Abstract
Objectives This study aimed to determine whether a multi-faceted model of management of work related musculoskeletal disorders reduced compensation claim costs and days of compensation for injured workers. Methods An intervention including early reporting, employee centred case management and removal of barriers to return to work was instituted in 16 selected companies with a combined remuneration over $337 million. Outcomes were evaluated by an administrative dataset from the Victorian WorkCover Authority database. A ‘quasi experimental’ pre–post design was employed with 492 matched companies without the intervention used as a control group and an average of 21 months of post-intervention follow-up. Primary outcomes were average number of days of compensation and average cost of claims. Secondary outcomes were total medical costs and weekly benefits paid. Results Information on 3,312 claims was analysed. In companies where the intervention was introduced the average cost of claims was reduced from $6,019 to $3,913 (estimated difference $2,329, 95 % CI $1,318–$3,340) and the number of days of compensation decreased from 33.5 to 14.1 (HR 0.77, 95 % CI 0.67–0.88). Medical costs and weekly benefits costs were also lower after the intervention (p < 0.05). Reduction in claims costs were noted across industry types, injury location and most employer sizes. Conclusions The model of claims management investigated was effective in reducing the number of days of compensation, total claim costs, total medical costs and the amount paid in weekly benefits. Further research should investigate whether the intervention improves non-financial outcomes in the return to work process.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Work disability due to musculoskeletal disorders (MSD) has both a personal and economical impact for all stakeholders. From an employer point of view MSD leads to lost production time and increased compensation premiums [1]. From an employee point of view MSD results in pain and disability [1]. If disability due to MSD persists, a worker can experience depression, loss of self-esteem and a decreased quality of life [2, 3], while an employer faces additional costs and a loss of profitability [1]. In Victoria, Australia, if the MSD arises from or is exacerbated by work, the worker is eligible for compensation under the Victorian WorkCover Authority (VWA) insurance scheme, regardless of fault. Musculoskeletal injuries represent the greatest proportion of VWA claims in Victoria, Australia, representing over 50 % of all claims made in the 2006/2007 financial year [4]. Prior studies have shown that not all lost days due to musculoskeletal disorders are necessary or even beneficial to rehabilitation efforts [5]; thus proactive return-to-work programs that lend assistance and provide temporary job modification to affected workers may ultimately offer greater profitability for employers. For employees an earlier return to work is likely to avoid some of the negative consequences associated with work disability.
The required elements of optimal management of MSD-related claims continues to be debated. The introduction of a continuum of care model (a consistent, evidence-based approach) for soft tissue injuries in Canada led to significant cost savings and improved return to work outcomes across an entire jurisdiction [6]. Case management can improve work outcomes when it is applied early, as demonstrated in the US [7], Sweden [8] and the Netherlands [9], and can increase motivation for return to work [10]. It appears that applying a consistent, evidence-based approach within an integrated case-management framework would be an appropriate and effective model for the management of musculoskeletal injuries in the state of Victoria, Australia.
Return to work is an important process in the recovery from injury [11]. While the measurement of return to work is in itself quite complex [12, 13], the consequences of being unable to work due to injury stretch beyond financial implications. The health consequences of being unable to work include a greater risk of poor mental and physical health [14] as well as reduced social and recreational activities [12]. Since the health benefits of being able to work have been well established [15]; how long a worker is absent from work after an injury is an important indicator of the management of MSD. Appropriate management is likely to reduce or even eliminate unnecessary days of lost work and facilitate early return to suitable work duties [16].
Return to work is a complex outcome that is difficult to measure [11–13]. For many workers the end of paid compensation approximates return to work, but compensation may continue beyond a first return to work and pain or disability may still persist [12]. Administrative databases tend to consist of data that is easy to collect, and the VWA collects data on each worker’s compensation claim in the state of Victoria, Australia. The analysis of this database may be useful to determine the effectiveness of a range of interventions on workers compensation outcomes.
The aim of this study was to evaluate a comprehensive approach to management of MSD related claims to determine whether this model of management reduced compensation claim costs and days of compensation for workers.
