Abstract
Purpose To evaluate whether a protocol for early intervention addressing the psychosocial risk factors for delayed return to work in workers with soft tissue injuries would achieve better long-term outcomes than usual (stepped) care. Methods The study used a controlled, non-randomised prospective design to compare two case management approaches. For the intervention condition, workers screened within 1–3 weeks of injury as being at high risk of delayed returned to work by the Örebro Musculoskeletal Pain Screening Questionnaire—short version (ÖMPSQ-SF) were offered psychological assessment and a comprehensive protocol to address the identified obstacles for return to work. Similarly identified injured workers in the control condition were managed under usual (stepped) care arrangements. Results At 2-year follow-up, the mean lost work days for the Intervention group was less than half that of the usual care group, their claim costs were 30% lower, as was the growth trajectory of their costs after 11 months. Conclusions The findings supported the hypothesis that brief psychological risk factor screening, combined with a protocol for active collaboration between key stakeholders to address identified psychological and workplace factors for delayed return to work, can achieve better return on investment than usual (stepped) care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Soft tissue (musculoskeletal) injuries are the most common work-related injuries and while little time is lost from work for most cases, a small proportion have delayed recovery and delayed return to work (RTW) [1, 2]. For this group, length of absence is associated with an increased risk of never returning to work; longer term ill-health and financial insecurity; and costs to the community [2,3,4]. Prospective studies indicate that psychological and social/environmental factors are strong predictors of delayed recovery and disability associated with chronic pain [5,6,7]. As many of these psychosocial risk factors (e.g. anxiety, depression, catastrophizing, poor workplace support) are modifiable, interventions targeting them could prevent long-term disability [8].
We know that psychologically-informed treatments provided for injured workers without psychological risk factors, are no better than usual treatment [9]. However, superior benefits have been found when they are employed only for patients with psychological risk factors [9,10,11].
When RTW is the goal, an additional focus on the workplace appears essential [12, 13] For example, an RCT of the effectiveness of a guideline-based intervention within one company, found implementation of the experimental intervention was impeded by unforeseen organizational obstacles at one of two sites, thereby undermining the results [14]. Recently, Cullen et al. [15] confirmed that better RTW results are obtained when treatment for injured workers is integrated with workplace support, but implementation is a major challenge. In a compensable environment, integrating the treatment protocol within the normal practice of the insurance company, as well as the workplace, has also been recognized as important [13].
At the conceptual level, the relatively new field of Implementation Science provides useful frameworks for addressing these challenges. The Exploration, Preparation, Implementation, Sustainment (EPIS) framework for implementation research [16] has been recommended for the conceptualization and planning of RTW interventions for injured workers [17] as it takes into account interacting and multi-level factors. Specifically, the EPIS framework identifies five domains to be considered: intervention characteristics, outer setting (regulators, treatment providers), inner setting (workplace), characteristics of the individuals involved, and the actual process of implementation. This perspective was used in the present study to guide the sustained implementation of the intervention protocol with an insurer and a large, multi-site workplace. The primary goal was to test whether early screening for psychological risk factors, coupled with an intervention that incorporated the EPIS perspective could achieve reduced lost time from work.
Methods
The work injury screen early (WISE) study intervention protocol was initially tested in a small pilot study in Sydney [18]. The protocol entailed a coordinated approach to injured hospital workers identified by a brief psychological screening instrument as high risk for delayed recovery. The intervention targeted both psychological and workplace risk factors. The usual-care approach, as recommended by the existing state-wide guidelines for injured workers [19], follows a stepped-care model [20] whereby considering psychological and social risk factors is indicated only after a poor response to initial treatment (6–8 weeks after the injury). In the WISE protocol, those injured workers (IWs) who had taken medically-sanctioned time off work were screened for psychological risk factors within the first 1–3 weeks after their injury, regardless of progress in initial treatment, and an intervention plan was to be implemented immediately.
Participants and Pain Sites
Study participants were recruited from consecutive injured (public) hospital workers with work-related soft tissue injury. Initial consent for screening (by telephone) was obtained by the insurance case manager 1–3 weeks after injury and those consenting were administered the 10-item Örebro Musculoskeletal Pain Screening Questionnaire—Short Form (ÖMPSQ-SF) [21, 22]. Additional consent from those offered the intervention arm of the trial was obtained later at the workplace.
The Case managers (CMs) of the insurance company (known as a ‘Scheme Agent’ in the New South Wales (NSW) Workers’ Compensation system) were divided into two independent teams by the senior management: one for the designated Intervention hospitals and the other for the designated Control (Usual Care) hospitals.
