Abstract
This study examined the following: (1) relationships between religiosity—as measured by religious service attendance—and screening for breast, cervical, and colorectal cancers; (2) the potential mediating role of social support; and (3) the potential moderating effect of race/ethnicity. Statistical analyses showed that religiosity was associated with greater utilization of breast, cervical, and colorectal cancer screening. Social support fully mediated the relationship between religiosity and Pap screening, and partially mediated the relationship between religiosity and colorectal screening, but had no effect on the relationship between religiosity and mammography screening. Race/ethnicity moderated the relationship between religiosity and social support in the cervical cancer screening model, such that the positive association between religiosity and social support was stronger for non-Hispanic Blacks than it was for non-Hispanic Whites. These findings have implications for the role of social networks in health promotion and can inform cancer screening interventions in faith-based settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A large body of research has focused on the influence of religiosity on individual and population health (Benjamins 2006; Chatters 2000; McCullough et al. 2000). Religiosity is a multidimensional construct defined by the belief in, practice of, or participation in the rituals and activities of an organized religion (Kaye and Raghavan 2002). Common dimensions of religiosity include denomination, service attendance, involvement/participation in religious activities, religious beliefs, and coping. Prior research has demonstrated that higher levels of religiosity are associated with more positive physical and mental health outcomes (Ellison and Levin 1998; Gartner et al. 1991; Levin and Chatters 1998; McCullough et al. 2000). Research has also shown that religiosity is associated with lower levels of behavioral risk (e.g., alcohol use) and higher levels of health-promoting behaviors (e.g., diet, exercise) (Benjamins 2006; Hill et al. 2007; Homan and Boyatzis 2010; Jessor et al. 1997; Kendler et al. 1997; Reindl Benjamins and Brown 2004; Rew and Wong 2006; Wallace and Forman 1998).
While religiosity is strongly associated with a wide range of positive health behaviors (Chatters 2000), there is mixed evidence for the relationship between religiosity and cancer screening. Studies with population-based and community samples have found increased screening rates among those who attend religious services (Allen et al. 2014; Benjamins 2006; Fox et al. 1998; Paskett 1999b; Reindl Benjamins and Brown 2004). Accordingly, cancer screening interventions are being designed for delivery in faith-based settings (Campbell et al. 2007; Holt et al. 2009, 2013; Ma et al. 2012; Morgan et al. 2010). Yet, not all studies have found increased screening among people who participate in religious services or faith-based interventions (Campbell et al. 2007; Husaini et al. 2001; Katz et al. 2008; Lukwago et al. 2003; Merrill 2001; Van Ness et al. 2002).
Few studies have examined the mechanisms through which religiosity impacts health behaviors, and there is a particular lack of information about its role in cancer screening. One theory (Berkman and Glass 2000) posits that social structures and networks found within faith-based settings may influence individual health attitudes and behaviors through the provision of social support. Social support encompasses emotional, instrumental, and informational functions (Gottlieb and Bergen 2010). With regard to cancer screening, individuals may draw on emotional support from church members to quell anxiety surrounding cancer screening procedures and results (Botoseneanu et al. 2011; Bradley 1995; Kinney et al. 2003; Kinney et al. 2005; McFall & Davila, 2008). This support may also influence social norms about the acceptability of screening, self-efficacy to seek and obtain screening tests, and provide encouragement to individuals who decide to screen (Nguyen et al. 2012). In addition, instrumental social support can facilitate the use of screening services, by reducing barriers such as cost, transportation, and language. Further, participation in religious organizations may provide individuals with exposure to health information and resources about cancer screening (Erwin et al. 1999; Nguyen et al. 2009; Schoenberg et al. 2009), which may result in more positive attitudes toward screening (Berkman and Glass 2000).
There are a limited number of published empirical studies that have examined the relationships between religious participation, social influences, and cancer screening behaviors (Benjamins, 2006; Kinney et al. 2003; McFall and Davila 2008). Limitations of prior research include a focus on only one screening behavior (Klassen and Washington 2008) and relatively small sample sizes (Gamarra et al. 2009). Moreover, a recent study found significant racial/ethnic differences across dimensions of religiousness and mental health, which suggests that race and ethnicity are important variables to consider when examining the link between religiosity and health (Cokley et al. 2012). However, prior research has primarily included relatively homogenous populations (Katapodi et al. 2002). Consequently, it is unknown whether the nature and the strength of associations between religiosity and cancer screening vary by race/ethnicity.
Better understanding the role of religiosity in screening behavior across racial/ethnic groups is important for cancer control efforts, as such knowledge could inform educational interventions delivered in faith-based settings. The purpose of this exploratory study is to examine the following: (1) relationships between religiosity (as measured by service attendance) and screening for breast, cervical, and colorectal cancers; (2) the potential mediating role of social support in these relationships; and (3) the potential moderating effect of race/ethnicity in understanding the relationship of religious service attendance and social support.
