Abstract
Aim: Musculoskeletal disorders (MSD) are a leading cause of work-related disability. This investigation explored the impact of MSD comorbid with depression and anxiety disorders, on labor force activity. Methods: The Australian Bureau of Statistics provided confidentialized data files collected from a household sample of 37,580 people. MSD, affective, and anxiety disorders were identified and employment restrictions were assessed at four levels of severity. Results: Anxiety and depression of six months duration was present in 12.1% of people with MSD. Comorbidity magnified the negative impacts of single conditions on labor force activity. Most at risk were people with back problems and comorbid depression, people with arthritis or other MSD and comorbid anxiety, males with MSD and comorbid depression, and females with MSD and comorbid anxiety. Conclusions: The results suggest that the occupational rehabilitation needs of people with MSD comorbid with depression or anxiety may currently be underestimated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal disorders (MSD) are the leading cause of work-related disability in Australia, representing 34.0% (237,103 people aged 16–64 years) of all Disability Support Pension (DSP) recipients as at June 2004 [1]. People with psychological or psychiatric disabilities constitute the next largest group at 25.4% of DSP recipients, or 177,129 people. In Europe, two of the most prevalent workplace health problems are backache (33% of the workforce) and neck or shoulder pain (23%) [2]. In the USA, occupational MSDs are the leading cause of work disability [3]. Of the psychiatric disorders, depression and anxiety disorders are the most prevalent and have substantial impacts on labor force participation and employment status throughout the working life [4–10].
A greater understanding of musculoskeletal disorders comorbid with anxiety and depression is needed to advance our knowledge of how psychosocial factors impact on occupational disability and rehabilitation. In this context two types of psychosocial risk factors have been identified. Type I, worker-related psychosocial factors, are distinguished from Type II, workplace or system related factors [11]. Among Type I risk factors, comorbid anxiety and depression are plausible candidates for intervention during occupational rehabilitation [12]. For instance, cognitive and emotional reactions to pain in MSDs are associated with greater functional limitations [13].
A possible mechanism is that symptoms of anxiety or depression adversely influence an individual's problem solving strategy, particularly in the presence of pain, which in turn results in greater disability through greater perceived functional loss [14]. Greater perceived functional limitations are subsequently associated with a greater risk of not resuming work among employees with work-related upper extremity disorders [15]. These studies highlight the possibility that anxiety and depression comorbid with musculoskeletal disorders and associated pain conditions, increases work-related disability and exacerbates the impact of both types of disorders on occupational rehabilitation outcomes.
However, at a population level little is known about how MSD combine with anxiety and depression to impact on labor force activity. In Australia, population level correlates of labor force activity associated with depression and anxiety disorders have been documented [8–10]. The impact of anxiety and depression on labor force activity is important because these disorders have a 12 month prevalence of 5–10% in the adult population yet often remain undetected and untreated [16–18]. Furthermore, among those that seek treatment a substantial proportion does not receive optimal treatment [19–20], and the benefit of treatment to labor force activity remains unclear [8].
This investigation sought to delineate the impact of MSD comorbid with depression and anxiety disorders on labor force activity among people of working age. The aim was to examine any impact on labor force activity associated with comorbidity in order to identify implications for policy makers and occupational rehabilitation practitioners. Four issues were explored: (i) the prevalence of MSD comorbid with anxiety or depression; (ii) whether some categories of MSD were more prone to comorbid anxiety or depression than others; (iii) whether sex or age differences were apparent; and (iv) whether any particular comorbid sub-group was more adversely affected in terms of impacts on labor force activity.
Methods
Data source
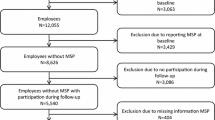
The Australian Bureau of Statistics (ABS) provided confidentialized data files from the Survey of Disability, Ageing and Carers (SDAC, 1998) conducted from 16 March to 29 May 1998 [21–22]. Data were collected from a household sample of 37 580 persons. The survey was authorised by the Australian Federal ‘Census and Statistics Act, 1905.’ The ABS protected the confidentiality of individuals surveyed in the data set by removing identifiable households (households with rare combinations of demographic characteristics) from the file, and where necessary, by aggregating variables to suppress the detail available. Hence, data from this investigation may not exactly match that reported elsewhere by the ABS. Other than reducing the total sample size by 1.5%, confidentiality protections did not limit our analyses.
