Abstract
A stratified randomized sample of 525 middle age (35–64 years old) men was used to study the relationships between self-reported level of church attendance (CA), self-reported religious faith (SRRF), religious well-being (RWB), existential well-being (EWB), self-actualization (SA), health, lifestyle, and participation in physical activity (PA). Religious measures (RWB, CA, and SRRF) were found to be dependent on psychosocial variables in terms of their relationships with PA, lifestyle, and health. On the other hand, psychosocial resourcefulness (SA, EWB, social support, and stress management) showed independent relationships with lifestyle, PA, and health. These findings indicate that the positive associations of psychological and sociological constructs with health are not related to or dependent upon ego syntonic religious identity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The impact of religiosity on health and lifestyle is currently a bourgeoning field of investigation. Koenig et al. (2001) wrote a critical, comprehensive, and systematic analysis of more than 1,200 studies and 400 research review articles on the relationship between religiosity and health. In the vast majority of the cross-sectional studies and prospective cohort studies, the presence of religious beliefs was consistently associated with better health and lifestyle practice (Koenig et al. 2001). Membership in a religious denomination and frequent participation in worship are associated, for instance, with lower mortality rates and disease. A meta-analytic review (McCullough et al. 2000) indicates that the effect of religious involvement on health is comparable in magnitude to the effect of exercise on coronary heart disease (CHD). However, as Koenig et al. (2001) demonstrate religious influences do not always convert into health benefits, and in some cases, the opposite seems to be true.
Problem Statement
Psychosocial resourcefulness is widely regarded as an important factor in optimal or positive psychological functioning and correlates well with psychological variables like self-esteem, self-confidence, internal locus of control, maturity, hardiness, self-acceptance, happiness, and self-actualization (Van der Merwe 1997; Koenig et al. 2001). Most if not all of the aforementioned measures of psychosocial resourcefulness also show clear and positive relationships with lifestyle, participation in physical activity and physical health (Van der Merwe 1997).
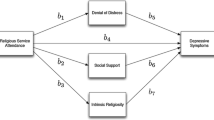
McCullough et al. (2000) suggest that the association of religious involvement and physical health might be more closely tied to the psychological support networks that religion provides rather than any positive psychological states engendered specifically by any particular form of religious experience. McCullough et al. (2000) further state that it is important to understand the mechanisms of the relationship between faith and health as well as the underlying interface between religious experience and psychological health. Several researchers have discussed possible pathways or mechanisms by which religiousness might influence health (McCullough et al. 2000; Koenig et al. 2001; George et al. 2002; Lawler and Young 2002). Research on the health benefits of religion has focussed primarily on four dimensions: (a) public participation (attendance at religious services and activities), (b) religious affiliation (membership in major religious groups), (c) private religious practices (e.g., prayer, meditation, reading religious materials), and (d) religious coping (the extent to which the individual turns to religion when coping with problems). These dimensions correlate positively but modestly with each other and not equally powerfully with health outcomes.
Attendance at religious services and religious coping are the two dimensions most strongly related to physical and mental health. Koenig et al. (2001) found no evidence that social support mediates the relationship of religion with physical and mental health. It seems then that it is not so much the social interaction or connectedness of religious practices within religious communities that mediates the putative effect of religion upon health but the impact of religion on thought processes and mental states. Jensen et al. (1990) found that religious beliefs need to be internalized before they affect adolescent lifestyle-related behaviors. George et al. (2002) indicate that there are clearly negative and positive forms of religious coping. Negative religious coping is characterized by feeling punished or abandoned by God, believing that illness is a result of sin, and similar cognitions. Positive religious coping is characterized by faith in God, the belief that God loves, cares for, and strengthens, the sense that one is working with God to manage and cure illness; a sense that one is part of a larger purpose; and having a sense of meaning.
These aspects (sense of meaning, having a larger purpose, feeling that life is manageable, feeling happy, and content) are also the characteristics of the psychologically healthy or self-actualized individual. This raises the question of whether those who are self-actualized benefit in better health even if they are not religious and to what extent the presence of self-actualized characteristics depends on not only being religious but also the quality of the religious experience. There is a need for a better understanding of how measures of religiousness (like self-reported religious faith (SRRF), church attendance, and the quality of the religious experience) relate to each other and to measures of psychosocial resourcefulness (like social support, stress management, and self-actualization).
