Abstract
Purpose Ability to return to work (RTW) after stroke has been shown to have positive psychosocial benefits on survivors. Although one-fifth of aneurysmal subarachnoid hemorrhage (aSAH) survivors suffer from poor psychosocial outcomes, the relationship between such outcomes and RTW post-stroke is not clear. This project explores the relationship between age, gender, race, marital status, anxiety and depression and RTW 3 and 12 months post-aSAH. Methods Demographic and clinical variables were collected from the electronic medical record at the time of aSAH admission. Anxiety and depression were assessed at 3 and 12 months post-aSAH using the State Trait Anxiety Inventory (STAI) and Beck’s Depression Inventory-II (BDI-II) in 121 subjects. RTW for previously employed patients was dichotomized into yes/no at their 3 or 12 month follow-up appointment. Results Older age was significantly associated with failure to RTW at 3 and 12 months post-aSAH (p = 0.003 and 0.011, respectively). Female gender showed a trending but nonsignificant relationship with RTW at 12 months (p = 0.081). High scores of depression, State anxiety, and Trait anxiety all had significant associations with failure to RTW 12 months post-aSAH (0.007 ≤ p ≤ 0.048). At 3 months, there was a significant interaction between older age and high State or Trait anxiety with failure to RTW 12 months post-aSAH (p = 0.025, 0.042 respectively). Conclusions Patients who are older and suffer from poor psychological outcomes are at an increased risk of failing to RTW 1-year post-aSAH. Our interactive results give us information about which patients should be streamlined for therapy to target their psychosocial needs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aneurysmal subarachnoid hemorrhage (aSAH) is a devastating stroke that is estimated to affect around 20 people per 100,000 every year in the United States [1]. Most occur between ages 40 and 60, but young children and the elderly are not immune [2, 3] The event itself is often fatal: the case fatality rate of aSAH is 50%, and one in eight victims die outside of the hospital [4]. If victims survive, one in five will suffer poor long-term psychological consequences, including anxiety and depression [5] The ability to return to work after stroke can have profound positive psychosocial benefits long-term, including increased expression of self-efficacy and motivation [6].
In addition to boosting self-efficacy and motivation, returning to work after aSAH has been shown to mitigate a large portion of the economic cost. When analyzing the economic impact, aSAH costs more than other types of stroke, including intracranial hemorrhage (ICH) or ischemic stroke. Average Medicare expenditures from the time of the initial event to four years post-stroke (including both inpatient and outpatient costs) were $48,327 for aSAH, $38,023 for ICH, and $39,396 for ischemic stroke [7]. The higher cost for aSAH patients is mainly due to higher direct costs (prescriptions, hospital stay, etc.). Increased indirect costs, although not included in these numbers, are also higher in the aSAH population. One indirect cost is the loss of work productivity. The combination of a typically younger age and higher morbidity rates means that the aSAH population is often unprepared or unable to retire while also being physically and cognitively incapable of returning to work. Therefore, their work productivity rates are much lower than other comparable stroke populations [7, 8].
Identifying the factors that influence ability to return to work post-aSAH will inform interventions that can help mitigate some of the negative impact of aSAH. Relevant literature suggests that the poor psychosocial outcomes that many aSAH survivors face post-stroke, such as anxiety and depression, can potentially impact ability to return to work. The evidence, however, is mixed [9]. While most studies found a significant relationship between depression and failure to return to work post-aSAH [5, 10, 11] others found no clear relationship between these variables [12, 13]. The literature also suggests a mixed relationship between anxiety and return to work post-aSAH [13, 14] Age and gender, while studied more extensively, also show mixed evidence in terms of their relation to return to work and quality of life post-aSAH [12, 15,16,17] Race has also not been explored as a possible factor that can influence return to work post-stroke.