The completed screening instruments were scored separately by the Research Manager, who advised only the CMs for the Intervention hospitals and the hospital’s return-to-work (RTW) Coordinators of the outcome. The insurance claims team, the workplace, and the treatment providers for the Control hospitals were not given this advice and were therefore blind to the risk status for their IWs. The workers from the Intervention hospitals met with their RTW Coordinator within a week to discuss what the study entailed. Those who consented were enrolled for the intervention arm of the study. Those who declined to participate received usual care (as for the Control condition, but were out of the study as their classification as high risk was no longer blinded). The identified high-risk workers from the Control hospitals received usual care under the NSW Workers’ Compensation system. Prospective participants were recruited between September 2013 and June 2015. This resulted in fewer participants being recruited than originally intended, but the funding bodies, including the employer, wanted recruitment to stop in order to enable the Control hospitals and others across the state to implement the intervention protocol. As a result, the Research Manager’s role was changed to Implementation Manager to facilitate the general implementation across the state during the follow-up period.
Specific Hypotheses Tested
The Intervention condition would have significantly fewer lost work days over the ensuing 2 years period.
The mean costs of claims (for lost time and treatments) would be less for the Intervention condition.
Inclusion/Exclusion Criteria
Health care workers reporting work-related soft tissue injuries that were accepted by the insurer, and had taken (medically-sanctioned) time off work due to their injury. All participants had to be able to read and speak English well enough to not require an interpreter. All participants provided verbal informed consent to participate in the screening phase prior to the telephone screening.
Exclusion Criteria
Prospective participants were excluded if they had made a stress (or psychological injury) claim, had no time off work, had been assessed by their treating doctor as requiring surgical intervention, or declined to participate.
Study Design
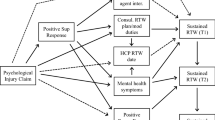
A controlled, non-randomised, prospective design was used (Fig. 1). The outcomes of high-risk workers from Intervention hospitals were compared with the outcomes of similar high-risk workers from other (public) hospitals (controls). Assignment of workers to Intervention or Control groups was based on which hospital employed them.
Public hospitals with the largest staffing levels were selected by the employer (the NSW Ministry of Health) to participate. The representative (MM) of the Ministry of Health (not the researchers) independently assigned the hospitals to Intervention (n = 11) or Control groups (n = 6) and attempted to balance those in inner city areas versus suburban and peripheral regions, as well as the injury rates for the previous 2 years. This was intended to maximise the chances of equivalent numbers in each condition.
Since both RTW coordinators and supervisors at each workplace were integral contributors to the intervention protocol and usual care, random assignment to treatment/control was not possible. Instead, blinding of the claims team, RTW coordinators, supervisors and treatment providers regarding the risk status of controls was employed.
Data on work status, lost days, and costs were maintained by the insurer as normal for a minimum of 2 years from the date of injury. At 1 year from the date of injury all participants were telephoned by an independent research assistant, blind to the group status of each worker, to answer questions on their current work and pain status, treatment and RTW experiences. Originally, it was intended to include a 5 year follow-up, but as mentioned earlier the funding bodies, including the employer, decided to stop the trial after 2-years of follow-up as they felt the outcomes were clear and they wanted to implement the protocol to the Control (usual care) sites and all public hospitals across the state. Follow-up data collection continued until the last participant reached the 2-year follow-up.
Sample Size
Based on differences in time lost for the high-risk patients in the pilot study (standardised mean difference approximately 0.3) and our expectation that our study would have a stronger effect, we used a standardised mean difference of 0.4, with alpha = 0.05 and power = 0.8 to calculate the sample for the main study [18]. This yielded a requirement of 100 cases per group, but to allow for possible drop-outs we added 10% per group (i.e. 110 high risk workers per group, 220 in total). This figure is similar to the estimated sample size for a similar study in Norway [23].
Protocol for Intervention Condition
As this study involved several stakeholders working in a coordinated way, the (abbreviated) roles of each are specified here. A fuller account is currently in preparation for separate publication. The implementation of the protocol by all stakeholders was monitored closely by the Research Manager throughout the project to ensure adherence, as much as possible.
Workplaces and RTW Coordinators
Workplace interventions depended upon what workplace RTW obstacles were identified by the psychologist or RTW coordinator for each worker. The RTW coordinator met (face to face) with all high risk workers within a week of the telephone screening to recruit them for the study and, if successful, to arrange for them to see the selected psychologist within the next week for an assessment and possible treatment.
The RTW coordinator was expected to be in regular contact with the workers, as well as their General Practitioner (GP), CM, and the treating psychologists throughout their treatment. They were also expected to work closely with each worker’s workplace supervisor to assist the RTW processes, including managing any identified workplace RTW obstacles.
Psychologists
To participate in the project the psychologists had to work near the Intervention hospitals, to be experienced in managing injured workers, and to agree to follow the intervention protocol. This required them to assess the workers within a week of referral and to address any identified psychological obstacles to RTW within six sessions. They were also expected to maintain regular contact with both the workplace (RTW coordinator) and other treatment providers, as appropriate (GP, physiotherapist).