According to Maslow (1970), self-actualization is the ultimate state of psychosocial resourcefulness. Hill and Hood (1999) indicate that self-actualization correlates negatively with various measures of religiosity and argue that this might indicate that religious commitments interfere with the development of self-actualization. While studying people whom he regarded as self-actualized, Maslow (1970, 1987) became aware of the importance of peak experiences and the role that the individual’s perception of God plays in the development of self-actualization. In his view, openness to mystical experiences and flexibility in religious views are central to optimal psychological health (Maslow 1970). On the other hand, people with a strong tendency to rational, mechanistic worldviews and who perceive their religious traditions to be perfect or beyond question tend not to be self-actualized (Maslow 1970).
This distinction might be important to consider when studying religiosity’s relationship with lifestyle and health. A rigid religious belief system and a mechanistic, authoritarian conceptual world view or core life philosophy could be accompanied by high levels of self-reported religious faith (SRRF), but not necessarily with quality relationships with God (RWB) and high levels of self-actualization. However, Maslow’s findings were based on interviews with a number of individuals that he identified as self-actualized, and it is unclear whether his conclusion would hold true for the general population.
Geller (1982, 1984) argues that the fundamental claims of both Rodgers and Maslow’s self-actualization theories are wrong, that they have little to offer in terms of understanding and improving the human condition, and that we would do better to reject the whole self-actualization theory. Self-actualization refers to being true to oneself, which according to Geller (1982, 1984) is a vague concept grounded in the theory that humans have a good or mystical essence. Characteristics of self-actualized individuals are that they have a higher than normal sense of purpose and that they seem less dependent on social approval than most people. They also perceive life as manageable, display high levels of goal-related commitment and seem to flourish in stressful or challenging circumstances.
Finally, positive psychological health could be related to quality of religious experience without it being a product of religious expression. Psychosocial health could therefore be the common denominator explaining to a large extent the associations between religiousness, lifestyle and health. Pargament (1997) indicates that the quality of the religious experience or how people engage religious beliefs in the process of coping might be crucial in understanding how religious beliefs and practices mediate health benefits. This suggests that high levels of self-reported religious faith in the absence of experiencing quality relationships with God might not relate to better physical and mental health. The questions also arises of whether quality relationships with God equate to better health in the absence of near optimum or at least reasonable levels of psychosocial health.
This study therefore aims to investigate the following questions: (1) Do measures of psychosocial health (self-actualization (SA), stress management, existential well-being and social support) influence the relationship between self-reported religious faith (SRRF) and religious well-being (RWB)? (2) Are SRRF, RWB, and SA related to lifestyle and health independently or only when present in combination with each other? (3) Which of these religious variables (SRRF and RWB) and psychosocial variables (SA, EWB, social support, and stress management) as well as lifestyle measures (physical activity, lifestyle, health responsibility, and nutrition) are the most important contributors to the variations in health?
Method
The subjects of the study were 525 Caucasian male inhabitants of Potchefstroom, a city with 129,000 inhabitants, located in the Northwest Province of South Africa. The city demographics still reflect, to a large extent, the Apartheid tendency where certain areas were more densely populated with either white or black populations. The nine suburbs or city sections that are most densely populated with white (Caucasian or European) inhabitants were targeted for the purpose of this study, and 12% of the white males between the ages 35 and 64 were randomly approached, in each of the suburbs, and asked to participate. This stratification process culminated in a sample of 533 males, of whom 525 eventually completed all the questionnaires. Females were not included because menopausal women could slant the health results, and Black Africans were excluded because of language/terminology differences could restrict and confound the data. These considerations will be addressed and investigated in follow-up projects. Conclusions drawn from this study therefore relate to males who are White Afrikaans speaking (90% of the group) and who are middle aged (35–64 years). They come from a Western tradition of organized religion, primarily the Calvinist stream of Protestant Christianity.
Measure of Illness
Symptomatology was measured through the Seriousness of Illness Rating Scale (IRS) (Wyler et al. 1968), a self-reported checklist of 126 commonly recognized physical and mental symptoms and diseases. In the development of this instrument, a general severity weight for each disorder was obtained by asking a large sample of physicians and lay persons to rate each of them. This carefully developed scale of seriousness of illness has served as a frequent tool in stress and illness studies (Kobasa et al. 1981; Schroeder and Costa 1984).
