Abstract
To improve the long-term results of psychological treatments, it is important to know why some people constantly have a healthy weight and others face difficulties in losing weight or maintaining it. This study aimed to identify psychological factors associated with maintaining or regaining weight loss and determine the psychological characteristics of individuals with different BMI levels. 282 adult participants responded to questionnaires measuring eating behaviors, general and specific irrational beliefs, and self-efficacy. We used MANOVA analysis to identify the differences between the categories of participants. Our results showed that there are differences between the regainers and maintainers VS those with healthy stable weight in terms of self-efficacy (F (2, 84) = 7.17, p = .001), irrationality (F (2, 84) = 8.15, p < .001), and eating behaviors (F (2, 84) = 7.95, p < .001). Furthermore, people with healthy weight had more self-efficacy about their eating behaviors (F (2,273) = 6.49, p = .002), and more cognitive restraint (F (2, 273) = 3.58, p = .029), lower levels of specific irrational beliefs (F (2, 273) = 10.17, p < .000) and emotional eating (F (2, 273) = 20.24, p < .000) than participants with obesity or overweight. Some psychological factors are relevant for weight loss and explain why some people with overweight or obesity find it difficult to lose weight and maintain it.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2016, World Health Organization (WHO) reported that worldwide more than 1.9 billion adults were overweight, of which more than 650 million were obese. This illness poses a significant risk for several chronic diseases, such as cardiovascular diseases, diabetes, musculoskeletal disorders, and some forms of cancers. Although there are many obesity treatments, WHO’s high numbers suggest that people’s weight loss attempts are arduous. Moreover, if they manage to succeed in these attempts, it is highly problematic for people with obesity or overweight to maintain their weight loss (Cooper et al., 2010).
There are three main evidence-based approaches to promoting weight loss: surgical treatment, pharmacotherapy, and behavioral treatment. Their efficiency is from 47% weight loss in surgical cases (O’Brien et al., 2013) to 10% in behavioral or pharmacotherapy treatment (Tak & Lee, 2021). Nevertheless, weight loss is almost always regained, and maintenance remains the most significant challenge (Cooper & Fairburn, 2001; Spirou et al., 2021). So it is essential to identify psychological factors that can generate and sustain weight-loss behaviors. Research in this field is important because we know little about the psychological mechanisms and determinants responsible for weight loss and maintenance of loss, which could improve or advance treatments for obesity (Byrne et al., 2003, 2004; Byrne, 2002).
Based on the current literature, the psychological factors that could engender weight loss are cognitive variables, such as self-efficacy and irrational beliefs, and behavioral variables, such as emotional eating and cognitive restraint. We will summarize below the research that has documented their relation to weight loss.
Many studies (Edell et al., 1987; Jeffery et al., 1984; Linde et al., 2006; Palmeira et al., 2007; Teixeira et al., 2010) found self-efficacy (SE) to be positively associated with weight loss, weight maintenance, and corresponding weight-loss behaviors (Linde et al., 2006).
In cognitive-behavioral therapy, more specifically in the Rational Emotive Behaviour Therapy (REBT) of Albert Ellis (Ellis, 1962, 1991, 1995), vulnerability factors for psychopathology are considered irrational beliefs (IB) (David et al., 2018). These beliefs are dysfunctional evaluative cognitions that lack pragmatic, empiric, and logical support. In contrast, rational beliefs (RB) are functional evaluative cognitions that have empirical and logical support, are pragmatic, and express preferences rather than demands (David et al., 2005). Rational and irrational beliefs are considered mechanisms of change because changing irrational beliefs lead to dysfunctional behaviors such as maladaptive coping strategies related to uncontrolled or emotional eating (Nolan & Jenkins, 2019). Irrational beliefs were found to be positively associated with dietary restraint (Ruderman, 1985), obsession with eating, dieting (Tomotake et al., 2002), and emotional eating (Nolan & Jenkins, 2019). Irrational food beliefs (IFB) are defined as cognitive distortions and unhealthy attitudes towards food (Osberg et al., 2008). In their review, Greaves et al., (2017) found that catastrophic thinking in response to failures, and rigid, rule-bound thinking influence the challenge of weight loss maintenance.
Behavioral factors, such as cognitive restraint, uncontrolled, and emotional eating, have been documented to predict weight change or weight maintenance (Teixeira et al., 2010, 2015). Also, Varkevisser et al., (2019) found a moderate level of evidence that uncontrolled eating and emotional eating during weight loss and weight loss maintenance were negatively predictive of weight loss maintenance. In a qualitative study, the lack of vigilance regarding weight control varies between individuals who maintain their weight loss and those who regain it (Byrne et al., 2003). Cognitive restraint (CR) (restrained eating) refers to conscious eating restriction to control body weight or lose weight. Uncontrolled eating (UE) is the tendency to eat more than usual or healthy due to a loss of control over intake, and emotional eating (EE) is the tendency to overeat in the presence of emotional distress (Blandine de Lauzon et al., 2004).