Nominated Treating Doctor (GP)—Primary Care General Medical Practitioners
The GPs were chosen by the injured workers, as per normal for injured workers in NSW. The CM at the insurance company contacted each GP in the initial stages of establishing the claim (their ‘3-point contact’ with the injured worker, GP, and RTW coordinator). The GPs were informed their patient was in an approved trial and details of the trial were provided by the RTW coordinator.
The (Insurance) Case Manager (CM)
The CM referred the participating workers to a selected independent medical consultant (usually an occupational or rehabilitation physician) for an early specialist review (between 6 and 8 weeks after the injury).
If required, the CM arranged a case conference involving the worker, their GP, RTW coordinator, and CM. The case conference was intended to review the obstacles to RTW and to reach agreement on a plan for overcoming them.
Independent Medical Consultants (IMCs)
The IMCs agreed to review all referred workers within 6–8 weeks and then to liaise with the GP, RTW Coordinator and CM. If appropriate, the IMC was asked to reassure the worker that s/he had a soft-tissue injury that would resolve fairly quickly and they should be able to RTW without risk.
Physiotherapists
As usual in NSW, the physiotherapists providing care were selected by the workers’ GPs and reported to the CM and GP on their progress. The physiotherapists treating Intervention workers were advised by the CM that the worker was participating in a study aimed at facilitating early RTW. The physiotherapists were expected to have a good understanding of the importance of an activity-based approach to treatment. The approved basic physiotherapy treatment plan was eight sessions.
Independent Physiotherapy Consultant (IPC)
An independent physiotherapist (RB) conducted a file review of any case if the treating physiotherapist requested more than eight sessions, and then recommended to the case manager if the request should be accepted or denied. When necessary, the IPC reminded the treating physiotherapists under review of the importance of using an activity-based approach.
Protocol for Control Condition
High risk workers at the Control hospitals received treatment as usual under the Work Cover NSW Soft Tissue Injury Guidelines [19].
Measures
Screening Measure
The ÖMPSQ-SF contains ten items, each scored on a 0–10 scale, to yield a possible score between 0 and 100. Workers scoring ≥ 50 (out of 100) were considered at high-risk of delayed recovery [21]. This criterion was validated in Sydney. [22]
Outcome Measures
Days to Pre-injury Duties (PID)
Operationalised as lost time from work (number of days reimbursed for missing work) over 2 years. The data on lost work time were obtained from the insurance company. Time to return to PID is not a binary variable and is complex (because after returning to work a worker may take more time off later). Accordingly, lost work days is the best available proxy for return to PID.
Total Claim Costs
These data were also obtained from the insurance company records. These include costs for both wage replacement and treatments, including the costs of the psychologists for the intervention group.
Supplementary Data
-
i.
Participants’ evaluation (answers to blinded follow-up interviews at 1 year). These were based on telephone follow-up by a research assistant blind to group membership. Included were the ÖMPSQ-SF, questions about the participants’ satisfaction (on a 0–10 scale) with how their work injury had been handled by the workplace, the insurer and the treatment providers, plus questions about any pain they might still be experiencing (copies available from the first author).
-
ii.
Acceptability of the intervention protocol for employer and insurer.
To evaluate the acceptability of the WISE protocol for the management of workers with recent musculoskeletal injuries by the insurer and employer their response was sought from representatives of both the employer (MM) and insurer (KM) at the end of recruitment.
Psychological Treatment Outcome Measures
The changes in psychological risk factors following the psychological treatments (only) were evaluated by the treating psychologists before and after their treatments using these measures:
- i.
ÖMPSQ-SF [21].
- ii.
The 21-item version of the Depression Anxiety Stress Scales (DASS) [24], assessed severity of distress. The three subscales were combined to produce a single score. Total scores could range between 0 and 63.
- iii.
The Brief Pain Inventory (BPI) (Interference scale) [25] provided a general measure of interference in daily activities due to pain. Possible scores can range from 0 to 10.
- iv.
The Pain Self-Efficacy Questionnaire (PSEQ) [26] measures the strength and generality of a patient’s beliefs about their ability to accomplish various activities despite their pain. Scores range from 0 to 60. Higher scores indicate stronger self-efficacy beliefs.
- v.
The Pain Catastrophising Scale (PCS) [27] provides a measure of distressing thoughts about pain. Total scores range between 0 and 52.
Statistical Analyses
The demographic and medical characteristics of the sample were described using means, standard deviation and response frequencies. The pre-post changes in scores on the psychometric instruments from pre- to post-(psychological) treatment were appraised using paired t-tests and linear mixed models (the latter to account for clustering by health district and to handle missing data by using all available data), and measures of effect size were examined by appraisal of standardised mean differences (Cohen’s d).
