Abstract
Background: Cumulative trauma disorders of the upper extremities (CTD) have become increasingly important in workers' compensation caseloads over the last two decades. Relative to occupational back pain, CTD have been much less studied. Methods: We analyzed post-injury employment patterns and return-to-work probabilities for a sample of Ontario workers with CTD, for up to five years after injury. Results for workers with CTD are compared to results for workers with back injuries or fractures. Results: Most workers with CTD return to work at least once, but a first return does not necessarily mark the end of work disability. Among workers absent at least once, 26% with CTD report a second injury-related absence, compared to 18% with back pain and 12% with fractures. After five years, focusing on first returns underestimates work-loss days associated with CTD by 32%. Conclusions: A substantial proportion of workers with CTD or work-related back pain experience injury-related absences after their first return to work. Focusing on the first return to work is misleading for both injury groups, but even more so for CTD, as they appear to be even more susceptible to multiple spells of work absence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cumulative trauma disorders of the upper extremities have become an increasingly important proportion of workers’ compensation claims over the last two decades. The disorders, involving muscles, tendons, or nerves, of the shoulder, arm, elbow, wrist, or hand, represent approximately four percent of current workers’ compensation caseloads [2–4], but a larger share of workers’ compensation costs. This is because a small fraction of upper extremity claims incurs lengthy spells of work absence and high indemnity costs; in this way, upper extremity disorders are similar to the more frequent cases of occupational back pain.
There is a considerable literature on the epidemiology, risk factors, and treatment outcomes of upper extremity disorders, but work-related outcomes and costs have been much less studied. The path-breaking studies of work outcomes have tended to focus on first returns to work and durations of initial spells of work absence, because these data are available on workers' compensation claims files. Yet we know from the recent literature on back pain that a return to work does not necessarily mark the end of the spells of work disability associated with a chronic condition. A recent survey of injured workers with upper extremity disorders indicates that recurrence of pain and associated work disability is also an important issue for this population [8].
The costs of cumulative trauma upper extremity disorders include the direct health care costs of treating the illness, and indirect costs including productivity losses, administrative costs, costs of training replacement workers, and psychosocial costs incurred by injured workers. A number of excellent cost studies have estimated the direct health care costs of upper extremity disorders from administrative claims data, and imputed productivity losses from the costs of indemnity benefits. Other indirect costs are exceedingly difficult to measure, although several surveys of injured workers suggest these costs are not insignificant. Again the literature on back pain, where recent studies have imputed productivity losses from estimates of wage losses in the post-injury period, may help guide the direction of future research on upper extremity disorders.
In this study, we apply methods we have used to study the costs and outcomes of work-related back pain to work-related upper extremity disorders. There are many similarities between the two injury groups: Both are occupational illnesses typically caused by cumulative stress rather than by a discrete accident or injury. Both are chronic conditions in which pain tends to recur and may be exacerbated by a return to work. The claim distributions for both injury groups are characterized by a small number of long-duration claims with high indemnity costs, skewing the cost distributions to the right. A logical next step in the research, therefore, is to apply methods, such as multiple spell models of work absence and survival curve analysis, that have been used to study the course of occupational back pain to upper extremity disorders. To place the work in context, we begin by summarizing the current literature on the costs and outcomes of upper extremity disorders.
Background
We conducted a literature search of articles referenced in the PubMed, MedLine, and EconLit databases, with publication dates after 1995, using the search phrases: upper extremity disorders/conditions—costs, work absence, work outcomes. The search retrieved approximately 75 articles. We exclude from our review articles that focus exclusively on the epidemiology or etiology of upper extremity disorders, articles that analyze costs or outcomes within a particular occupational subgroup, and articles that analyze the outcomes of different treatment protocols. The principal findings of the remaining studies are summarized below.
Duration of work absence
The majority of claims for work-related upper extremity disorders are resolved quickly and the worker returns to work before the waiting period for indemnity benefits expires. Most studies of post-injury work absence for upper extremity disorders report median days absent from work equals zero [3, 4] (Cheadle et al., 1994). Typical workers’ compensation caseloads involve 80 percent or more ‘medical only’ (no indemnity benefits paid) claims, so upper extremity disorders are no exception.
On the other hand, a small but significant proportion of workers with upper extremity disorders experience unusually lengthy spells of work absence. A BLS study of lost-time illnesses and injuries in 1997, for example, shows that, relative to other injury groups, upper extremity disorders are associated with the highest proportion of cases with durations of work absence in excess of 31 days (BLS 1999). Yassi, et al. [13], studying upper limb repetitive strain injuries in Manitoba, report that mean time lost is significantly greater for these claims (71.4 days) than for non-repetitive strain injuries (33.6 days). In a study of 1994 claims from a single large workers’ compensation insurer, Hashemi et al. [4] report that more than 50 percent of cases involve no lost time, but mean duration of work absence overall exceeds 12 weeks. Feuerstein et al. [3] observe similar trends in a study of workers’ compensation claims for upper extremity disorders in the federal workforce. Among lost time claims with carpal tunnel syndrome, mean duration of work absence is 17 weeks, with 60 percent of claimants absent 10 weeks or more. Among lost time claims with entheosopathy of the elbow, mean duration is 16 weeks, with 49 percent absent 10 weeks or more.