Methods
Data Source and Sample
Data for this study come from the National Cancer Institute’s (NCI) 2005 Health Information National Trends Survey (HINTS 3). The HINTS is a cross-sectional survey that assesses health communication among the US adult population with specific focus on cancer-related information. The 2005 survey used random digit dialing to obtain a nationally representative sample. All interviews were completed over the telephone, and data were collected from February 2005 through August 2005. Households were contacted over telephone to determine eligibility, and the screener response rate was 34 %. After eligibility was determined, the respondent took part in the extended interview, and the response rate was 61 %. Further detailed descriptions of the sampling strategy and survey methodology are available elsewhere (US Department of Health and Human Services 2005). The HINTS survey was completed by 5,394 participants. The present study focused on non-Hispanic Whites (n = 4,152), non-Hispanic Blacks (n = 454), and Hispanics (n = 496) as these racial and ethnic groups comprised 96 % (N = 5,102) of the total survey respondents.
Measures
Religious service attendance was captured in one item asking, “Not including funerals and weddings, how often do you attend religious services?” (every week/once or twice a month/a few times a year/never). We dichotomized responses to reflect whether respondents ever attended religious services or never attended religious services.
A Social Support Index was constructed by summing three items that encompass facets of social support: membership in social networks, emotional support, and instrumental support. Respondents were asked: “How many community organizations are you currently a member of?” (values provided by respondents), “Do you have friends or family members that you talk to about your health?” (yes/no), and “How many people live near you who you can rely on in case you need a ride to visit your health care provider?”(values provided by respondents). Respondents received a point for each item if they indicated any count equal to or greater than one, for a possible range of scores from 0 to 3 with lower scores indicating lower social support.
Race/ethnicity served as the moderator variable for the analyses. Respondents were asked, “Are you Hispanic or Latino?” If they responded yes, they were categorized as Hispanic, regardless of other race affiliation. Respondents were also asked, “Which one or more of the following would you say is your race?” Non-Hispanic respondents were categorized as White or Black if they identified with either racial category. Those who responded as multiracial or “other” were excluded from the analyses.
Recent cancer screening was assessed with the following questions (adapted for each screening test): “When did you have your most recent Pap smear/mammogram/stool blood test using a home kit/sigmoidoscopy or colonoscopy?” Respondents were considered up-to-date with their most recent screening test based on the following criteria: women ages 18 and older who received a Pap test within the past 3 years, women ages 40 and older who received a mammogram within the past 2 years, and men and women ages 50 and older who received an FOBT in the past year or an endoscopy within the past 5 years. These criteria are based on the 2005 recommendations by the US Preventive Services Task Force (1995). Each respondent was scored using a dichotomized outcome of yes/no for each screening test based on appropriate inclusion criteria.
In our regression analyses, we controlled for variables associated with cancer screening. These covariates included age (values provided by respondents), educational attainment (less than high school diploma/high school graduate or GED/college and beyond), household income (values provided by respondents), and insurance status (uninsured/insured).
Statistical Analysis
All analyses were conducted using SAS (version 9.3) and SAS-callable SUDAAN (version 10; SAS institute, Inc., Cary NC) to account for the complex sampling procedure used to collect HINTS data. Note that the analyses were not weighted because the statistical procedures implemented in this study are not equipped to handle sampling weights. The exclusion criteria mentioned previously resulted in sample sizes of n = 1,474 for Pap smear, n = 1,286 for mammogram, and n = 1,373 for the colorectal cancer screening outcome. We first calculated descriptive statistics of the sample. We then examined bivariate associations between our demographic covariates, religious service attendance, the Social Support Index, and cancer screening.
Lastly, we conducted moderated mediation analyses following conditional process modeling approaches offered by Hayes (2013). Haye’s conditional process modeling (Hayes 2013) is an emerging technique for testing mediation and offers unique capabilities that are not found in traditional methods of testing mediation (e.g., the Causal Steps Approach) such as the simultaneous testing of both moderated and mediated relationships (Baron and Kenny 1986; Judd and Kenny 1981). Conditional process modeling is similar to structural equation modeling techniques; however, it does not require latent variables for path analysis. Conditional process modeling tests indirect effects through bootstrapping and can provide respective confidence intervals. Unlike more traditional tests of indirect effects such as the conservative Sobel test, conditional process modeling does not require assumptions for normally distributed populations and it is ideal for dichotomous outcomes that require nonparametric testing (Mackinnon et al. 1995). Point and bias-corrected 95 % bootstrap confidence interval estimates of indirect effect sizes are generated using 1,000 bootstrap samples (Hayes 2013).