For the return to work outcomes—lost work days—the primary analysis was based on the data at 24 months post-injury, for which all participants had data. The data available for this variable are a proxy for days to PID, but are not technically a time-to-event variable (as described above), and were complete (i.e., no censored observations) so differences between the Intervention and Control groups on this variable were examined in several ways.
First, an independent-samples t test with 1000 bootstrapped samples (because of anticipated skew) was conducted and 95% bias-corrected and accelerated confidence intervals (95% BCa CI), with equal variances not assumed, were calculated. Second, a Cox regression analysis, which avoids the assumption of normality by treating lost work days as a time-to-event variable (i.e., a proxy for days to PID), was conducted and predictors (in this case, Intervention vs. Control condition) of lost work days were identified. Third, treating lost work days as a binary variable, participants were classified as either having returned to work or not after 3 months (the time after which pain is classified as chronic [28], and the groups were compared using the Fisher test. The equality of variances between the two groups was also examined.
For the cost data, the equality of variances between the two groups was examined. Change in cumulative costs over time was calculated using a linear mixed model with repeated measures (with autoregressive variance–covariance matrix), accounting for clustering by health district. Because bootstrapping was not available for this analysis, the positive skew of the cost data was accounted for by taking the natural logarithm of cost, whose distribution closely approximated normal.
Responses to the blinded telephone interviews at 1-year were compared between groups using χ2 tests of independence for categorical variables and independent-samples t-tests for continuous variables using the Hochberg Type I error correction method [29].
Results
Number of Claims
A total of 1655 claims were received in the study period. Exclusions included severe injuries (n = 299), no lost time (n = 416), ineligible claims (n = 111). This left 829 eligible claims for screening. Of these, 580 (70%) were screened, 77 (9%) refused screening, and 172 (21%) were missed due to contact difficulties (see Fig. 2).
In total, 133/366 (36%) from the Intervention hospitals and 75/213 (35%) from the Control hospitals were identified as high risk. This suggests the two samples were comparable in terms of psychological risk characteristics.
Mean lost work days for high risk cases in the Control condition was 66.5 (SD = 116.2) versus 20 days (SD = 30, median = 10.1) for the low-risk cases (Cox regression hazard ratio = 0.5, p < .001). This finding supports the validity of the ÖMPSQ-SF as a screening measure in discriminating between those likely to be delayed in RTW and those who are not [22].
Final Sample
Intervention Condition
Of the 133 high-risk Intervention claims, 67 (50%) refused the psychological assessment. Of the 66 who agreed to a psychological assessment, 10 (15%) refused to have psychological treatment, 6 (8%) withdrew from treatment, 4 (6%) were assessed by the psychologist as not requiring their treatment, and 2 (3%) required additional (beyond 5 sessions) psychological treatment. Of the 46 (70%) who attended some Psychological treatment, 1 was later found to have had no initial time loss and 11 required surgery (both of which were exclusion criteria, but were missed when the data were recorded by the CM at the time). These 12 (16%) were excluded, leaving a total of 54/66 (82%) for analyses by intention-to-treat principles. There was no significant difference in ÖMPSQ-SF scores between those who refused psychological assessment (mean = 57.5, SD = 6.8) and those who agreed (mean = 59.6, SD = 7.1), 95% BCa CI (− 4.54, 0.13).
Control Condition
Of the 75/213 (68%) high-risk Control claims, 5 had no initial time loss, and 11 required surgery. After these 16 were excluded the total for the Control condition was reduced to 59.
Loss to Follow-Up
As the data on time lost from work and costs were maintained by the insurer, none of the 113 (54 Intervention + 59 Control) participants were lost to follow-up over the 24 months.
Characteristics of the Injured Workers in Both Groups
The average age of the sample was 45 years (range 23–75), and 80% were women (reflecting the nature of the workforce in hospitals). Occupational categories were broad, and included registered nurses, security staff, orderlies, technicians, managers, administrative staff, and paramedics. Mean baseline OMPSQ-SF scores did not differ significantly between Intervention (mean = 58.94, SD = 6.73) and Control groups (mean = 59.46, SD = 8.56), t(111) = 0.35, p = .725.
Main Injury Sites and Medical Diagnoses
Based on the medical reports, ‘Backs’ represented about a third of cases, the upper limbs and lower limbs next most frequent. The most common diagnoses were: Trauma to Muscles (41); Soft Tissue Injuries due to Trauma or unknown mechanisms (22); Trauma to Joints and Ligaments, unspecified (17); Contusion, Bruising and Superficial Crushing (7); Disc Displacement, Prolapse, Degeneration or Hernia (5).
Psychology Treatment Outcomes
The psychologists, on average, provided five treatment sessions and exceeded this in only two cases. The results indicate the identified psychological risk factors were significantly reduced following treatment (see Fig. 3). It should be noted that these measures were collected for the Intervention group only in order to test if changes occurred on these variables as expected.
