and somatic diseases in a cross-sectional and a longitudinal setting based on wave 1 participants (2004–2005) from SHARE who were followed up in waves 2 (2006–2007), 4 (2011), and 6 (2015), adjusted for European region, gender, age at interview, education, marital status, and employment
An inverse association between taking part in a religious organization and odds of diseases was indicated for all diseases except from hypertension (OR 1.00), with borderline significant associations for stroke (OR 0.80, 95% CI 0.62, 1.03), cancer (OR 0.78, 95% CI 0.60, 1.00), and multiple diseases (OR 0.92, 95% CI 0.83, 1.02). Lower odds were also indicated for diabetes, lung disease, and ulcer (Fig. 1b). In the interaction model, we found lower odds of lung disease in wave 2 (Supplementary Table 1). We found an association between taking part in a religious organization and gender in the overall model, with lower odds of ulcer for men (OR 0.56, 95% CI 0.35, 0.91) but no association for women (OR 1.07, 95% CI 0.80, 1.43).
No overall associations were found between being religiously educated and diseases (Fig. 1c); however, in the interaction model, lower odds of multiple diseases were found in wave 2 (Supplementary Table 1). Moreover, we found an association with gender, indicating higher odds of lung disease for men who were religiously educated (OR 1.28, 95% CI 0.94, 1.72), whereas lower odds were found for women (OR 0.73, 95% CI 0.56, 0.97).
We found no associations between comparison 1 and diseases in the overall model; although all estimates were below one (Fig. 1d). In the interaction model (wave 2), we found an indication of lower odds of multiple diseases for the more religious compared with all other respondents. When comparing the more religious with the less religious people (comparison 2), we found no associations with diseases, except for an indication of lower odds of lung disease (OR 0.65, 95% CI 0.41, 1.03) (Fig. 1e). The association was significant in wave 2. For comparison 3, we found higher odds of heart attack (OR 1.49, 95% CI 1.13, 1.98) for the less religious, compared with the non-religious people (Fig. 1f). Conversely, in the interaction model (wave 6), we found lower odds of cancer for people who prayed, compared with people who were non-religious. No associations remained significant after adjusting for multiple testing.
In investigating interactions between religiosity measures and regions, we found only few interactions and no clear pattern (Table 2).
When examining the associations between religiosity measures and diseases in wave 1, results indicated that people who prayed had higher odds of ulcer (OR 1.25, 95% CI 0.99, 1.56) and of having at least two chronic diseases (OR 1.12, 95% CI 0.99, 1.26). Participating in a religious organization was associated with lower odds of heart attack (OR 0.74, 95% CI 0.60, 0.90), stroke (OR 0.68, 95% CI 0.50, 0.95), and diabetes (OR 0.72, 95% CI 0.58, 0.90). The more religious had lower odds for stroke (OR 0.67, 95% CI 0.46, 0.99), diabetes (OR 0.75, 95% CI 0.58, 0.97), and cancer (OR 0.67, 95% CI 0.46, 0.95) compared with other respondents, and lower odds of diabetes (OR 0.62, 95% CI 0.39, 0.98) than people who only prayed (Fig. 1a–f; Supplementary Table 1).
Discussion
Findings in the present study, based on a large sample of Europeans aged 50+ interviewed over 10 years, suggested associations between religiousness and diseases with the effect of the associations depending on the type of religiousness. We hypothesized that restful religiousness (praying, taking part in a religious organization, and being religiously educated) was associated with lower odds of diseases, and that this effect was weaker or even reversed among the less religious individuals (praying only). Our results suggested that restful religiousness was associated with lower odds of some diseases, particularly cancer, whereas little evidence was present that crisis religiousness was associated with higher odds of disease.