Measure of Self-Actualization, Lifestyle, and Physical Activity
Walker et al.’s (1987) Health Promoting Lifestyle Profile (HPLP) was used to evaluate self-actualization. An overall measure of the health-promoting component of lifestyle was obtained along with measures of six subscales: (1) self-actualization, (2) health responsibility, (3) exercise, (4) nutrition, (5) interpersonal support, and (6) stress management. The three aspects of self-actualization that this sub scale assesses are personal growth, life satisfaction, and close personal relationships. This scale assesses personal growth by examining issues like experiencing growth, having long-term goals, being aware of strengths and weaknesses, setting goals, respecting accomplishments and having a purpose in life. Life satisfaction is assessed by whether the person likes himself/herself, feels happy/content, looks forward to the future, finds his/her days challenging and has a satisfying environment. Interpersonal support was determined by a 15-item scale. The scale incorporates items concerned with a sense of intimacy and closeness (rather than more casual interpersonal relationships). The scale focuses on amount of contact, but also includes aspects that relate to subjective satisfaction (with interpersonal support) such as being able to praise others, enjoying touching, having meaningful interpersonal relationships, spending time with close friends and being able to express feelings.
The seven Belloc and Breslow habits (BB) (Berkman and Syme 1979) were used to evaluate the respondents’ likelihood of engaging in health-promoting behavior. Respondents were asked to answer ‘yes’ or ‘no’ to statements about these habits: (1) eating three meals daily without snacking, (2) eating breakfast daily, (3) participating in moderate exercise two to three times a week, (4) maintaining moderate body weight, (5) not smoking, (6) drinking little or no alcohol, and (7) sleeping enough (7–8 h a night). Men and women of all age groups following six or seven of these habits lived 9 and 11 years longer, respectively, than individuals answering ‘yes’ to three or less according to Berkman and Syme (1979). The quality of the respondents’ participation in physical activity was measured and quantified with the Physical Activity Index (Sharkey 1984).
Measure of Quality of Personal Relationship with God
Ellison’s (1983) Spiritual Well-Being Scale (SW) was used to measure quality of personal relationships with God. This instrument consists of 20 items responded to on a six-point scale ranging from strongly agree to strongly disagree. Responses for each of the items are assigned a numerical value of 1–6. Ten of the items are designed to measure quality of personal relationship with God or Religious Well-Being (RWB) and 10 items measure Existential Well-Being (EWB).
Self-Reported Religious Faith (SRRF)
Self-reported religious faith was measured with a two-item religiosity index: “How often do you attend religious services?” and “How religious are you?” (Oleckno and Blacconiere 1991). The choices were “Never”, “Sometimes”, “Often” and “Routinely” for the first question and “Very Religious”, “Somewhat Religious” and “Not Religious” for the second question. A religiosity variable (CA/SRRF) was created by combining these two items. For the purpose of the ANOVA, the respondents were divided into two groups, low and high, according to their responses to the first question (SRRF). Those who chose the option “very religious” were classified as high and those who chose the options “somewhat” and “not at all” were rated as low.
Coronary Risk Index
Coronary risk was assessed with an Index developed by Bjurstrom and Alexiou (1978). This index assesses risk by assigning a risk value on a likert scale format to 14 coronary risk factors. The risk factors include age, heredity, body weight, smoking, exercise, cholesterol, systolic blood pressure, diastolic blood pressure, gender, stress, present cardiovascular disease symptoms, past personal history of cardiovascular disease, diabetes mellitus, and gout.
Statistical Analysis of the Data
The Statistica computer software statistical analysis package was used to analyze the data. The relationships of SRRF, RWB and SA with lifestyle, IRS, the physical activity index, and the coronary risk index (CRI) were analyzed with correlations, a factorial ANOVA, as well as with a multiple regression analysis.
For the purpose of the factorial ANOVA, the respondents were placed in groups with regard to SA and SRRF. Regarding SA, those with values higher or equal to 80% of the group distribution were classified as high and those with values lower than 20% as low. Respondents with values between 21 and 79% of the group distribution were classified as moderate. Respondents were dichotomized into two groups, low and high, with regard to their response to the question: “How religious are you?” Those who responded “very religious” were classified as high and those who answered “somewhat” and “not at all” were rated low. The Newman-Keuls post hoc test was used to determine group statistical differences.
