Abstract
The objectives were to develop a population model for placebo-corrected moxifloxacin QT interval in healthy subjects using non-linear mixed effects modeling and to examine effect of covariates on the observed QT. Based on the parameters of interest, optimizations of observation times and number of subjects were proposed. A pool of four thorough QT studies was used, representing 99 subjects receiving placebo and moxifloxacin. The data was modeled using Monolix. The placebo effect on QT was satisfactorily described using a 2-oscillator model. It reflected the circadian rhythm variability which is taken into account when assessing the time-matched mean difference on QT between treatment and baseline. Based on this model, the moxifloxacin effect on QT was satisfactorily described by the same equation with the adjunct of a direct and proportional drug concentration-effect. The Emax model provided the best description of the effect. The unique covariate was gender for both baseline QTc and individual heart rate correction factor. The present design included up to 16 observations for pharmacodynamics. Using this model, 9 observation times for pharmacodynamics provided satisfactory estimates for the parameters of interest (Emax). With 15% precision limit on Emax, 60 subjects was optimal. The simultaneous placebo-moxifloxacin QT model proposed is an interesting alternative to the ICH E14 guideline in assessing QT prolongation effect. This approach provides accurate information over a range of concentrations using different relationships (slope or Emax models) to quantify the drug-response relationship versus placebo. This allowed optimizing the observation times and number of subjects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As detailed in the International Conference on Harmonization (ICH) E14 Guidance for Industry, a clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential of new drugs in development should be conducted [1]. Both a placebo arm and a positive control arm should be included in any “Thorough QT” (TQT) trial in order to validate the results of the study. The placebo group not only allows determination of the effects of spontaneous variability, but it also provides the comparison group by which to determine more accurately the drug effect. The positive control should be an agent that consistently results in an effect at the level of regulatory concern in order to demonstrate study sensitivity to detect such an effect. Therefore, a typical TQT study is comprised of four treatment arms of which placebo and 400 mg of the fluoroquinolone antibiotic moxifloxacin [1, 2]. Standardization of study conditions can also help to minimize the influence of confounding factors. It is crucial that experimental conditions be uniform across all treatment groups to provide assurance that effects observed in both the placebo and positive control arms occurred under the same conditions as for the investigational medicinal product arms. The relationship between drug concentration and QT/QTc effects is routinely assessed during regulatory reviews [3–5]. The moxifloxacin effect on QT was previously satisfactorily described with a direct and proportional concentration effect [6].
The objectives of this study were to develop a population PD model for placebo-corrected moxifloxacin QT interval in healthy subjects using non-linear mixed effects modeling and to examine possible effect of covariates on the observed QT interval such as gender, adult females having been shown to exhibit longer baseline QT/QTc intervals and a greater propensity to develop torsade de pointes (TdP) upon exposure to drugs that prolong the QT/QTc interval than males [7]. Based on the parameters of interest optimizations of observation times and number of subjects were proposed.
Methods
Four TQT studies that collected ECG data after placebo and moxifloxacin treatment were pooled for this assessment providing a sample size of 99 healthy male and female subjects and rich PD data.
All studies were conducted according to the GCP and local regulations and were approved by a local Ethics Committee or an Independent Review Board. Written informed consent was obtained from each subject before any study procedure was carried out. Certified healthy subjects aged 18–45 years were eligible. All subjects underwent a screening process after which eligibility was assessed by the investigators before randomization.
All studies were randomized, double-blind, double-dummy of parallel design. In order to allow the double-dummy, the moxifloxacin tablets were over-encapsulated in a size 00 gelatin capsule and were undistinguishable from the placebo. The over-encapsulation did not yield different PK results in this pool when compared to published data [8]. Only the moxifloxacin arm was used, comprising a single dose of placebo the day before moxifloxacin in order to establish a 24-hour “baseline” ECG profile, the same subjects receiving a single oral dose of 400 mg of moxifloxacin the next day under the same conditions. ECGs were performed at the same time points on both treatment days. The number of evaluable subjects in each study ranged from 22 to 29.