However, the main limitation of current literature on this topic is that most studies only look at the difference between obese vs. non-obese individuals and do not consider those who have succeeded or not losing and maintaining weight loss achieved. Only a few studies analyzed this comparison between maintainers and regainers of weight loss. Moreover, most of these studies were quasi-qualitative, relying exclusively on a semi-structured interview or open-ended questions (Byrne, 2002; Lewis et al., 2010). The novel element of our study is that we analyzed irrational beliefs, and examined them in terms of the differences between weight loss maintainers and regainers. Other recent research (Nolan & Jenkins, 2019) was limited to determining if irrational beliefs are associated with food addiction and emotional eating and found that emotional eating mediated the former’s effect on the latter.
We contend that it is essential to know why some people gain weight or find it difficult to lose weight to improve the long-term effects of psychological treatments. Although information exists regarding specific behaviors associated with maintaining or losing weight, we know far less about the psychological factors determining if these behaviors will be maintained. In short, it is unclear why some individuals succeed in weight loss, whereas others do not (Raman et al., 2013).
Objectives
Our study aims to identify which cognitive factors (general and food-specific irrationality, self-efficacy) and behavioral factors (cognitive restraint, uncontrolled and emotional eating) differ between those who have succeeded or not maintaining weight loss and those who could not. Our second aim is to identify psychological variables that characterize better how people with different BMI levels think and behave about food. Therefore, we had two hypotheses. First, the cognitive factors (general and food-specific irrationality, self-efficacy) and behavioral factors (cognitive restraint, uncontrolled and emotional eating) differ between participants who have succeeded or not in maintaining weight loss. More specifically, according to the studies cited above, we expected participants in the Maintainers group to have a higher level of self-efficacy, a lower level of irrational thinking, and a lower frequency of problematic eating behaviors than those from the Regainers group. Second, the cognitive factors (general and food-specific irrationality, self-efficacy) and behavioral factors (cognitive restraint, uncontrolled and emotional eating) differ between participants with different levels of BMI. Related to this hypothesis, we expected participants with a healthy level of BMI to have a higher level of self-efficacy, a lower level of irrational thinking, and a lower frequency of problematic eating behaviors than those with a level of BMI specific to Overweight or Obesity.
Because this research has two aims, we divided it into two sub-studies: study 1 A and 1B.
Study 1 A
Method
Participants and procedures
Our study was conducted following the Declaration of Helsinki, and the protocol was approved (22.655/22.11.2019) by the Ethics Committee of the university where the research was conducted.
Participants registered in the study and completed online the participation consent, information about the study, the data processing, and the questionnaires. The average completion time for each subject was approximately 35 min. At their request, participants in this study received by e-mail the individual results of the completed questionnaires.
The participants were eligible if they were over 18 years old. For this study, we analyzed them in three categories. The first category contained individuals with a constant healthy weight over the last two years. The second category contained individuals who lost a minimum of 10% of their weight in the last two years and they maintained it. The third category contained individuals who lost a minimum of 10% of their weight in the last two years and they regained min 5% of their weight loss through one year. These categories have been defined in other previous studies (Byrne et al., 2003; McGuire et al., 1999). A 5–10% weight loss is considered sufficient to produce significant health benefits, and these benefits are sustained if that weight loss is maintained (Cooper & Fairburn, 2001; Wing et al., 2011). They were recruited from April to June 2019 via online social media.
Depending on the information received regarding weight and whether they have lost weight in the last two years or not, the first author assigned them into three groups (maintainers, regainers, and healthy stable). There was a total consensus between authors regarding the categories.
Measures
All the questionnaires used in this study except for General Attitudes and Beliefs Scale – Short Version (GABS-SV) were developed for this study, through the back-translation method (Roth et al., 2013). First, the original English version was translated into Romanian by the first author, a bilingual clinical psychologist, then back-translated and checked by the second author, a bilingual clinical psychologist.
Eating self-efficacy was measured using the Weight Efficacy Lifestyle Questionnaire – short form (WEL-SF) (Ames et al., 2012). It is a psychometrically valid measure of self–efficacy for controlling eating with eight items. The response is given using a Likert scale in 0 to10 points: 0 for „Not confident at all” and 10 indicates „Very confident.” Higher total scores are associated with higher eating self-efficacy and motivation to make positive lifestyle changes. Cronbach’s α for the scale used in this study was 0.92. The scale had been translated into Romanian.
We measured the irrational beliefs with the 26-item General Attitudes and Beliefs Scale – Short Version (GABS-SV) (Lindner et al., 2007) with one rational subscale, and six irrationality subscales. These are: Self-Downing, Need for Achievement, Need for Approval, Need for Comfort, Demands for Fairness, and Other Downing, based on Albert Ellis’s rational-emotional theory. A total score based on the sum of the subscales scores can be used to assess a total level of irrationality. The scale uses Likert-type ratings from 1 – strongly disagree to 5 strongly agree. In this study, was used the Romanian version of GABS-SV. The scale used in this study has good reliability (Cronbach’s α = 0.89). High scores indicate high irrationality.