As is typical in workers’ compensation claim distributions, the hazard function (conditional probability of remaining on disability) for upper extremity claims declines at a decreasing rate as work absences lengthen, so that a small fraction of injured workers with the longest spells of work absence have extremely low probabilities of returning to work. In a study of workers’ compensation cases filed in Washington state from 1987–89, Cheadle et al. (1994) report that 18 percent of carpal tunnel cases are absent at least six months, 12 percent absent at least 12 months, and 7 percent absent two years or more. Hashemi et al. [4], analyzing data for more than 21,000 workers with upper extremity claims (including claims for neck pain) report that 23 percent are absent at least one month, 11 percent absent at least six months, and 7 percent absent one year or more. Evidence from these two studies suggests that approximately five percent of workers with upper extremity claims are unlikely ever to return to work. Indeed, Yassi et al. [13] report that 3 percent of workers in their sample of Manitoba claims were unable to return to work at all.
The lengthy spells of work absence associated with some cases of upper extremity disorders imply large productivity losses for employers, but productivity losses are not limited to time absent from work. A growing body of literature has begun to focus on the impact of disabling health conditions on workers’ productivity on the job, and two recent studies suggests that the on-the-job productivity losses associated with upper extremity disorders may be considerable. In 1996, Morse and Warren (1998) conducted a telephone survey of 374 persons with chronic upper extremity pain; 292 persons reported their pain was work-related. Among the cases of work-related upper extremity disorders, 35 percent reported having to cut down on their work pace, although only 4 percent reported having to go on disability. Keogh et al. [6] conducted a telephone survey of 575 Maryland workers who filed compensation claims for cumulative trauma upper extremity disorders. At the time of interview, one to four years post-onset, over 50 percent of workers reported that their symptoms continued to interfere with work.
Productivity losses associated with upper extremity disorders may also be incurred during spells of work absence subsequent to the first return to work, because of the recurrent nature of the conditions. Yassi et al. [13] report that 19 percent of Manitoba workers in their sample experienced a recurrence of injury after return to work. Pransky et al. [8] report evidence on recurrence from a survey of injured workers. The authors distributed self-reported questionnaires to workers who filed claims for work-related upper extremity conditions with the New Hampshire State Department of Labor between August and September 1994. Approximately one-fourth of respondents reported experiencing a recurrence of the upper extremity condition, where recurrence is defined as re-injury or worsening of the same injury. One-third of those who experienced a recurrence also lost time from work. The Pransky et al. results are only suggestive for cumulative trauma upper extremity disorders overall, because the sampling strategy includes acute conditions, such as fractures, burns and lacerations, and over-samples indemnity claims. Nevertheless, the results of both studies imply that it is useful to look beyond the first return to work when analyzing the outcomes of upper extremity disorders.
Costs and job loss
Empirical studies of the costs of upper extremity disorders rely heavily on administrative workers’ compensation claims data, and consistently show that mean claim costs are between $5000 and $8000 (Table 1). The highly skewed nature of the duration distribution for upper extremity claims, however, indicates that the mean is a poor measure of the costs of a typical claim. Webster and Snook (1994), for example, analyzing the costs of cumulative trauma upper extremity claims filed with a large national workers’ compensation insurer in 1989, report mean total medical and indemnity payments of $8,070, while median costs are only $824. The most costly 25 percent of claims account for 89 percent of costs. Feuerstein et al. [3] report that, among lost-time claims, 18 percent of carpal tunnel cases account for 53 percent of indemnity costs, while 23 percent of entheosopathy cases account for 67 percent of costs.
The total cost burden of work-related upper extremity disorders is large because of the relatively high incidence of the conditions. Data from the Washington state fund shows an annual incidence rate of 2.6 per 100 workers for upper extremity disorders overall, with one-third of cases and one-half of lost workdays attributed to cumulative trauma disorders (NRC 2001). The most recent data from the BLS reports incidence rates of 11.6 per 100,000 workers for lost-time claims involving cumulative trauma upper extremity disorders (nature of injury is sprain, carpal tunnel syndrome, tendonitis, or pain) (BLS 2003). Silverstein et al. [11] estimate total direct costs of cumulative trauma upper extremity disorders to be $6.5 billion annually, assuming an incidence rate of 116 per 10,000 workers for all work-related upper extremity claims, average claim costs of $5837 (based on data from the Washington state fund) and 96 million full-time workers in the U.S.