Results and Discussion
Means and standard deviations for the spiritual well-being, lifestyle, and health status scales are shown in Table 1. The group mean scores for RWB, EWB, and SWB compare favorably with group means reported by Bufford, Paloutzian, and Ellison (1991). The highest score possible for the RWB subscale is 60 and with a group mean of 51.2, there is the possibility of a ceiling effect. Bufford et al. (1991) indicate in this regard that the spiritual well-being scale does not discriminate well among people scoring above the mean (50th percentile) and is therefore limited in its ability to identify individuals functioning at the highest level of spiritual well-being.
Spirituality and Health
Scores on the total spiritual well-being scale, the two subscales existential well-being and religious well-being, self-reported religious faith (SRRF) and church attendance were correlated with measures of lifestyle, physical activity, and health (Table 2). The two religiosity variables (SRRF and CA) correlated moderately with each other (r = 0.54, p < 0.001) and this compares well with correlations (r = 0.543) reported by Oleckno and Blacconiere (1991).
The correlation between SRRF and self-actualization is r = 0.32, which means they share 10% (0.322 = 0.10 × 100) of their variance. The implication is that the effects of SRRF and self-actualization on health and lifestyle will not be confounded. Also, as the results in Table 2 indicate, self-actualization shows a more meaningful coefficient of determination (r 2) to the variances of psychosocial constructs, such as health responsibility (0.362 = 12.9% versus 0.142 = 1.96%), social support (0.852 = 72% versus 0.282 = 7.8%), and stress management (0.552 = 30% versus 0.172 = 2.8%) than SRRF. Self-actualization also explains more of the variances of overall health (HPLP- 0.802 = 64% versus 0.282 = 7.8%), the Coronary risk index (0.142 = 1.96% versus 0.062 = 0.4%) and the illness rating scale (0.232 = 5.3% versus 0.142 = 1.96%) than SRRF. Religiousness therefore seems to relate statistically significantly (p ≤ 0.05) but weakly to measures of psychosocial resourcefulness, quality of religious experience, and very weakly with measures of lifestyle and health.
Self-reported religious faith (SRRF) shares 20% (0.452 = 0.20) of its variance with RWB and 8.4% (0.292 = 0.084) with EWB, while church attendance shares 29% (0.472) and 15% (0.392) of its variance with RWB and EWB, respectively. This is significant in the context of this study, because it clearly demonstrates that neither ego syntonic religious identity, or what might be called ‘complacent religiousness’ or ‘blind faith’, nor conventional religious behavior (seing oneself as religious and regularly attending religious services) is synonymous with quality relationships with God and/or higher levels of existential well-being (a sense of coherence or that life is a positive, happy, and meaningful experience). Self-actualization (SA) correlates more strongly with EWB than CA (0.53 versus 0.39) and SRRF (0.53 versus 0.29). SA therefore shares more of its variances with EWB (0.532 = 28.1%) than is the case with either CA (15.2%) or SRRF (8.4%). This is because both the SA and EWB questionnaires include questions about sense of meaning and purpose, while the CA and SRRF questionnaires do not. Also, the SA scale has questions about personal relationships and personal growth and accordingly share more of its variance with SS (0.582 = 72.3%) and SM (0.552 = 30.3%) than is the case with EWB (0.432 = 18.5% with SS and 0.322 = 10.2% with SM) which has no questions about personal growth and relationships.
It is not clear whether self-actualization’s stronger correlation with SS and SM than with EWB really makes a difference in terms of health and lifestyle because SA does not show stronger correlations with the physical activity index (0.10 versus 0.21), the Belloc and Breslow habits (0.11 versus 0.22), the Coronary risk index (−0.14 versus −0.16), the illness rating scale (−0.23 versus −0.26) and nutritional habits (0.17 versus 0.17) than EWB.
The two measures of self-reported religious faith (how religious are you and regular church attendance) showed weaker correlations with lifestyle and health (health responsibility, nutritional habits, the Belloc and Breslow habits, the Coronary risk index, and the Illness rating scale) than self-actualization and existential well-being. Existential well-being and self-actualization also correlated better with measures of psychosocial resourcefulness (social support and stress management). This is in line with current theory that the mechanism of the relationship of faith/religion with health might be mediated by lifestyle and psychosocial factors (Lawler and Young 2002; Edmondson et al. 2005).