Furthermore, the existing literature has shown that non-standardized instrumentation could be contributing to this lack of definitive evidence [9]. Therefore, we seek here to characterize the relationship between depression, anxiety, age, race, gender, and marital status related to return to work post-aSAH using the well accepted and standardized measuring tools of the Beck’s Depression Inventory (BDI-II) and the State-Trait Anxiety Inventory (STAI). Exploring these relationships with valid and reliable instrumentation, as well as with clinical and demographic data, will help guide the rehabilitation process for aSAH patients and clinicians by allowing the identification of patients at higher risk for failure to return to work. Healthcare professionals can therefore streamline patients for counseling and other therapeutic services, helping to increase the psychosocial wellbeing of survivors [6], and to decrease some of the economic impact of aSAH.
Methods
Research Subjects
This work constitutes a secondary data analysis of a NIH funded parent study on aSAH patients recruited through the Neurovascular Intensive Care Unit at the University of Pittsburgh Medical Center. The patient or legal proxy signed an informed consent form for the use of their data, and all procedures were in accordance with the ethical standards of the institutional research board and with the 1964 Helsinki declaration. The datasets analyzed during the current study are available from the authors on reasonable request, and upon acceptable application to the data management board from the parent study.
Patients were included in the parent study if they were (1) newly diagnosed with aSAH verified via cerebral angiogram, (2) had a Hunt and Hess grade > 3 (reflecting the presence of neurologic deficit and change in the level of consciousness at the time of hemorrhagic event) and/or Fisher grade > 2 (reflecting the presence of subarachnoid hemorrhage of at least 1 millimeter on CT scan), (3) were over 18 years old, (4) were able to read/speak English, and (5) had no prior history of neurological disorders. Patients were excluded from this secondary data analysis if they reported pre-morbid depression or anxiety. The retrospective aspect of the study limits the ability to discuss referrals of severely depressed patients who may have expressed suicidal ideation. Patients were included in this current analysis if they were administered the Work Limits Questionnaire at their 3 and/or 12 month follow-up appointment. Only patients who were previously employed were administered this questionnaire.
Measures
The demographic variables of age, race, gender, and marital status at the time of stroke were obtained from the patient, proxy, or electronic medical record. Age was calculated at the time of aSAH and reported as years and fractional years. Race was self- or proxy-report and categorized as Caucasian, African-American, Pacific Islander, and Asian. Marital status was dichotomized into married or not married, which then encompassed patients who were single, divorced, and widowed. The category of co-habitation was not included in the parent study. All participants fell into one of these categories of marital status, and only 4 out of the 121 patients included in analysis changed marital status over the course of 1-year follow-up.
As a part of the parent study, subjects were followed for 12 months post-aSAH. During face-to-face follow-up interviews at 3 and 12 months, subjects were asked if they returned to work or not. This information was dichotomized into return to work or not, and this binary variable was used as the outcome measure for this project.
Anxiety was measured using the State-Trait Anxiety Interview (STAI) at 3 and 12 months. The STAI measures both State (anxiety related to a situation), and Trait anxiety (anxiety as a part of an individual’s personality). Scores range from 20 to 80, and higher scores reveal greater anxiety. Evidence suggests that STAI is considerably reliable in any population with internal consistency coefficients of 0.94 and 0.93 for multiple sclerosis patients [18]. Moreover, considerable evidence attests to the validity of the STAI as a measure of both State and Trait anxiety (for an in depth discussion on this topic, see [19]).
In a similar fashion, the Beck’s Depression Inventory II (BDI-II) was used to measure depressive symptoms at 3 and 12 months post-aSAH. Scores on this test range from 0 to 83 with higher scores indicating more severe depression. This assessment tool is known to be highly reliable, with internal consistency coefficients ranging from 0.79 to 0.90 and a test–retest correlation of 0.72 across 20 studies [20, 21].
Statistical Analysis
Bivariate associations between each individual demographic and psychosocial variable with the outcome of return to work were first assessed independently. The categorical variables—gender and race—were analyzed using chi-squares or Fisher’s exact test, while continuous variables including age, BDI-II, State and Trait anxiety scores were analyzed using independent t tests. Statistical significance was set at an alpha of < 0.05. A multiple binary regression model was then performed controlling for all covariates, including age, gender, race, and marital status. These demographics were chosen as covariates based on their significance in preliminary analysis. The interaction between relevant variables was included in regression analysis. Two types of analyses were performed. Adjusted analyses included adjustment for the covariates above. Unadjusted analyses did not allow adjustment for these variables. Trending significance was set at an alpha of < 0.10. SPSS Statistics for Windows, Version 24.0 (Armonk, NY) was used for all data analysis.