Estimates of the costs of work-related upper extremity disorders derived from administrative data are certain to underestimate the true costs on society, however, because many cases go unreported, and because indemnity benefits may not cover periods of prolonged or recurrent spells of work absence. Among the cases of self-reported work-related musculoskeletal disorders interviewed by Morse and Warren (1998), only 11 percent had filed a workers’ compensation claim. In a more recent study, applying capture-recapture analysis to seven years of Connecticut data, Morse et al. (2005) estimate that only six to eight percent of work-related upper extremity musculoskeletal disorders are reported.
Research suggests that approximately one-third of workers with upper extremity disorders are at risk of prolonged employment instability following their injury. In the Keogh study [6], 38 percent of workers report that they were voluntarily or involuntarily separated from their time of injury job, and 28 percent were out of work at the time of interview (one to four years post-onset). Workers with higher incomes, less severe injuries, and members of a labor union at the time of injury were more likely to be employed. Roquelaure et al. [9] conducted a study of 514 workers who filed compensation claims for upper extremity musculoskeletal disorders in Pays de la Loire, France. Two years after filing their claims, 65 percent of workers had returned to their time of injury employer, but 18 percent had been dismissed. Older workers, and workers with multiple diagnoses for upper extremity disorders, were at higher risk of dismissal.
Persons with upper extremity disorders often report severe financial hardship on their families, suggesting that lengthy or recurring spells of work absence are under-compensated. Keogh et al. [6] report that, following a work-related upper extremity injury, 16 percent of families could not afford to maintain their car, 32 percent borrowed money from friends or family, and 36 percent had been contacted by a collection agency. Compared to a control group without upper extremity pain, persons with upper extremity disorders are significantly more likely to report that they have moved for financial reasons, lost a home or car, or lost health insurance (Morse and Warren, 1998).
In sum, most upper extremity injuries involve little or no time off work, and medical costs less than $1000. A small, but costly, minority of cases, however, exhibits lengthy spells of work absence associated with a huge cost burden on the workers’ compensation system and the families of injured workers. Some evidence suggests that recurring spells of work absence may increase the disability burden further, but this hypothesis is not well documented. To begin to quantify the long-term work disability associated with upper extremity disorders we analyze patterns of post-injury work experience for a sample of Ontario workers with cumulative trauma upper extremity disorders and conduct survival curve analyses comparing upper extremity disorders to back pain and fractures.
Methods
First return to work
We use a logistic model to estimate the determinants of whether or not a worker with an upper extremity disorder returns to work. The binary dependent variable equals one if a worker is employed at any time between the date of onset and the date of interview, and zero otherwise. The likelihood function is
where \(i \in E\) if the ith worker returns to work (or never experiences a work absence), and \(i \in \bar E\) if he does not. The vector Z includes variables that influence the decision to return to work, α is a corresponding vector of coefficients, and Φ represents the cumulative distribution function of a logistic random variable.
We assume a worker returns to work if the wage offered by an employer is equal or greater than the worker's value of leisure time (reservation wage). Variables in the vector Z represent factors that influence post-onset offer wages and reservation wages, including demographic and human capital characteristics, institutional factors that affect the demand for labor, and workers’ compensation benefits. The model also includes relevant characteristics of the pre-injury job, because an injured worker's best opportunity to return to work is likely with his pre-injury employer.
Our previous work has demonstrated, however, that a return to work does not necessarily mark the end of the work disability associated with chronic and recurrent conditions, such as back pain. Many types of upper extremity disorders can be classified as chronic and recurrent, and are also likely to be characterized by repeated episodes of work disability. To analyze the experiences of workers with upper extremity disorders after the first return to work, we consider the subset of workers who return to work at least once, and identify the determinants of four distinct patterns of post-onset employment.
Patterns of post-injury employment
We define four mutually exclusive patterns of post-injury employment, according to the number of returns to work attempted between the date of onset and date of interview, and employment status at the date of interview. The assumption of four distinct patterns is based on a review of the descriptive data with the objective of defining the minimum number of patterns that define the distinguishing characteristics of different post-onset employment experiences. The patterns are:
-
1.
The worker returns to work after an initial spell of work absence, and is employed at interview (Single return, employed).
-
2.
The worker returns to work, leaves her first post-onset job for reasons associated with the upper extremity disorder, and is not subsequently employed (Single return, not employed).
-
3.
The worker experiences multiple spells of work absence and returns to work related to the upper extremity disorder, but she is employed at interview (Multiple returns, employed).
-
4.
The worker experiences multiple work absences and returns, and is unemployed at interview, for reasons related to the upper extremity disorder (Multiple returns, not employed).
To analyze the determinants of post-onset employment for workers with upper extremity disorders, we estimate a multinomial logit model of the probability that a worker experiences single or multiple returns to work, and is employed at interview. The categorical dependent variable identifies one of the four employment patterns described above. Independent variables represent characteristics that affect the post-onset offer wage and reservation wage functions. The multinomial logit model is specified as follows.
