Abstract
A simple yet promising approach to construct bi-layered scaffolds using bioactive ceramics and biodegradable polymers is presented. This method involves two versatile fabrication techniques used in the field of TE: foam replication process and electrospinning. By the foam replication method, three-dimensional 45S5 bioactive glass (BG)-based scaffolds with high porosity, in the range of 95.8 ± 0.9 %, were produced. To improve the mechanical properties of the BG scaffolds, dip-coating using polycaprolactone (PCL) was performed, which led to a significant increase in the compressive strength of the scaffolds. In order to develop a bi-layered construct, bead-less submicrometric fibers of collagen-PCL were electrospun over the PCL-coated BG scaffolds. Surface morphology, surface properties and mechanical strength of the bi-layered construct were evaluated using scanning electron microscopy analysis, contact angle measurements and compressive strength testing, respectively. In vitro degradation of the collagen-PCL fibers in phosphate buffered saline and in vitro bioactivity of the bi-layered constructs in simulated body fluid were investigated. Formation of hydroxyapatite on the PCL-coated BG and along the morphology of the collagen-PCL fibers was ascertained using different characterization techniques. The bi-layered construct is intended for interface tissue engineering applications where the PCL-coated BG scaffold, which is highly bioactive, can serve as a support for the bone side and the composite collagen-PCL submicrometric fibers are intended for the cartilage side.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Osteochondral defects, i.e. diseases and injuries affecting both the articular cartilage and the subchondral bone, are very widespread. Trauma, tumor or osteoarthritis (OA) are the main reasons for the damage of the articular cartilage [1]. Conventional therapies such as drilling and debriding, autologous cartilage transplantation and implantation may fail at long-term outcomes [1].
In the past two decades, TE has emerged as a promising alternative treatment for OA and other osteochondral defects [2]. Osteochondral TE combines the regeneration of the articular cartilage and the subchondral bone and requires the understanding of the bone and cartilage structure, composition and function. Bone is a composite structure consisting of collagen type I and HA (nano)crystals. The main function of bone is to provide structural support for the body [3]. Cartilage is a highly specialized connective tissue usually present between bone surfaces which aids in smooth sliding of bones, providing a wear resistant surface being capable of sustaining high loading [4]. The extracellular matrix (ECM) of the cartilage is mainly comprised of water, collagen type II and proteoglycans [5]. A variety of scaffold designs, fabrication methods and biomaterial-based strategies have been proposed for osteochondral TE [6–8]. The development of scaffolds for the osteochondral interface requires mimicking the native ECM, independently for cartilaginous and bony tissues, and for this purpose layered scaffolds are favorable as the structural and mechanical properties for each layer can be tailored. Layered constructs are more challenging and difficult to design but they provide the most appropriate functionalities essential for osteochondral TE [9–11]. Accordingly, biomaterials and fabrication methods must be specifically chosen for the bone and cartilage sides.
45S5 BG (Bioglass®) was discovered by Hench in 1969 and was the first artificial material shown to be able to bond to living tissues [12]. The composition of 45S5 BG (in wt%) is 45 % SiO2, 24.5 % Na2O, 24.5 %CaO, 6 % P2O5 and the main advantage of this material is that it is highly surface reactive, building a HA layer on its surface when in contact with physiological fluid and therefore, it is classified as a Class A bioactive material [12].
Collagen is a natural polymer which has 29 known types and functions as the basic building material present ubiquitously in almost every tissue with outstanding mechanical properties. Collagen also plays a significant role in maintaining the biological and structural integrity of the tissues [13]. Mature articular cartilage comprises two-thirds by dry weight of collagens, 15–30 % proteoglycans, chondrocytes and other minor proteins [14]. PCL is a biodegradable and biocompatible synthetic polymer which is widely used in TE [15]. It is one of the few polymers which is miscible with most other polymers and this attribute makes it attractive to blend with natural proteins in order to obtain natural/synthetic polymeric composites and blends which offer suitable mechanical, degradation and surface properties [15].
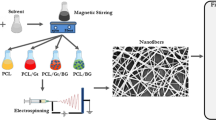
The fabrication of bi-layered scaffolds involves the application of a series of techniques such as polymer foam replication, dip-coating and electrospinning. Foam replication technique is a cost-effective, rapid method to produce highly porous inorganic scaffolds with adjustable pore dimensions and of any desired shape in accordance with the bone defect [16]. Dip-coating process serves as a suitable technique to improve the mechanical properties of bioactive glass or ceramic scaffolds by coating with a polymeric solution [17]. The polymeric coating should help in holding fragmented pieces of a scaffold together in cases of damage [18]. Electrospinning is a versatile and feasible technique for the fabrication of nanofibrous scaffolds for biomedical and tissue engineering applications with mechanical properties and physical dimensions similar to the ECM of the natural tissues [19, 20]. To build bi-layered constructs, in this study, composite nanofibers of PCL and collagen were electrospun, directly over PCL-coated 45S5 BG scaffolds for the first time following an approach introduced by Yunos et al. [11] for PDLLA fibers. Morphological, chemical and mechanical properties of the PCL-coated 45S5 BG scaffolds and the collagen-PCL nanofibers were evaluated.