Mean ÖMPSQ-SF score reduced from high-risk to low risk range (58.9; SD = 7.6 vs. 35.4; SD = 14.8, respectively), standardised mean difference, d = 1.99. The improvements on all measures were clinically and statistically (p < .0005) significant, when analysed using both paired t-tests and linear mixed models to account for clustering by health district. The standardised mean difference (d) for each was in the large range (> 0.8). For distress (DASS total score) d = 0.81; for disability (BPI) d = 1.15; for pain self-efficacy (PSEQ) mean score improved from 33.1 (SD = 13.6) to 45.8 (SD = 12.8), d = − 0.97. Although not high initially, the mean score on catastrophising (PCS), the SMD for improvement in pain catastrophising was still 0.91.
Return to Work Outcomes (lost work days)
At 24 months post injury, the mean lost work days was 66.5 (SD = 116.2) for the Control condition and 31.7 (SD = 36.7) for the Intervention condition (Fig. 4). Using the t-test approach, the confidence interval (8.8, 65.1) did not include 0, indicating a group difference.
Secondly, using Cox regression, the proportional hazards assumption was satisfied, and the group difference was not significant (hazard ratio = 1.39, p = .088). Thirdly, using the Fisher test approach, the proportion with lost work days > 3 months was significantly greater in the Control group vs the Intervention group (see Table 1).
It was also found that the variability in days lost over the first 24 months was significantly higher in the Control condition than in the Intervention condition (F = 14.37, p < .001).
Cost Outcomes
Costs comprise a combination of payment for lost time at work and treatment-related costs.
Mean (Total) Costs
At 24 months, the group mean total costs for the Intervention condition were $16,443 and for the Control condition were $23,405, a difference of $6962. Although this represents a 30% difference, and is of importance to the insurer and employer, an independent samples t-test with 1000 bootstrapped samples revealed this difference was not statistically significant (95% CI − 1369.76, 15,634.60). However, the difference in variability for costs between the groups was statistically significant (F = 13.32, p < .001), with smaller variability in the Intervention condition than the control condition, consistent with the pattern of variability found in the days lost results.
Costs Over Time
In the first 10–11 months, there was little difference in the growth in average costs between the Intervention group and the Control group, but thereafter the Control group costs continued to rise while the Intervention group costs appeared to plateau, indicating effective return to PID. As expected, using the 24-month data, cumulative costs significantly increased over time, F(23, 2538.19) = 163.37, p < .001. The difference in change over time between groups was statistically significant (F(23, 2538.19) = 4.611, p < .001), indicating that the costs were rising more rapidly over time for the Controls compared to the Intervention condition.
Another way of describing the evolution of costs over time is presented in Fig. 5. This includes the outcomes in claims costs up to and beyond the formal analyses conducted on 24-month follow-up data by showing the claim costs over 46 months (primarily, lost time from work as this was the major cost driver). This figure reveals a gradual decline towards zero (apart from the odd spike) for the Intervention group, whereas payments for the Control group continue to peak increasingly over time.
Participants’ Evaluation (Blinded Follow-Up Interviews at 1 Year)
One year after entering the study 75 (66.4% of the total) participants were available for the blinded telephone interviews. Of the 75, 35 (47%) were from the Intervention condition and 40 (53%) were Controls. For this subset, baseline ÖMPSQ scores did not differ significantly between the Intervention (mean = 58.6, SD = 6.1) and Control (mean = 58.3, SD = 6.8) groups, 95% BCa CI (− 3.26, 2.63), indicating no initial risk status differences.
Of the questions asked about satisfaction with the RTWC, workplace manager, and case manager, there were no differences between groups on satisfaction with the RTWC or workplace manager, but there was a difference in satisfaction with the case manager, with the Intervention group reporting higher satisfaction (7.4 vs. 5.8, p < 0.03; for Intervention vs. Control, respectively). The only other difference found related to the presence of ongoing pain, which also favoured the Intervention group. Ongoing (chronic) pain was assessed by two statements [“Always present (intensity varies)” and “Often present (pain free periods < 6 h)”] 14 (43.7%) and 4 (14.3%) of the Control and Intervention condition participants, respectively, confirmed one of these statements (χ2 = 16.23 (p = .001). However, using the Hochberg Type I error correction method, the differences in satisfaction and presence of chronic pain were not statistically significant due to the number of variables tested and the small number of cases. Accordingly, these findings should be treated as preliminary and requires further study.
The Validity of Results: Acceptability of the Protocol to the “Stakeholders”
At the completion of recruitment, all participating hospitals were offered the opportunity to either employ the WISE protocol or resume usual care for managing injured workers, as per the Control condition. All the hospitals (Intervention and Control) elected to employ the WISE protocol.
In addition, the feedback from the claims teams indicated their relationships and communications with the RTW coordinators at the Intervention hospitals had noticeably improved during the study.