The irrational food beliefs were measured with the Irrational Food Beliefs Scale (IFB) (Osberg et al., 2008), which has good reliability for both irrational (Cronbach’s α = 0.89) and rational (Cronbach’s α = 0.70) food beliefs. The scale has been validated on the general population and against other scales that measured related constructs. It has 57 items of which 41 measure irrational beliefs about food and 16 rational ones. The responses are made using Likert-type ratings from 1 – strongly disagree to 4 strongly agree. The highest scores are significantly associated with weight gain and poor weight loss maintenance. The scale had been translated into Romanian and Cronbach’s alpha for the scale in the present study was 0.88.
The eating behaviors were measured using the Three-Factor Eating Questionnaire revised (TFEQ- R21) (Cappelleri et al., 2009; Tholin et al., 2005). The. The scale measures three aspects of eating behavior: cognitive restraint (CR), uncontrolled eating (UE), and emotional eating (EE). It has 21 items. The responses are on a four-point Likert scale ranging from 1 Definitely true to 4 Definitely false with three subscales, one for each domain. Higher scores indicate greater CR, UE, or EE. The scale was translated into Romanian. The Cronbach’s alpha for the scale in the present study was 0.90.
Weight was self-reported. Participants were asked to complete an online questionnaire about their weight in kilograms from three years, two years, one year ago, and the actual one. We need this information to identify their weight loss history. They were also asked to report their height in centimeters.
Statistical methods
Before the statistical analyses, after the visual examination of separate boxplots of all variables, an extreme outlier at Irrational Food Beliefs (more than 3 SD from the group mean) was detected. The score was changed to be one unit above the next highest score in the data set (Field, 2009b). Descriptive statistical analyses were computed to describe the characteristics of the participants, reported as the mean (± SD).
We computed a MANOVA to detect group differences in terms of psychological factors. All data were analyzed using the program Statistical Package for the Social Sciences 20 (SPSS). Because this is an exploratory study and we had no specific hypotheses about how the categories differ in terms of variables, we computed a post hoc analysis using the Games-Howell procedure to compare these differences. This procedure is the most powerful and accurate when sample sizes are unequal, or there is any doubt that group variances are equal (Field, 2009a).
To measure the internal consistency (Cronbach’s alpha) of each translated questionnaire used in this study, we computed Reliability Analyses procedures for using the same software.
Results
Participants
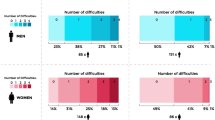
The participants’ flow for study 1 A is described in Fig. 1. The Mean age was 31.05 (SD = 11.37), all adults with a mean BMI of 24.98 kg/m² (SD = 5.58), 82 were women and five men. We grouped them into three categories of interest: 14 Maintainers, 35 Regainers, and 38 with Healthy Stable Weight (Byrne et al., 2003) (see Fig. 1).
The final sample (N = 87) size yielded a statistical power of 0.80 to detect an effect size f²(V) = 0.32 with a Type I error probability of α = 0.05 (Faul et al., 2007).
Outcomes
Using Pillai’s trace, results showed a significant effect of categories on the variables considered V = 0.49, F(22,150) = 2.22, p < .05, η² = 0.25. To determine the nature of this effect, separate univariate ANOVAs were further conducted, and the results are presented in Table 1, showing that category has had a significant effect on self-efficacy, irrational food beliefs, need for approval, uncontrolled eating, cognitive restraint, and emotional eating. We found no significant effect of categories on other irrational thinking styles such as self downing, other downing, need for approval, need for comfort, need for achievement, or demanding for fairness (see Table 1).
The post hoc analysis results showed significant differences between categories when we compared Regainers with Maintainers or Healthy Stable Weight participants on self-efficacy and irrational food beliefs: Regainers had a lower level of self-efficacy than Maintainers and a higher level of irrationality. In comparing Regainers and Normal Stable Weight, we also found significant differences namely, a higher frequency of uncontrolled and emotional eating. In terms of cognitive restraint, the results showed that Maintainers restraint significantly more than Regainers or Healthy Stable Weight. When we compared Regainers with Healthy Stable Weight, we found significantly higher levels of uncontrolled and emotional eating. The results showed that Maintainers cognitive restraint significantly more than Regainers or Healthy Stables. The difference between those with Healthy Stable Weight and Maintainers was non-significant on the other variables. (See Table 2).
Discussion study 1 A
This study reveals the quantitative differences in thinking and behaving between individuals who have succeeded to maintain or not maintain weight loss. Only a few studies analyzed this comparison between maintainers and regainers. Moreover, most of these studies were quasi-qualitative, relying on a semi-structured interview or open-ended questions (Byrne, 2002; Lewis et al., 2010). A novel element is that we analyzed the level of general and specific irrational beliefs. This is important because these beliefs are considered mechanisms of change: changing irrational beliefs leads to changes in dysfunctional behaviors such as maladaptive coping strategies related to eating behaviors (Nolan & Jenkins, 2019).