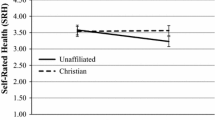
To determine whether SRRF would show a relationship with quality of personal relationship with God (RWB), lifestyle and health independent of self-actualization, a two-way analysis of variance was conducted. Results of this analysis are presented in Tables 3 and 4, as well as in Figs. 1 and 2.
Self-Reported Religious Faith, Self-Actualization, and Religious Well-Being
Religiosity showed a statistically significant (p ≤ 0.05) relationship with the quality of an individual’s personal relationship with God. This was evident in all three self-actualization groups. Self-actualization also showed a statistically significant (p ≤ 0.05) relationship with RWB independent from level of religiousness.
Respondents low in religiosity but high in self-actualization reported better quality relationships with God than individuals with low self-actualization and high religiosity scores (compare groups b and e in Table 3). However, the difference is not statistically significant.
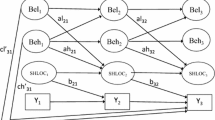
The results in Table 3; Fig. 1 indicate that self-actualization influenced the relationship between SRRF and RWB. In all three of the self-actualized groups, those perceiving themselves as religious (high SRRF) reported statistically significant higher quality relationships with God than those perceiving themselves as not religious (see three lines in Fig. 1). The higher the level of self-reported religious faith, the higher the quality of the individual’s relationship with God. People classified as ‘high’ with regard to self-actualization reported better overall quality relationships with God. This was the case regardless of whether they perceive themselves to be religious or not (compare group e with group b). Level of psychological functioning (self-actualization) therefore seems to determine or predict the quality of the individual’s relationship with God. The question now arises of whether this also affected the health protective value of religiousness.
Self-Reported Religious Faith, Self-Actualization, and Health
Results of a factorial ANOVA, where the dependent and independent relationships of self-reported religious faith and self-actualization were compared with measures of health, are reported in Table 3; Fig. 2. Respondents were grouped according to SRRF (low and high) and self-actualization (low, moderate, and high) for the purpose of these statistical comparisons.
Self-reported religious faith showed no relationship with lifestyle, health or coronary risk independent of self-actualization (Fig. 2). The pattern(s) seen in Fig. 2 showing the clear and independent relationship of self-actualization with the illness rating scale are also evident with other measures of health (coronary risk index) as well as with measures of lifestyle (five subscales of the HPLP, Belloc and Breslow habits, physical activity index), as can be seen in Table 3. Higher levels of religiosity on the other hand were not concomitant with higher or lower lifestyle, health or coronary risk index values within any of the self-actualization groups.
The F-ratio, p-values, Eta2, and Wilks Lambda scores of the factorial Anova reported in Table 3 can be seen in Table 4. This Table provides information on the independent and combined contributions of SA and SRRF to the variances of the dependent variables. Self-actualization (SA) contributes more to the variances of virtually all the dependent variables (except nutrition) than self-reported religious faith (SRRF). The Wilks Lambda scores indicate that the two independent variables (SA and SRRF) in combination fail to explain between 70 and 98% of the variances of the dependent variables, with the exception of social support where they fail to explain 40% of the variance. These are small overall contributions to measures of lifestyle and health by both independent variables (SA and SRRF).
These results indicate that the dependent variables contribute statistically significantly (p ≤ 0.05) to psychological constructs, lifestyle, and health, with SA being the more dominant independent contributor. However, neither of the two independent variables (SA and SRRF) explain independently, or in combination, major parts of variability within any of the dependent variables.
A multiple regression analysis was done to determine the individual predictive value of the measures of religiousness and psychosocial resourcefulness. The results of this analysis are reported in Table 5. Measures of religious and psychosocial resourcefulness were entered to predict scores on the illness rating scale, lifestyle (Belloc and Breslow habits), the physical activity index (PAI), health responsibility (HR), and nutrition.
The results indicate that lower health status and lifestyle scores were predicted by higher psychosocial (EWB, SA and SS) scores but not by religiousness (CA, SRRF, CA./SRRF-ratio and RWB).