Materials and Methods
Setting
When a worker in Victoria, Australia, sustains an MSD “out of or in the course of any employment” [17], they are eligible for compensation under the VWA compensation scheme. Under Victorian law all employers must take out injury insurance, with the premium calculated according to industry size, industry sector and past performance in dealing with compensation claims [18]. The insurer determines whether a claim is accepted according to interpretation of legislation [17]. Once a claim is accepted, compensation covers medical, rehabilitation and wage replacement costs. Compensation covers all reasonable medical costs and a proportion of the injured worker’s average weekly earnings. Wage replacement ceases when the worker earns more than the amount they are being compensated, or they are assessed as fit for normal duties. In a small number wage replacement is stopped if the worker is considered not to be complying with rehabilitation. Wage replacement may continue until retirement age if the worker’s capacity remains very restricted and is unlikely to change. Treatment costs are generally covered up to one year after wage replacement ceases. The insurer determines when a claim can closed based on interpretation of legislation [17], the worker’s capacity to work and the likelihood that capacity may change [18].
Employers in Victoria are responsible for the management of injuries in the workplace, including appointing a return to work coordinator and development of a return to work plan for an injured worker. It is the role of the return to work coordinator to assist the worker return to work as soon as possible, including liaising with managers, treating practitioners and the insurer. VWA has established a list of competencies for return to work coordinators [18] and provides 2 day training courses and a range of resources to support Return To Work Coordinators. RTW Coordinators have a highly variable level of training and experience. The return to work coordinator may be appointed just for the duration of the return to work process, or in the case of employers with a remuneration of greater than $2 million, the return to work coordinator is required to be a permanent role within the company. Depending on the employer size and past history in managing claims, they may also be required to develop an occupational rehabilitation program for their workers. Despite the legal requirement for and support provided to return to work coordinators, there is the potential for a wide range of attitudes and responses to work injuries, dependent on the employer and the resources available to devote to work injury management.
Good work injury practices are encouraged through two mechanisms. The first is the past experience rating used to determine the premium the employer pays for injury insurance. Employers with a poor history of injury claims pay a higher premium. The second is that earlier return to work will lead to lower costs for the employer, as the employer is required to pay the first 10 days of compensation and the first $450 of medical costs for an injured worker [18]. As a result, ensuring efficient work injury management has clear benefits for the employer in terms of direct costs and insurance premium costs. Rising costs and maintaining productivity are also likely to be strong drivers for employers to improve their work injury practices.
Description of the Intervention
The intervention was applied at company level with the aim of addressing the post work injury practices within a workplace. The intervention model was a multifaceted approach based on principles of early appropriate intervention, proactive management of the return to work process and supporting the worker (Table 1). The case companies engaged the intervention provider through a commercial contract and paid a monthly fee to employ the intervention. There was no performance based payment made to the intervention company, although renewal of the contract acted as an incentive for the intervention company to improve return to work outcomes. The monthly fee varied depending on the size of the case company.
Early Appropriate Medical Intervention
The intervention consisted of a 24-h telephone contact line manned by trained injury managers to provide immediate professional assistance and encourage early reporting of a workplace injury. The aim was to receive notification within 20–60 min of the injury, with longer than 24 h considered a delayed injury report. The worker was able to seek care from their usual medical practitioner, or offered medical care at a local preferred medical clinic. Preferred allied health and medical specialists were also utilised. The aim was to shorten waiting times for appropriate procedures in order to encourage return to work with the assignment of suitable duties.
Workplace Intervention
Once an injury was reported, an injury manager was assigned to manage the process and guide the employee, employer and other parties throughout the course of return to work. The injury manager aimed to facilitate contact between the key parties involved in the rehabilitation and return to work of the injured worker. The supervisor/line manager was involved in the process from the outset and if necessary senior management was engaged to assist resolution of difficulties, predominantly when appropriate alternative duties and support for the worker were not being provided. Furthermore, contact with Human Resources within the company allowed non work-injury issues to be addressed.