Let the utility function of an injured worker be given by
where \(W_{ij}^O\) represents the offer wage, and \(L_j\) represents hours of leisure in \(j = 1\ldots4\) possible employment patterns. The vector X, which includes variables that determine the post-onset offer wage and value of leisure time, is assumed constant across employment patterns but the corresponding vector of coefficients, \(\beta _j\), and the random error term, \(\varepsilon _{ij}\), are allowed to vary. Workers who never return to work after onset are excluded because we assume the utility derived from at least one of the employment patterns is greater than the utility derived from not working at all.
Consider a worker who returns to work after an initial absence and remains employed thereafter (j=1). The worker follows this pattern because she is capable of working and derives more utility from staying at work than from any of the three alternatives. Thus, the probability of observing a worker in the first pattern is
Similar expressions hold for the other three employment patterns.
Assuming the underlying distributions of \(\varepsilon _{ij}\) are type I extreme-value distributed, the probability of observing the ith worker in the jth employment pattern is
for j=1, 2, 3 and
for the reference pattern, j=4. If we define a set of four dummy variables \(Y_{ij} ,j = 1 \ldots 4\), such that Y ij =1 if the ith worker exhibits the jth employment pattern, Y ij =0 otherwise, then the log likelihood function for the model is
Maximizing equation (5) yields estimates of the parameters \(\beta _j\) for three employment patterns relative to an omitted pattern, in this case Pattern 4 (Multiple returns, not employed). The estimated coefficients of the multinomial logit function do not, however, represent the marginal effects of individual characteristics on observed patterns of employment. We convert the coefficients to measures of marginal effects and, for ease of comparison among variables, express the results as semi-elasticities as follows:
In equations (6a) and (6b), k and j are indices across the four employment patterns, while m is an index across the explanatory variables in X i .
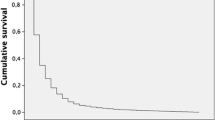
Lost work time
While the patterns model provides a more complete profile of post-injury work experiences than traditional models that use the first return to work as an endpoint, the model is incomplete in that it does not account for durations of spells of work absence. Workers who experience identical patterns of post-injury employment may accrue very different productivity losses if durations of work absence differ. To begin to quantify the cumulative productivity losses associated with upper extremity disorders, across multiple spells of work absence, we conduct a survival curve analysis. A survival curve plots the conditional probability that spells of work absence continue, on the vertical axis, against time absent from work, on the horizontal axis. The area under the curve is an estimate of the productivity losses (cumulative days absent from work) for a sample of injured workers. We compare survival curves for upper extremity disorders to: (1) back pain, another cumulative trauma injury, and (2) fractures, a more traditional injury typically associated with a discrete workplace event. In what follows, the survival curve method is described in greater detail.
Consider a work-related injury with onset at time t=0, that results in a spell of work absence. If the cumulative distribution function for time to return to work is F(t), then the fraction of workers remaining out of work because of injury is S(t)=1−F(t). S(t) is called the survival function and the survival curve is a graphical representation of S(t), with the proportion of the sample absent from work shown on the vertical axis and time t on the horizontal axis.
A hypothetical survival function for workers with upper extremity disorders (and other work-related injuries) is expected to exhibit the following characteristics: At t=0, S(t)=100 percent, because survival curve analyses typically exclude medical only claims, so initially 100 percent of the sample is absent from work. As claim duration time passes, S(t) decreases at a decreasing rate. In other words, most workers with upper extremity disorders return to work within a relatively short period of time, but the probability of return to work decreases as time elapses from date of onset. Thus, the survival curve is a convex, downward-sloping function from an intersection point on the vertical axis. The area under the curve represents cumulative days of work absence, or productivity losses, accrued by a sample of injured workers from date of onset through t days of work disability.
Now consider comparisons of different types of work-related injuries. If the survival curve for injury group A lies everywhere above the curve for injury group B, productivity losses are greater for injury A and the difference between the areas under the two curves (that is, the area between the curves) is a measure of the difference in productivity losses, as measured by days of work absence. Survival curves may cross – indicating that workers with injury A, for example, have higher probabilities of return to work shortly after onset, but lower probabilities of return as claim duration progresses. Again, the injury with greater productivity losses can be identified by comparisons of the area under each survival curve.
We estimate and plot survival curves for our sample of workers with upper extremity disorders, compared to workers with back injuries or fractures. Survival curves are plotted for the first, second, third and fourth spells of work absence following onset, in an attempt to depict the cumulative productivity losses associated with upper extremity disorders. Beyond four spells, sample sizes become too small to plot survival curves.