The negative signs for existential well-being (EWB = −0.17), self-actualization (SA = −0.261), and social support (SS = −0.231) indicate that for every 1 standard deviation increase in SA, EWB, and SS, there is a 0.17, 0.26, and 0.23 decrease in the respective IRS values. As lower IRS scores indicate better health, this signifies that higher EWB, SA, and SS scores are predictive of better health.
The issue of the true contribution and of the hierarchical contribution of religious (SRRF, Church attendance and RWB), psychosocial (SA, social support, EWB, and stress management), and lifestyle measures to the variance of health now arises. More specifically, the question arises whether religious and psychosocial variables would contribute at all to the variance of physical health in a stepwise multiple regression analysis if lifestyle measures are included as part of such an analysis?
The contribution of the seven Belloc and Breslow lifestyle habits and the religious and psychosocial measures to the variance of the IRS was evaluated by means of a stepwise multiple regression analysis (Table 6). The results show that regular physical exercise contributed most, namely 10.5%, to the variance of Wylers’s Illness Rating Scale (IRS). Five other variables also contributed statistically significantly (p ≤ 0.05) to the variance of IRS: self-actualization (3.9%), social support (1.7%), not smoking (1.2%), maintaining body weight (1.0%), and existential well-being (0.7%). Self-reported religious faith (SRRF) was listed as a non-significant (p > 0.05) contributor. Religious well-being was not listed as a contributor. The combined contribution of the nine variables listed as contributors to the variance of the IRS was only 19.8%.
Conclusions
In this study, self-actualization shares 28 and 23% of its variance with existential well-being (EWB) and religious well-being (RWB), respectively. The two measures of religiosity (SRRF and CA), on the other hand, shares between 10 and 15% of their respective variances with self-actualization and EWB. Religiosity was therefore not a particularly strong predictor of sense of meaning or purpose. Psychosocial constructs such as social support and stress management were more clearly and powerfully related to measures of meaningfulness and purpose (SA and EWB) than SRRF and CA. Religious well-being (RWB) shared a statistically significant percent (p ≤ 0.05) of its variance (23%) with self-actualization, but was a poor independent predictor/contributor to measures of lifestyle and health.
George et al. (2000) proposed three mechanisms whereby religion could be related to health: the promotion of health behaviors, provision of social support and the coherence hypothesis. Our study indicates that the relationships between religiosity (RWB, SRRF and CA), lifestyle, and health might be mediated by psychosocial mechanisms and lifestyle.
Individuals with high levels of self-actualization scored best in lifestyle and health measures. These individuals, whether they perceived themselves as religious or not, seemed to have healthier lifestyles and reported better health. Religious measures, on the other hand, correlated significantly (p ≤ 0.05) with psychosocial resourcefulness (self-actualization, stress management, and social support) but contributed very little to the variances of these constructs and showed poor independent relationships with health and lifestyle. This finding suggests that the association of religious involvement with physical health is closely related to psychosocial resourcefulness and that these positive psychosocial states are not necessarily a product of, or dependent upon, religiousness.
Miller and Thoresen (2003) observed that nearly all the findings on spirituality/religion and health come from research conducted in the USA. This limits the extent to which current data can be generalized to other populations. Our study contributes to current knowledge by providing data from a non-USA population. However, organized religion in South Africa has a strong Western influence, primarily the Calvinist form of Protestant Christianity with relatively rigid (even negative) views of activities like meditation, yoga and other Eastern spiritual practices such as mindfulness meditation and Thai Chi. Several researchers have shown that these Eastern spiritual practices improve psychosocial health and characteristics like self-actualization and self-esteem (Seeman et al. 2003; Chandler et al. 2005).
Whether the findings of this study apply to other religious paths, females, and diverse ethnic or cultural groups are questions that need further investigation. Powell et al. (2003) reviewed studies investigating the relationship of religious service attendance with mortality and report a 25% reduction in mortality with increasing levels of church/service attendance after adjustment for confounders, in at least 6 studies.