2 Materials and methods
2.1 Materials
Melt-derived BG powder of 45S5 composition with a particle size of 2 µm (Schott AG, Mainz, Germany) and polyvinylalcohol (PVA) (Merck Schuchardt OHG, Hohenbrunn, Germany) were used for scaffold fabrication. Fully reticulated polyurethane (PU) foams with 45 ppi (pores per inch) (Eurofoam Deutschland GmbH, Wiesbaden, Germany) acted as temporary templates for the final scaffolds made by foam replica method [16]. The PU templates were cut with a punch to cylindrical shape with a diameter of 12 mm. In the dip-coating process, PCL (Sigma-Aldrich, St. Louis, USA) (Mn 80.000) was dissolved in chloroform (Merck KGaA, Darmstadt, Germany). The electrospinning solution was prepared by dissolving collagen type I from calf skin (Sigma-Aldrich, St. Louis, USA) and PCL (1:1) in 1,1,1,3,3,3–Hexafluoro-2-propanol (HFP) (Carl Roth GmbH, Karlsruhe, Germany). The degradation study was carried out in PBS (Sigma-Aldrich, St. Louis, USA).
2.2 Fabrication of 45S5 bioactive glass scaffolds
The BG scaffolds were fabricated by the foam replica method introduced in 2006 [16]. In this method, a slurry was prepared by mixing BG powder with PVA and deionized water. PVA acts as binder to control the viscosity of the slurry and to promote the adhesion of the glass particles to the PU foam. The PU foams were dipped into the slurry and squeezed manually to remove the excess slurry to avoid blocking of the pores during the sintering process. The green bodies were dried at room temperature overnight and were, later, put into the furnace. For densification of the 45S5 BG scaffolds, the green bodies were sintered at 1000 °C. During the sintering process, the PU templates were burned out and the BG powder densified. The temperature profile of the sintering process involves heating up to 450 °C for 1 h at a rate of 2 °C/min and then to the sintering temperature (1000 °C) at a rate of 2 °C/min, before cooling down to room temperature at a rate of 5 °C/min [16].
2.3 Dip-coating of 45S5 bioactive glass scaffolds
Dip-coating is a simple method used to coat bioactive glass scaffolds with biodegradable polymers to improve their mechanical properties [21]. This process involves dipping of the scaffolds for several times in a polymer solution and drying them at room temperature. In the present study, dip-coating was executed on the 45S5 BG scaffolds by dipping them three times into PCL solution. Polymeric solutions with 2.5 and 5 wt/v% of PCL in chloroform were prepared and the scaffolds were manually immersed into the PCL solutions. Different time periods such as 45 s, 1, 2.5 and 5 min were tried and the scaffolds were dipped three times for each time period. The drying time between each dipping was 2 h. Based on the porosity and mechanical strength, the best performing PCL-coated 45S5 BG scaffolds among this group were selected and taken for further investigations.
2.4 Electrospinning
The scaffold layer for the cartilage side was fabricated by electrospinning using a laboratory device (Type BI-HVG-P60R-EM, Linari Engineering S.r.l, Valpiana, Italy). A 1:1 collagen-PCL solution was prepared by dissolving PCL and collagen in HFP. Initially, 8, 6 and 4 wt/v% of polymer solutions (1:1 ratio of PCL/collagen) were prepared. The first two solutions were concentrated and too viscous. The solution with 4 wt/v% had an appropriate viscosity to be electrospun. The PCL/collagen solution was filled in a glass syringe with a metal needle of 0.8 mm diameter. For obtaining a constant polymer flow rate, a syringe pump (BSP-99M, Braintee Scientific Inc., Braintee, US), was used during the experiments. The syringe was connected to a high voltage source. The voltage was set to 16 kV and the flow rate was maintained at 0.8 ml/h. The grounded collector was wrapped in aluminum foil, and it was positioned at a distance of 12–13 cm from the needle. The collagen-PCL fibers were collected on the aluminum foil and these fibers were taken for further characterization and degradation studies.
2.5 Development of bi-layered constructs
In this step, the PCL-coated 45S5 BG scaffolds were positioned on the aluminum foil using circular double sided tapes. PCL/collagen nanofibers were collected on the top surface of the PCL-coated scaffolds. Scissor and a sharp razorblade were used to cut the fibers around the scaffolds and to remove them from the aluminum foil.
2.6 Porosity measurements and optical microscopy
After the dip-coating process, the porosity of the PCL-coated scaffolds was calculated. For this purpose, the surface and cross sections of the PCL-coated scaffolds were investigated using an optical microscope (M50, Leica Microsystems GmbH, Wetzlar, Germany). The porosity of the sintered scaffolds was determined by using the two formulas mentioned below. The porosity (P foam ) of the uncoated scaffolds and the porosity of the polymer coated scaffolds (P coated foam ) were calculated via Eqs. (1) and (2), respectively [21].
where W foam and W coated foam are the masses of the uncoated 45S5 BG scaffold and PCL coated scaffold respectively (determined by measuring the weights); ρ BG is the theoretical density of the scaffold material (assuming the value of amorphous 45S5 BG: 2.7 g/cm3) and ρ polymer is the density of solid PCL (1.145 g/cm3); V foam and V coated foam are the volumes of the uncoated scaffold and the PCL coated scaffold, respectively. For this calculation, three scaffolds for each immersing time and PCL composition were weighed before and after dipping using an electronic analytical balance. The size of the scaffolds was measured with a caliper before and after dip-coating.
2.7 Characterization studies—morphology, structural analysis and surface/wetting properties
2.7.1 Surface morphology
To analyze the surface morphology of the samples, images were made by a scanning electron microscope (SEM) (Quanta 200, FEI Company, Hilsboro, US) at different magnifications. Samples were fixed on stubs using double sided carbon stickers. Silver paint was used as an additional adhesive and to improve conductivity. Finally, the samples were sputter coated with gold and then observed under SEM.