An issue is how to control for censored cases (not yet returned to work) in the survival analyses. The survival curves are Kaplan-Meier estimates of the survival function, using full information maximum likelihood techniques that account for censored data. A limitation of the data is that, after the first spell of work absence, the censoring variable is missing for over half the observations. In these cases we assume the spell is censored because all the information we have is that the absence spell lasted at least as long as indicated in the data.
All estimation is conducted in SAS, with the LIFETEST procedure used to obtain the Kaplan-Meier estimates.
Data and variables
Data and exclusion criteria
The data come from the Survey of Ontario Workers with Permanent Impairments, the largest survey of injured workers ever conducted. The survey population includes all workers examined for permanent disability assessment by physicians of the Ontario Workers’ Compensation Board (now renamed the Workplace Safety and Insurance Board) between June 1989 and June 1990. The survey combines detailed information on post-injury employment and earnings obtained from interviews with injured workers, with workers’ compensation claims data obtained from administrative records. Workers in the survey were injured between 1967 and 1990 but more than two-thirds have injury dates after 1984. All the workers in the sample have permanent partial impairments resulting form a workplace illness or injury, so the data represent a relatively severe subset of the typical workers’ compensation caseload. The Ontario survey is 15 years old, but to our knowledge it is the only workers’ compensation database with extensive pre-and post-injury job information.
We restrict the sample to workers with diagnoses of upper extremity disorders, based on ICD-9 diagnostic codes and definitions reported in workers’ administrative claims files (Appendix Table A1). The relevant ICD-9 codes identify workers with upper extremity sprains and strains, injuries to nerves, synovitis, tendonitis, and white finger disease, as well as carpal tunnel syndrome and epicondylitis [3]. In cases where ICD-9 codes are missing, we identify upper extremity disorders based on nature of injury and part of body codes, including upper extremity sprains and strains, and upper extremity inflammation of joints. Excluding cases with missing data, there are 1,317 workers with upper extremity disorders in the sample.
The survival curves and employment patterns models are based on subsets of this sample, with additional restrictions. To estimate survival curves, we restrict the sample to workers who provide complete data on spells of work and work absence for five years post-injury (or until the observation is censored at the date of interview). The samples for the survival analysis include 879 upper extremity cases, compared to 3,723 back cases and 849 fractures. To analyze post-injury patterns of employment, we restrict the sample to workers who return to work at least once, to workers who have a date of interview no less than three years after date of onset, and we exclude censored cases. This assures a minimum three-year post-onset work history in which to observe employment patterns. With these additional restrictions, the sample for the patterns model includes 303 workers.
Variable definitions
Independent variables in the return to work and patterns models represent factors that influence post-onset offer wages and reservation wages, including human capital characteristics, labor demand, workers’ compensation benefits, and characteristics of the pre-injury job. An injured worker's human capital is measured by: education (=1 for high school or college graduate); job experience (=1 for workers who have at least five years experience with the pre-injury employer); and age, a proxy for potential experience in other jobs. Characteristics of the pre-injury job include union membership (=1 for union) and employment in a physically demanding industry (=1 for workers in the agriculture, construction, or mining industries). All else equal, we expect physically demanding employment to have a negative impact on post-onset employment outcomes, because it is more difficult for workers with chronic disorders to return to physical jobs. This is a cautious prediction, however, as some sedentary jobs (eg. clerical work) may be equally aggravating for workers with upper extremity disorders. The predicted effect of union membership on post-onset employment is ambiguous because, on the one hand, unions may protect the job rights of injured workers, but, on the other hand, union work rules may make it more difficult to provide accommodations that facilitate returns to work. The workers’ compensation benefit replacement rate, the ratio of expected temporary disability benefits to pre-injury wages, is included in the models to capture the disincentive effects of disability benefits on returns to work. Finally, labor demand is represented by gender (=1 for female) and region (=1 for northeast). The northeast region of Ontario had persistently high unemployment rates throughout the period in which the injuries occurred.Footnote 1
Results
First return to work
Table 2 reports means and coefficient estimates of the first return to work model for the full sample of 1,317 workers with upper extremity disorders. Despite the fact that all the workers had permanent impairments resulting from their injury, 80 percent had returned to work at least once by the time of interview. The mean age of the sample was 41, with 49 percent males, and 26 percent employed in physically demanding industries.