Also, the employer, the NSW Ministry of Health, based on their experience with the WISE protocol, elected to adopt the protocol for all public hospitals across the state, including the Control hospitals, and this was implemented over the following year (2016) with the help of the Research Manager.
Discussion
Combined with our earlier paper on the validity of the OMPSQ-SF [22], this trial provides evidence that psychological screening can identify injured workers at high risk of delayed RTW, and that a comprehensive protocol to address the identified needs of these workers was associated with less lost work time than usual (stepped) care. Importantly, the pattern of results was evaluated over a 2-year follow-up period.
These findings are strengthened by their consistency with those of Cullen et al. [15] that indicated better RTW outcomes are more likely when the psychological treatment is linked closely to the workplace. The findings are also consistent with recommendations [9, 10] that early psychosocial intervention for recently injured people should be reserved for those with identified psychological risk factors. The improvements on the psychological risk factors following treatment by the psychologists confirms these are modifiable.
At 24 months follow-up, average claims costs showed an advantage for the intervention condition of just under $7000 per case, which, although not statistically significant, represents a 30% difference. Interestingly, the Control group costs continued to rise over time, while the Intervention group costs appeared to plateau at about 10–11 months. This suggests the intervention provided better value for money over usual care.
The higher variability in lost time and costs for the Control over the Intervention condition may reflect the more subjective individual decision-making approach by the claims team under usual care arrangements versus the more standardised WISE protocol. The reported improved working relationships between the workplace and claims teams for the intervention hospitals should also be noted in this context. The decision-making processes for the usual care condition are consistent with a stepped-care approach (whereby intervention decisions are based on failure of initial treatments). In contrast, the WISE protocol was consistent with a matched-care approach [30] with early risk screening followed closely by treatment based on individual psychological assessment, rather than a stepped-care paradigm with its inherent delays in obtaining such help.”
Åsenlöf et al. [31] demonstrated similar benefits for early matching of patients with low back pain (in primary care) to treatment based on individual behavioural assessments versus guideline-informed exercise-based treatment.
A key goal in occupational injury research is implementation of the findings into normal practice [14] The fact that all participating hospitals chose to maintain the WISE protocol for managing their injured workers, and that the employer adopted the protocol for all public hospitals across the state indicates the acceptability of the protocol. This outcome also provides support for the theoretical framework (EPIS) [17] concerning the implementation of an intervention within a complex organisation. In this case, the research team engaged with the insurer and the employer at multiple levels of management, including senior management and those most directly involved (the Case Managers and RTW Coordinators), as well as the workers’ compensation scheme regulator, and the clinicians involved in service delivery to facilitate the implementation of the protocol.
In evaluating the study’s strengths and limitations, the lack of random assignment to either condition is a limitation, but as indicated in the Methods section, it would have risked compromising the protocol at the different workplaces and at the claims office. This is a recognised problem for the evaluation of complex interventions in a multi-stakeholder environment, where many interacting elements contribute to the intervention process [32]. Possible options in this situation include cluster randomisation and stepped-wedge designs [33], and these were considered but had to be rejected for practical reasons. Instead, we manualized the intervention, which was based on a previous pilot study, and maintained as much blinding as possible for the control condition.
The high proportion (50%) of high-risk workers who declined participation in the study is a serious challenge for implementation into usual practice, but not uncommon in similar workplace research studies. For example, a Norwegian study [23] reported that 310 of 723 eligible patients declined to participate, and in a Dutch study [34] reported that only 145 of 686 suitable employees participated in their study. These high refusal rates may be related to workers’ understandable concerns about the possibility of jeopardising their chances of RTW. Clearly, more research is needed on ways of encouraging injured workers to participate in intervention trials. Finally, as only one large employer was involved it cannot be assumed the same outcomes would be found with smaller employers, where there may be less flexibility to provide job accommodations. Future studies should test similar protocols with small and mid-size employers.
Strengths of the study include its systematic use of screening and a protocol-driven complex intervention for workers within 1–3 weeks of injury, along with the 2 year follow-up. The early identification process administered to all injured workers with lost time claims by a busy claims office not only provides a measure of ecological validity for the study, but may have yielded a more generalizable sample relative to studies recruiting from clinic attenders, where there may be delays in seeking care. The long-term follow-up was also a strength, especially given that most studies in this area have a 12 month, or less, follow-up period (e.g., [24, 35]. That differences between groups continued to strengthen over time, even after 10–11 months post-injury, suggest that future studies in this area should consider longer timeframes for their evaluations.