2.7.2 Structural analysis
Fourier-transform infrared (FTIR) spectroscopy (Q5000, TA Instruments) was used in order to identify the chemical composition of the scaffolds and the fibers. Electrospun collagen-PCL fiber meshes were analyzed using the attenuated total reflectance (ATR) method. Infrared spectra were obtained over a wavenumber range between 4000 and 525 cm−1 at 4 cm−1 resolution. To investigate uncoated and PCL coated scaffolds, they were pressed to pellets of 13 mm diameter.
2.7.3 Surface/wetting properties of the collagen-PCL fibers
The wettability of a material surface can be analyzed by measuring the contact angle [22]. In this investigation, the contact angle measurement is necessary to assess the water affinity of the nonwoven PCL/collagen fiber meshes. The measurement was carried out using the sessile drop technique by a video contact angle device (DSA30, Krüss). After adjusting the base drop line, deionized water (3 µl) was dropped on the surface of the PCL/collagen nanofibers. The contact angle was measured five times for each sample and the average angle was calculated subsequently.
2.8 Mechanical testing
PCL coated 45S5 BG scaffolds were tested to determine their compressive strength using a Zwick Roell Z050 mechanical tester with a 50 N load cell at a crosshead speed of 1 mm/min at room temperature. The scaffolds were positioned between two parallel plates. The cross-sectional area was calculated and a typical stress–strain curve was obtained. Three scaffolds from each group were tested and uncoated 45S5 BG scaffolds were also tested for comparison.
The tensile strength of the collagen-PCL fibrous meshes was tested and for this purpose, the meshes were cut into rectangular strips (4 cm × 0.5 cm). The thickness of the meshes was measured by a digital gauge and the rectangular mesh strips were clamped into the grips of the mechanical tester (Frank, control system obtained from Zwick/Roell). The strips were stretched (v = 5 mm/min) until fracture using a 500 N load cell. The test was performed at room temperature. Tensile strength σ m and Young’s modulus E of the PCL/collagen meshes were calculated.
2.9 In vitro degradation and bioactivity studies
2.9.1 In vitro degradation in PBS
The in vitro degradation of the collagen-PCL scaffolds was assessed in PBS solution at 37 °C over a period of 21 days. For this study, the collagen-PCL fibrous mesh was cut using a punch into circular shapes of 8 mm diameter. The samples were placed in a 24 well plate at room temperature. 1 ml of PBS was added to each sample in the well plate and the PBS was changed every second day. The aim of this part of the study was to detect the presence of collagen in the fibers after degradation, without the formation of any new phases. Thus PBS was used in this study (and not SBF as immersion in SBF could lead to precipitation of mineral phases).
2.9.2 In vitro bioactivity study
In order to know the influence of PCL-coating on the bioactivity of the 45S5 BG scaffolds, a standard in vitro procedure in SBF was carried out. SBF solution was prepared as described by Kokubo et al. [23]. The bi-layered constructs were immersed in 50 mL of SBF and kept in a shaking incubator at 90 rpm (KS 4000 I control, IKA, Germany) and 37 °C. The pH of the solution was maintained at 7.4 and the solution was replaced twice a week. Samples were collected from the incubator after 7, 14 and 21 days, rinsed in deionized water, dried at room temperature and taken for further characterization such as SEM and FTIR. X-ray diffraction (XRD) analysis of the bi-layered constructs was performed using an X-ray diffractometer (D8 ADVANCE, Brucker, Madison, US) equipped with a VÅNTEC-1 detector. Data were recorded in the range of 2θ = 20°–50° using a step size of 0.0014° and Cu Kα radiation (λ = 0.15406 nm).
3 Results
3.1 Dip-coating—porosity
The porosities were calculated by Eqs. (1) and (2). Table 1 summarizes the results of the porosity measurement for the 45S5 BG scaffolds which were dipped in the solutions of 2.5 and 5 wt/v% of PCL for 45 s, 1 min, 2.5 and 5 min. All scaffolds were dipped three times at an interval of 2 h.
As expected, 45S5 BG scaffolds dip-coated with 2.5 wt/v% PCL solution exhibit higher porosity than the group which was coated with 5 wt/v% PCL solution. This is because the solution with 5 wt/v% of PCL was more viscous. However, when cross sections were made, it was obvious that the scaffolds coated with 2.5 wt/v% of PCL remained brittle inside and they broke easily as they had a rigid outer surface covered with PCL but a brittle inner region. There were no significant differences in the porosity values with respect to the dipping time. There is a tendency to achieve higher porosity when the scaffolds were immersed into the PCL solution for 5 min. In the cases where scaffolds were immersed for less than 5 min, the polymer solution just covered the surface of the struts and partially blocked the pores. Considering the above two factors, the 45S5 BG scaffolds which were dip-coated in 5 wt/v% of PCL solution for 5 min provided the right balance between porosity and structural robustness. In these scaffolds, the weight percentage of PCL present in the coated scaffolds was calculated as 17 % on average. The mechanical strength of all the groups of PCL-coated 45S5 BG scaffolds was determined and the values were also considered to choose the best group for developing the bi-layered constructs. The compression strength results are discussed in Sect. 3.4.