The largest estimated effect in the return to work model was the negative coefficient for the workers’ compensation benefit replacement rate. The magnitude of the estimated coefficient indicated a much greater elasticity of employment with respect to disability benefits than we had found in similar models estimated for samples of work-related back cases [5]. The sensitivity of workers with upper extremity disorders to the work disincentives could reflect a greater fear of re-injury if they return to the same job, lower job satisfaction leading to a reluctance to return to work, greater difficulty in providing job accommodations for upper extremity cases, or a number of other factors. In results not shown, we found some evidence supporting the accommodations hypothesis: upper extremity cases were less likely to receive any of the types of job accommodations reported in the data (reduced hours, light work, flexible schedule, modified equipment, special training) than were back cases or fractures. The most common accommodation for all three groups was light work. Only 35 percent of upper extremity cases reported a light work accommodation on their first return to work, compared to 40 percent of back cases and fractures.Footnote 2 , Footnote 3
Other variables that were significant determinants of return to work include age, industry, work experience, and union membership. Older workers, and workers employed in a physically demanding industry, were less likely to return after an upper extremity injury than other workers. The importance of age and industry effects in the return to work model were consistent with the findings of Roquelare et al. (2005). Union members, and workers with five or more years experience with their time-of-injury employer were more likely to return to work than other workers. The union effects were consistent with results reported by Keogh et al. [6], where union members were significantly more likely to return to their time of injury employers, and to be employed one-four years after an upper extremity injury, than non-union members.
Employment patterns
In previous research with the Ontario data [5], we have shown that a first return to work does not necessarily mark the end of the spells of work disability associated with a cumulative trauma disorder, such as back pain or carpal tunnel syndrome. To analyze the employment experiences of workers with upper extremity disorders after the first return to work, we restricted our sample to workers who returned to work at least once following injury, and classified the remaining 303 cases into one of the four employment patterns described above. The distribution across employment patterns is reported in Table 3, and compared to our previous results for back pain.
Again, we found considerable movement in and out of employment after the first return to work. Two-thirds of workers who returned to work following an upper extremity injury reported subsequent spells of work absence associated with the original injury (Patterns 2-4). Nearly 30 percent left their first post-injury job for injury-related reasons and never returned to work (Pattern 2), while 37 percent experienced multiple spells of work and work absence (Patterns 3-4). The results were remarkably consistent with our previous work on back pain (e g. 33% of upper extremity cases, 34% of back cases, in Pattern 1), providing further support for the similar nature of the conditions. One difference is that upper extremity cases were more likely than back cases to make repeated attempts to return to work (37% vs. 32% in Patterns 3-4).
To analyze the determinants of post-injury employment patterns, we estimated a multinomial logit model in which the dependent variable identified one of the four mutually exclusive patterns described above, and the independent variables were identical to those in the first return to work model. Table 4 reports means of the independent variables by employment pattern. Five variables, namely, age, gender, education, work experience and union membership, exhibited considerable differences in means across patterns, and appeared to be potentially important determinants of employment experiences after the first return to work. Older workers were less likely to experience multiple returns ending in employment (Pattern 3), while workers with five or more years experience with their time of injury employers were less likely to be not employed after a single return (Pattern 2). Being male and having a high school education or better were associated with being employed at the date of interview (Patterns 1,3). Finally, union membership was associated with a successful first return to work (Pattern 1) and, to a lesser degree, with multiple spell patterns (Patterns 3, 4).
To determine which of these relationships are significant when other variables are held constant, we estimated the determinants of episodes of employment that occurred after a first return to work using the multinomial logit model. Estimated coefficients were converted to semi-elasticities so they could be interpreted as marginal effects, with the results presented in Table 5. The χ2 statistics that appear in the last column indicate the joint significance of a variable across all employment patterns.
Three associations were shown to be significant in the multinomial model: (1) Older workers were less likely to make multiple attempts to return to work (Patterns 3, 4). The probability of being employed after multiple returns decreased by 3.4 percent with each year of age, while the probability of not being employed after multiple returns decreased by 0.5 percent. (2) Males were more likely to follow patterns that end in employment at the interview date (Patterns 1, 3). The probability of staying employed after the first absence was 61 percent greater for men than for women, while the probability of staying employed after multiple absences was 33 percent greater. (3) Finally, workers with five or more years experience with their time of injury employer were significantly more likely to be employed in their first post-injury job at the date of interview than non-union members. The probability of experiencing Pattern 1 (single absence, employed) was 35 percent greater for more experienced workers, while the probability of Pattern 2 (single absence, not employed) was 57 percent smaller.
We hypothesized that the chronic, recurrent nature of upper extremity disorders, and the risk of re-injury after return to work, contributed to the unstable post-injury work patterns experienced by many workers. To our knowledge, Pransky et al. [8] was the only previous study to identify risk factors associated with recurrence; these included shorter job tenure, employment in manual jobs, and job dissatisfaction. We did not have measures of job satisfaction or manual labor on the Ontario data, but we did find a significant association between tenure (work experience) and employment patterns, consistent with the Pransky et al. study.
Survival analyses
The repeated spells of work absence experienced by many workers with upper extremity disorders suggested that mean productivity losses associated with the disorders might be comparable to the losses associated with back pain. To quantify the losses, we computed survival curves for samples of workers with upper extremity disorders, back pain, and fractures, for first, second, third and fourth spells of work absence, and compared cumulative work absence days in the first five years after onset. The results indicated that cumulative days lost for upper extremity disorders were 83 percent of the days lost for back pain cases, but the losses attributed to upper extremity disorders were under-estimated if one focused only on the first spell of work absence.