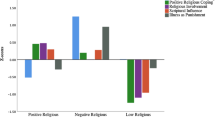
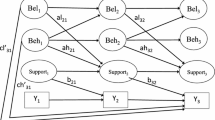
When testing for moderated mediation, we adjusted for relevant covariates (i.e., age, educational attainment, household income, and insurance status). Religious service attendance served as the main predictor variable for cancer screening. Social support served as the mediator variable for the relationship between religious service attendance and cancer screening. Race/ethnicity (contrast indicators were constructed with non-Hispanic Whites as the reference group) served as the moderator variable for the association between religious service attendance and social support. Recent breast cancer screening, cervical cancer screening, and colorectal cancer screening served as the outcome variables in three separate models. Refer to Figs. 1, 2, 3 for the moderated mediation analyses. Values provided in the figures represent path coefficients. Significant path coefficients are denoted.
Results
Population Descriptives
There were a total of 3,366 (66 %) females and 1,736 (34 %) males with a mean age of 52 years (SD = 17.88). Nearly, two-thirds (60 %) had received some college training or more. More than half (56 %) were married, 27 % had incomes that were $75,000 or more, and 88 % reported having health insurance. See Table 1.
Bivariate Associations Among Study Variables
See Table 2.
Conditional Process Modeling—Moderated Mediation
Results of the conditional process analyses are summarized in Table 3 and are described below.
Recent Mammography
The overall model (Fig. 1) accounted for a significant proportion of variance for recent mammography screening (χ 2 = 1,308.57, p ≤ .01; the Nagelkerke R 2 value = .07 and the Cox and Snell R 2 value = .04). The direct path from religious service attendance on recent mammogram screening was significant and was associated with higher likelihood of a recent receipt of a mammogram [β = .70, χ 2 (1) = 3.96, p ≤ .001]. Religious service attendance was positively associated with social support [β = .62, t(1,284) = 13.31, p ≤ .001]. The relationship between social support and recent mammogram screening was not significant [β = .16, χ 2 (1) = 1.51, p = .13]. The findings do not indicate a mediated model; the indirect effect of religious service attendance = (.62) × (.16) = .10; 95 % CI (−.03, .24). Racial identification did not moderate the relationship between religious service attendance and social support.
Recent Pap Screening
The overall model (Fig. 2) accounted for a significant proportion of variance for recent Pap screening (χ 2 = 793.68, p ≤ .001; the Nagelkerke R 2 value = .19 and the Cox and Snell R 2 value = .09). The direct path from religious service attendance on recent Pap testing was not significant [β = .28, χ 2 (1) = 1.17, p = .24]. Religious service attendance was positively associated with social support [β = .51, t(1,472) = 11.76, p ≤ .001]. The association between the social support and recent Pap testing was significant [β = .38, χ 2 (1) = 2.75, p = .01], indicating that higher levels of social support were associated with increased likelihood of having a recent Pap test. These findings suggest a fully mediated model; the indirect effect of religious service attendance = (.51) × (.38) = .19; 95 % CI (.04, .36). Racial identification moderated the mediation model such that the positive association between religious service attendance and social support was stronger for non-Hispanic Blacks than it was for non-Hispanic Whites [β = .35, t(1,472) = 1.97, p = .05].
Recent Colorectal Cancer Screening
The overall model (Fig. 3) accounted for a significant proportion of variance for recent colorectal screening (χ 2 = 1,780.61, p ≤ .001; the Nagelkerke R 2 value = .09 and the Cox and Snell R 2 value = .07). The direct path from religious service attendance on recent colorectal screening was significant [β = .40, χ 2 (1) = 2.63, p ≤ .001]. Religious service attendance was positively associated with social support [β = .61, t(1,367) = 13.86, p ≤ .001]. The association between social support and recent colorectal screening was significant and positive [β = .28, χ 2 (1) = 3.21, p ≤ .001]. The findings suggest a partially mediated in model; the indirect effect of religious service attendance = (.61)*(.28) = .17; 95 % CI (.07, .28). Racial identification did not moderate the relationship between religious service attendance and social support.
Discussion
This study suggests that participation in religious activities is strongly related to the recent use of cancer early detection tests. We found that higher levels of religious service attendance were associated with greater utilization of screening tests for breast, cervical, and colorectal cancers, even after controlling for relevant covariates (i.e., age, education, household income, and insurance status). These findings are consistent with prior studies that demonstrate relatively high levels of cancer screening utilization among those who regularly attend religious services (Allen et al. 2014; Fox et al. 1998; Paskett et al. 1999a).
Our analysis showed that religious service attendance was associated with increased social support. In addition, social support fully mediated the relationship between religious service attendance and recent Pap testing, partially mediated the relationship between religious service attendance and recent colorectal screening, and failed to mediate religious service attendance and recent mammography. This suggests that the underlying mechanisms that link religious service attendance with cancer screening may involve the various functions of social support found in social networks and communities. The functions of social support span a range of activities that include dissemination of information about the importance of screening and resources for obtaining screening services (informational support) (Gotay and Wilson 1998), helping individuals plan, schedule, and follow-through with health care visits (instrumental support) (Kang and Bloom 1993; Suarez et al. 1994), and helping to assuage fears and anxiety associated with screening tests (emotional support) (Allen et al. 2014; Katapodi et al. 2002).