3.2 Scaffold morphology
Figure 1a shows the cross-section of the 45S5 Bioglass® scaffolds dip-coated with 5 wt/v% PCL solution. The open pore structure was maintained in the 5 wt/v% PCL-coated scaffolds as can be seen from the SEM image. The microstructure shown in Fig. 1a is typical for this type of BG based scaffolds fabricated by the form replica method, which usually features surface defects such as microcracks as well as a remaining central hole inside the struts, which is the result of the burning out of the sacrificial PU foam [16]. Clearly, such highly porous and microcracked structure will exhibit very low mechanical strength which is the main reason why polymer coatings are considered [17, 21], as discussed also further below. Figure 1b shows the polymeric coating on a single scaffold strut at a higher magnification and the black arrow indicates the PCL coating. It can be observed that the outer corner of the strut is not covered with the PCL coating. Visual inspection indicates that the PCL coating was not homogeneous which is not considered a drawback in principle, as an inhomogeneous polymer coating will enable some areas of the BG struts to be in direct contact with the biological medium, which is required to exploit the bioactivity of the bioactive glass surface [24].
SEM micrographs of a cross-section of 45S5 bioactive glass scaffold dip-coated with 5 wt/v% PCL solution, b PCL coating on a single BG strut at a higher magnification, c electrospun collagen-PCL fibers, d, e a single PCL-coated scaffold strut with nanofibers of collagen-PCL after electrospinning for 10 and 80 min, respectively
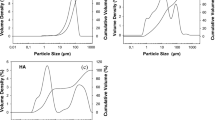
Beadless nonwoven collagen-PCL meshes were obtained with fibers in the nanoscale or submicrometric range. Figure 1c shows the SEM images of electrospun collagen-PCL nanofibers. The diameter of ten randomly chosen fibers from eight SEM pictures was measured with the program ImageJ (National Institute of Health, USA). Fibers with the minimal diameter of 119 nm and the maximal diameter of 651 nm were detected. The average fiber diameter was calculated to be 405 nm.
Figure 1d, e illustrate the collagen-PCL nanofibers on top of PCL-coated 45S5 BG scaffold after 10 and 80 min of electrospinning, respectively. In Fig. 1d, a single scaffold strut can be seen with collagen-PCL nanofibers on it. A thicker mesh of collagen-PCL nanofibers, PCL-coating and a single strut of the PCL-coated scaffold can be seen in Fig. 1e. The thickness of the PCL/collagen mesh deposited for 80 min was obtained from SEM observation and it was estimated to be 3.5 µm (Fig. 1e).
3.3 Surface properties
For contact angle measurement, a drop of deionized water was set on the collagen-PCL nanofibrous mesh surface. Within a minute, the drop was completely absorbed by the fibers. Five measurements were made and the average contact angle was calculated to be 31.7° ± 0.9°. This value indicates that the fibers are highly hydrophilic [25]. In comparison with the contact angle of single PCL fibers which is about 103° [26], collagen, as expected, improved significantly the surface wettability of the collagen-PCL nanofibers. Collagen nanofibers have been reported to be highly hydrophilic with a contact angle of around 30° [27].
3.4 Mechanical properties
The results of the compressive strength testing of PCL dip-coated 45S5 BG scaffolds are summarized in Table 2.
The scaffolds dip-coated with 5 wt/v% of PCL solution possessed a higher compressive strength than the other tested samples.
After considering the results of porosity measurements and mechanical testing, scaffolds which were dip-coated with 5 wt/v% PCL solution for 5 min were chosen for further characterization. This scaffold system combines high porosity (79 ± 1 %) and suitable mechanical properties (σ = 0.24 ± 0.06 MPa). The stress–strain curves of scaffolds dip-coated with 5 wt/v % PCL solution (not shown here) exhibited less jagging than the curves of the uncoated and 2.5 wt/v% PCL dip-coated scaffolds. The improvement of the mechanical properties of bioactive glass scaffolds by application of a polymer coating has been reported by several researchers [10, 21, 28, 29]. For example, Chen et al. [21] asserted an enormous improvement in the mechanical properties of PDLLA coated 45S5 BG-based scaffolds in comparison to uncoated scaffolds. It was hypothesized that PDLLA filled the micropores and microcracks on the struts improving the mechanical properties [21]. PCL is likely to improve the mechanical properties of the present 45S5 BG scaffolds in the similar way and specific strengthening and toughening mechanism acting in this type of polymer coated scaffolds have been discussed recently [28].
The tensile strength of the collagen-PCL fibrous meshes with various thicknesses was measured and the average tensile strength was found to be 2.5 ± 0.1 MPa; the calculated Young’s modulus is 23 ± 10 MPa. Meshes with higher thickness provide higher values of tensile strength than thin meshes, which is likely due to the fact that more fibers are oriented along the elongation direction than in thin meshes. Therefore, more fibers are stretched in the elongation direction contributing to the tensile strength.
3.5 In vitro degradation of electrospun collagen-PCL fibers
The electrospun fibers of collagen-PCL were evaluated using SEM and FTIR after the in vitro degradation in PBS for 21 days. Figure 2a, b show SEM images of electrospun collagen-PCL nanofibers before and after degradation in PBS and an obvious difference can be seen between both images. Directly after electrospinning, the collagen-PCL fibers possess a defined shape with diameters in the submicrometric range. In contrast, after 21 days of immersion in PBS, the fibers are swollen and they do not have a defined structure. In our collagen-PCL electrospun mesh, collagen contributes to 50 % of the composite and comparing the degradation time of PCL, collagen, as a natural polymer, degrades faster [30]. This might be the reason for the difference in the structure of the collagen-PCL fibers after degradation.