Table 6 shows the fraction of injured workers experiencing subsequent spells of work absence attributed to a work-related injury, conditional on an initial absence from work. Workers with upper extremity disorders were much more likely to experience multiple spells than workers with either back pain or fractures. More than 25 percent of workers with upper extremity disorders experienced a second spell of work absence, compared to 18 percent of workers with back pain and 12 percent of workers with fractures. This explains why analyses limited to the first spell of work absence tended to underestimate lost workdays associated with upper extremity disorders relative to other injury groups. Beyond the second absence, the proportions of workers experiencing subsequent spells were similar for upper extremity disorders and back pain.
Cumulative lost workdays are determined by numbers of spells of work absence and their duration, so we added a duration component to the analysis by comparing survival curves for the three injury groups. Figures 1–4 show survival curves for the first, second, third and fourth spells of work absence. Mean durations of first work absence were quite long for these workers with permanent impairments: 456 days for upper extremity disorders, compared to 584 days for back pain and 541 for fractures. The survival curve for upper extremity cases exhibited the typical convex shape (Fig. 1), with 50 percent of workers returned at six months, 65 percent at one year, and 76 percent at two years. The survival curve was everywhere below the curves for back pain and fractures, indicating there were fewer days lost, on average, in the first spell of work absence for upper extremity disorders. In fact, as shown in the left side of Table 7 (lost days based on first spell only), among upper extremity cases, mean days lost in the first absence spell were 78 percent of mean days lost among back cases.
Results for the second absence spell show that the survival curves for back cases and upper extremity disorders begin to converge (Fig. 2). Mean durations of work absence were 1,209 days for fractures, 912 days for back pain, but only 717 days for upper extremity disorders. This is primarily because the samples of fractures and back cases included a greater number of lengthy, censored cases. A test for significant differences between the survival curves for backs and upper extremities could not reject homogeneity at the five percent level. Results for subsequent absence spells (Figs. 3 and 4) were similar, with the survival curves for backs and upper extremities showing greater losses than the curve for fractures.
In sum, among this sample of workers with relatively severe injuries, mean durations of first spells of work absence were longer for back cases and fractures than for upper extremity cases. On the other hand, upper extremity cases were more likely to experience subsequent spells of work absence attributed to their injury. Across the five-year period, focusing on the first spell of work absence underestimated cumulative work loss days for upper extremity cases by approximately 33 percent, compared to approximately 25 percent for back cases and 20 percent for fractures (Table 7). After five years, the cumulative losses attributed to upper extremity disorders were 83 percent of the losses attributed to back pain, compared to 78 percent when we counted only first spells of work absence. Thus, the losses for back cases and upper extremity disorders began to converge after the first spell of work absence.
Discussion
The results of this study suggest that post-injury employment outcomes for workers with cumulative trauma disorders of the upper extremities are similar to outcomes for workers with occupational back pain. Most workers, even with more severe injuries, return to work at least once after injury, but the first return to work does not necessarily mark the end of the period of work disability associated with an upper extremity disorder. Two-thirds of workers experience subsequent injury-related work absences attributed to the original injury. Focusing on the first return to work is misleading for both injury groups, but even more so for upper extremity cases, as they appear to be even more susceptible to multiple spells of work absence than back cases.
An important limitation of the study is that the data are 15 years old. Cole et al. [1], however, show that interventions to reduce repetitive strain injuries require significant amounts of time to show demonstrable outcomes, and the interventions are often hampered by institutional and organizational constraints. There have not been significant advances in treating upper extremity disorders, or in identifying effective job accommodations to facilitate returns to work, over this time period, nor have ergonomic interventions been widely adopted. Further, our literature review shows that mean workers’ compensation costs for upper extremity disorders are relatively stable over the 1990’s. Ideally, we would like to have a more recent data set with the depth and detail of the Ontario survey, but it appears that not much has changed over the last 15 years, and our results are broadly relevant to work-related upper extremity disorders today.
Another limitation is that the data are restricted to workers with permanent partial impairments, which typically represent less than 10 percent of workers’ compensation caseloads, and one-third of lost-time claims [10]. This limits the generalizability of the results, and the results should be interpreted for the relevant population only. One advantage of the restriction to permanent partial cases is that it creates a relatively homogeneous sample of more severe injuries, and we have no other direct measure of severity on the data.
The results suggest that the correlates of first returns to work are not precisely the same as the correlates of ultimate work success, at least for our sample of severe upper extremity injuries. In the return to work logistic, for example, union membership and employment in a physically demanding industry are important explanatory variables, while gender is not. In the multinomial patterns model, the opposite is true. Return to work logistic models, therefore, probably provide biased estimates of the correlates of productivity losses associated with cumulative work absences.