The fact that social support did not mediate the relationship between religious service attendance and breast cancer screening could be due to several factors. Mammography campaigns have been highly successful and screening rates are high; mammography may be perceived as a less intrusive test, as compared to Pap testing and colorectal cancer screening (e.g., colonoscopy). Null findings may also be due to our measure of social support, which assessed global (general) social support, as opposed to support specifically related to cancer screening tests. Lastly, the population that needs regular mammography testing may differ from the study’s other populations. The eligible population for regular cervical cancer screening is comprised of a subset of younger females that may include immigrant women who may rely more on social support found within religious networks than older nonimmigrant women. In addition, eligible populations for colorectal cancer screening include both men and women, and research indicates that there may be gender differences in the role of health cognitions on cancer screening that could influence the efficacy of social support (Lee and Im 2013). As a result, future studies should address gender differences in the association between social support and cancer screening.
We observed that the positive association between religious service attendance and social support differed across racial groups, but not for all types of screening. Overall, the association between religious service attendance and social support was stronger among non-Hispanic Blacks as compared to non-Hispanic Whites. Yet, this was true only for recent cervical cancer screening; there were no significant differences by race for recent breast or colorectal cancer screening. Although Black and White women demonstrate similar high rates of cervical cancer screening in national surveys, the sociodemographic characteristics that are associated with screening differ among these populations. For example, a study by Selvin and Brett (2003) found that income, education, and Medicaid were stronger predictors of recent cancer screening among non-Hispanic Whites than non-Hispanic Blacks, suggesting racial differences in the role of structural barriers in cancer screening (Selvin and Brett 2003). Black women face greater social disadvantage (e.g., poverty) than other groups, as well as significant barriers to cervical cancer screening that include inadequate access to health care services, poor knowledge of screening recommendations, culturally inappropriate or insensitive cancer control materials, competing priorities, fear and fatalism, low literacy, and mistrust of the health care system (Thomas et al. 2005; Wolff et al. 2003). It may be that Black women rely more heavily on social support from religious networks to overcome these barriers to screening for cervical cancer, a potentially stigmatized cancer due to the sexual transmission of HPV (Lichtenstein 2003; Perrin et al. 2006). Continued research that explores the potential moderating role of race/ethnicity in other population-based surveys is warranted to determine whether this finding can be replicated.
Across all groups, the use of colorectal cancer screening was substantially lower than utilization of breast and cervical cancer screening. Notably, Hispanic women had lower rates of recent screening than any other subgroup in this sample. This finding is consistent with other national surveys (Bolen et al. 2000; Merrill et al. 2013; CDC 2012) and likely reflects issues of inadequate access to health care, disadvantaged socioeconomic status, and potential language and cultural barriers (Diaz et al. 2008). For example, 40 % of the Hispanics in our sample lacked health insurance, compared to 15 % of non-Hispanic Blacks and 8 % of non-Hispanic Whites. In addition, 42 % of the Hispanics in our sample lacked a high school diploma, compared to 21 % of non-Hispanic Blacks and 8 % of non-Hispanic Whites.
Several limitations of this study warrant mention. First, the cross-sectional nature of our analysis limits our ability to make causal inferences or rule out reciprocal causation. Second, the size of the Hispanic sample is small, thus limiting our ability to conduct subgroup analyses across heterogeneous Hispanic ethnicities. Third, this study assessed only one dimension of religiosity—religious service attendance. While attendance of religious services is an important aspect of religiosity, it is not a comprehensive measure of religious commitment, coping, or behavior. Studies considering other dimensions of religiosity (e.g., denomination, beliefs) that likely influence health behavior on multiple levels and through multiple pathways are needed. Some studies have found that use of preventative services varies by denomination (e.g., Mainline Protestant or Jewish denominations use certain preventive services more than Evangelical Protestants) (Benjamins 2006; Reindl Benjamins and Brown 2004; Shelton et al. 2011) and that religious beliefs of certain religious groups may deter cancer screening (Azaiza and Cohen 2006; Underwood et al. 1999). Therefore, it would be important for future studies to examine the influence of denominational differences on screening behavior.
Nonetheless, this study contributes new information to the field of religion and health through its unique methodological approach, which can lend additional insights into underlying mechanisms that relate religiosity to cancer screening behavior. The large and relatively diverse sample enabled us to examine interactions among religious service attendance, social support, and multiple cancer screening behaviors and assess the potential moderating role of race/ethnicity in these relationships.