Sampling
The survey design and operation are detailed elsewhere [8–10, 21–22]. The survey took place in both urban and rural areas in all states and territories, except in remote and sparsely settled parts of Australia. Statistical adjustments for not sampling remote residents in the Northern Territory were applied because unlike other states, approximately 20% of Northern Territory residents live in remote areas. Participants included all persons except prisoners, non-Australian diplomatic personnel, and members of non-Australian defence forces stationed in Australia. The survey sample was selected using multistage sampling techniques based on census collection districts. The effective sample included 15 316 private dwellings (one per 400 private dwellings in Australia); and 399 non-private dwelling units (i.e. hotels, motels, boarding houses, educational and religious institutions, guest houses, construction camps, short-term caravan parks, youth camps and camping grounds, staff quarters, and self-care components of retirement villages). Non-private dwellings were selected separately from private dwellings to ensure adequate representation. Each non-private dwelling was given a chance of selection proportional to the average number of persons accommodated.
Information was obtained from 93% of households sampled. Completed interviews were obtained from 35 569 persons or 94.4% of the total sample. Partial non-responses included income-refusal, 1.9% of the total sample; income-don't know 3.4%. Full non-responses included refusals 0.1%; non-contacts 0.1%; and language problems, death, illness or other, less than 0.05%. The secondary sampling strategy captured people of working age (15–64 years) in six mutually exclusive diagnostic categories (see column 1 of Table 2). Application of ABS population weights [21–22] revealed an estimated 1.3 million people of working age with ICD-10 MSD which had persisted or were likely to persist for 6 months or more.
Identifying persons with depression, anxiety, and MSD
All categories of health conditions were systematically investigated and coded according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision [23]. Interviews were conducted in the field using a computer-assisted interview protocol with pick lists to aid the identification of health conditions underlying self-reported activity restrictions. A large proportion of health conditions were coded automatically in the field. Experienced ABS household interviewers, who were not medically trained, received three days training in the computer assisted interview schedule and the embedded ICD-10 classification system. The 1998 schedule was updated from a similar survey conducted in 1993.
Musculoskeletal, affective and anxiety disorders were identified from converging sources of information: by self-report, by interviews with a responsible adult of the household, or by another responsible adult person assisting with the interview. Responsible adults typically included legal guardians, parents, first degree relatives, and adults with formal caring responsibilities. The musculoskeletal and mental health condition sections of the interview each began with the question: “Does anyone in the household need to be helped or supervised in doing things because of a (physical disorder/mental illness) or condition?” This question was followed by a series of open and closed questions, similar to a decision tree, to reveal activity and employment restrictions, the nature of disabilities, and underlying health conditions.
For this secondary investigation ICD-10 classifications of mental disorders were identified hierarchically. Anxiety as the primary disorder was excluded when comorbid with schizophrenia, other psychoses, and depression. Anxiety as the primary condition included: phobias (agoraphobia, social phobia and specific phobia, ICD-10 code F40); panic disorder and generalized anxiety disorder (F41); obsessive compulsive disorder (F42); acute stress disorder and posttraumatic stress disorder (F43); and other neurotic, stress related or somatoform disorders (F44–48). ICD-10 classifications of depression and mood affective disorders (F30–39) excluded postnatal depression and comorbidity with schizophrenia and other psychoses. Depression and affective disorders included mania (F30), bipolar affective disorder (F31), depression (F32–33), persistent mood disorders (F34), and other affective disorders (F38–39).
MSD comprised: arthritis and related disorders (M00-19); acquired deformities of joints and limbs (M20–21); back problems (M40–54); occupational overuse syndrome (M70); synovitis or tenosynovitis (M65); other muscle and soft tissue disorders (M60-63, M66–68, M71–79); osteoporosis (M80–81); other acquired limb and joint deformities (M95); and other MSD (M22–36, M82–94, M96–99). For analysis these were aggregated into back problems (59.7% of the non-comorbid musculoskeletal disorder sample), arthritis and related disorders (32.0%), and other MSD (8.3%).
Text fields recorded any disorders reported which did not appear to match items on the field computer pick lists. Codes for all text entries were determined post interview by more experienced ICD-10 coders back at the office. This was necessary because some disorders were collected under more general descriptive categories within the pick lists. For instance, acute stress disorder (F43.0) and posttraumatic stress disorder (F43.1) were both coded under the description ‘nervous tension/stress’. To ensure accuracy, all interviews were checked until each interviewer achieved 90% agreement or higher with an experienced coder. Sample monitoring of coding continued throughout the data collection phase. Although no reliability and validity information are available for the interview schedule as a whole, it has been revised since its first use in a similar large population survey in 1993. The complete interview protocol for the 1998 survey is available from the ABS.