The injury manager’s role was to foster a relationship of respect and care between employers and employees in order to improve recovery time, reduce instances of litigation and facilitate early return to work.
The intervention aimed to have a positive impact on the work injury culture within the work place. This included addressing any negative connotations of an injury at work, and encouraging a positive attitude towards rehabilitation and re-integration of the worker. This was performed in a consistent, systematic fashion via monthly meetings and discussion with supervisors about specific cases, informal education and some specific supervisor training sessions. Senior manager input was sought, and generally provided. Senior managers were involved through feedback and reporting, through individual cases (for example the CEO contacting the worker to check on their wellbeing), dealing with recalcitrant managers, and leading their organisation in the principles of the program.
Support for the Worker
The injury manager had regular communication with the worker as a professional who understood the work injury system and the anticipated outcomes. The injury manager provided a supportive focus on the worker’s condition, including psychosocial advice and reassurance where necessary (for example to address fear avoidance of activity for back pain). Contact may have been limited to one or two phone calls in simple instances, or occurred over many months for more complex cases. Regardless of complexity, the injury manager worked to remove as many barriers as possible to the successful management of the person’s injury and return to work. Injury managers encouraged the worker to obtain evidence based treatment and cease ineffective treatments, and worked with their health practitioners to achieve this. The injury manager also worked with the treating doctor to avoid delays in specialist referrals, and delays in insurer approval for treatment such as surgery.
Claims Management
The injury manager liaised with the claims manager within the insurer setting. In occasional cases where the case manager had concerns about worker cooperation, claims management strategies such as an independent medical review were used as an additional strategy.
Injury Managers
Injury managers managed cases by telephone contact, or directly at the workplace through a regular time commitment at the workplace. Injury managers were selected on their communication skills, and ability to project manage. Injury management software assisted with timely management of case management actions and streamlined electronic communication. The injury manager’s role could be considered similar to the stated role of a return to work coordinator. However, the high level of specific training and the consistent application of all processes were intended to enable injury managers to perform these responsibilities at a higher level. The injury manager was an employee of the intervention company, and was authorised by the worker to communicate with different parties regarding the worker’s situation. Standard practices applied regarding medical confidentiality. Issues such as diagnosis, work capacity and restrictions, treatment and investigations are documented on certificates and are not considered medically confidential, but were dealt with sensitively.
Dataset
An administrative dataset was extracted from the main VWA database to gather information regarding companies who had undertaken the intervention and companies maintaining usual work injury practices. A ‘quasi experimental’ pre–post design with historical and concurrent controls was employed (Fig. 1).
The intervention companies had engaged the providers of the intervention in order to reduce costs associated with work injuries and improve work injury practices within their organisation. Data was gathered from these companies from the beginning of the intervention up to March 2004 (post implementation period). Information was then gathered for the same company for the same length of time before the intervention was applied (pre implementation period). For example, if the intervention had been in place for 24 months before March 2004, data was gathered for the 24 months preceding the intervention (i.e. the post intervention period spanned from March 2002 to March 2004 and the pre implementation period spanned from March 2000 to March 2002). The intervention had been in place for an average of 21 months across the 16 intervention companies. All companies that received the intervention were included in this study.
Data was also extracted from 492 control companies matched to the intervention companies for employer size and industry sector to serve as a concurrent control group. Claim information was gathered from January 1999 to December 2001 (pre implementation period) and from January 2002 to March 2004 (post implementation period). The pre implementation data collection period was longer than the post implementation for control companies; however the average number of claims per month across both periods was similar. The data was extracted from the main VWA database using an algorithm to capture approximately three control claims for each intervention claim, matched for industry sector and employer size.
This allowed three comparisons to determine the effectiveness of the intervention (Fig. 1). The primary analysis compared the intervention companies’ claims before and after the intervention to determine whether the intervention had an impact on outcomes. Two further comparisons were made using information from the control companies. First the data for the pre intervention period was compared to determine whether any baseline differences existed between the intervention and control companies. Second, the data from control companies for the pre implementation period and post implementation period were compared to determine whether any changes occurred over time without the intervention to rule out secular changes as an explanation for any observed differences.