Implications for Intervention
In all, our study suggests that harnessing the power of social ties and the social support that is provided by faith-based organizations and networks may be a successful cancer control intervention strategy. These conclusions are supported by published intervention studies, such as Body & Soul and The North Carolina Breast Cancer Screening Program, which demonstrated that faith-based interventions that employ lay health advisors (also known as “community health workers”) can be effective in increasing screening participation (Earp et al. 2002; Resnicow et al. 2004). While the specific roles of lay health advisors have varied in intervention research, they generally include the dissemination of health messages (informational support), reduction in barriers to access of screening tests (instrumental support), and provision of emotional support to those who may be fearful of screening.
Consistent with results from five national probability samples (Taylor et al. 1996), our results indicate that older non-Hispanic Blacks attend religious services more regularly than other racial/ethnic groups. These findings suggest that faith-based models of social influence may be particularly valuable for reaching underserved non-Hispanic Blacks, who generally have less access to screening services and are more likely to be diagnosed with cancer at late stages (Davis et al. 1994). Faith-based organizations play central roles in many Black communities, and a substantial body of research has shown that they are willing partners in cancer prevention and control efforts (Campbell et al. 1999, 2007). Given their unique ability of to reach large audiences, stable infrastructures, altruistic missions, elaborate communication channels, and natural social networks, faith-based organizations offer an important opportunity for interventions to reduce cancer screening disparities (Baskin et al. 2001). Interventions that utilize social support offer the potential to draw on the strengths of faith-based organizations—the relationships between members, the importance of the family, and traditional cultural and religious values—to improve screening among high-risk groups.
Researchers should continue to seek novel ways to understand how social influence and support structures in faith-based settings can be utilized to promote the appropriate use of screening. Specifically, studies that assess various dimensions of social support (e.g., emotional, instrumental) and those that assess both general and screening-specific support would be valuable. If certain dimensions of social support are found to be particularly important in screening, then interventions that focus on these support dimensions will likely be more effective. Since religious service attendance had a direct influence on screening behaviors, future research should also explore other mediating pathways, such as attitudinal, structural, and sociocultural influences. In addition, examining the effects of religious service attendance at later points in the cancer continuum (e.g., follow-up to an abnormal finding, treatment adherence, end of life) might offer insights into other potential ways to work with faith-based organizations to impact health. Faith-based organizations are often very involved in offering support for those that are sick and dying (Taylor et al. 2000); this suggests that they may have the capacity to include preventative health support to their missions. Finally, more information on beliefs stemming from religious traditions, teachings, and practices that may influence screening behaviors would be valuable, as they can inform the development of interventions to increase screening in specific subgroups with high rates of cancer, as well as in the general population.
References
Allen, J. D., Pérez, J. E., Pischke, C. R., Tom, L. S., Juarez, A., Ospino, H., et al. (2014). Dimensions of religiousness and cancer screening behaviors among church-going Latinas. Journal of Religion and Health, 53(1), 190–203. doi:10.1007/s10943-012-9606-9
Azaiza, F., & Cohen, M. (2006). Health beliefs and rates of breast cancer screening among Arab women. Journal of Womens Health, 15(5), 520–530. doi:10.1089/jwh.2006.15.520.
Baron, R. M., & Kenny, D. A. (1986). The moderator mediator variable distinction in social psychological-research—conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. doi:10.1037/0022-3514.51.6.1173.
Baskin, M. L., Resnicow, K., & Campbell, M. K. (2001). Conducting health interventions in black churches: A model for building effective partnerships. Ethnicity and Disease, 11(4), 823–833.
Benjamins, M. R. (2006). Religious influences on preventive health care use in a nationally representative sample of middle-age women. Journal of Behavioral Medicine, 29(1), 1–16.
Berkman, L. F., & Glass, T. (2000). Social integration, social networks, social support, and health. In L. F. Berkman & I. Kawachi (Eds.), Social epidemiology (pp. 137–173). USA: Oxford University Press.
Bolen, J. C., Rhodes, L., Powell-Griner, E. E., Bland, S. D., & Holtzman, D. (2000). State-specific prevalence of selected health behaviors, by race and ethnicity–Behavioral Risk Factor Surveillance System, 1997. MMWR CDC Surveillance Summaries, 49(2), 1–60.
Botoseneanu, A., Alexander, J. A., & Banaszak-Holl, J. (2011). To test or not to test? The role of attitudes, knowledge, and religious involvement among US adults on intent-to-obtain adult genetic testing. Health Education and Behavior, 38(6), 617–628.
Bradley, D. E. (1995). Religious involvement and social resources—evidence from the data set Americans changing lives. Journal for the Scientific Study of Religion, 34(2), 259–267.
Campbell, M. K., Demark-Wahnefried, W., Symons, M., Kalsbeek, W. D., Dodds, J., Cowan, A., et al. (1999). Fruit and vegetable consumption and prevention of cancer: the Black Churches United for Better Health project. American Journal of Public Health, 89(9), 1390–1396.