Disability, long-term health conditions, and employment restrictions
The survey used the World Health Organization's International Classification of Impairments, Disabilities and Handicaps [24] as a framework to identify disability and the associated level of restriction. Participants had a disability if they had an impairment or restriction in everyday activities that was likely to last for six months or more. It was possible to have musculoskeletal, depression or anxiety disorders as a long-term health condition, but without activity restrictions and hence, without a disability.
Employment restrictions were assessed at four levels of severity (profound, severe, moderate, and mild) in parallel with the definitions of independent living activity restrictions (not examined in this investigation) and were intended to apply to both physical and mental disorders. Profound was defined as unable to perform employment or a core activity, or always needing assistance. Severe was defined as needing assistance to perform employment or a core activity. Moderate referred to not needing assistance, but having difficulty. Mild referred to having no difficulty, but using aids or equipment because of disability. Further descriptions of terms and variables used in the survey are available [22].
Analysis
The analysis was restricted to people of working age (15–64 years) with MSD, depression or anxiety disorders as the primary underlying conditions in the household component of the survey. Depression comorbid with anxiety was incorporated within the depression group. Population weights were provided by the ABS as an individual level variable [22, p. 21]. These estimates provided the starting point for calculation of standard errors in SAS [25] using jack-knife replication, an established method of standard error estimation in population surveys [26–27]. Estimates with standard errors less than 25% of the estimate value are considered by the ABS as sufficiently reliable for most purposes. Relative standard errors greater than 25% are marked accordingly in the tables provided. Statistically significant differences in prevalence estimates were examined by Z-scores for difference. Bonferroni adjustment to a 99% confidence level accommodated multiple pair-wise comparisons.
Results
MSD of at least six months duration were found in 1 457 210 Australians of working age in 1998 (SE 23 085). Among those 12.1% had comorbidity with respect to anxiety or depressive disorders of six months or more duration. The most prevalent of the two comorbid disorders was anxiety representing 7.1% of people with MSD (74 414, SE 5 157). Comorbid depression affected a further 5.0% of the musculoskeletal disorder group (36 845, SE 4 008), see Tables 1 and 2.
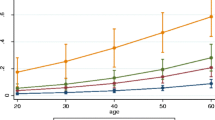
MSD comorbid with anxiety were similarly prevalent among males and females at ages 15–34 years. However at ages 35–54 and 55–64 years, the proportions of females with comorbid anxiety exceeded that of males, although the Z-scores of difference were not significant at the 99% confidence level. A similar gradient emerged in favor of females with MSD comorbid with depression, which again did not reach statistical significance. MSD comorbid with anxiety were more prevalent than MSD comorbid with depression (p < .001, in both sexes, see Table 1).
Labor force participation decreased monotonically across healthy controls, MSD, anxiety, depression, comorbid anxiety, and comorbid depression (p < .001 for all pair-wise comparisons, see Table 2). The proportion not in the labor force ranged from 19.9% among healthy controls to 62.6% among people with MSD and comorbid depression. Although the proportion looking for work remained relatively stable in comparison, significantly fewer people with MSD looked for work compare to healthy controls (p < .001). The proportion looking for work increased to 7.5% among people with anxiety disorders compared to MSD (5.2%, p < .001). Compared to the anxiety disorder group, the proportion looking for work was similar among those with depression, comorbid anxiety and comorbid depression (differences were not significant at the 99% confidence level).
The relative stability among proportions looking for work indicated that the greatest effect of these disorders on labor force activity, is in terms of reduced labor force participation. This indicates that comorbid disorders are not merely associated with increased unemployment, but are associated with job seeker discouragement, where job seekers cease actively looking for work. Among particular subgroups, strong effects of comorbid anxiety or depression emerged. For instance, the proportion of people with MSD comorbid with depression and not in the labor force, was three times that of healthy Australians, and almost twice that of people with MSD alone.
Back problems were the most prevalent form of MSD, followed by arthritis (p < .001, see Table 3). Each MSD subgroup had a unique age profile. As expected, arthritis prevalence increased with age such that 10.0% were aged 15–34 years; 45.4% were 35–54 years; and 44.6% were 55–64 years. The ‘other’ musculoskeletal subgroup was more evenly distributed with 25.5% aged 15–34 years, 49.3% 35–54 years, and 25.2% 55–64 years. The prevalence of back conditions was similar to that of other MSD at 15–34 years (25.1%), were more prevalent at 35–54 years (55.1%), and were less prevalent at ages 55–64 years (19.8%). Although comorbid anxiety and depression occurred in similar proportions within each of the three MSD sub-groups, depression was marginally more prevalent among other MSD (5.0% vs. 2.6% among back problems, and 1.9% among arthritis, see Table 4). Due to high relative standard errors these proportional differences did not reach statistical significance.