Coincident thorough PD and moxifloxacin PK time points were determined based upon the known PK profile of the investigational medicinal products under development and therefore vary slightly between the studies (refer to Table 1). In this analysis, only the PD data were used. The population PK parameters determined from a previous analysis [6] using the same pool were used in this analysis and their values fixed in the model.
Because they have been shown to exert an effect on the QT/QTc interval, posture, sleep and food intake were taken into account when assessing QT/QTc interval. Because of these predictable changes, subject conditions and timing of ECG collection were standardized across studies.
However, in 1 out 4 studies of the pool, the subjects were administered moxifloxacin in fasting condition, a snack being served 2 h after, followed by a lunch and dinner at T4H and T12H, respectively. In the 3 other studies, the subjects received moxifloxacin 30 min–1 h after a standard-fat breakfast followed by lunch and dinner at T4H and T12H, respectively.
Twelve-lead ECGs were recorded in triplicate at each time point with at least one minute between measurements. All measurements were performed after a minimum 10-minute supine rest. They were digitized and sent to a centralized reading center for semi-automatic (“manual”) reading. The reader was blinded as to time-point, treatment and replicate number. The average of triplicate ECG at each time point was used in the analysis. Among the ECG parameters measured, the mean QT interval and mean heart rate (HR) were used in this PD analysis. As they are known to exert influence on the QT interval, the following covariates were recorded: baseline electrolytes (sodium, potassium and calcium), age and gender. Race and body size descriptors (body weight, height, body mass index, lean body mass and ideal body weight) were also collected or calculated and tested on both the PK (as previously reported [6]) and the PD models.
Pharmacodynamic modeling
Pharmacodynamics
QT interval, HR and QTc exhibit a circadian rhythm. The rhythmicity of the cycle should be taken into consideration when assessing potential QT prolongation effect of a drug [9–11]. Although the TQT study conditions are standardized to minimize the influence of external factors, the reason for this observation could be inherent to the study conditions (the subjects receiving meals, their position changing during the day or some subjects sleeping between assessments, the precision of measure) or a true circadian rhythm [12]. In rhythmology, the most important descriptive method is based on the periodic regression analysis. This is a sinusoidal approximation using sine or cosine function, the cosinor analysis [13]. It provides estimation of rhythm parameters such as mesor, amplitude, and acrophase of circadian rhythmic changes. It helps describe the biological rhythms and facilitates the statistical comparison between oscillatory biological phenomenon.
However, many biological rhythms may deviate from a single periodic function. Assuming a fundamental period of T = 24 h, a multi-oscillator function can be derived to describe the deviation from a single function. This includes several periodic functions with different harmonic components. The multiple harmonic model is usually derived from the fundamental period T and N sub-harmonics whose periods are T/N [14]. Therefore the general form of the equation is:
In this analysis, 1–4 cosine functions were investigated for the circadian rhythm (CIRC1–CIRC4), first using the placebo data. Once validated, the same models were tested against moxifloxacin data. The different models were then:
where QTc0, \( {\text{RR}},\alpha ,{\text{ A}}_{\text{n}} ,\phi_{\text{n}} \) and t denote the triplicate mean predose (baseline) corrected QT interval (intercept)(ms), interval between successive R waves (related to HR), individual heart rate correction factor, the amplitudes of circadian rhythm (ms), the phases (h) and the clock time effect (h), respectively.
Then, the effect of moxifloxacin plasma concentration (CP) (mg/L) was applied using the possible relationships below, slope models (slope (ms.L/mg) parameter) and Emax model (Emax (ms) and EC50 (mg/L) parameters).
Structural models
Slope models
Additive relationship:
Proportional relationship:
E max models
Additive relationship:
Proportional relationship:
Once the best model was selected, the placebo-corrected QT interval difference can be derived from:
Variability models
BSV (η) model was modeled as:
Where Pj is the value of PD parameter with the jth individual, PTV is the typical value of P for the population, η denotes the difference between PJ and PTV
The residual variability (ε) was modeled using additive or proportional error structures as:
Where y ij is the j th observation in the i th individual, F ij is the corresponding model prediction and ε ij is a normally distributed random error with a mean = 0 and a variance σ².