Results
Descriptive Statistics
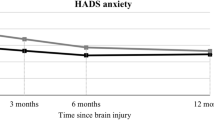
The average age of subjects (N = 121) was 53.92 years (SD ± 11.16), and the majority were female (71.1%), Caucasian (91.7%), and married (67.8%), which represents the average demographics of the greater Pittsburgh aSAH population (Table 1). In order to be included in this analysis, all subjects had to have complete data with both 3 and 12 month time points for BDI-II, STAI, and a binary measure of return to work. Average BDI-II score at 3 months was 7.54 (SD ± 6.66) and 8.12 (SD ± 6.54) at 12 months. A score of 20 or higher on the BDI-II scale indicates risk for moderate to severe depression. State anxiety averaged 34.24 (SD ± 12.09) at 3 months and 34.40 (SD ± 12.95) at 12 months, whereas Trait anxiety had a mean of 34.16 (SD ± 10.83) at 3 months and a mean of 31.19 (SD ± 11.98) at 12 months. A score of 40 or higher on the STAI scale indicates moderate to high anxiety. In our sample, 80 subjects reported a return to work at 3 months, while 82 subjects reported a return to work at 12 months.
Psychosocial Analyses
Scores of BDI-II, State anxiety, and Trait anxiety were highly correlated at 3 and 12 months post-aSAH (Table 2). Therefore, these measures could not be run together in multiple regression analysis.
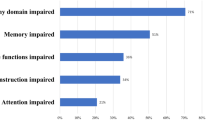
When analyzed as a continuous variable, older age was a significant predictor of failure to return to work at 3 (p = 0.003) and 12 months post-aSAH (p = 0.011; Table 3). But this does not give information on whether there were critical time points that may be skewing the data (for instance, around typical retirement age). To further investigate the relationship between age and ability to return to work, age was categorized into 5-year intervals and the percent chance of returning to work in each category was calculated (Figs. 1 and 2). As suspected, higher age categories were significantly associated with higher percent chance of not returning to work. For example, the age group of 61–65 had a 90% chance of not returning to work, whereas patients who were 51–55 had a 57% chance of not returning to work 3 months post-aSAH. However, we did not find that there was a particular critical period cut-point for a failure to return to work.
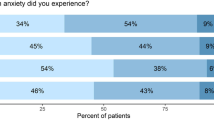
Even after controlling for the covariates of race and martial status, higher scores of depression, State anxiety and Trait anxiety at 3 and 12 months were all significant independent predictors of failure to return to work at 12 months post-aSAH (0.007 ≤ p ≤ 0.048). Female gender only showed a trending association with failure to return to work at 12 months post-aSAH (p = 0.081; Table 3).
Interactions
The interactions between older age and high 3-month State anxiety, older age and high 3-month Trait anxiety, older age and high 12-month Trait anxiety all significantly predicted failure to return to work 12-months post-aSAH (p = 0.025, 0.045, and 0.017, respectively; Table 4). Moreover, the relationships between failure to return to work 12 months post-aSAH and older age and high 3-month BDI-II, older age and high 12-month BDI-II, and older age and high 12-month State anxiety all trended toward statistical significance (p = 0.052, 0.077, and 0.052, respectively).
Discussion
The findings of this study demonstrate that the ability to return to work can be significantly impacted by demographic and psychosocial variables post-aSAH. Older age, female gender, and higher scores on the BDI-II, and STAI were all associated with failure to return to work 3–12 months post-aSAH. Interactions amongst these variables (such as between age and 3-month State anxiety) demonstrated significant associations with return to work 3 and 12 months post hemorrhagic stroke. These results demonstrate some of the characteristics exhibited by patients that are at risk for failing to return to work, as all of these show a significant association with return to work. We have selected the demographic parameters based upon previous literature on the topic, so these associations were not surprising. But the psychosocial parameters that we investigated had not yet been explored in the context of aSAH, and so these associations were a bit more novel. They were even more interesting when interactive relationships were considered. Other studies have not yet explored these synergistic relationships between such factors; therefore we feel that our significant results are innovative in their clinical applicability.