Variables gathered included employer remuneration (an indication of employer size), industry sector, mechanism of injury, injury location, gender, claim costs (including medical, allied health, benefit and legal costs) and the number of days of compensation. Given that the first 10 days of compensation and first $450 of medical costs were paid by the employer in the VWA system, for a day of compensation to appear in the database, the employer had already paid for 10 days of compensation. Similarly, a cost appearing in the database had exceeded $450. Therefore it was possible to accrue claim costs without registering any days of compensation; any paid lost days of work meant that at least 10 days of work absence had occurred.
Outcomes
Primary Outcomes
The primary outcomes were the average number of days of compensation paid and the average cost of claims. The number of days of compensation was used a proxy for the time taken to return to work. The total cost of claim was made up of the sum of all recorded costs, including costs resulting from treatment, wage benefits and lump sum compensation payments. An effective intervention would lead to a reduced number of days of compensation paid and reduced total claim costs.
Secondary Outcomes
Secondary outcomes were the total medical costs and weekly benefits paid. Total medical costs were made up of the costs incurred through treatment by doctors, at hospital, or allied health and other rehabilitation costs. The weekly benefits paid was the amount attributed to wage replacement costs. An effective intervention would reduce both these costs.
Analysis
Descriptive statistics were calculated for both the intervention and control companies. To determine the impact of the intervention on the number of days of compensation, survival analysis was conducted using Kaplan–Meier curves and Cox regression analysis [19]. Kaplan–Meier curves were used to describe the end of compensation payments for intervention and control companies with data censored at 365 days of compensation. The initial model tested included all potentially confounding variables (employer remuneration, industry type, injury code, mechanism and location, and gender); however this model later was trimmed to only include variables significantly contributing to the model. The magnitude of the intervention’s effect for the intervention companies pre and post implementation was adjusted after controlling for potential confounders in the Cox regression analysis and hazard ratios and 95 % confidence intervals were calculated [19].
The difference between total costs of claims was determined using a generalised linear model. The Gamma distribution was used in analysis as a means of dealing with positively skewed data [20]. Potential cofounders (gender, industry classification and employer remuneration) were controlled for in the analysis. Analyses were performed using SPSS version 17 [21].
Finally the differences in total claim costs and days of compensation for the intervention companies before and after the intervention was investigated to determine whether any patterns existed based on injury location, industrial sector or employer size.
Approval for the study was granted by the relevant faculty human ethics committee.
Results
Information regarding 3,312 claims was captured from the VWA database (Table 2). The majority of claims were coded as sprains or strains with the most injuries affecting the back. Shoulder and neck injuries were also common. Muscular stress in different tasks was the most commonly recorded mechanism of injury, accounting for over 50 % of total claims. The mean and standard deviations for days of compensation, total costs, medical costs and weekly benefits are provided in Table 3. The differences between each group for the three comparisons are provided in Table 4.
Primary Analysis: Comparison of Intervention Companies Pre and Post Intervention
After the intervention was applied, the intervention companies performed significantly better on all outcomes (p < 0.05) (Table 4). There were significantly fewer days of compensation (Fig. 2), lower medical costs and lower weekly benefits. Overall the average cost of a claim was $3,913 post intervention compared to $6,019 for the pre intervention period (adjusted difference $2,329, 95 % CI $1,318–$3,340).
Kaplan–Meier curve describing days of compensation pre and post intervention period for the intervention companies (n = 815). In the post intervention period there were significantly fewer days of compensation (mean 14.1 days) compared to the pre intervention period (mean 33.5 days) (HR 0.77, 95 % CI 0.67–0.88)
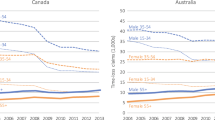
The difference between pre intervention and post intervention claims is illustrated further according to injury location (Fig. 3a, b), industry sector (Fig. 4a, b), company size in terms of remuneration (Fig. 5a, b).