Data analysis
Data were analyzed using the nonlinear mixed effect modeling software program Monolix version 3.1S R2 [15] (http://wfn.software.monolix.org). The pharmacokinetic estimates determined in a precedent analysis were fixed in the model for the pharmacodynamic analysis [6]. The placebo QT time-courses were analyzed first. Then the QT time-courses with placebo and with moxifloxacin were simultaneously analyzed. The parameters were estimated by computing the maximum likelihood estimator of the parameters without any approximation of the model (no linearization) using the stochastic approximation expectation maximization (SAEM) algorithm combined to a MCMC (Markov Chain Monte Carlo) procedure. BSVs were estimated using an exponential error model. Parameter shrinkage was calculated as {1-sd(η)/ω}, where sd(η) and ω are the standard deviation of individual η parameters and the population model estimate of the BSV, respectively. The Likelihood Ratio Test (LRT) including the log-likelihood, the Akaike information criterion (AIC) and the Bayesian information criterion (BIC) was used to test different hypotheses regarding the final model, covariate effect on pharmacodynamic parameters, residual variability model (proportional versus additive error model), structure of the variance–covariance matrix for the BSV parameters. Diagnostic graphics and other statistics were obtained using the R program [16]. From the final model, 100 simulations were performed and the predicted data were compared to the observed data using the visual predictive check (VPC) method. Briefly, the 5, 50 and 95th percentiles at each time from both the simulated and observed data were overlaid on the observed data by using the R program. Then, a visual inspection was performed to ensure centering of the observed data around the model-predicted median and if the proportion of observations out of the model-predicted 5 and 95th percentile curves were not significantly different from 10%.
Results
Population characteristics
From the 99 healthy subjects investigated, 1,401 ECG were available for analysis with a mean of 14.2 time points per subject (range 11–16) during the placebo treatment and 1,403 ECG were available for analysis with a mean of 14.2 time points per subject (range 11–16) during the moxifloxacin treatment.
The subject characteristics at entry into the studies are summarized in Table 2. There were 60 males and 39 females of whom 78 were Caucasian, 9 were Black, 3 were Asian and 9 were multiracial. All subjects were within the reference ranges established for a healthy population by each investigational site for laboratory, vital signs and ECG parameters.
Population pharmacokinetic data
A two-compartment open model with a transit-effect delay in absorption was used [17]. The population PK parameters as determined in a previous population PK analysis [6] with the same pooled subjects were included in the final model (see appendix). The PK covariate effect (body size i.e. lean body weight) was included in the model as a regression variable.
Pharmacodynamic modeling
Among the 4 models tested the 2, 3 and 4-oscillator models were satisfactory (see Table 3) for placebo QT interval circadian rhythm. A model with 2 oscillators (summation from c = 2 to N = 3, equation 1) provided the best BIC value. The parameters of the model were then QTc0, baseline corrected QT interval (intercept); α, individual HR correction factor; A1 and A2, the amplitudes of circadian rhythm; \( \phi_{ 1} \) and \( \phi_{ 2} \), the phases. A proportional error model was finally used to describe the residual variability (lowest BIC, better precision of the estimates), and the between-subject (BSV or η) variabilities could be estimated for all parameters (Table 4). As expected, the main covariate was gender for baseline corrected QT and to a lesser extent on individual heart rate correction factor α [7, 18]. Gender was not found to have a significant effect on the other parameters of the models. No covariance terms were identified to be significant between the parameters. The proportional error model of residual variability provided better results than the constant error model, with similar shrinkages estimator.
The moxifloxacin plus placebo data were analyzed using the same approach in order to confirm that the oscillators selected for placebo were fitting the whole data, especially if the circadian rhythm could be described by the same model as placebo. As shown in Table 5, the same 2-oscillator model provided the lowest values in terms of AIC and BIC. Thus, it was selected for the analysis of the covariates effects..