The results of this study reveal significant differences between the abovementioned categories regarding self-efficacy, irrational food beliefs, uncontrolled eating, and emotional eating. We also found that the irrational belief type regarding the need for approval (e.g., “When people whom I want to like me disapprove of me or reject me, I can not bear their disliking me”) also differed significantly between categories. Post hoc analysis showed that self-efficacy is significantly lower among the Regainers than among the Maintainers or the Healthy Stables, although the latter two categories did not differ significantly. In a recent review (Varkevisser et al., 2019), self-efficacy for weight management was also found to be a determinant that influences weight loss maintenance by stimulating behavior change.
When we examined irrational food beliefs, they were significantly higher among the Regainers than among the Maintainers or the Healthy Stable. We found no significant differences in irrational food beliefs between participants in the Maintainers or Healthy Stable categories. Our findings can explain why Maintainers can keep the lost weight in that they imply that eating is easier to restrain when it is not associated with irrational attitudes such as eating is a source of comfort, relaxation, or the reason for social events.
Moreover, the irrational belief related to the need for approval was significantly higher among the Regainers group than in the Healthy Stable group. It might be that their weight loss motivation is not intrinsic but activated by this irrational belief and this could be the cause of failures in maintaining their weight. Their efforts for weight loss are driven by their need for approval and not because is a healthy thing. This finding is an exciting result that future research needs to investigate further.
Regarding eating behaviors, the Regainers cognitively restraint significantly less than Maintainers. Also, the Regainers group eats significantly more often uncontrolled and emotional than the Healthy Stable group. These findings are in line with other studies which found that emotional eating was associated with greater regain (Sainsbury et al., 2019) and that restrained eating is important to weight maintenance (Levinge et al., 2020). Also, emotional eating and internal disinhibition were found to negatively impact weight loss (Frayn & Knäuper, 2018).
Maintainers and individuals in the Healthy Stable category did not differ in their eating behaviors, except for Cognitive Restraint, an ability learned probably in the weight loss process. Maintainers do not differ significantly from Regainers in terms of uncontrolled and emotional eating; however, increased cognitive restraint among Maintainers may reduce eating behaviors associated with regaining weight, unlike Regainers.
Our results align with previous research, which found that self-efficacy and eating behaviors are important psychological factors in weight loss and weight maintenance (Elfhag & Rossner, 2005; Teixeira et al., 2010, 2015; Varkevisser et al., 2019; Byrne, 2002) also found that the Regainers have more dysfunctional thoughts in terms of dichotomous thinking than the Maintainers. We found that different types of irrationality: food-related and need for approval, are also factors that can be characteristic to a category or another and, therefore, can be essential to address in weight management.
Study 1B
Method
Participants and procedures
The procedure regarding participants was identical to the one described in Study 1 A, except that we analyzed them into three groups under the BMI level: participants with obesity (BMI > 30), overweight (25 < BMI < 30) and healthy weight (18.5 < BMI < 24.9).
Measures
All the questionnaires used in this study were identical to the ones used in Study 1 A. We also computed Cronbach’s α for each questionnaire:
Eating self-efficacy was measured using the Weight Efficacy Lifestyle Questionnaire – short form (WEL-SF) (Ames et al., 2012). Cronbach’s α for the scale used in study 1B, was 0.91.
We measured the irrational beliefs with the 26-item General Attitudes and Beliefs Scale – Short Version (GABS-SV) (Lindner et al., 2007). The scale used in study 1B has a good reliability Cronbach’s α = 0.89.
The irrational food beliefs were measured with the Irrational Food Beliefs Scale (IFB) (Osberg et al., 2008), which has good reliability (Cronbach’s alpha was 0.89).
The eating behaviors were measured using the Three-Factor Eating Questionnaire revised (TFEQ- R21) (Cappelleri et al., 2009; Tholin et al., 2005). The Cronbach’s alpha for the scale in the present study was 0.86.
Weight was self-reported.
Statistical methods
The procedure to analyze data was the same as used in Study 1 A. The only modification is that in this study we did not detect extreme outliers (more than 3 SD from the group mean).
Results
Participants
The participants’ flow for study 1B is described in Fig. 2. After analyzing for eligibility, we included participants 276 adults with a mean age of 31.3 (SD = 11.20) and a mean BMI of 26.93 kg/m² (SD = 5.54). We organized into three groups depending on their BMI: Obesity (78), Overweight (81), and Healthy Weight (117). Of these, 258 were women, and 18 were men (see Fig. 2).
The final sample (N = 276) size yielded a statistical power of 0.80 to detect an effect size f²(V) = 0.14 with a Type I error probability of α = 0.05 (Faul et al., 2007).