Praying without other religious activities is often seen as a marker of crisis religiousness, indicative of personal and health problems already being present (Hvidt et al. 2016; Koenig et al. 2012; Levin 2012, 2013; Litwin et al. 2017). This is consistent with the cross-sectional analysis in the present study that indicated higher odds of ulcer and of having at least two chronic diseases for people who prayed. Our longitudinal findings on heart attack and high cholesterol also support this assumption, although we cannot exclude that findings for heart attack may be explained—at least partly—by survival bias due to differential survival across religious groups (Chida et al. 2009; McCullough et al. 2000). Few studies have investigated associations between praying and CHD or related cardiovascular functions. A case–control study in a Muslim population found that prayer was inversely associated with acute coronary syndrome (Burazeri et al. 2008), whereas a multi-ethnic study of 5474 people found no reduction in risk for cardiovascular disease associated with greater religiosity, including prayer/meditation (Feinstein et al. 2010). One study examining associations between prayer habit and CHD in India found no association for those living in urban areas, whereas prayer was associated with a lower likelihood of CHD in rural areas (Gupta et al. 1997). In the present study, praying did not have effect in one direction only. Praying had a protective effect on cancer after 2 and 11 years of follow-up, and people who prayed had lower odds of cancer after 11 years than non-religious people.
Our longitudinal results suggested that taking part in a religious organization was inversely associated with cancer. Although there is inadequate evidence to support the hypothesis that R/S protects against cancer mortality (Powell et al. 2003), there is increasing evidence to indicate that R/S relates to many of the psychological, social, and behavioral factors that influence endocrine and immune functions which have an impact on cancer growth (Koenig et al. 2012). A review of 18 studies examining the risk of cancer in Christian and non-Christian samples concluded that lifestyle factors explained the reduced risk for cancer associated with a Christian affiliation (Hoff et al. 2008). This is consistent with research indicating that R/S is associated with certain health behaviors including less smoking and alcohol use (Koenig 2015), greater use of preventive health services including cancer screening (Reindl Benjamins and Brown 2004), and greater adherence to health behaviors (Park et al. 2008), suggesting that R/S may be associated with reduced cancer risk (Park et al. 2016), a hypothesis supported by this study.
To better assess the public health importance of religiosity, we considered effects of numerous diseases simultaneously. Recent evidence suggests that such “outcome-wide epidemiology” is often preferable to current standard practices (VanderWeele 2017a). Our study considered nine different outcomes and examined six religiosity measures. Considered separately, a number of estimates suggested evidence for associations between religiousness and diseases. Among the four comparisons for which we hypothesize a protective association (religious organization, religious education, comparisons 1 and 2), we found that 30 of the 36 associations were in a protective direction, three were equal to null (OR 1.00), and three were in an adverse direction (ORs 1.10 and 1.16). However, although we used the preferable Holm–Bonferroni method to adjust for multiple testing (Holm 1979), the associations did not pass the threshold (p = 0.05), which emphasizes the challenges evaluating numerous outcomes at once (VanderWeele 2017b).
Previous research (Hvidt et al. 2016; Ryan et al. 1993) suggests that restful religiousness is more pronounced in religious societies such as Southern Europe, whereas crisis religiousness is more often seen in secular countries such as in Northern Europe. In line with previous studies (Ahrenfeldt et al. 2017; Croezen et al. 2015; Di Gessa and Grundy 2014), we did not find country variations in most of the associations. Despite the fact that women often are more religious than men (Deaton 2009; Trzebiatowska and Bruce 2012), few associations between religiousness and diseases differed by gender in this study.
The strengths of this study were the large sample size of Europeans and the opportunity to investigate the associations between religiousness and diseases in a longitudinal design with multiple waves of data, including harmonized disease measures from ten European countries and the possibility of adjustment for several potential confounders. This longitudinal design, excluding people with the specific disease at baseline, and with outcomes measured over several waves, is important in order to try to rule out reverse causation (VanderWeele et al. 2016).
A concern in this study was attrition from the sample, which could bias estimates if R/S people have better survival and are more willing to participate in surveys compared with non-religious people (Koenig et al. 2012). If R/S people have better survival, for which evidence is quite strong (Chida et al. 2009; McCullough et al. 2000), it is possible that the more religious people who have had a heart attack could end up in the sample, while non-religious people with a heart attack might have died. This may explain—at least, in part—the longitudinal findings of higher odds for heart attack for people who prayed. Although it would have been preferable to consider mortality in the analyses, it is problematic due to the large number of participants with unknown vital status in SHARE. Another limitation is the low response rate ranging between 44 and 67% in SHARE wave 1. If, for instance, people participating in the survey are more religious and have fewer diseases compared with non-respondents, the associations, e.g., toward lower odds of diseases for people who take part in a religious organization, might have been strengthened. Moreover, misclassification might be an issue, because diseases were self-reported, and we had one-third missing values regarding the variables “praying” and “being religiously educated.” Also, we cannot rule out that there may be people with traits of crisis religiosity among those brought up with religion, practicing religion, and praying and conversely that there may be people with restful religiousness among those who only report to pray. To eliminate bias and make reverse causation less likely, we excluded prevalent diseases at baseline, with the effect of reducing the study sample, making a type II error (a “false negative” finding) more likely.