The results show that the patterns model of post-injury employment, developed for work-related back pain, is broadly applicable to a wide range of cumulative trauma disorders. Applying the model to different types of disorders can help identify exactly where productivity losses are likely to occur, and help target interventions at appropriate points in the recovery cycle. For example, our results suggest that workers with upper extremity disorders who are returning to work are a prime target for job accommodations, to reduce the risk of recurrence of injury and multiple spells of work absence. Yet, studies show that only about 13 percent of workers with repetitive strain upper extremity disorders receive modified work accommodations when they return to work [7.
Compared to work-related back pain, cumulative trauma upper extremity disorders are relatively under-studied. We do not have good estimates of the comprehensive costs of the disorders, nor do we have extensive analyses of return to work and duration of work absence across different worker populations. Upper extremity disorders are not as common nor as costly as back pain, but significant under-reporting to workers’ compensation suggests that the productivity losses and costs to injured workers are several orders of magnitude greater than current estimates suggest.
Notes
We use the pre-injury wage and year of injury to determine the expected temporary disability benefit, taking account of benefit maxima and minima at the time the worker was injured, and then calculate an expected replacement rate. Permanent disability benefits are not included in the models because they are not conditioned on prior wage losses or current work status, so they are not expected to have the strong work disincentives associated with temporary disability benefits. In addition, although such benefits may have an income effect on work decisions, as a practical matter they are not available in our data.
The estimated coefficient of the replacement rate variable is nearly 50 percent greater, in absolute value, than the estimated effect in a similar model for back cases.
One possible explanation is that upper extremity disorders tend to occur in occupations/industries where it is more difficult to return to work after an injury than in the occupations/industries where back injuries and fractures are more likely to occur. We do not have occupation data on the Ontario data, but we re-estimated our models with a complete set of industry controls. Other industry variables were not significant and did not change the results for the replacement rate.
References
Cole DC, Van Eerd D, Bigelow P, Rivilis I. Integrative interventions for MSDs: nature, evidence, challenges and directions. (In process.) 2005.
Fabrizio AJ. Work-related upper extremity injuries: prevalence, cost and risk factors in military and civilian populations. Work 2002;18:115–21.
Feuerstein M, Miller VL, Burrell LM, Berger R. Occupational upper extremity disorders in the federal workforce. J Occup Environ Med 1998;40:546–55.
Hashemi L, Webster BS, Clancy EA, Volinn E. Length of disability and cost of workers’ compensation low back pain claims. J Occup Environ Med 1998;39:937–45.
Johnson WG, Baldwin ML, Butler RJ. Back pain and work disability: the need for a new paradigm. Ind Relat 1998;37:9–34.
Keogh JP, Nuwayhid I, Gordon JL, Gucer PW. The impact of occupational injury on injured worker and family: outcomes of upper extremity cumulative trauma disorders in Maryland workers. Am J Ind Med 2000;38:498–506.
Morse TF, Dillon C, Warren N, Levenstein C, Warren A. The economic and social consequence of work-related musculoskeletal disorders: The Connecticut Upper-Extremity Surveillance Project (CUSP). International Journal of Occupational and Environmental Health 1998;4:209–16.
Pransky G, Benjamin K, Hill-Fotouhi C, Fletcher KE, Himmelstein J. Occupational upper extremity conditions: a detailed analysis of work-related outcomes. J Occup Rehabil 2002;12:131–8.
Roquelaure Y, Cren S, Rousseau F, Touranchet A, Dano C, Fanello S, Penneau-Fontbonne D. Work status after workers' compensation claims for upper limb musculoskeletal disorders. Occup Environ Med 2004;61:79–81.
Sengupta I, Reno V, Burton JF Jr Workers’ compensation: benefits, coverage, and costs, 2003. Washington DC: National Academy of Social Insurance, 2005.
Silverstein B, Viikari-Juntura E, Kalat J. Work-related musculoskeletal disorders of the neck, back and upper extremity in Washington state: 1990–1998. Technical report no. 40-4A-2000. Olympia, WA: SHARP Program, 2000.
Silverstein B, Welp E, Nelson N, Kalat J. Claims incidence of work-related disorders of the upper extremities: Washington state, 1987 through 1995. Am J Public Health 1998;88:1827–33.
Yassi A, Sprout J, Tate R. Upper Limb Repetitive Strain Injuries in Manitoba. Am J Ind Med 1996;30:461–72.
Author information
Authors and Affiliations
Corresponding author
Additional information
Prepared for a Meeting on: Upper Extremity Disorders in the Workplace; Sponsored by: Office Ergonomics Research Committee, Annapolis, Maryland, September 23–24, 2005
Rights and permissions
About this article
Cite this article
Baldwin, M.L., Butler, R.J. Upper extremity disorders in the workplace: Costs and outcomes beyond the first return to work. J Occup Rehabil 16, 296–316 (2006). https://doi.org/10.1007/s10926-006-9043-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-006-9043-2