When looking at 12-month return to work rates, the interaction between older age and higher rates of 3 or 12 month BDI-II, State anxiety, or Trait anxiety all were significant or trending predictors of failure to return to work. In other words, older patients who suffer from moderate to severe depression or anxiety have a high likelihood of failing to return to work at 1-year post-aSAH. This result agrees with previous data considering a variety of illnesses, which also found these same factors to be true [22].
Older age alone was also a significant predictor of failure to return to work 3 and 12 months post-aSAH. This is similar to studies by Carter and Czapiga which described a similar trend [15, 16]. While proximity to retirement age could be the simplest and most obvious reason for this trend, other factors such as increased comorbidities and age-related cognitive changes still need consideration as potential influencing factors.
Female gender has been shown to be significantly associated with failure to return to work following a variety of illnesses, including heart disease [22, 23]. This finding has been postulated to be a result of societal expectations. But these associations could also be confounded by higher rates of depression seen in female patients, which may impair returning to work [24].
In our sample, we only found gender to be a trending predictor of failure to return to work. It is not clear whether these results could simply be attributable to the high portion of female subjects in this sample (71%, which is typical for the aSAH clinical population) or whether this is a true finding. In our analysis of the interactive effect of female gender and marital status, married women were not significantly more likely to fail to return to work than non-married women.
In all adjusted analysis, higher rates of depression at 3 and 12 months significantly predicted a failure to return to work 3 and 12 months post-aSAH. High BDI-II scores 3 months post-aSAH had a trending association with failure to return to work 12 months post hemorrhagic stroke in unadjusted analysis. This is in agreement with other studies that found that depression and anxiety are significantly associated with failure to return to work for these patients [5, 11]. The reduced motivation, poor self-care, and low productivity associated with severe depression make sense as possible reasons why depressed patients are less likely to return to work post hemorrhagic stroke. Symptoms of anxiety such as racing thoughts, fear, poor concentration, and fatigue could also impede a return to work. Furthermore, Trait anxiety 3 and 12 months post-aSAH was significantly associated with a failure to return to work 12 months post hemorrhagic stroke in adjusted analysis. This builds on the finding that anxious patients are less likely to return to work 1 year post hemorrhagic stroke. Quinn et al. also found that people who were unable to return to work 12 months post hemorrhagic stroke were more likely diagnosable or borderline for a Wimbledon Self-Report Scale mood disorder (measure of both depression and anxiety) 12 months post-stroke [17].
State anxiety at 3 and 12 months is a significant predictor of failure to return to work 12 months post-aSAH in adjusted analysis. Additionally, high State anxiety at 3 months is also significantly associated with failure to return to work 12 months post-aSAH in unadjusted analysis. When considering the recovery trajectory over a whole year’s time, high levels of State anxiety experienced 3 months post-stroke still significantly affect a patient’s ability to return to work 12 months later. We interpret this to mean that those who are anxious in relation to their health condition are less likely to return to work. It is possible that these individuals may not want to add any perceived stresses of employment again, and so this phenomenon carries through to result in less likelihood of a return to work at both 3 and 12 months’ post-aSAH. In contrast, those individuals that are more anxious as a general personality trait are only less likely to return to work at 3 months’ post-aSAH, and so their anxiety may be less related to the effect that employment stress has on their helath. This has been previously described in a study by Vilkki which found that moderate to severe anxiety was associated with lower employment levels as far out as 10 years post-aSAH [14]. Anxious patients are therefore at a severe risk of inability to return to work for a long period of time after physical recovery. As healthcare providers, recommending potential resources for therapeutic support (i.e. stroke support groups) and/or stressing the significance of therapeutic coping mechanisms could help these patients.