Of the non-comorbid musculoskeletal subgroups, the arthritis subgroup had the greatest negative effect on labor force participation (p < .001 for all three comparisons). With comorbidity, the greatest impact on labor force participation was among people with back problems and comorbid depression (70.2% not in the labor force, see Table 4). The next greatest effect was associated with other MSD and comorbid anxiety (69.2% not in the labor force). Comorbid depression had a proportionally greater negative effect than comorbid anxiety on labor force participation among those with back conditions at a trend level (p=.037). Comorbid anxiety promised greater negative leverage on arthritis (p=.013), but not among ‘other’ MSD. Within each of the MSD subgroups, comorbid anxiety or depression exacerbated the effects on labor force participation, in an effect range varying from 25% to over 200% (see Table 4).
Comorbid disorders affected males and females differently. Three times as many females had MSD and comorbid anxiety, than males had MSD and comorbid depression (p < .001). Females with MSD and comorbid anxiety were more likely to exit the labor force than males (62.9% vs. 48.9%, p=.009, see Table 5). This indicates a greater resilience among males to the adverse effects of comorbid anxiety. Whereas, in terms of comorbid depression, the labor force participation of males and females was similar in magnitude (63.7 & 60.9% respectively) to that of females with comorbid anxiety (see Table 5).
At ages 15–34 years almost as many males as females had MSD and comorbid anxiety (48.6 vs. 51.4%) while at ages 55–64 years females with MSD and comorbid depression outnumbered males (64.2 vs. 35.8%). In terms of labor force activity, subgroup differences (see Table 5) revealed that the impact of comorbid disorder also depended on sex. The greatest labor force disadvantage was found among males with comorbid depression (25.9% employed, see Table 5), followed by females with comorbid anxiety disorders (28.6% employed, see Table 5). Furthermore, when seeking employment these two groups were less likely to be successful, as 13.2% of males with comorbid depression, and 8.5% of females with comorbid anxiety were actively looking for work (vs. 5.2% among those with MSD alone, p < .001 for both comparisons). Although males with comorbid anxiety were the least adversely affected (45.5% employed), the impact on this subgroup was substantial compared to people with no comorbid anxiety or depression (61.4% employed, p < .001).
Discussion
These results indicate a substantial (12.1%) prevalence of comorbid depression and comorbid anxiety among people of working age with MSD. This prevalence concerns only the more severe and persistent forms of anxiety and depression with current or expected durations of six months or more. Hence, this is likely to be a conservative estimate of those with MSD experiencing problems with anxiety or depression. The prevalence of anxiety comorbid with MSD was similar for both males and females at ages 15–34 years, increasing markedly for females thereafter. Comorbid anxiety was more prevalent than comorbid depression, yet comorbid depression had a greater overall impact on labor force activity (see Table 2). Most at risk were people with back problems and comorbid depression, people with arthritis or other MSD and comorbid anxiety, males with MSD and comorbid depression, and females with MSD and comorbid anxiety. In these subgroups the impact on labor force activity approached that found among people with psychotic disorders (21.1% employed) [28], a group typically requiring the most intensive and continuous forms of vocational assistance.
Furthermore, the prevalence of comorbid anxiety and depression identified in this investigation does not capture sub-clinical anxiety or depression, general psychological distress, related somatoform, substance misuse, or adjustment disorders, which are also known to co-occur with MSD. Psychosocial factors are recognized as important in occupational rehabilitation of MSD [11–12] and psychological conditioning is already accepted as a key ingredient of effective occupational rehabilitation for people with non-specific MSD [29]. However, these results suggest an even more comprehensive approach is needed, one which coordinates psychological assessment and treatment as a routine component of occupational rehabilitation for people with comorbid musculoskeletal and psychiatric disabilities.
Addressing the work-related disability and increased labor force disadvantage associated with these comorbid conditions with respect to a particular individual, may be complicated by multi-factorial sources of work-related disability. For instance, treatments for MSD, pain, anxiety and depression, are seldom 100% effective. Complex disorder combinations, multiple partially effective treatments, the possibility of deterioration with potential for relapse, will continue to challenge occupational rehabilitation providers. However, until more is known about how best to manage these comorbid disorders in occupational rehabilitation, more effective and specific treatments can be sought which target particular employment restrictions. In addition, workplace strategies can be broadened to accommodate, as far as possible, the comorbid mental health problems identified.