In order to confirm the presence of collagen in the electrospun fibrous mesh after 21 days in PBS, ATR-FTIR measurements were done. Figure 3 illustrates the ATR-FTIR results of collagen-PCL fibers before and after degradation in PBS for different periods. It can be observed that the characteristic bands of both collagen and PCL were present in the spectra. All functional groups which were detected in the sample before degradation were also found after the degradation study.
Table 3 summarizes all detected bands in the spectrum of PCL/collagen fibers, indicating also the positions of the bands (from the literature) which are given for comparison purposes. The characteristic bands at 2944 and 1725 cm−1 refer to C–H and C=O groups in PCL, respectively. Further typical bands of amide I, amide II and amide III were detected representing the triple helical structure of collagen. All bands which correspond to PCL and collagen were found in the FTIR spectra, confirming the collagen-PCL content of the fibers. Values from the literature are also given for comparison purpose [31, 32].
3.6 In vitro bioactivity study
The bi-layered constructs were analyzed using SEM, FTIR and XRD after the in vitro bioactivity study in SBF for 21 days. The electrospun fibrous mesh was removed from the bi-layered construct after the SBF study and the side which was in contact with the PCL-coated 45S5 BG scaffold was investigated under SEM. Figure 5a, b show SEM images of the PCL-coated scaffolds and the collagen-PCL mesh, respectively, after 21 days of immersion in SBF. Interestingly, the formation of crystalline HA occurred on both layers of the bi-layered construct. The globular, cauliflower shape typical for HA [21] can be observed in the SEM images. Figure 4a indicates that the PCL coating does not affect the bioactivity of the BG scaffolds. It can be seen from Fig. 4b that HA crystals are homogenously growing on the lower side of the fibrous mesh, following the dimensions and morphology of the collagen-PCL fibers. Energy dispersive X-ray spectroscopy (EDX) analysis was used to ascertain the presence of HA on the collagen-PCL mesh as shown in Fig. 4c. Ca and P elements were detected in the spectrum confirming apatite formation [33].
Figure 5 shows the FTIR spectra of the bi-layered constructs after immersion in SBF for 7, 14 and 21 days in comparison with the spectrum of scaffolds which were not immersed in SBF. The HA formation is confirmed by the appearance of bands at ~567, 600 and 1017–1090 cm−1 corresponding to the bending and stretching vibration of phosphate groups (PO4 3−), respectively. The band at 878 cm−1 corresponds to the vibration mode of carbonate groups (CO3 2−) and suggests the formation of carbonated HA [34].
XRD measurements of the bi-layered constructs after immersion in SBF were taken only for day 7 and day 21. Figure 6 shows the XRD spectra of the bi-layered scaffolds (PCL-coated 45S5 BG with electrospun collagen-PCL fibers on top) after an immersion time of 7 and 21 days in SBF, respectively.
In the obtained spectra of PCL dip-coated BG/PCL/collagen scaffolds, the typical HA peaks appear at 26°, at 31° and at 43° for samples immersed for 7 days in SBF. This result is in correlation with values found in the literature [35, 36]. All peaks referring to HA crystals are marked with black arrows in Fig. 6. There is an increase in the intensity of the peaks between 7 and 21 days of immersion suggesting that more HA was formed after 21 days. The bioactivity of the PCL-coated 45S5 BG scaffolds was maintained, as confirmed by the presence of HA peaks on the XRD patterns.
4 Discussion
4.1 General aspects
Driven by increasing demand, osteochondral defects require novel strategies for the regeneration of the damaged osteochondral region. Osteochondral TE opens up the possibility of engineering scaffold constructs and combining them with functional cells and signaling molecules to regenerate the osteochondral region. Bi-layered structures satisfy the conditions to engineer the osteochondral region and they require the right combination of manufacturing techniques and biomaterials to reproduce the structure of the articular cartilage/subchondral bone interface.