The high correlation between depressive symptoms, State anxiety, and Trait anxiety, suggests that these psychosocial variables are not independent but highly linked. These results show that patients who are anxious are likely to also be depressed and vice versa. Furthermore, any of these psychosocial or mood disorder disturbances affect one’s likelihood of returning to work. Therefore, it is appropriate that healthcare professionals looking to refer for therapy screen for both anxiety and depression in aSAH survivors even if patients are only exhibiting signs for one or the other. Early screening and intervention for these poor psychosocial outcomes could in turn further increase rates of return to work.
This research is subject to certain limitations. The small sample size of our study in comparison to other relevant literature limits our generalizability. However, we did collect a broad variety of data for these subjects, which allowed novel interactive findings for this group despite the small sample size.
Despite this breadth of data, certain variables that could be influential were still not captured. Physical functional outcome measures (such as Glasgow Outcome Scale, or Modified Rankin Scale scores) were not available for the majority of our subjects. This creates a potential confound as those that are severely physically impaired may not be able to maintain employment in any capacity. Prospective study designs should include such measures.
Another variable that could not be fully analyzed was household income data. Again, this data was not available for all subjects, and so we were sharply limited to analyze its full influence on return to work. This factor has not been explored in previous literature and we hypothesize that it could be a significant push to return to work, as well as a reason that a return to work is not imperative. Future studies that gather income data should consider both the evaluation of the income level of the aSAH patient, as well as the percentage that the income earned by the patient contributed to the total household income. This would give a better index of family income dependence as a modifying variable for return to work post-aSAH.
Future work should also consider the influence of complex familial relationships. While we analyzed marital status as a binary variable in this project (married or not married, which included single, divorced, and widowed individuals), the parent study did not include data on cohabitation, which would likely reveal strong support systems in place for those individuals. The need to care for children and parents was not considered in this study as a potential reason why some patients may decide not to return to work. Cultural and racial differences in the influence of these types of variables should also be considered, as these could similarly impact return to work.
This study provides clinicians with insight into patient who are at higher risk for failing to return to work after aSAH. Patients who are older and display symptoms of depression and/or anxiety, should be streamlined for therapy that targets their psychosocial needs. Through such dedicated care aSAH patients may be able to return to a higher quality of life for years after their hemorrhagic stroke.
References
Ziemba-Davis M, Bohnstedt BN, Payner TD, Leipzig TJ, Palmer E, Cohen-Gadol AA. Incidence, epidemiology, and treatment of aneurysmal subarachnoid hemorrhage in 12 midwest communities. J Stroke Cerebrovasc Dis. 2014;23(5):1073–1082.
Jordan LC, Johnston SC, Wu YW, Sidney S, Fullerton HJ. The importance of cerebral aneurysms in childhood hemorrhagic stroke: a population-based study. Stroke 2009;40(2):400–405.
Rinkel GJ, Djibuti M, Algra A, van Gijn J. Prevalence and risk of rupture of intracranial aneurysms: a systematic review. Stroke 1998;29(1):251–256.
van Gijn J, Kerr RS, Rinkel GJ. Subarachnoid haemorrhage. Lancet 2007;369(9558):306–318.
Morris PG, Wilson JT, Dunn L. Anxiety and depression after spontaneous subarachnoid hemorrhage. Neurosurgery 2004;54(1):47–52.
Medin J, Barajas J, Ekberg K. Stroke patients’ experiences of return to work. Disabil Rehabil. 2006;28(17):1051–1060.
Lee WC, Christensen MC, Joshi AV, Pashos CL. Long-term cost of stroke subtypes among Medicare beneficiaries. Cerebrovasc Dis. 2007;23(1):57–65.
Taylor TN, Davis PH, Torner JC, Holmes J, Meyer JW, Jacobson MF. Lifetime cost of stroke in the United States. Stroke 1996;27(9):1459–1466.
Turi E, Conley Y, Stanfill AG. A literature review of psychosocial comorbidities related to working capacity after aneurysmal subarachnoid hemorrhage. J Neurosci Nurs. 2017;49(3):179–184.
Buunk AM, Groen RJ, Veenstra WS, Spikman JM. Leisure and social participation in patients 4–10 years after aneurysmal subarachnoid haemorrhage. Brain Inj. 2015;29(13–14):1589–1596.