Campbell, M. K., Hudson, M. A., Resnicow, K., Blakeney, N., Paxton, A., & Baskin, M. (2007). Church-based health promotion interventions: Evidence and lessons learned. Annual Review of Public Health, 28, 213–234. doi:10.1146/annurev.publhealth.28.021406.
Centers for Disease Control and Prevention. (2012). Cancer screening—United States, 2010. MMWR. Morbidity and Mortality Weekly Report, 61(3), 41–45.
Chatters, L. M. (2000). Religion and health: Public health research and practice. Annual Review of Public Health, 21, 335–367. doi:10.1146/annurev.publhealth.21.1.335.
Cokley, K., Garcia, D., Hall-Clark, B., Tran, K., & Rangel, A. (2012). The moderating role of ethnicity in the relation between religiousness and mental health among ethnically diverse college students. Journal of Religion and Health, 51(3), 890–907. doi:10.1007/s10943-010-9406-z.
Davis, D. T., Bustamante, A., Brown, C. P., Wolde-Tsadik, G., Savage, E. W., Cheng, X., et al. (1994). The urban church and cancer control: a source of social influence in minority communities. Public Health Reports, 109(4), 500–506.
Diaz, J. A., Roberts, M. B., Goldman, R. E., Weitzen, S., & Eaton, C. B. (2008). Effect of language on colorectal cancer screening among Latinos and non-Latinos. Cancer Epidemiology Biomarkers Prevention, 17(8), 2169–2173. doi:10.1158/1055-9965.epi-07-2692.
Earp, J. A., Eng, E., O’Malley, M. S., Altpeter, M., Rauscher, G., Mayne, L., et al. (2002). Increasing use of mammography among older, rural African American women: Results from a community trial. American Journal of Public Health, 92(4), 646–654. doi:10.2105/Ajph.92.4.646.
Ellison, C. G., & Levin, J. S. (1998). The religion-health connection: evidence, theory, and future directions. Health Education and Behavior, 25(6), 700–720.
Erwin, D. O., Spatz, T. S., Stotts, R. C., & Hollenberg, J. A. (1999). Increasing mammography practice by African American women. Cancer Practice, 7(2), 78–85.
Fox, S. A., Pitkin, K., Paul, C., Carson, S., & Duan, N. (1998). Breast cancer screening adherence: Does church attendance matter? Health Education and Behavior, 25(6), 742–758.
Gamarra, C. J., Paz, E. P., & Griep, R. H. (2009). Social support and cervical and breast cancer screening in Argentinean women from a rural population. Public Health Nursing, 26(3), 269–276. doi:10.1111/j.1525-1446.2009.00779.x.
Gartner, J., Larson, D. B., & Allen, G. D. (1991). Religious commitment and mental-health: A review of the empirical literature. Journal of Psychology and Theology, 19(1), 6–25.
Gotay, C. C., & Wilson, M. E. (1998). Social support and cancer screening in African American, Hispanic, and Native American women. Cancer Practice, 6(1), 31–37.
Gottlieb, B. H., & Bergen, A. E. (2010). Social support concepts and measures. Journal of Psychosomatic Research, 69(5), 511–520. http://dx.doi.org/10.1016/j.jpsychores.2009.10.001.
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press.
Hill, T. D., Ellison, C. G., Burdette, A. M., & Musick, M. A. (2007). Religious involvement and healthy lifestyles: evidence from the survey of Texas adults. Annals of Behavioral Medicine, 34(2), 217–222. doi:10.1080/08836610701566993.
Holt, C. L., Litaker, M. S., Scarinci, I. C., Debnam, K. J., McDavid, C., McNeal, S. F., et al. (2013). Spiritually based intervention to increase colorectal cancer screening among African Americans: Screening and theory-based outcomes from a randomized trial. Health Education and Behavior, 40(4), 458–468. doi:10.1177/1090198112459651.
Holt, C. L., Roberts, C., Scarinci, I., Wiley, S. R., Eloubeidi, M., Crowther, M., et al. (2009). Development of a spiritually based educational program to increase colorectal cancer screening among African American men and women. Health Communication, 24(5), 400–412.
Homan, K. J., & Boyatzis, C. J. (2010). Religiosity, sense of meaning, and health behavior in older adults. International Journal for the Psychology of Religion, 20(3), 173–186. doi:10.1080/10508619.2010.481225.
Husaini, B. A., Sherkat, D. E., Bragg, R., Levine, R., Emerson, J. S., Mentes, C. M., et al. (2001). Predictors of breast cancer screening in a panel study of African American women. Women and Health, 34(3), 35–51.
Jessor, R., Turbin, M. S., & Costa, F. M. (1997). Protective factors in adolescent health behavior. Journal of Personality and Social Psychology, 75(3), 788–800.
Judd, C. M., & Kenny, D. A. (1981). Process analysis—estimating mediation in treatment evaluations. Evaluation Review, 5(5), 602–619. doi:10.1177/0193841x8100500502.