In this investigation, the polymer (PU) foam replication technique was chosen to fabricate the scaffolds for the bone section of the construct. This technique has numerous advantages over other conventional techniques such as the ability to produce highly porous scaffolds with adjustable pore dimensions, ability to tailor the size and shape of the scaffolds according to the requirement of the bone defect, being cost-effective and not involving the use of toxic chemicals [16]. Scaffolds obtained from foam replication technique exhibit a pore structure that resembles that of the trabecular bone which is an added advantage of the method. Scaffolds made from 45S5 BG using this technique have shown connective, open pore structure with a porosity of ~95 % and pore size in the range of 400–700 µm [16]. On the other hand, bioactive glass is brittle and therefore unsuitable for load-bearing applications in bone tissue engineering [12]. In order to improve the mechanical integrity of the highly porous scaffolds, the application of polymeric coatings has been suggested [21]. Several synthetic (PDLLA, PHB) and natural (gelatin, alginate) polymers have been used to coat the brittle 45S5 BG scaffolds to improve their mechanical properties [29]. Hum et al. [37] investigated recently different biopolymeric coatings such as collagen, gelatin, PCL, alginate and PLLA over 45S5 BG scaffolds. According to their findings, PCL-coating increased the scaffold stiffness by 58 % in comparison with uncoated scaffolds and therefore, PCL was considered a promising polymer for enhancement of the mechanical competence of 45S5 BG scaffolds in this study. Also, it was confirmed that PCL coating did not clog the micropores which is essential for efficient cell seeding of scaffolds and bone tissue in-growth. Following this information, the 45S5 BG-based scaffolds in this study were coated with 5 wt/v% PCL solution for 5 min and the coating process was repeated three times at an interval of 2 h. The porosity of the PCL-coated scaffolds was high (~80 %) and the compressive strength was 0.24 ± 0.06 MPa which is a notable improvement in comparison with the value of the uncoated scaffolds (0.01 MPa). It should also be noted that the PCL-coated BG scaffolds behaved in a “flexible foam-like” manner compared to the brittle nature of the as-sintered (un-coated) 45S5 BG scaffolds, thereby reducing handling difficulties [10]. In fact the coated scaffolds were qualitatively robust and they could be safely handled during all the processing steps of this study. Further aspects of the “toughening effect” imparted by a polymer coating to highly porous, brittle scaffolds, have been discussed in a recent review article [38]. In addition, and based on results on similar PDLLA coated BG scaffolds [21], it can be anticipated that the compressive strength of the PCL-coated scaffolds will not significantly decrease even after immersion in SBF, due to the formation of a HA/PCL nanocomposite film on the strut surface, as suggested in the literature [21]. The compressive strength of spongy bone is in the range of 0.2–4.0 MPa [39]. Thus the chosen system (45S5 BG scaffolds dip-coated with 5 wt/v% PCL solution) falls in this range and therefore, it is suitable to be used as scaffold for the bone side for applications in osteochondral TE.
In order to fabricate the cartilage side of the bilayered construct, electrospinning technique was used. Electrospinning refers to the technique of drawing very fine fibers on a nanoscale or submicrometric range by applying high electric potential and this method is applicable to a wide range of polymers [40]. Fibers in the nanoscale and submicrometric ranges offer a much larger scope for tissue engineering and biological applications than conventional (micrometric sized) fibers [41]. Electrospun nanofibrous matrices show morphological similarities to the natural extracellular matrix and they are characterized by high surface to volume ratio, high porosity and variable pore size distribution exhibiting properties that can modulate the cellular behavior [20]. Several biopolymers have been electrospun to produce nanofibrous scaffolds for cartilage tissue engineering [42–44]. For example, Casper et al. [45] produced PCL nanofibers through electrospinning with or without chitosan coating and implanted them in 6-month old rabbits. Cell infiltration was observed in all scaffolds and the uncoated PCL nanofibrous scaffolds showed higher levels of sulfated glycosaminoglycan and cartilage yield. The study demonstrated that it is possible to seed PCL nanofibrous scaffolds with periosteal cells in vivo to produce engineered cartilage in vitro [45]. In the present investigation, we electrospun collagen-PCL mixtures to obtain nanofibrous meshes for the cartilage region of the OC construct. Beadless, non-woven fibers of size in the range of 400–600 nm were processed (Fig. 1c). Degradation studies in PBS indicated major differences in the morphology of the fibers (Fig. 2a, b) which is likely due to the fact that collagen contributes to 50 % of the electrospun nanofibrous composite and, being a natural polymer, it degrades faster than PCL. However, FTIR spectroscopy analysis confirmed the presence of collagen in the nanofibrous composite even after 21 days in PBS (Fig. 3).
4.2 Biomimetics of the osteochondral region—composition, structure and morphology
The application of functionally graded and layered materials in the biomedical field has been considered for a number of years [46] and new concepts are continuously being put forward to improve the performance of implants and scaffolds. In this study, in order to build the osteochondral scaffold, bioinspired design was followed which resulted in a bi-layered construct mimicking the osteochondral region comprising a highly bioactive, porous bone side and a collagen-containing fibrillar cartilage section.
Interestingly, electrospinning a thin layer of collagen-PCL nanofibers over the PCL-coated 45S5 BG scaffolds resulted to some extent in fiber alignment. The collagen-PCL nanofibers were stretched and aligned in between the struts of the underlying scaffold as observed in SEM images (Fig. 7a, b). The construct appears to be highly porous with channel-like pores in between the nanofibers. This structure resembled the superficial zone (top zone) of the packed and aligned parallel with collagen fibrils densely packed and aligned parallel to the articular surface. Chondrocytes in this zone should also align parallel, being flattened and elongated [47].
With increasing deposition time, the alignment in the collagen-PCL nanofibers is lost. However, a densely packed collagen-PCL nanofibrous mesh with high content of collagen (50 %) is obtained over the PCL-coated 45S5 BG scaffolds. The most important advantage of 45S5 bioactive glass, making it a promising material for bone scaffold fabrication, is the ability of its surface to react readily with the surrounding biological medium. It is well known that 45S5 BG exhibits high bioactivity (Class A biomaterial) and it is both osteoconductive and osteogenic [12]. Following the in vitro studies of the present bi-layered construct in SBF for 21 days, it was found that the PCL coating does not interfere with the formation of hydroxyapatite on the scaffold surfaces and therefore, the bioactivity of the 45S5 BG scaffolds is not compromised by the presence of the coating. This may be due to the fact that PCL coating was not completely homogeneous leaving parts of the strut surfaces directly exposed to SBF. It was also noticed that the lower side of the collagen-PCL nanofibrous mesh, which was in contact with the PCL-coated 45S5 BG surfaces, was highly mineralized and the formation of hydroxyapatite crystals was confirmed (Fig. 4b) along the nanofibrous morphology. This structure is very similar to the native calcified cartilage zone where endochondral ossification occurs and the cartilage is mineralized with calcium phosphate [48]. When complete mineralization occurs, chondrocytes undergo apoptosis, blood vessels invade this zone and new bone is laid down by osteoblasts [48].