Powell et al. (2003) conclude that religion’s protective value against cardiovascular disease is largely mediated by lifestyle, and their research also failed to support a link between depth of religiousness and physical health. We measured health with the illness rating scale and a coronary risk index, both of which have limitations. The IRS includes all physical ailments (like accidents and infectious diseases) over the last year and not just chronic and lifestyle-related diseases. This could weaken the strength of the relationships that psychosocial mechanisms and religiosity show with IRS, but would not influence relationships with lifestyle or the CRI. The CRI includes aspects such as gender, age, stress, and participation in physical activity and should therefore have a stronger relationship with both lifestyle and psychosocial constructs like stress management. However, neither religiosity nor the psychosocial measuring devices share more of their respective variances with the CRI than is the case with the IRS. It is consequently debatable whether health status measuring devices per se are the reason for the relatively weak relationships found between measures of religiosity and health.
The limitations of this study should be noted. First, the results from a sample of middle aged males with a strict conservative Western Calvinist religious orientation may not be applicable to other populations. Second, the cross-sectional nature of the study precludes causal interpretation, and third, the data was obtained from self-reported questionnaires, which may have base expectancy effects.
Finally, the operational definitions of religiosity and self-actualization used in the study were rather narrow in scope. More multidimensional or comprehensive measuring devices should be utilized in future studies that focus on enhancing current understanding of the mechanisms by which religiosity and psychosocial resourcefulness relate to health.
What these results in the final analysis indicate is that measuring devices that essentially assess ego syntonic religious identity, as well as what was called above complacent religiousness or “blind faith” (seeing oneself as religious and regularly attending religious services), might not be sensitive or comprehensive enough to explore the intricate relationships between religious orientation and health. As stated in the introduction, it seems that it is not so much the social interaction or connectedness of religious practices that mediates effect, but the impact of religion on thought processes and mental states. Mental thought processes that foster positive health outcomes (like being self-actualized) is, however, not dependent -in our sample- on being religious or on the quality of the religious experience. This might not be the case with all types of religious orientation. Aspects like meditation, level of faith development, God concept and peak experiences might impact positively on mental processes in the sense that it could enhance self-actualization thought process.
Latest trends in this area of research include the development and use of instruments that capture spirituality and mysticism. Measuring devices can now focus specifically on feelings of transcendence and experiences of something bigger than the ego/self and the material world. This avenue of research is in line with Maslow’s observations that openness to mystical experiences and flexibility in religious views are central to optimal psychological health. Important questions that therefore need to be considered are: whether experiences of a sense of meaning and/or purpose are purely secular phenomena or whether they are advanced by (if not grounded in) peak experiences and higher levels of faith development? These experiences and/or the level of faith development are likely to affect the quality of religious experience and how people engage religious beliefs in the process of coping. This, as Pargament (1997) indicated, might be crucial to understanding how religious beliefs and practices mediate health benefits.
In this study, SA shared only 23% (0.482 = 23.0) of its variance with RWB (quality of religious experience). Self-actualization (SA) also correlated slightly better with health responsibility (0.36 versus 0.23), the physical activity subscale (0.21 versus 0.19), social support (0.85 versus 0.44), stress management (0.55 versus 0.33) and the illness rating scale (−0.23 versus −0.18) than RWB. As indicated, the RWB scale used in this study seems to have a ceiling effect and is therefore limited in its ability to identify individuals with the highest levels of quality religious experiences.
To advance knowledge on how religious beliefs mediate health, it would therefore be useful to investigate whether self-actualization, psychosocial resourcefulness, health and lifestyle practices, and their respective interrelationships are advanced and/or influenced by factors like level of faith development, quality of the religious experience, God concept, spirituality, and mysticism.
References
Berkman, L., & Syme, S. (1979). Social networks, host resistance, and mortality: A nine year follow-up study of Alameda Country residents. American Journal of Epidemiology, 109, 186–204.
Bjurstrom, L. A., & Alexiou, N. G. (1978). A Program of heart disease intervention for public employees: A five year report. Journal of Occupational Medicine, 20(8), 521–531.
Bufford, R. K., Paloutzian, R. F., & Ellison, C. W. (1991). Norms for the spiritual well-being scale. Journal of Psychology and Theology, 19(1), 56–70.
Chandler, H. M., Alexander, C. N., & Heaton, D. P. (2005). The transcendental meditation program and postconventional self-development: A 10-year longitudinal study. Journal of Social Behavior and Personality, 17, 93–121.
Edmondson, K. A., Lawler, K. A., Jobe, R. L., Younger, J. W., Piferi, R. L., & Jones, W. H. (2005). Spirituality predicts health and cardiovascular responses to stress in young adult women. Journal of Religion and Health, 44(2), 161–171.