In conclusion, findings in this study suggested associations between religiousness and somatic diseases among middle-aged and elderly Europeans. Our findings lend support to the hypothesis that restful religiousness was associated with lower odds of some diseases, whereas little evidence was present that crisis religiousness was associated with higher odds of disease. More research is needed to better understand the impact of religiousness on diseases, and to distinguish between different types of religiousness to better understand how religiousness influences health.
References
Ahrenfeldt, L. J., Möller, S., Andersen-Ranberg, K., Vitved, A. R., Lindahl-Jacobsen, R., & Hvidt, N. C. (2017). Religiousness and health in Europe. European Journal of Epidemiology. https://doi.org/10.1007/s10654-017-0296-1.
Aldwin, C. M., Park, C. L., Jeong, Y.-J., & Nath, R. (2014). Differing pathways between religiousness, spirituality, and health: A self-regulation perspective. Psychology of Religion and Spirituality,6(1), 9.
Allport, G. W., & Ross, J. M. (1967). Personal religious orientation and prejudice. Journal of Personality and Social Psychology,5, 432–443. https://doi.org/10.1037/0022-3514.5.4.432.
Batson, C. D., Schoenrade, P., & Ventis, W. L. (1993). Religion and the individual: A social–psychological perspective. Oxford: Oxford University Press.
Bergmann, M., Kneip, T., Luca, D., Giuseppe, Scherpenzeel, & Annette. (2017). Survey Participation in the Survey of Health, Ageing and Retirement (SHARE), wave 1–6. Based on Release 6.0.0 (March 2017). SHARE working paper series 31-2017. Munich: SHARE-ERIC.
Blumenthal, J. A., Babyak, M. A., Ironson, G., Thoresen, C., Powell, L., Czajkowski, S., et al. (2007). Spirituality, religion, and clinical outcomes in patients recovering from an acute myocardial infarction. Psychosomatic Medicine,69(6), 501–508. https://doi.org/10.1097/PSY.0b013e3180cab76c.
Borsch-Supan, A., Brandt, M., Hunkler, C., Kneip, T., Korbmacher, J., Malter, F., et al. (2013). Data resource profile: The Survey of Health, Ageing and Retirement in Europe (SHARE). International Journal of Epidemiology,42(4), 992–1001. https://doi.org/10.1093/ije/dyt088.
Burazeri, G., Goda, A., & Kark, J. D. (2008). Religious observance and acute coronary syndrome in predominantly Muslim Albania: A population-based case-control study in Tirana. Annals of Epidemiology,18(12), 937–945. https://doi.org/10.1016/j.annepidem.2008.09.001.
Chida, Y., Steptoe, A., & Powell, L. H. (2009). Religiosity/spirituality and mortality. A systematic quantitative review. Psychotherapy and Psychosomatics,78(2), 81–90. https://doi.org/10.1159/000190791.
Croezen, S., Avendano, M., Burdorf, A., & van Lenthe, F. J. (2015). Social participation and depression in old age: A fixed-effects analysis in 10 European countries. American Journal of Epidemiology,182(2), 168–176. https://doi.org/10.1093/aje/kwv015.
Deaton, A. (2009). Aging, religion, and health. NBER Working Paper No. 15271.
Di Gessa, G., & Grundy, E. (2014). The relationship between active ageing and health using longitudinal data from Denmark, France, Italy and England. Journal of Epidemiology and Community Health,68(3), 261–267. https://doi.org/10.1136/jech-2013-202820.
Feinstein, M., Liu, K., Ning, H., Fitchett, G., & Lloyd-Jones, D. M. (2010). Burden of cardiovascular risk factors, subclinical atherosclerosis, and incident cardiovascular events across dimensions of religiosity: The multi-ethnic study of atherosclerosis. Circulation,121(5), 659–666. https://doi.org/10.1161/circulationaha.109.879973.