Outcomes
Results showed a significant multivariate effect of categories on the variables considered V = 0.25, F(22,528) = 3.45, p < .001, η² = 0.13. To determine the nature of this effect, separate univariate ANOVAs were further conducted, and the results showed that group has had a significant effect on self-efficacy, irrational food beliefs, need for comfort and demand for fairness, uncontrolled eating, cognitive restraint, and emotional eating (see Table 3).
Based on post hoc analysis, when we compared the Obesity with the Healthy Weight group, we found a statistically significant lower level of self-efficacy and a higher level of irrational food beliefs. In terms of eating behaviors, in the Obesity group, we found higher levels of uncontrolled eating, emotional eating, and a lower level of cognitive restraint than in the Healthy Weight group. When we examined the Overweight and the Healthy Weight group, we found that participants from the first group had a statistically significant lower level of self-efficacy and a higher level of irrational food beliefs than the ones from the latter (see Table 4). Also, participants from the Overweight group had a significant higher level of emotional eating and a lower level of cognitive restraint than the ones in the Healthy Weight group.
The post hoc analysis results showed significantly higher levels of need for comfort when we compared the Obesity and Overweight groups with the Healthy Weight group. On the demand for fairness, the difference was statistically significant only between the Overweight and Normal Weight groups (see Table 4), the latter having lower levels.
Discussion study 1B
Previous research explored the potential utility of irrational beliefs and eating behaviors in weight management (Nolan & Jenkins, 2019; Teixeira et al., 2010, 2015) and how some are associated with obesity (Fathabadi et al., 2017; Lewis et al., 2010; Tomotake et al., 2002). Study 1B revealed the psychological differences between persons with obesity, overweight, and healthy weight. We determined significant differences between the aforementioned groups regarding self-efficacy (e.g., “I can resist overeating when I am in a social setting”, etc), irrational food beliefs (e.g.,“Food is a substitute source of comfort”, “To diet is to give up the pleasure of eating”, etc), uncontrolled eating, cognitive restraint, and emotional eating. Our analysis also found that two irrational thinking styles called demanding fairness (e.g., “It is awful and terrible to be treated unfairly by people in my life”) and need for comfort (e.g., “It is unbearable being uncomfortable, tense, or nervous, and I can not stand it when I am”), are also significantly different between these groups.
Post hoc analysis showed that participants from the Obesity or Overweight groups have a significantly lower level of self-efficacy than those from the Healthy weight group. Our results are similar to others (Sainsbury et al., 2019) which found that a perceived success of weight loss maintenance was negatively correlated with BMI. We found no significant differences in terms of self-efficacy between the Obesity and Overweight group. This result can be explained, considering that these two categories of people have gained weight continuously and do not have a desired or healthy weight.
The level of irrational food beliefs was significantly higher in participants from the Obesity group or the Overweight than those from the Healthy weight group but not significantly different between the first two groups. This finding is an exciting result because the attitude towards food can change eating behaviors (Osberg et al., 2008).
Regarding specific types of irrationality not related to food, we found that the levels of need for comfort were significantly higher for those from the Obesity group or the Overweight than those from the Healthy weight group. Also, we found higher levels of demand for fairness in those with overweight. The high level of need for comfort and the demandingness for fairness might explain the inability of participants with overweight or obesity to adhere to a diet, and is a potential mechanism of emotional eating to regulate the negative emotions triggered by these beliefs. These relations need to be further investigated. These results are not necessary in contrast with other findings (Nolan & Jenkins, 2019) which found that irrational beliefs were not correlated with BMI since, in their study, they measured the total level of irrational beliefs given by GABS and not on each type, detailed by this questionnaire.
In terms of eating behaviors, the participants from the Obesity group or the Overweight reported a significantly higher rate of emotional eating, uncontrolled eating, and less cognitive restraint than those from the Healthy weight group. These findings align with others which showed that emotional eating was linked to higher BMI (Sainsbury et al., 2019) and together with internal disinhibition negatively impacted weight outcomes (Frayn & Knäuper, 2018). We found no significant differences in eating behaviors between obese and overweight groups which suggests that similar cognitive mechanisms are involved in both overweight and obesity-related behaviors.
Our results are consistent with previous research and study 1 A, which found that self-efficacy and eating behaviors are important psychological factors in weight loss and maintenance (Elfhag & Rossner, 2005; Teixeira et al., 2010, 2015).
Limitations
Although, used in other studies (Byrne, 2002; Sainsbury et al., 2019), the fact that categories used in this research were made based on retrospective self-reported data on weight, and therefore a remembering bias is possible, can be considered a limitation. In addition, we consider a limitation the fact that we do not know how these participants lost weight. We consider it possible that if the participants lost weight after psychological interventions which aimed to change cognitions or behaviors regarding food, may have influenced them. Also if the participants had comorbid medical (e.g. endocrinological) diseases or were receiving medication (e.g. for mental disorders) that might have caused them to regain the weight they lost is considered another limitation of this study.