The effects of moxifloxacin on the QT interval were investigated using direct concentration-QT (C-QT) tendency analysis. Slope and Emax models were investigated [6]. For the Slope models, the proportional relationship with the slope and concentration provided a better description of the effect than did the additive effect model where the slope estimate was not significantly different from zero. Thus, this model was discarded. The proportional effect Slope model was selected to assess the effect of covariates on the model. The parameters of the model were then QTc0, α, A1 and A2, \( \phi_{ 1} \) and \( \phi_{ 2} \) and the slope effect.
The additive effect Emax model (parameters Emax and EC50), provided a better description of the effect than did the proportional Emax and the Slope models based on the AIC and BIC values and was retained as the best covariate-free model (see Table 5).
For both the slope and Emax models, the BSVs were estimated for all structural parameters but \( \phi_{ 2} \). The between-occasion variability (BOV or γ) was tested on each parameter of the models, but was significant on the \( \phi_{ 2} \) parameter only. No covariance terms were significant. The parameter estimates of the proportional effect Slope model with a proportional error model of residual variability is provided in Table 6. For the additive effect Emax models the proportional error model of residual variability provided similar results as the constant error model, including similar shrinkages (refer to tables 7 and 8). The proportional residual error model was finally chosen on the basis of better statistics when comparing the models relative to the bias, precision, correlation, slope (= 1) and intercept (= 0) between observed (OBS) and model-predicted (PRED) data.
The main covariate effect was gender for baseline corrected QT interval and individual heart rate correction factor. No other covariate (e.g. electrolytes, race, age) were found to significantly influence our model.
Table 7 summarizes the final population estimates for this model in which the QT interval increase related to drug concentration is described by an additive Emax model. All parameters were well estimated with low relative standard errors. The empirical Bayesian estimate shrinkages were generally high except for QTC0 and α.
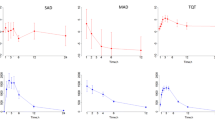
The QT time-courses using the final model are depicted in Fig. 1 for the circadian rhythm (placebo) and moxifloxacin effects on the QT interval. The visual predictive check (VPC) for females and males are depicted separately in Figs. 2 and 3 for the placebo and moxifloxacin treatment. For both, the observed QT intervals were centered around the model-predicted median and the proportion of observations out of the model-predicted 5 and 95th percentile curves were not significantly different from 10%.
Visual predictive check for the circadian changes of QT interval with placebo The dashed lines denote the 5 and 95th percentiles from bottom to top of 100 Monte Carlo simulated predictions. The solid lines stand for the median the observed QT. The bottom and top lines include the 90% confidence interval
Visual predictive check for the effect of moxifloxacin on QT interval. (o) observed data. The dashed lines denote the 5 and 95th percentiles from bottom to top of 100 Monte Carlo simulated predictions. The solid lines stand for the median the observed QT. The bottom and top lines include the 90% confidence interval
The comparative QT time-courses, moxifloxacin versus placebo, as well as the placebo-subtracted QT using the final model are depicted in Fig. 4 for men and women.
Limited sampling strategy
The PFIM program (version 3.2.1) optimises designs in the context of population pharmacodynamics-pharmacokinetics (i.e., the number of samples per subject, the sampling times and the number of subjects) [19]. The aim was to decrease the number of observations. The optimal sampling times were determined using 100 subjects, then the number of subjects was optimized using these times. The estimated %rse for the parameters were in the range of about 11–73%. The Emax parameter, that contributes most to the QT interval prolongation, had a particularly accurate %rse of 11%. The observation time points for the QT interval should minimize the %rse of the “Emax” and “EC50” parameters, since the difference in QT is a function of the moxifloxacin concentration via these parameters. Tables 9 and 10 summarize the results. The following 9 observation times for QT, 0.75, 1.75, 2.5, 3, 3.5, 4, 12, 14 and 16 h, provided a 12% rse for the estimation of the Emax parameter. Deleting 2 time points resulted in a small increase in the %rse to 15%. Based on a 15% precision limit on Emax a sample size of 60 subjects was optimal.