Kang, S. H., & Bloom, J. R. (1993). Social support and cancer screening among older black Americans. Journal of the National Cancer Institute, 85(9), 737–742.
Katapodi, M. C., Facione, N. C., Miaskowski, C., Dodd, M. J., & Waters, C. (2002). The influence of social support on breast cancer screening in a multicultural community sample. Oncology Nursing Forum, 29(5), 845–852. doi:10.1188/02.onf.845-852.
Katz, M. L., Kauffman, R. M., Tatum, C. M., & Paskett, E. D. (2008). Influence of church attendance and spirituality in a randomized controlled trial to increase mammography use among a low-income, tri-racial, rural community. Journal of Religion and Health, 47(2), 227–236.
Kaye, J., & Raghavan, S. K. (2002). Spirituality in disability and illness. Journal of Religion and Health, 41(3), 231–242. doi:10.1023/A:1020284819593.
Kendler, K. S., Gardner, C. O., & Prescott, C. A. (1997). Religion, psychopathology, and substance use and abuse: A multimeasure, genetic-epidemiologic study. American Journal of Psychiatry, 154(3), 322–329.
Kinney, A. Y., Bloor, L. E., Dudley, W. N., Millikan, R. C., Marshall, E., Martin, C., et al. (2003). Roles of religious involvement and social support in the risk of colon cancer among Blacks and Whites. American Journal of Epidemiology, 158(11), 1097–1107. doi:10.1093/aje/kwg264.
Kinney, A. Y., Bloor, L. E., Martin, C., & Sandler, R. S. (2005). Social ties and colorectal cancer screening among Blacks and Whites in North Carolina. Cancer Epidemiology, Biomarkers and Prevention, 14(1), 182–189.
Klassen, A., & Washington, C. (2008). How does social integration influence breast cancer control among urban African-American women? Results from a cross-sectional survey. BMC Women’s Health, 8(1), 1–10. doi:10.1186/1472-6874-8-4.
Lee, H. Y., & Im, H. (2013). Colorectal cancer screening among Korean American immigrants: Unraveling the influence of culture. Journal of Health Care for the Poor and Underserved, 24(2), 579–598.
Levin, J. S., & Chatters, L. M. (1998). Religion, health, and psychological well-being in older adults: Findings from three national surveys. Journal of Aging and Health, 10(4), 504–531. doi:10.1177/089826439801000406.
Lichtenstein, B. (2003). Stigma as a barrier to treatment of sexually transmitted infection in the American deep south: issues of race, gender and poverty. Social Science and Medicine, 57(12), 2435–2445. http://dx.doi.org/10.1016/j.socscimed.2003.08.002.
Lukwago, S. N., Kreuter, M. W., Holt, C. L., Steger-May, K., Bucholtz, D. C., & Skinner, C. S. (2003). Sociocultural correlates of breast cancer knowledge and screening in urban African American women. American Journal of Public Health, 93(8), 1271–1274.
Ma, G. X., Gao, W., Tan, Y., Chae, W. G., & Rhee, J. (2012). A community-based participatory approach to a hepatitis B intervention for Korean Americans. Progress in Community Health Partnerships, 6(1), 7–16. doi:10.1353/cpr.2012.0002.
Mackinnon, D. P., Warsi, G., & Dwyer, J. H. (1995). A simulation study of mediated effect measures. Multivariate Behavioral Research, 30(1), 41. doi:10.1207/s15327906mbr3001_3.
McCullough, M. E., Hoyt, W. T., Larson, D. B., Koenig, H. G., & Thoresen, C. (2000). Religious involvement and mortality: A meta-analytic review. Health Psychology, 19(3), 211–222. doi:10.1037//0278-6133.19.3.211.
McFall, S. L., & Davila, M. (2008). Gender, social ties, and cancer screening among elderly persons. Journal of Aging and Health, 20(8), 997–1011.
Merrill, R. M. (2001). Demographics and health-related factors of men receiving prostate-specific antigen screening in Utah. Preventive Medicine, 33(6), 646–652.
Merrill, R. M., Harris, J. D., & Merrill, J. G. (2013). Differences in incidence rates and early detection of cancer among non-Hispanic and Hispanic Whites in the United States. Ethnicity and Disease, 23(3), 349–355.
Morgan, P. D., Fogel, J., Tyler, I. D., & Jones, J. R. (2010). Culturally targeted educational intervention to increase colorectal health awareness among African Americans. Journal of Health Care for the Poor and Underserved, 21(3), 132–147.
Nguyen, A. B., Belgrave, F. Z., & Sholley, B. K. (2009). Development of a breast and cervical cancer screening intervention for Vietnamese American women: A community-based participatory approach. Journal of Womens Health, 18(5), 754–755.