This study included mainly women and their overrepresentation in this study can be considered another limitation since it may limit the generalizability. The imbalance can be explained because women are more motivated and interested in their health, body weight, and body image than men (Roslim et al., 2021), and under social pressure, they are more willing to change their weight (Grogan, 2016) but also because women were associated with a higher number of weight loss attempts through a lifetime. With all this, a recent study found that gender was not significantly predictive of weight loss maintenance (Varkevisser et al., 2019).
Other limitations are the small number of participants and the fact that the study is cross-sectional. Therefore, a causal prediction or explanation is not appropriate. Thus, future studies should include a larger sample and employ a longitudinal design to overcome these limitations.
General conclusions
We found that psychological factors could potentially explain why some people may or may not maintain their weight following successful weight loss. Also, the results of study 1B specify relevant cognitive factors (i.e., self-efficacy, irrational beliefs) and eating behaviors of participants with obesity or overweight and how they differ from those with a healthy weight.
Our findings have important clinical implications because to improve weight loss maintenance interventions it is essential to study successes and failures. To know how individuals who succeed or failed in weight loss maintenance think and behave is crucial to increase the rate of success of psychological interventions. This information is important so that during the weight-loss intervention, we develop in our patients the skills necessary for maintenance, skills identified in those from the Maintainers group.
To create more efficient interventions for weight loss and its maintenance, it is also important to know the psychological characteristics of people with obesity or overweight. For example, given that people with obesity or overweight have a high level of need for comfort and demand for fairness, psychological interventions must address and restructure these beliefs. Also, the steps of the intervention must be calibrated to these needs until these beliefs are restructured. Thus, for an improved and tailored psychological intervention for weight loss, clinicians can consider their cognitive and behavioral characteristics of them.
Availability of Data and Material
Data are available on request.
Code Availability
Not applicable.
References
Ames, G. E., Heckman, M. G., Grothe, K. B., & Clark, M. M. (2012). Eating self-efficacy: Development of a short-form WEL. Eating Behaviors, 13(4), https://doi.org/10.1016/j.eatbeh.2012.03.013
de Blandine, M., Deschamps, V., Lafay, L., Borys, J. M., Karlsson, J., Ducimetière, P., & Charles, M. A. (2004). The Three-Factor Eating Questionnaire-R18 Is Able to Distinguish among Different Eating Patterns in a General Population. The Journal of Nutrition, 134(9), 2372–2380. https://doi.org/10.1093/jn/134.9.2372
Byrne, S., Cooper, Z., & Fairburn, C. (2003). Weight maintenance and relapse in obesity: a qualitative study. International Journal of Obesity, 27(8), 955–962. https://doi.org/10.1038/sj.ijo.0802305
Byrne, S. M. (2002). Psychological aspects of weight maintenance and relapse in obesity. Journal of Psychosomatic Research, 53(5), 1029–1036. https://doi.org/10.1016/S0022-3999(02)00487-7
Byrne, S. M., Cooper, Z., & Fairburn, C. G. (2004). Psychological predictors of weight regain in obesity. Behaviour Research and Therapy, 42(11), 1341–1356. https://doi.org/10.1016/j.brat.2003.09.004
Cappelleri, J. C., Bushmakin, A. G., Gerber, R. A., Leidy, N. K., Sexton, C. C., Lowe, M. R., & Karlsson, J. (2009). Psychometric analysis of the Three-Factor Eating Questionnaire-R21: Results from a large diverse sample of obese and non-obese participants. International Journal of Obesity, 33(6), https://doi.org/10.1038/ijo.2009.74
Cooper, Z., Doll, H. A., Hawker, D. M., Byrne, S., Bonner, G., Eeley, E. … Fairburn, C. G. (2010). Testing a new cognitive behavioural treatment for obesity: A randomized controlled trial with three-year follow-up. Behaviour Research and Therapy, 48(8), 706–713. https://doi.org/10.1016/j.brat.2010.03.008
Cooper, Z., & Fairburn, C. G. (2001). A new cognitive behavioural approach to the treatment of obesity. Behaviour Research and Therapy, 39(5), 499–511. https://doi.org/10.1016/S0005-7967(00)00065-6
David, D., Cotet, C., Matu, S., Mogoase, C., & Stefan, S. (2018). 50 years of rational-emotive and cognitive-behavioral therapy: A systematic review and meta-analysis. Journal of Clinical Psychology, 74(3), 304–318. https://doi.org/10.1002/jclp.22514