Discussion
The circadian rhythm of the QT interval after placebo dosing was satisfactorily described using a 2-oscillator model. Based on this model, the moxifloxacin effect on QT was satisfactorily described by the same equation with the adjunct of an Emax additive drug concentration-effect. This is the first time the effect of moxifloxacin on QT is ascribed to an Emax model with the estimation of an EC50, previous studies used a proportional concentration effect.
The visual predictive check showed that this population model was accurate in both the description of the phenomenon but also in the description of the variability. As expected, the gender was a significant covariate in our QT models. As shown before, adult females exhibited longer baseline QT/QTc intervals [6]. They also present a greater propensity to develop torsades de pointes upon exposure to drugs that prolong the QT/QTc interval than males [7]. No statistically significant relationship was detected between gender and parameter Emax showing no particular propensity to develop higher QT prolongation when female. Normal electrolyte concentrations were ensured in the selected healthy population which may explain why these covariates had no significant effect.
This study showed the need for a careful placebo control of QT/QTc investigations and consideration of circadian rhythm of the QT interval. As shown in Fig. 4, QT variations occurred after placebo dosing. The adjunct of a baseline placebo assessment of ECG changes greatly improves the quality of the conclusions drawn on QT prolongation observed during investigational product treatment. Incorrect conclusions on QT prolongation can be made if the drug-induced prolongation is not corrected for placebo. In this study, the placebo and moxifloxacin administrations were done on 2 consecutive days. The days of assessments were close enough to ensure that the study conditions were similar. Thus, the same diurnal rhythm evidenced with placebo was deemed applicable to the moxifloxacin day. It would not have been necessarily the case with a cross-over study design with wash-out periods where subjects or study conditions are more likely to differ. However, as a single sequence placebo/moxifloxacin was applied to each study of the pool, this could have lead to a bias if a given condition influencing the QT interval was specific to one or the other day. Except PK sampling not performed on the placebo day, no other difference was evidenced.
Finally, this PD model allows some proposals for optimized sampling strategies maintaining satisfactory estimates of the parameters of interest. The present design included up to 16 time points for the pharmacodynamic evaluations. Using the selected population model, 9 observation times for QT interval could provide satisfactory estimates for the main parameters of interest. Because drug pharmacokinetics is generally known before a TQT study and the largest QT variation depends on the peak drug concentration, some limited sampling strategy designed to accurately describe the peak drug concentration could be used in order to investigate maximal QT variations.
The ICH E14 guidance sets strict limits for the interpretation of drug-induced QTc changes [1]. Because the interpretation is driven by the upper confidence interval rather than by the mean QTc change, the sample size of a TQT study is high [20]. The sample size necessary for a TQT study depends on the assumed within-subject variance based on the number of ECGs to be used and the maximum allowable placebo-adjusted true mean change from baseline increase in QTc (10 ms according to the E14 guidance). In addition, the sample size requirements for a TQT study depend on the assumed true effect of the study drug [21]. When considering the C-QT analysis, the sample size can be determined by setting an acceptable threshold of variability on the parameter of interest. The C-QT analysis and modeling approach proposed in this work is an interesting alternative to the ICH E14 guideline in assessing the QT prolongation effect. Although our models used one dose level (400 mg) of moxifloxacin, this approach provides accurate information over a range of concentrations using different relationships (slope or Emax models) to quantify the concentration–response relationship. The development of C-QT analysis as part of TQT studies is an important step to assess an investigational medicinal product potential for QT prolongation. Extension to modeling of the C-QT relationship using early phase I studies data like the first in Man, provides a unique opportunity to study the effect on QT over a wide range of concentrations [3, 22]. This would also allow early detection of QT prolongation signal and impact further clinical plan, especially TQT study positioning, or design of studies when a robust TQT analysis is not yet available.