Comparison of Intervention and Control Companies in Pre Intervention Period
The intervention and control companies did not differ on the primary outcomes pre intervention. However, the intervention companies had significantly higher medical costs than the control companies (p < 0.05). Overall the average medical costs for the intervention companies was $3,378 compared to $2,891 for the control companies (estimated difference $505, 95 % CI $39–$970) (Table 4).
Comparison of Control Companies Across Pre and Post Intervention Periods
There were no significant differences (p > 0.05) on any of the outcomes for the control companies when comparing claims from the pre intervention period and the post intervention period (Table 4).
Discussion
Analysis of the VWA database demonstrated that the intervention model of management of MSD was effective in improving cost-based outcomes. The total average cost of a claim in the intervention companies was reduced by 35 % after the intervention was applied, and the number of days of compensation was reduced by 58 %. These results underline the effectiveness of the intervention in reducing overall total claim costs, medical costs, and the number of days of compensation.
The intervention aimed to commence the injury management process as early as possible by early reporting via an injury hotline. Early intervention has been shown to improve outcomes for occupational injuries [22–24], and the intervention model studied aimed to consistently begin the process of supporting the injured worker within an hour of the injury. Another mechanism likely to reduce time lost is for the worker to receive a high standard of medical care. This was achieved through discussion with the worker’s usual health practitioners and referral to experienced occupational health practitioners where possible. Experienced occupational practitioners are more likely to be aware of and implement evidence-based interventions [16]. The health practitioners utilised within the intervention were encouraged to become familiar with the nature of the workplace in question and the type of alternate duties likely to be available. Finally, injury managers worked with the treating doctor and insurer to avoid any delays in approvals required for specialist treatment. As a result, early return to the workplace with the allocation of suitable alternate duties was more likely, leading to less time lost [16, 23].
One of the major areas for emphasis as part of the intervention was the facilitation of communication between the major parties concerned. The literature identifies that communication between key stakeholders is a challenge [16, 24] and that interventions that encourage collaboration are likely to improve outcomes [22]. In simple cases, the injury managers facilitated open communication between the injured worker, treating physician and the direct supervisor. In more complex cases the injury manager aimed to ensure other parties, such as human resources, the union or senior management were open to communication throughout the process.
This can often be difficult to achieve depending on the level of cooperation provided by each stakeholder. The overall aim of the intervention was to remove barriers to return to work and positively influence the work injury culture within the workplace. The benefits of this approach are demonstrated in this study in the reduction in the number of days of compensation and overall costs per claim.
The reduction in the cost and duration of claims demonstrated in the medium term is likely to lead to further cost reductions long term. The costs associated with worker’s compensation claims are dominated by a small proportion of long term and expensive cases [25–27]. By reducing claim duration it is likely to reduce the number of longer term and expensive claims [28].
Further investigation of the difference between pre and post intervention claims revealed some unexpected findings. While the effect for different body locations and industrial sectors demonstrated similar trends, there was a difference in results for companies with remuneration between $5 and $10 million. Further examination of the companies in this size range is difficult given a relatively small number of claims per company. The increased average claim cost is explained by small number of complex claims occurring within a relatively small establishment, driving average costs upwards. However, even in this category the average number of days of compensation appeared to be reduced by the intervention, suggesting the intervention still had positive effects within these companies.
Other mechanisms behind the apparent effectiveness of the intervention must be considered. The intervention companies engaged the intervention via a commercial contract, implying a prior commitment to improving work injury practices from senior management. This may spur other changes outside of the intervention to improve injury management which then filter down through the organisation. The desire of the intervention companies to improve work injury practices could mean these companies are intrinsically different from the control companies (i.e. a selection bias exists). However, at the time of the introduction of the intervention, there was not a perceived company-wide impetus for change within the intervention companies. Furthermore, the comparison of the intervention companies to the control companies at baseline demonstrated that they were not significantly different on the primary outcome measures. So while selection bias may exist across the intervention companies, it is unlikely to be a major explanation of the differences demonstrated.