Nguyen, A. B., Hood, K. B., & Belgrave, F. Z. (2012). The relationship between religiosity and cancer screening among Vietnamese women in the United States: The moderating role of acculturation. Women and Health, 52(3), 292–313.
Paskett, E. D., Case, L. D., Tatum, C., Velez, R., & Wilson, A. (1999a). Religiosity and cancer screening. Journal of Religion and Health, 38(1), 39–51.
Paskett, E. D., Tatum, C. M., D’Agostino, R., Rushing, J., Velez, R., Michielutte, R., et al. (1999b). Community-based interventions to improve breast and cervical cancer screening: Results of the Forsyth County Cancer Screening (FoCaS) Project. Cancer Epidemiology, Biomarkers and Prevention, 8(5), 453–459.
Perrin, K. M., Daley, E. M., Naoom, S. F., Packing-Ebuen, J. L., Rayko, H. L., McFarlane, M., et al. (2006). Women’s reactions to HPV diagnosis: Insights from in-depth interviews. Women and Health, 43(2), 93–110. doi:10.1300/J013v43n02_06.
Reindl Benjamins, M., & Brown, C. (2004). Religion and preventative health care utilization among the elderly. Social Science and Medicine, 58(1), 109–118.
Resnicow, K., Campbell, M. K., Carr, C., McCarty, F., Wang, T., Periasamy, S., et al. (2004). Body and Soul: A dietary intervention conducted through African-American churches. American Journal of Preventive Medicine, 27(2), 97–105. doi:10.1016/j.amepre.2004.04.009.
Rew, L., & Wong, Y. J. (2006). A systematic review of associations among religiosity/spirituality and adolescent health attitudes and behaviors. Journal of Adolescent Health, 38(4), 433–442.
Schoenberg, N. E., Hatcher, J., Dignan, M. B., Shelton, B., Wright, S., & Dollarhide, K. F. (2009). Faith moves mountains: An Appalachian cervical cancer prevention program. American Journal of Health Behavior, 33(6), 627–638.
Selvin, E., & Brett, K. M. (2003). Breast and cervical cancer screening: Sociodemographic predictors among White, Black, and Hispanic women. American Journal of Public Health, 93(4), 618–623. doi:10.2105/Ajph.93.4.618.
Shelton, R. C., Snavely, A. C., De Jesus, M., Othus, M. D., & Allen, J. D. (2011). HPV vaccine decision-making and acceptance: Does religion play a role? Journal of Religion and Health,. doi:10.1007/s10943-011-9553-x.
Suarez, L., Lloyd, L., Weiss, N., Rainbolt, T., & Pulley, L. (1994). Effect of social networks on cancer-screening behavior of older Mexican-American women. Journal of the National Cancer Institute, 86(10), 775–779.
Taylor, R. J., Chatters, L. M., Jayakody, R., & Levin, J. S. (1996). Black and white differences in religious participation: A multisample comparison. Journal for the Scientific Study of Religion, 35(4), 403–410. doi:10.2307/1386415.
Taylor, R. J., Ellison, C. G., Chatters, L. M., Levin, J. S., & Lincoln, K. D. (2000). Mental health services in faith communities: The role of clergy in black churches. Social Work, 45(1), 73–87. doi:10.1093/sw/45.1.73.
Thomas, V. N., Saleem, T., & Abraham, R. (2005). Barriers to effective uptake of cancer screening among Black and minority ethnic groups. International journal of palliative nursing, 11(11), 562, 564–571.
Underwood, S. M., Shaikha, L., & Bakr, D. (1999). Veiled yet vulnerable: Breast cancer screening and the Muslim way of life. Cancer Practice, 7(6), 285–290.
US Department of Health and Human Services. (2005). Health information trends survey, 2005. Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, National Cancer Institute.
U.S. Preventative Services Task Force. (1995). Guide to clinical preventative services. Baltimore, MD: Recommendations of the US Preventative Services Task Force.
Van Ness, P. H., Kasl, S. V., & Jones, B. A. (2002). Are religious women more likely to have breast cancer screening? Journal of Religion and Health, 41(4), 333–346.
Wallace, J. M., & Forman, T. A. (1998). Religion’s role in promoting health and reducing risk among American youth. Health Education and Behavior, 25(6), 721–741. doi:10.1177/109019819802500604.
Wolff, M., Bates, T., Beck, B., Young, S., Ahmed, S. M., & Maurana, C. (2003). Cancer prevention in underserved African American communities: barriers and effective strategies: A review of the literature. WMJ, 102(5), 36–40.
Acknowledgments
This study was supported in part by Cooperative Agreement Number U48DP001946 from the Centers for Disease Control and Prevention. The findings and conclusions in this journal article are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leyva, B., Nguyen, A.B., Allen, J.D. et al. Is Religiosity Associated with Cancer Screening? Results from a National Survey. J Relig Health 54, 998–1013 (2015). https://doi.org/10.1007/s10943-014-9843-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-014-9843-1