Gupta, R., Prakash, H., Gupta, V. P., & Gupta, K. D. (1997). Prevalence and determinants of coronary heart disease in a rural population of India. Journal of Clinical Epidemiology,50(2), 203–209.
Hoff, A., Johannessen-Henry, C. T., Ross, L., Hvidt, N. C., & Johansen, C. (2008). Religion and reduced cancer risk: What is the explanation? A review. European Journal of Cancer,44(17), 2573–2579. https://doi.org/10.1016/j.ejca.2008.08.001.
Holm, S. (1979). A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics,6(2), 65–70.
Huber, P. J. (1967, 1967). The behavior of maximum likelihood estimates under nonstandard conditions. Paper presented at the Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability, Vol. 1. Statistics, Berkeley, CA.
Hvidt, N. C., Hvidtjorn, D., Christensen, K., Nielsen, J. B., & Sondergaard, J. (2016). Faith moves mountains–mountains move faith: Two opposite epidemiological forces in research on religion and health. Journal of Religion and Health. https://doi.org/10.1007/s10943-016-0300-1.
Koenig, H. G. (2012). Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry, 2012, Article ID 278730. https://doi.org/10.5402/2012/278730.
Koenig, H. G. (2015). Religion, spirituality, and health: A review and update. Advances in Mind-Body Medicine,29(3), 19–26.
Koenig, H. G., King, D. E., & Carson, V. B. (Eds.). (2012). Handbook of religion and health. Oxford/New York: Oxford University Press.
Levin, J. (2012). Religion and physical health among older Israeli Jews: Findings from the SHARE-Israel study. Israel Medical Association Journal,14(10), 595–601.
Levin, J. (2013). Religion and mental health among Israeli Jews: Findings from the SHARE-Israel study. Social Indicators Research,113(3), 769–784. https://doi.org/10.1007/s11205-012-0113-x.
Linardakis, M., Papadaki, A., Smpokos, E., Sarri, K., Vozikaki, M., & Philalithis, A. (2015). Are religiosity and prayer use related with multiple behavioural risk factors for chronic diseases in European adults aged 50+ years? Public Health,129(5), 436–443. https://doi.org/10.1016/j.puhe.2015.02.006.
Litwin, H., Schwartz, E., & Avital, D. (2017). Religiosity and well-being among older Jewish Israelis: Findings from SHARE. Journal of Religion, Spirituality & Aging,29(2–3), 208–223. https://doi.org/10.1080/15528030.2015.1132491.
McCullough, M. E., Hoyt, W. T., Larson, D. B., Koenig, H. G., & Thoresen, C. (2000). Religious involvement and mortality: A meta-analytic review. Health Psychology,19(3), 211–222.
Neyrinck, B., Lens, W., Vansteenkiste, M., & Soenens, B. (2010). Updating Allport’s and Batson’s framework of religious orientations: A reevaluation from the perspective of self-determination theory and Wulff’s social cognitive model. Journal for the Scientific Study of Religion,49(3), 425–438.
Park, C. L., Masters, K. S., Salsman, J. M., Wachholtz, A., Clements, A. D., Salmoirago-Blotcher, E., et al. (2016). Advancing our understanding of religion and spirituality in the context of behavioral medicine. Journal of Behavioral Medicine. https://doi.org/10.1007/s10865-016-9755-5.
Park, C. L., Masters, K. S., Salsman, J. M., Wachholtz, A., Clements, A. D., Salmoirago-Blotcher, E., et al. (2017). Advancing our understanding of religion and spirituality in the context of behavioral medicine. Journal of Behavioral Medicine,40(1), 39–51. https://doi.org/10.1007/s10865-016-9755-5.
Park, C. L., Moehl, B., Fenster, J. R., Suresh, D. P., & Bliss, D. (2008). Religiousness and treatment adherence in congestive heart failure patients. Journal of Religion, Spirituality & Aging,20(4), 249–266. https://doi.org/10.1080/15528030802232270.
Powell, L. H., Shahabi, L., & Thoresen, C. E. (2003). Religion and spirituality. Linkages to physical health. American Psychologist,58(1), 36–52.