David, D., Montgomery, G. H., Macavei, B., & Bovbjerg, D. H. (2005). An empirical investigation of Albert Ellis’s binary model of distress. Journal of Clinical Psychology, 61(4), 499–516. https://doi.org/10.1002/jclp.20058
Edell, B. H., Edington, S., Herd, B., O’Brien, R. M., & Witkin, G. (1987). Self-efficacy and self-motivation as predictors of weight loss. Addictive Behaviors, 12(1), 63–66. https://doi.org/10.1016/0306-4603(87)90009-8
Elfhag, K., & Rossner, S. (2005). Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity Reviews, 6(1), 67–85. https://doi.org/10.1111/j.1467-789X.2005.00170.x
Ellis, A. (1962). Reason and emotion in psychotherapy
Ellis, A. (1991). The revised ABC’s of rational-emotive therapy (RET). Journal of Rational-Emotive and Cognitive-Behavior Therapy, 9(3), 139–172. https://doi.org/10.1007/BF01061227
Ellis, A. (1995). Changing rational-emotive therapy (RET) to rational emotive behavior therapy (REBT). Journal of Rational-Emotive & Cognitive-Behavior Therapy, 13(2), 85–89. https://doi.org/10.1007/BF02354453
Fathabadi, J., Izaddoust, M., Taghvaee, D., Shallani, B., & Sadeghi, S. (2017). Prediction the risk of obesity based on irrational beliefs, health locus of control and health-oriented lifestyle. Journal of Research in Psychological Health, 11(3), 1–12. https://doi.org/10.29252/rph.11.3.1
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/BF03193146
Field, A. (2009a). Discovering Statistics using SPSS Statistics. SAGE Publications
Field, A. (2009b). Discovering Statistics using SPSS Statistics Third Edition. In SAGE Publications (Vol. 66)
Frayn, M., & Knäuper, B. (2018). Emotional Eating and Weight in Adults: a Review. Current Psychology, 37(4), https://doi.org/10.1007/s12144-017-9577-9
Greaves, C., Poltawski, L., Garside, R., & Briscoe, S. (2017). Understanding the challenge of weight loss maintenance: a systematic review and synthesis of qualitative research on weight loss maintenance. Health Psychology Review, 11(2), 145–163. https://doi.org/10.1080/17437199.2017.1299583
Grogan, S. (2016). Body Image:Body Image: Understanding Body Dissatisfaction in Men, Women and Children, Third Edition (third). Routledge. https://www.taylorfrancis.com/books/9781317400431
Jeffery, R. W., Bjornson-Benson, W. M., Rosenthal, B. S., Lindquist, R. A., Kurth, C. L., & Johnson, S. L. (1984). Correlates of weight loss and its maintenance over two years of follow-up among middle-aged men. Preventive Medicine, 13(2), 155–168. https://doi.org/10.1016/0091-7435(84)90048-3
Levinge, E., Stapleton, P., & Sabot, D. (2020). Delineating the psychological and behavioural factors of successful weight loss maintenance. Heliyon, 6(1), https://doi.org/10.1016/j.heliyon.2019.e03100
Lewis, S., Thomas, S. L., Blood, R. W., Hyde, J., Castle, D. J., & Komesaroff, P. A. (2010). Do Health Beliefs and Behaviors Differ According to Severity of Obesity? A Qualitative Study of Australian Adults. International Journal of Environmental Research and Public Health, 7(2), 443–459. https://doi.org/10.3390/ijerph7020443
Linde, J. A., Rothman, A. J., Baldwin, A. S., & Jeffery, R. W. (2006). The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychology, 25(3), 282–291. https://doi.org/10.1037/0278-6133.25.3.282
Lindner, H., Kirkby, R., Wertheim, E., & Birch, P. (2007). Scala de atitudini si convingeri generale, forma scurta–GABS-SV [General Attitudes and Beliefs Scale, Short Version–GABS-SV](Romanian adaptation by Trip, S.). Sistem de evaluare clinica [A system for clinical assessment]. Cluj-Napoca:RTC
McGuire, M. T., Wing, R. R., Klem, M. L., Lang, W., & Hill, J. O. (1999). What predicts weight regain in a group of successful weight losers? Journal of Consulting and Clinical Psychology, 67(2), 177–185. https://doi.org/10.1037/0022-006X.67.2.177
Nolan, L. J., & Jenkins, S. M. (2019). Food Addiction Is Associated with Irrational Beliefs via Trait Anxiety and Emotional Eating. Nutrients, 11(8), 1711. https://doi.org/10.3390/nu11081711
O’Brien, P. E., MacDonald, L., Anderson, M., Brennan, L., & Brown, W. A. (2013). Long-term outcomes after bariatric surgery: Fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. In Annals of Surgery (Vol. 257, Issue 1). https://doi.org/10.1097/SLA.0b013e31827b6c02
Osberg, T. M., Poland, D., Aguayo, G., & MacDougall, S. (2008). The Irrational Food Beliefs Scale: Development and validation. Eating Behaviors, 9(1), 25–40. https://doi.org/10.1016/j.eatbeh.2007.02.001
Palmeira, A. L., Teixeira, P. J., Branco, T. L., Martins, S. S., Minderico, C. S., Barata, J. T. … Sardinha, L. B. (2007). Predicting short-term weight loss using four leading health behavior change theories. International Journal of Behavioral Nutrition and Physical Activity, 4(1), 1–12. https://doi.org/10.1186/1479-5868-4-14