Ellison, C. W. (1983). Spiritual well-being: conceptualization and measurement. Journal of Psychology and Theology, 11(4), 330–340.
Ellison, C. G. (1991). Religious involvement and subjective well-being. Journal of Health and Social Behavior, 32, 80–99.
Ellison, C. W., & Smith, J. (1991). Towards and integrative measure of health and well-being. Journal of Psychology and Theology, 19(1), 35–48.
Geller, L. (1982). The failure of self-actualization theory: A critique of Carl Rogers and Abraham Maslow. Journal of Humanistic Psychology, 22, 56–73.
Geller, L. (1984). Another look at self-actualization. Journal of Humanistic Psychology, 24, 93–106.
George, L. K., Ellison, C. G., & Larson, D. B. (2002). Explaining the relationship between religious involvement and health. Psychological Inquiry, 13(3), 190–200.
George, L. K., Larson, D. B., Koenig, H. G., & McCullough, M. E. (2000). Spirituality and health: What we know, what we need to know. Journal of Social and Clinical Psychology, 19(2), 102–116.
Hill, P. C., & Hood, R. W. (1999). Measures of religiosity. Birmingham: Religious Education Press.
Jensen, L., Newall, R. J., & Holman, T. (1990). Sexual behaviour, church attendance, and permissive beliefs among unmarried young men and women. Journal of Scientific Study of religion, 29, 113–117.
Kobasa, S. C., Maddi, S. R., & Courington, S. (1981). Personality and constitution as mediators in the stress-illness relationship. Journal of Health and Social Behavior, 22, 368–378.
Koenig, H. G., McCullough, M. E., & Larson, D. B. (2001). Handbook of religion and health. Oxford: Oxford University press.
Lawler, K. A., & Young, J. W. (2002). Theobiology: An analysis of sprirituality; cardiovascular responses, stress, mood, and physical health. Journal of Religion and Health, 41(4), 347–362.
Maslow, A. H. (1970). Religions, values, and peak-experiences. New York: Penguin Books USA, Inc.
Maslow, A. H. (1987). Motivation and personality. New York: Addison-Wesley Educational Publishers, Inc.
McCullough, M. E., Hoyt, W. T., Larson, D. B., Koenig, H. G., & Thoresen, C. (2000). Religious involvement and mortality: A meta-analytic review. Health Psychology, 19(3), 211–222.
Miller, W. R., & Thoresen, C. E. (2003). Spirituality, religion and health. American Psychologist, 58(1), 24–35.
Oleckno, W. A., & Blacconiere, M. J. (1991). Relationship of religiosity to wellness and other health-related behaviors and outcomes. Psychological Reports, 68, 819–826.
Pargament, K. I. (1997). The psychology of religion and coping. New York: Guilford Press.
Powell, L. H., Shahabi, L., & Thoresen, C. E. (2003). Religion and spirituality: Linkages to physical health. American Psychologist, 58(1), 36–52.
Schroeder, D. H., & Costa, P. T. (1984). Influence of life event stress on physical illness: substantive effects or methodological flaws. Journal of Personality and Social Psychology, 46, 853–863.
Seeman, T. E., Dubin, L. F., & Seeman, M. (2003). Religiosity/Spirituality and health: A critical review of the evidence of biological pathways. American Psychologist, 58, 53–63.
Sharkey, B. J. (1984). Physiology of fitness. Champaign, IL: Human Kinetics.
Van der Merwe, S. (1997). The relationship between physical activity and spiritual well-being with lifestyle and health. Potchefstroom (Unpublished PhD-thesis—PU for CHE).
Walker, S. N., Sechrist, K. R., & Pender, N. J. (1987). The health promoting lifestyle profile: development and psychometric characteristics. Nursing Research, 36(2), 76–78.
Wyler, A. R., Masuda, M., & Holmes, T. H. (1968). Seriousness of illness rating scale. Journal of Psychosomatic Research, 11, 363–374.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dreyer, L.I., Dreyer, S. Religious Involvement, Psychosocial Resourcefulness, and Health. J Relig Health 51, 1172–1187 (2012). https://doi.org/10.1007/s10943-010-9423-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-010-9423-y