Across the pre intervention and post intervention periods there were differences in the number of claims recorded. The greater number of pre intervention claims compared to post intervention claims for the control companies is explained by a slightly longer time period used to collect pre intervention data. The monthly claim rate remained stable across the pre intervention period for the control companies so this is unlikely to have affected results. However, there were 51 more claims recorded for the intervention companies in the post intervention period. The intervention fostered reporting of cases, and this is likely to be the reason for increase in claim numbers in the intervention companies. Encouragement of reporting reflects a more positive attitude towards work injury practices as injured workers may be more likely to file a claim if they feel the workplace will be supportive and there are no negative consequences of doing so.
Study Strengths and Limitations
The major strength of the study was that it covered a ‘real life’ intervention that was operational in the everyday setting and tested the intervention across a range of industries and employer sizes. The database was collected by a body external to the employers and company providing the intervention, increasing the confidence that the data collected is free of bias from the interested parties. The large sample size, the use of two control groups for comparison and the research design increase the confidence that the differences seen are due to the intervention and not extraneous factors.
However the study is also limited by the information captured in the database. The database recorded variables of an administrative nature, consisting of data easy to draw from information required when a VWA claim is made. The compromise for access to large numbers of injury claims is the restriction to variables easily collected within the system. In reality the information required to describe the complex return to work process is difficult to describe [1, 11] and even more difficult to capture in administrative databases. As a result the outcomes investigated are not the outcomes of interest for all stakeholders. It cannot be deduced from this study whether the intervention improved outcomes from the worker’s perspective or from an employer’s productivity perspective. The information is useful from an employer’s work injury cost perspective, an insurer’s perspective and from the perspective of the VWA. Further research is required to investigate the impact of the intervention on other return to work outcomes.
The intervention companies were medium to large companies. It is not possible to determine whether the intervention would be effective for smaller employers.
While the intervention reduced the number of days of compensation and overall costs of claims, these benefits must be weighed up with the extra costs of providing the intervention. The cost of the intervention was paid by the employer and in the commercial setting this would only continue if the benefits of reduced compensation premiums outweigh the costs of the service. The insurance system in place determines the insurance premium payable by the employer based on the past history of claims. Therefore, the intervention is also likely to lead to a reduced insurance premium through reduction in claims costs, as well as a reduction in indirect costs. Furthermore, the intervention is likely to replace the role of the return to work coordinator within the company, allowing them to undertake a different role within the company. As a result, a detailed cost-benefit analysis of the intervention is beyond the scope of this paper.
Conclusion
The model of management investigated was effective in reducing the number of days of compensation, total claim costs, total medical costs and the amount paid in weekly benefits. The database was gathered by a body external to the involved parties, meaning any bias in the outcomes is likely to be low. However, the nature of information collected in administrative databases means further research must be done to determine whether the intervention is beneficial to all stakeholders in the return to work process.
References
Young AE, Wasiak R, Roessler RT, McPherson KM, Anema JR, van Poppel MN. Return-to-work outcomes following work disability: stakeholder motivations, interests and concerns. J Occup Rehabil. 2005;15:543–56.
Loisel P, Durand M, Berthelette D, Vezina N, Baril R, Gagnon D, et al. Disability prevention: new paradigm for the management of occupational back pain. Dis Manag Health Outcomes. 2001;9:351–60.
Waddell G. The back pain revolution. 2nd ed. Edinburgh: Churchill Livingstone; 2004.
WorkSafe. 2006–2007 statistical summary. http://www.worksafe.vic.gov.au/wps/wcm/resources/file/eb1d2d029a7c85e/Statistical_Summary_2006_07.pdf (2008). Accessed 10 Apr 2008.
Bernacki EJ. Factors influencing the costs of workers’ compensation. Clin Occup Environ Med. 2004;4:249–57.
Stephens B, Gross DP. The influence of a continuum of care model on the rehabilitation of compensation claimants with soft tissue disorders. Spine. 2007;32:2898–904.
Butler RJ, Johnson WG, Gray BP. Timing makes a difference: early nurse case management intervention and low back pain. Prof Case Manag. 2007;12:316–27.