Reindl Benjamins, M., & Brown, C. (2004). Religion and preventative health care utilization among the elderly. Social Science and Medicine,58(1), 109–118.
Ryan, R. M., Rigby, S., & King, K. (1993). Two types of religious internalization and their relations to religious orientations and mental health. Journal of Personality and Social Psychology,65(3), 586.
Salmoirago-Blotcher, E., Fitchett, G., Hovey, K. M., Schnall, E., Thomson, C., Andrews, C. A., et al. (2013). Frequency of private spiritual activity and cardiovascular risk in postmenopausal women: The Women’s Health Initiative. Annals of Epidemiology,23(5), 239–245. https://doi.org/10.1016/j.annepidem.2013.03.002.
Schnall, E., Wassertheil-Smoller, S., Swencionis, C., Zemon, V., Tinker, L., O’Sullivan, M. J., et al. (2010). The relationship between religion and cardiovascular outcomes and all-cause mortality in the Women’s Health Initiative Observational Study. Psychology & Health,25(2), 249–263. https://doi.org/10.1080/08870440802311322.
Sorensen, T., Danbolt, L. J., Lien, L., Koenig, H. G., & Holmen, J. (2011). The relationship between religious attendance and blood pressure: The HUNT study, Norway. International Journal of Psychiatry in Medicine,42(1), 13–28. https://doi.org/10.2190/PM.42.1.b.
Stefanek, M., McDonald, P. G., & Hess, S. A. (2005). Religion, spirituality and cancer: Current status and methodological challenges. Psycho-Oncology,14(6), 450–463. https://doi.org/10.1002/pon.861.
Thygesen, L. C., Hvidt, N. C., Hansen, H. P., Hoff, A., Ross, L., & Johansen, C. (2012). Cancer incidence among Danish Seventh-day Adventists and Baptists. Cancer Epidemiology,36(6), 513–518. https://doi.org/10.1016/j.canep.2012.08.001.
Trzebiatowska, M., & Bruce, S. (2012). Why are women more religious than men? Oxford: Oxford University Press.
VanderWeele, T. J. (2017a). Outcome-wide epidemiology. Epidemiology,28(3), 399–402. https://doi.org/10.1097/ede.0000000000000641.
VanderWeele, T. J. (2017b). Religion and health in Europe: Cultures, countries, context. European Journal of Epidemiology,32(10), 857–861. https://doi.org/10.1007/s10654-017-0310-7.
VanderWeele, T. J., Jackson, J. W., & Li, S. (2016). Causal inference and longitudinal data: A case study of religion and mental health. Social Psychiatry and Psychiatric Epidemiology,51(11), 1457–1466. https://doi.org/10.1007/s00127-016-1281-9.
WHO. (2017). Noncommunicable diseases. Retrieved from http://www.euro.who.int/en/health-topics/noncommunicable-diseases/noncommunicable-diseases. Accessed 28 Aug 2017.
Acknowledgements
This paper uses data from SHARE waves 1, 2, 4, and 6 (https://doi.org/10.6103/share.w1.600, https://doi.org/10.6103/share.w2.600, https://doi.org/10.6103/share.w4.600, https://doi.org/10.6103/share.w6.600), see Borsch-Supan et al. (2013) for methodological details (Borsch-Supan et al. 2013). The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: No. 211909, SHARE-LEAP: No. 227822, SHARE M4: No. 261982). Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Funding
There was no specific funding for this study. Linda Juel Ahrenfeldt, Stine Tving Kjøller, and Sören Möller had full access to the data, and all authors had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
LJA contributed to the literature search, study question and design, performed data analyses, prepared the first draft of the paper, and drafted the final version; NCH contributed to the study design and to the interpretation of results; STK contributed to the literature search and to data analyses; SM contributed to data analyses and to the interpretation of results, and RLJ critically reviewed and revised the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no conflicts of interest in relation to the present article.
Ethical Approval
For this type of study, formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ahrenfeldt, L.J., Hvidt, N.C., Kjøller, S.T. et al. Religiousness and Diseases in Europe: Findings from SHARE. J Relig Health 58, 1925–1937 (2019). https://doi.org/10.1007/s10943-018-0664-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-018-0664-5