References
U.S. Department of Health and Human Services Food and Drug Administration (2005) International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use. The clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs (ICH E14). Rockville, MD
Bayer Pharmaceuticals (2003) Avelox (moxifloxacin) package insert. West Haven, CT
Garnett C, Beasley N, Bhattaram VA, Jadhav PR, Madabushi R, Stockbridge N, Tornoe CW, Wang Y, Zhu H, Gobburu JV (2008) Concentration-QT relationships play a key role in the evaluation of proarrhythmic risk during regulatory review. J Clin Pharmacol 48:13–18
Russell T, Riley SP, Cook JA, Richard L, Lalonde RL (2008) A perspective on the use of concentration-QT modeling in drug development. J Clin Pharmacol 48:9–12
Bloomfield D, Krishna R (2008) Commentary on the clinical relevance of concentration/QTc relationships for new drug candidates. J Clin Pharmacol 48:6–8
Grosjean P, Urien S (2012) Reevaluation of moxifloxacin pharmacokinetics and their direct effect on the QT interval. J Clin Pharmacol 52:329–338
Drici MD (2001) Influence of gender on drug-acquired long QT syndrome. Eur Heart J Suppl K(3 Suppl):K41–K47
Stass H, Kubitza D (1999) Pharmacokinetics and elimination of moxifloxacin after oral and intravenous administration in man. J Antimicrob Chemother 43(Suppl B):83–90
Piotrovsky V (2005) Pharmacokinetic-pharmacodynamic modeling in the data analysis and interpretation of drug-induced QT/QTc prolongation. AAPS J 7:E609–E624
Smetana P, Batchvarov V, Hnatkova K, Camm AJ, Malik M (2003) Circadian rhythm of the corrected QT interval: impact of different heart rate correction models. Pacing Clin Electrophysiol 26:383–386
Browne KF, Prystowsky E, Heger JJ, Chilson DA, Zipes DP (1983) Prolongation of the Q-T interval in man during sleep. Am J Cardiol 52:55–59
Malik M, Hnatkova K, Schmidt A, Smetana P (2008) Accurately measured and properly heart-rate corrected QTc intervals show little daytime variability. Heart Rhythm 5(10):1424–1431
Nelson W, Tong YL, Lee JK, Halberg F (1979) Methods for cosinor-rhythmometry. Chronobiologia 6:305–323
Fernandez JR, Hermida RC, Mojo A (2009) Chronobiological analysis techniques. Application to blood pressure. Philos Trans R Soc A 367:431–445
Kuhn E, Lavielle M (2005) Maximum likelihood estimation in nonlinear mixed effects models. Comput Stat Data Anal 49:1020–1030
R Development Core Team (2009) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Savic RA, Jonker DM, Kerbusch T, Karlsson MO (2007) Implementation of a transit compartment model for describing drug absorption in pharmacokinetic studies. J Pharmacokinet Pharmacodyn 34:711–726
Sullivan TJ, Lettieri TJ, Liu P, Heller A (2001) The influence of age and gender on the pharmacokinetics of moxifloxacin. Clin Pharmacokinet 40(Suppl 1):1–18
Bazzoli C, Retout S, Mentré F (2010) Design evaluation and optimisation in multiple response nonlinear mixed effect models: PFIM 3.0. Comput Methods Programs Biomed 98(1):55–65
Malik M, Hnatkova K, Ford J, Madge D (2008) Near-thorough QT study as part of a first-in-man study. J Clin Pharmacol 48:1146–1157
Bloomfield DM, Kost JT, Ghosh K, Hreniuk D, Hickey LA, Guitierrez MJ, Gottesdiener K, Wagner JA (2008) The effect of moxifloxacin on QTc and implications for the design of thorough QT studies. Clin Pharmacol Ther 84(4):475–480
Rohatagi S, Carrothers TJ, Kuwabara-Wagg J, Khariton T (2009) Is a thorough QTc study necessary? The role of modeling and simulation in evaluating the QTc prolongation potential of drugs. J Clin Pharmacol 49(11):1284–1296
Acknowledgments
We acknowledge Franck Poitiers, Biostatistics Department of sanofi R&D, for the building of the pooled study database.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 11.
Rights and permissions
About this article
Cite this article
Grosjean, P., Urien, S. Moxifloxacin versus placebo modeling of the QT interval. J Pharmacokinet Pharmacodyn 39, 205–215 (2012). https://doi.org/10.1007/s10928-012-9242-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-012-9242-8