A variety of biomaterials such as bioactive glasses and biopolymers such as PDLLA, PCL, collagen, chitosan, gelatin and alginate combined with several processing techniques such as foam replica method, freeze drying and electrospinning have been used to develop layered constructs for interface tissue engineering [8, 10, 11, 49–51]. Taking cues from these previous works, we successfully fabricated for the first time a bi-layered structure consisting of a trabecular-bone shaped scaffold made of 45S5 BG and a collagen-containing fibrous mesh resembling the articular cartilage. The presence of collagen in the structure and also the formation of hydroxyapatite due to the reactivity of the BG will stimulate a physiologically relevant environment for the cells to adhere and proliferate, and therefore the scaffolds developed in this study constitute a promising alternative for osteochondral TE applications. As a future perspective, it is necessary to investigate the interfacial strength and possible delamination of the electrospun fibers from the porous 45S5 BG scaffold. Also, cell biology studies will provide understanding of the cell growth, differentiation and migration on the bi-layered constructs.
5 Conclusions
In summary, a bioinspired bi-layered scaffold using bioactive 45S5 BG and biodegradable fibrous layers of collagen-PCL has been developed. Foam replication technique produced highly porous, dense 45S5 BG-based scaffolds similar to the spongy bone structure. Dip-coating by PCL significantly enhanced the mechanical competence of the scaffolds. Electrospinning was used to build a layer of submicrometric collagen-PCL fibrous mesh over the BG scaffolds. Thin layers of electrospun collagen-PCL meshes over the 45S5 BG scaffolds showed alignment of the fibers in between the struts which is hypothesized to be advantageous for the flattening, elongation and attachment of chondrocytes. Results from in vitro SBF studies of the bi-layered constructs showed that the bioactivity of the 45S5 BG-based scaffolds is not affected by the presence of the PCL coating. Mineralization occurred in the fibrous composite’s surface which is in contact with the PCL-coated scaffold. Hydroxyapatite crystals were found, which have grown along the surface of the collagen-PCL fibers. From these findings, we can conclude that the developed bi-layered construct has the ability to mimic the native tissue region and has the potential to be used for osteochondral TE.
References
N.J. Castro, S.A. Hacking, L.G. Zhang, Ann. Biomed. Eng. 40, 1628 (2012)
R. Langer, J.P. Vacanti, Science 260, 920 (1993)
D.W. Sommerfeldt, C.T. Rubin, Eur. Spine J. 10(Suppl 2), S86 (2001)
J.M. Mansour, in Kinesiology: the mechanics and pathomechanics of human movement, ed. By C. A. Oatis (Lippincott Williams and Wilkins, Philadelphia, 2003), p. 66
B. Scopp, J. Mandelbaum, Orthop. Sport. Med. Board Rev. Man. 2, 1 (2005)
S.P. Nukavarapu, D.L. Dorcemus, Biotechnol. Adv. 31, 706 (2013)
I. Martin, S. Miot, A. Barbero, M. Jakob, D. Wendt, J. Biomech. 40, 750 (2007)
P. Nooeaid, V. Salih, J.P. Beier, A.R. Boccaccini, J. Cell Mol. Med. 16, 2247 (2012)
T.J. Levingstone, A. Matsiko, G. Dickson, F.J. O’Brien, J.P. Gleeson, Acta Biomater. 10, 1996 (2014)
L. Liverani, J.A. Roether, P. Nooeaid, M. Trombetta, D.W. Schubert, A.R. Boccaccini, Mater. Sci. Eng. A 557, 54 (2012)
D.M. Yunos, Z. Ahmad, V. Salih, A.R. Boccaccini, J. Biomater. Appl. 27, 537 (2013)
L.L. Hench, J. Mater. Sci. Mater. Med. 17, 967 (2006)
P. Balasubramanian, M. Prabhakaran, M. Sireesha, S. Ramakrishna, Adv. Polym. Sci. 251, 173 (2013)
F.C. Linn, L. Sokoloff, Arthritis Rheum. 8, 481 (1965)
A. Cipitria, A. Skelton, T.R. Dargaville, P.D. Dalton, D.W. Hutmacher, J. Mater. Chem. 21, 9419 (2011)
Q.Z. Chen, I.D. Thompson, A.R. Boccaccini, Biomaterials 27, 2414 (2006)
D. Mohamad Yunos, O. Bretcanu, A. R. Boccaccini, J. Mater. Sci. 43, 4433 (2008)
S. Dorozhkin, T. Ajaal, Proc. Inst. Mech. Eng. Part H J. Eng. Med. 223, 459 (2009)