Hedlund M, Zetterling M, Ronne-Engstrom E, Carlsson M, Ekselius L. Depression and post-traumatic stress disorder after aneurysmal subarachnoid haemorrhage in relation to lifetime psychiatric morbidity. Br J Neurosurg. 2011;25(6):693–700.
Harris C. Factors influencing return to work after aneurysmal subarachnoid hemorrhage. J Neurosci Nurs. 2014;46(4):207–217.
Powell J, Kitchen N, Heslin J, Greenwood R. Psychosocial outcomes at 18 months after good neurological recovery from aneurysmal subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2004;75(8):1119–1124.
Vilkki J, Juvela S, Malmivaara K, Siironen J, Hernesniemi J. Predictors of work status and quality of life 9–13 years after aneurysmal subarachnoid hemorrahage. Acta Neurochir. 2012;154(8):1437–1446.
Carter BS, Buckley D, Ferraro R, Rordorf G, Ogilvy CS. Factors associated with reintegration to normal living after subarachnoid hemorrhage. Neurosurgery 2000;46(6):1326–1333 (discussion 1333–1334).
Czapiga B, Kozba-Gosztyla M, Czapiga A, Jarmundowicz W, Rosinczuk-Tonderys J, Krautwald-Kowalska M. Recovery and quality of life in patients with ruptured cerebral aneurysms. Rehabil Nurs. 2014;39(5):250–259.
Quinn AC, Bhargava D, Al-Tamimi YZ, Clark MJ, Ross SA, Tennant A. Self-perceived health status following aneurysmal subarachnoid haemorrhage: a cohort study. BMJ Open. 2014;4(4):e003932.
Santangelo G, Sacco R, Siciliano M, Bisecco A, Muzzo G, Docimo R, et al. Anxiety in multiple sclerosis: psychometric properties of the State-Trait Anxiety Inventory. Acta Neurol Scand. 2016;134(6):458–466.
Spielberger C. State-trait anxiety inventory: bibliography. 2nd ed. Washington, DC: Consulting Psychologists Press; 1989.
Smarr KL, Keefer AL. Measures of depression and depressive symptoms: beck depression inventory-II (BDI-II), center for epidemiologic studies depression scale (CES-D), geriatric depression scale (GDS), hospital anxiety and depression scale (HADS), and patient health questionnaire-9 (PHQ-9). Arthritis Care Res. 2011;63(Suppl 11):S454–S466.
Dozois DJA, Covin R. The Beck Depression Inventory-II (BDI-II), Beck Hopelessness Scale (BHS), and Beck Scale for Suicide Ideation (BSS). In: Hilsenroth MJ, Segal DL, Hersen M, editor. Comprehensive handbook of psychological assessment. Hoboken: Wiley; 2004.
Cancelliere C, Donovan J, Stochkendahl MJ, Biscardi M, Ammendolia C, Myburgh C, et al. Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropr Man Therap. 2016;24(1):32.
Dreyer RP, Wang Y, Strait KM, Lorenze NP, D’Onofrio G, Bueno H, et al. Gender differences in the trajectory of recovery in health status among young patients with acute myocardial infarction: results from the variation in recovery: role of gender on outcomes of young AMI patients (VIRGO) study. Circulation 2015;131(22):1971–1980.
Kornstein SG, Schatzberg AF, Thase ME, Yonkers KA, McCullough JP, Keitner GI, et al. Gender differences in chronic major and double depression. J Affect Disord. 2000;60(1):1–11.
Acknowledgements
Funding for this study was received from the National Institutes of Health/National Institute of Nursing Research R01 NR004339 (PI: Sherwood and Poloyac) and T32NR009759-09 (PI: Conley).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Turi, E.R., Conley, Y., Crago, E. et al. Psychosocial Comorbidities Related to Return to Work Rates Following Aneurysmal Subarachnoid Hemorrhage. J Occup Rehabil 29, 205–211 (2019). https://doi.org/10.1007/s10926-018-9780-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-018-9780-z