Selander J, Marnetoft SU. Case management in vocational rehabilitation: a case study with promising results. Work. 2005;24:297–304.
Lambeek LC, Van Mechelen W, Knol DL, Loisel P, Anema JR. Randomized controlled trial of integrated care to reduce disability from chronic low back pain in working and private life. BMJ. 2010;340:c1035.
Hogelund J, Holm A. Case management interviews and the return to work of disabled employees. J Health Econ. 2006;25:500–19.
Young AE, Roessler RT, Wasiak R, McPherson KM, van Poppel MN, Anema JR. A developmental conceptualization of return to work. J Occup Rehabil. 2005;15:557–68.
Elfering A. Work-related outcome assessment instruments. Eur Spine J. 2006;15:S32–43.
Wasiak R, Young AE, Roessler RT, McPherson KM, van Poppel MN, Anema JR. Measuring return to work. J Occup Rehabil. 2007;17:766–81.
Waddell G, Burton K, Aylward M. Work and common health problems. J Insur Med. 2007;39:109–20.
Costa-Black KM, Loisel P, Anema JR, Pransky G. Back pain and work. Best Pract Res Clin Rheumatol. 2010;24:227–40.
Loisel P, Buchbinder R, Hazard R, Keller R, Scheel I, van Tulder M, et al. Prevention of work disability due to musculoskeletal disorders: the challenge of implementing evidence. J Occup Rehabil. 2005;15:507–24.
Occupational Health and Safety Act 2004 (2004).
WorkSafe Victoria 2011. http://www.worksafe.vic.gov.au (2011). Accessed 6 July 2011.
Tabachnick BG, Fidell LS. Using multivariate statistics. 4th ed. Boston: Allyn and Bacon; 2001.
Faddy M, Graves N, Pettitt A. Modeling length of stay in hospital and other right skewed data: comparison of phase-type, gamma and log-normal distributions. Value Health. 2009;12:309–14.
Polar Engineering and Consulting. PASW Statistics 17. 17.0.2 ed2009. (2009).
Carroll C, Rick J, Pilgrim H, Cameron J, Hillage J. Workplace involvement improves return to work rates among employees with back pain on long-term sick leave: a systematic review of the effectiveness and cost-effectiveness of interventions. Disabil Rehabil. 2010;32:607–21.
Williams RM, Westmorland MG, Lin CA, Schmuck G, Creen M. Effectiveness of workplace rehabilitation interventions in the treatment of work-related low back pain: a systematic review. Disabil Rehabil. 2007;29:607–24.
Frank J, Sinclair S, Hogg-Johnson S, Shannon H, Bombardier C, Beaton D, et al. Preventing disability from work-related low-back pain. New evidence gives new hope—if we can just get all the players onside. CMAJ. 1998;158:1625–31.
Federspiel CF, Guy D, Kane D, Spengler D. Expenditures for nonspecific back injuries in the workplace. J Occup Med. 1989;31:919–24.
Hashemi L, Webster BS, Clancy EA. Trends in disability duration and cost of workers’ compensation low back pain claims (1988–1996). J Occup Environ Med. 1998;40:1110–9.
Williams DA, Feuerstein M, Durbin D, Pezzullo J. Health care and indemnity costs across the natural history of disability in occupational low back pain. Spine. 1998;23:2329–36.
Loisel P, Lemaire J, Poitras S, Durand MJ, Champagne F, Stock S, et al. Cost-benefit and cost-effectiveness analysis of a disability prevention model for back pain management: a six year follow up study. Occup Environ Med. 2002;59:807–15.
Acknowledgments
This work was supported by Canadian Institutes of Health Research (CIHR) grant(s) FRN: 53909. The authors would like to thank the management and staff of OccCorp Pty Ltd for their assistance in describing the intervention examined in this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iles, R.A., Wyatt, M. & Pransky, G. Multi-Faceted Case Management: Reducing Compensation Costs of Musculoskeletal Work Injuries in Australia. J Occup Rehabil 22, 478–488 (2012). https://doi.org/10.1007/s10926-012-9364-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-012-9364-2