W.-E. Teo, W. He, S. Ramakrishna, Biotechnol. J. 1, 918 (2006)
Q.P. Pham, U. Sharma, A.G. Mikos, Tissue Eng. 12, 1197 (2006)
Q.Z. Chen, A.R. Boccaccini, J. Biomed. Mater. Res. A 77, 445 (2006)
K.L. Menzies, L. Jones, Optom. Vis. Sci. 87, 387 (2010)
T. Kokubo, H. Takadama, Biomaterials 27, 2907 (2006)
O. Bretcanu, S. Misra, I. Roy, C. Renghini, F. Fiori, A.R. Boccaccini, V. Salih, J. Tissue Eng. Regen. Med. 3, 139 (2009)
F. Tan, M. Naciri, M. Al-Rubeai, Biotechnol. Bioeng. 108, 454 (2011)
M.A. Alvarez-Perez, V. Guarino, V. Cirillo, L. Ambrosio, Biomacromolecules 11, 2238 (2010)
R. Ravichandran, J.R. Venugopal, S. Sundarrajan, S. Mukherjee, S. Ramakrishna, World J. Cardiol. 5, 28 (2013)
P. Nooeaid, J.A. Roether, E. Weber, D.W. Schubert, A.R. Boccaccini, Adv. Eng. Mater. 16, 319 (2014)
O. Bretcanu, A.R. Boccaccini, V. Salih, J. Mater. Sci. 47, 5661 (2012)
J.M. Hackett, T.T. Dang, E.C. Tsai, X. Cao, Materials (Basel). 3, 3714 (2010)
J. Venugopal, Y.Z. Zhang, S. Ramakrishna, Nanotechnology 16, 2138 (2005)
A.K. Bassi, J.E. Gough, M. Zakikhani, S. Downes, J. Tissue Eng. 2011, 1 (2011)
D.M. Yunos, Z. Ahmad, A.R. Boccaccini, J. Chem. Technol. Biotechnol. 85, 768 (2009)
M. Bil, J. Ryszkowska, J.A. Roether, O. Bretcanu, A.R. Boccaccini, Biomed. Mater. 2, 93 (2007)
J. Huang, L. Di Silvio, M. Wang, I. Rehman, C. Ohtsuki, W. Bonfield, J. Mater. Sci. Mater. Med. 8, 809 (1997)
J. Roether, A. Boccaccini, L. Hench, V. Maquet, S. Gautier, R. Jérôme, Biomaterials 23, 3871 (2002)
J. Hum, K.W. Luczynski, P. Nooeaid, P. Newby, O. Lahayne, C. Hellmich, A.R. Boccaccini, Strain 49, 431 (2013)
A. Philippart, A.R. Boccaccini, C. Fleck, D.W. Schubert, J.A. Roether, Expert Rev. Med. Devices 12, 93 (2015)
M.P. Wolcott, Mater. Sci. Eng. A 123, 282 (1990)
T. Subbiah, G.S. Bhat, R.W. Tock, S. Parameswaran, S.S. Ramkumar, J. Appl. Polym. Sci. 96, 557 (2005)
S. Ramakrishna, K. Fujihara, W.-E. Teo, T.-C. Lim, Z. Ma, In An Introduction to Electrospinning and Nanofibers (World Scientific, Singapore, 2005), p. 382
J.M. Coburn, M. Gibson, S. Monagle, Z. Patterson, J.H. Elisseeff, Proc. Natl. Acad. Sci. 109, 10012 (2012)
N.W. Garrigues, D. Little, J. Sanchez-Adams, D.S. Ruch, F. Guilak, J. Biomed. Mater. Res. A 59784, 28 (2013)
A. Thorvaldsson, H. Stenhamre, P. Gatenholm, P. Walkenström, Biomacromolecules 9, 1044 (2008)
M.E. Casper, J.S. Fitzsimmons, J.J. Stone, A.O. Meza, Y. Huang, T.J. Ruesink, S.W. O’Driscoll, G.G. Reinholz, Osteoarthritis Cartilage 18, 981 (2010)
W. Pompe, H. Worch, M. Epple, W. Friess, M. Gelinsky, P. Greil, U. Hempel, D. Scharnweber, K. Schulte, Mater. Sci. Eng. A 362, 40 (2003)
B.L. Schumacher, J.A. Block, T.M. Schmid, M.B. Aydelotte, K.E. Kuettner, Arch. Biochem. Biophys. 311, 144 (1994)
H. Mitsuyama, R.M. Healey, R.A. Terkeltaub, R.D. Coutts, D. Amiel, Osteoarthr. Cartil. 15, 559 (2007)
Q. Yao, P. Nooeaid, R. Detsch, J.A. Roether, Y. Dong, O.-M. Goudouri, D.W. Schubert, A.R. Boccaccini, J. Biomed. Mater. Res. A. 102, 4510 (2014)
P. Gentile, V. Chiono, C. Tonda-Turo, C. Mattu, F. Baino, C. Vitale-Brovarone, G. Clardelli, Mater. Lett. 89, 74 (2012)
P. Gentile, M. Mattioli-Belmonte, V. Chiono, C. Ferretti, F. Baino, C. Tonda-Turo, C. Vitale-Brovarone, I. Pashkuleva, R.L. Reis, G. Ciardelli, J. Biomed. Mater. Res. A 100, 2654 (2012)
Acknowledgments
The authors would like to acknowledge the European Commission funding under the 7th Framework Programme (Marie Curie Initial Training Networks; Grant Number: 289958, Bioceramics for bone repair). The authors thank Dr. Patcharakamon Nooeaid, Ms Yaping Ding, Mr Wei Li and Dr Menti Goudouri (Institute of Biomaterials, University of Erlangen-Nuremberg) for experimental support.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balasubramanian, P., Roether, J.A., Schubert, D.W. et al. Bi-layered porous constructs of PCL-coated 45S5 bioactive glass and electrospun collagen-PCL fibers. J Porous Mater 22, 1215–1226 (2015). https://doi.org/10.1007/s10934-015-9998-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10934-015-9998-5