The heterogeneous nature of the participants’ injuries, although considered ‘soft tissue’ was also a strength. In contrast to those studies limited to one site of injury, this study expanded the practice of psychosocial screening to work injuries in general. Another strength was the use of a contemporaneous control condition of similarly injured workers. This controlled for the possible effects of changes in legislation, insurance claims practice, and workplace policies that could affect the management of injured workers (see [36, 37]. Finally, the use of actual, and not estimated, claims costs enables readers to evaluate the return on investment for the use of the protocol. Even so, we did not assess costs to the injured workers and that is a limitation that must be addressed in future as they can be substantial [38].
In summary, this study evaluated a multi-level, protocol-driven intervention by multiple stakeholders for injured workers screened as at-risk of delayed recovery due to psychosocial factors. The findings supported the hypothesis that brief psychological risk factor screening, combined with a protocol for active collaboration between key stakeholders to address identified psychological and workplace factors for delayed return to work, can achieve better return on investment than usual (stepped) care.
Change history
14 August 2019
The original version of this article unfortunately contained a spelling error in one of the co-authors’s names. The family name of the co-author was incorrectly displayed as “James McCauley” instead of “James McAuley. The original article has been corrected.
References
Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, et al. Prognosis of recent onset low back pain in Australian primary care: an inception cohort study. Br Med J. 2008. https://doi.org/10.1136/bmj.a171.
Social Research Centre. Return to work survey, 2017/18 headline measures report. Canberra: Safe Work Australia; 2018.
Johnson D, Fry T. Factors affecting return to work after injury: a study for the Victorian WorkCover Authority. Melbourne Institute of Applied Economic and Social Research Melbourne, 2002.
Schofield DJ, Shrestha RN, Percival R, Callander EJ, Kelly SJ, Passey ME. Early retirement and the financial assets of individuals with back problems. Eur Spine J. 2011;20(5):731–736.
Campbell P, Wynne-Jones G, Muller S, Dunn KM. The influence of employment social support for risk and prognosis in nonspecific back pain: a systematic review and critical synthesis. Int Arch Occup Environ Health. 2013;86:119–137.
Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? JAMA. 2010;303:1295–1302.
Mallen CD, Peat G, Thomas E, et al. Prognostic factors for musculoskeletal pain in primary care: a systematic review. Br J Gen Pract. 2007;57:655–661.
Main CJ, Phillips CJ, Watson PJ. Secondary prevention in health care and occupational settings in musculoskeletal conditions focusing on low back pain. In: Schultz IZ, Gatchel RJ, editors. Handbook of complex occupational disability claims: early risk identification, intervention and prevention. New York: Springer; 2005. p. 387–404.
Jellema P, van der Windt DA, van der Horst HE, Blankenstein AH, Bouter LM, Stalman WAB. Why is a treatment aimed at psychosocial factors not effective in patients with (sub)acute low back pain? Pain. 2005;118:350–359.
Nicholas MK, Linton SJ, Watson PJ, Main CJ. The early identification and management of psychological risk factors (Yellow Flags) in patients with low back pain: a reappraisal. Phys Ther. 2011;91:737–753.
Sullivan MJL, Feuerstein M, Gatchel R, Linton SJ, Pransky G. Integrating psychosocial and behavioral interventions to achieve optimal rehabilitation outcomes. J Occup Rehabil. 2005;15:457–489.
Franche R-L, Baril R, Shaw W, Nicholas MK, Loisel P. Workplace-based return-to-work interventions: optimizing the role of stakeholders in implementation and research. J Occup Rehabil. 2005;15(4):525–542.
Pransky G, Fassie J-B, Besen E, Blanck P, Ekberg K, Feuerstein M, Munir F. The Hopkinton conference working group on workplace disability prevention. Sustaining work participation across the life course. J Occup Rehabil. 2016;26:465–479.
McCluskey S, Burton AK, Main CJ. The implementation of occupational health guidelines principles for reducing sickness absence due to musculoskeletal disorders. Occup Med. 2006;56:237–242.
Cullen KL, Irvin E, Collie A, Clay F, Gensby U, Jennings PA, et al. Effectiveness of workplace interventions in return-to-work for musculoskeletal, pain-related and mental health conditions: an update of the evidence and messages for practitioners. J Occup Rehabil. 2018;28:1–15.
Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Mental Health Serv Res. 2011;38:4–23.
Main CJ, Shaw WS, Tetrick LE, Ehrhart MG, Pransky G. Implementation science and employer disability practices: embedding implementation factors in research designs. J Occup Rehabil. 2016;26:448–464.
Pearce G, McGarity A, Nicholas MK, Linton SJ, Peat J. Better outcomes in worker’s compensation through very early selective intervention. Paper presented at: 2008 Combined Conference of the Australasian Faculty of Rehabilitation Medicine and the Australasian Faculty of Occupational and Environmental Medicine; Adelaide, Australia; May, 2008.
WorkCover NSW. Improving outcomes: Integrated, active management of workers with soft tissue injury (2008). Work Cover website: www.workcover.nsw.gov.au.