Raman, J., Smith, E., & Hay, P. (2013). The clinical obesity maintenance model: an integration of psychological constructs including mood, emotional regulation, disordered overeating, habitual cluster behaviours, health literacy and cognitive function. In Journal of obesity (Vol. 2013). https://doi.org/10.1155/2013/240128
Roslim, N. A., Ahmad, A., Mansor, M., Aung, M. M. T., Hamzah, F., Hassan, H., & Lua, P. L. (2021). Hypnotherapy for overweight and obese patients: A narrative review. Journal of Integrative Medicine, 19(1), 1–5. https://doi.org/10.1016/j.joim.2020.10.006
Roth, W. M., Oliveri, M. E., Sandilands, D. D., Lyons-Thomas, J., & Ercikan, K. (2013). Investigating Linguistic Sources of Differential Item Functioning Using Expert Think-Aloud Protocols in Science Achievement Tests. International Journal of Science Education, 35(4), https://doi.org/10.1080/09500693.2012.721572
Ruderman, A. J. (1985). Restraint and irrational cognitions. Behaviour Research and Therapy, 23(5), 557–561. https://doi.org/10.1016/0005-7967(85)90103-2
Sainsbury, K., Evans, E. H., Pedersen, S., Marques, M. M., Teixeira, P. J., Lähteenmäki, L. … Sniehotta, F. F. (2019). Attribution of weight regain to emotional reasons amongst European adults with overweight and obesity who regained weight following a weight loss attempt. Eating and Weight Disorders, 24(2), https://doi.org/10.1007/s40519-018-0487-0
Spirou, D., Smith, E., Wood, K., & Raman, J. (2021). The clinical obesity maintenance model: a structural equation model. Eating and Weight Disorders, 26(6), https://doi.org/10.1007/s40519-020-01034-y
Tak, Y. J., & Lee, S. Y. (2021). Long-Term Efficacy and Safety of Anti-Obesity Treatment: Where Do We Stand? Current Obesity Reports, 10(1), 14–30. https://doi.org/10.1007/s13679-020-00422-w
Teixeira, P. J., Carraça, E. V., Marques, M. M., Rutter, H., Oppert, J. M., De Bourdeaudhuij, I. … Brug, J. (2015). Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Medicine, 13(1), 1–16. https://doi.org/10.1186/s12916-015-0323-6
Teixeira, P. J., Silva, M. N., Coutinho, S. R., Palmeira, A. L., Mata, J., Vieira, P. N. … Sardinha, L. B. (2010). Mediators of Weight Loss and Weight Loss Maintenance in Middle-aged Women. Obesity, 18(4), 725–735. https://doi.org/10.1038/oby.2009.281
Tholin, S., Rasmussen, F., Tynelius, P., & Karlsson, J. (2005). Genetic and environmental influences on eating behavior: The Swedish Young Male Twins Study. American Journal of Clinical Nutrition, 81(3), https://doi.org/10.1093/ajcn/81.3.564
Tomotake, M., Okura, M., Taniguchi, T., & Ishimoto, Y. (2002). Traits of irrational beliefs related to eating problems in Japanese college women. The Journal of Medical Investigation: JMI, 49(1–2), 51–55. http://www.ncbi.nlm.nih.gov/pubmed/11901760
Varkevisser, R. D. M., van Stralen, M. M., Kroeze, W., Ket, J. C. F., & Steenhuis, I. H. M. (2019). Determinants of weight loss maintenance: a systematic review. Obesity Reviews, 20(2), 171–211. https://doi.org/10.1111/obr.12772
Wing, R. R., Lang, W., Wadden, T. A., Safford, M., Knowler, W. C., Bertoni, A. G. … Wagenknecht, L. (2011). Benefits of Modest Weight Loss in Improving Cardiovascular Risk Factors in Overweight and Obese Individuals With Type 2 Diabetes. Diabetes Care, 34(7), 1481–1486. https://doi.org/10.2337/dc10-2415
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
LTC made the project administration, conceptualization, methodology, validation, investigation, formal analysis, and writing – original draft; OAD made conceptualization, methodology, validation, investigation, supervision, and writing –review & editing, and DOD made the supervision.
Corresponding author
Ethics declarations
Conflicts of Interest/Competing Interests
The authors report no conflict of interest.
Ethics Approval
The protocol has the ethical approval 22.655/22.11.2019 of the Ethics Committee from the Babes-Bolyai University, Cluj- Napoca, Romania, where the research was conducted.
Consent to Participate
The participants registered in the study and completed online the participation consent, information about the study, the data processing, and the questionnaires. The continuation of the study depended exclusively on the agreement offered at this stage.
Consent for Publication
All authors had final approval of the submitted versions.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Comșa, L.T., David, O.A. & David, D.O. Relevant Psychological Factors in Weight Management. How to Think and Behave to Lose Weight and Maintain it for Good. J Rat-Emo Cognitive-Behav Ther 41, 176–192 (2023). https://doi.org/10.1007/s10942-022-00455-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10942-022-00455-1