Balderson BHK, Von Korff M. The stepped care approach to chronic back pain. In: Linton SJ, editor. New avenues for the prevention of chronic musculoskeletal pain and disability, vol. 1. Amsterdam: Elsevier; 2002. p. 237–243.
Linton SL, Nicholas MK, MacDonald S. Development of a short form of the Örebro Musculoskeletal Pain Screening Questionnaire. Spine. 2012;36:1891–1895.
Nicholas MK, Costa DSJ, Linton SJ, Main CJ, Shaw W, Pearce G, et al. Predicting return to work in a heterogeneous sample of recently injured workers using the brief ÖMPSQ-SF. J Occup Rehabil. 2018;29:295–302.
Myhre K, Marchand GH, Leivseth G, Keller A, Bautz-Holter E, Sandvik L, et al. The effect of work-focused rehabilitation among patients with neck and back pain: a randomized controlled trial. Spine. 2014;39:1999–2006.
Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335–343.
Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med. 1994;23(2):129–138.
Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. 2007;11:153–163.
Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7:524–532.
Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain. 2015;156:1003–1007.
Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75(4):800–802.
Linton SJ, Nicholas MK, Shaw W. Why wait to address high-risk cases of acute low back pain? A comparison of stepped, stratified, and matched care. Pain. 2018;159:2437–2441.
Åsenlöf P, Denison E, Lindberg P. Individually tailored treatment targeting activity, motor behavior, and cognition reduces pain-related disability: a randomized controlled trial in patients with musculoskeletal pain. J Pain. 2005;6(9):588–603.
Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. Br Med J. 2000;321:684–686.
Medical Research Council (2009). Developing and evaluating complex interventions: new guidance. www.mrc.ac.uk/complexinterventionsguidance.
van Oostrom SH, van Oostrom W, van Mechelen BT, de Vet HCW, Knol DL, Anema JR. A workplace intervention for sick-listed employees with distress: results of a randomised controlled trial. Occup Environ Med. 2010. https://doi.org/10.1136/oem.2009.050849.
Whitfill T, Haggard R, Bierner SM, Pransky G, Hassett RG, Gatchel RJ. Early intervention options for acute low back pain patients: a randomized clinical trial with one-year follow-up outcomes. J Occup Rehabil. 2010;20:256–263.
Main CJ, Sullivan MJL, Watson PJ, Greasley K. Pain and work: organizational perspectives. In: Main C, Sullivan MJL, Watson P, editors. Pain management: practical applications of the biopsychosocial perspective in clinical and occupational settings. 2nd ed. Edinburgh: Churchill Livingstone; 2008. p. 391–669.
Harbeck RV, Leahy MJ, Hunt HA, Fong C, Welch EM. Employer factors related to workers’ compensation claims and disability management. Rehabil Counsel Bull. 1991;34:210–226.
Social Research Centre. The cost of work-related injury and illness for australian employers, workers and the community: 2012–13. Canberra: Safe Work Australia; 2015.
Acknowledgements
This study was supported by a Grant from the NSW Ministry of Health, EML Insurance, and SI-CORP (now icare). We would like to specifically acknowledge the contributions to the study by Karen Munk, Tamara Sprod, Rachel Elmes, Claims managers and staff at EML; Robert Lloyd, Susan Rafty, and Steven Hunt at icare; Michele Murphy and John Roach from NSWHealth, and the CEO’s, General Managers, and RTW coordinators at each participating hospital, as well as the Occupational Physicians and Dr Rob Borland, University of Sydney, who provided independent advice. We also thank the injured workers who voluntarily participated, and the helpful feedback on earlier drafts of this manuscript from Glen Pransky, Ian Cameron, Chris Maher, Alex Collie, and Amanda Williams.
Funding
This study was supported by a Grant from the NSW Ministry of Health, EML Insurance, and SI-CORP (now icare). The Grant funding supported only the work performed by the two project managers (Michael Gleeson, and Raphael Z Pinto).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was approved by the Sydney Local Health District Human Research Ethics Committee at Concord Hospital (17/06/2013), and the Human Research Ethics Committees of each participating hospital. The study was registered prospectively with the Australian and New Zealand Clinical Trials Registry (# ACTRN12613000847718). The system regulator, WorkCover(NSW), also gave its written approval for the protocol employed in the study.
Additional information
We would like to dedicate this paper to the memory of Dr Garry Pearce who played a critical role in the establishment and conduct of the study but died before the paper was completed.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The typo in the co-author name has been corrected.
Rights and permissions
About this article
Cite this article
Nicholas, M.K., Costa, D.S.J., Linton, S.J. et al. Implementation of Early Intervention Protocol in Australia for ‘High Risk’ Injured Workers is Associated with Fewer Lost Work Days Over 2 Years Than Usual (Stepped) Care. J Occup Rehabil 30, 93–104 (2020). https://doi.org/10.1007/s10926-019-09849-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-019-09849-y