Implications for policy makers, income support providers and practitioners
The most disadvantaged subgroups of people with MSD comorbid with anxiety or depression show impacts on labor force activity approaching that found among people with psychotic disorders. This means that some people may need more intensive and continuous forms of vocational rehabilitation than is typically provided to people with MSD alone. Although the ingredients of evidence-based employment services designed specifically for people with psychiatric disabilities have been identified [30], there is as yet no evidence that all these ingredients are needed for people with MSD comorbid with anxiety or depression. It is plausible that some blending of effective ingredients in both approaches to occupational rehabilitation may be required. In the meantime, policy makers can help by increasing the availability of more continuous and intensive forms of vocational assistance. Income support providers could assist by incorporating anxiety and depression screening into routine assessments of income support entitlements and formal referrals to occupational rehabilitation, to ensure that those with more challenging comorbid psychiatric disorders are referred to the most appropriate type of service.
Limitations
This survey has several important limitations which have been discussed previously [8–10]. Limitations include methodological differences in depression and anxiety specifications and classification protocols, which mean these findings are not readily compared to other population surveys [18, 31–32]. The study was limited by the use of ICD-10 classifications by lay interviewers, a necessary method given the large scale nature of the survey, but less rigorous than standardised screening or diagnostic interviews. As a minimum duration of six months was required for all health conditions identified, this can mean less sensitivity compared to other diagnostic schema [33] and an emphasis on more severe and persistent disorders. As mental disorders were not the primary focus of the SDAC 1998, not all relevant population sub groups were included in the sampling strategy. Prisoners, indigenous communities, residents of psychiatric institutions, and homeless persons were not specifically targeted. Limited information was available on ethnicity, language spoken at home, the type and nature of treatments received and the nature of employment assistance obtained.
The cross-sectional nature of this survey precluded discovering relationship directions and precluded an empirical determination of whether musculoskeletal disorders (and associated pain) are an antecedent or a consequence of clinical anxiety or depression. Another issue which could not be investigated concerns the extent that sub-clinical emotional distress hinders occupational rehabilitation outcomes. Although general emotional distress is recognized as an important Type I psychosocial risk factor [11–12] it is unclear from previous studies whether this has been of a clinical magnitude or not. Another issue that could not be investigated here, is the potential for interaction between anxiety and depression and Type II psychosocial risk factors, the systemic and other work-related sources of psychological distress [11]. This is a promising area for further investigation because it is plausible that at an individual level these comorbid disorders may interact dynamically with workplace and systemic psychosocial risk factors.
Conclusion
This investigation found that MSD and comorbid anxiety and depression magnified single disorder impacts on labor force participation, part-time and full-time employment, and job seeking activities. Most at risk were people with back problems and comorbid depression, people with arthritis or other MSD and comorbid anxiety, males with MSD and comorbid depression, and females with MSD and comorbid anxiety disorders. These subgroups experienced a level of labor force disadvantage approaching that found among people with psychotic disorders, a group for whom the most intensive and continuous forms of occupational rehabilitation are reserved. Individually tailored occupational rehabilitation programs can be enhanced by coordinated assessment and treatment of anxiety and depression where links to MSD-related pain are also taken into account. In addition, more research is urgently needed to explore how comorbid anxiety and depression increase work-related disability and how these disorders contribute to both Type I and Type II psychosocial risk factors in occupational rehabilitation.
References
Department of Employment and Workplace Relations. Characteristics of Disability Support Pension customers—June 2004. http://www.jobable.gov.au/DSPreport/2004/sec2.asp
European Communities. Work and health in the EU: A statistical portrait data 1994–2002. Office for Official Publications of the European Communities. Luxembourg: Panorama of the European Union.
Melhorn JM. Occupational orthopaedics in this millennium. Clin Orthop 2001;385:23–35.
Lerner D, Adler DA, Chang H, Lapitsky L, Hood MY, Perissinotto C, et al. Unemployment, job retention, and productivity loss among employees with depression. Psychiatr Serv 2004;55(12):1371–8.
Berndt ER, Finkelstein SN, Greenberg PE, Howland RH, Keith A. Workplace performance effects from chronic depression and its treatment. J Health Econ 1998;17:511–35.
Conti DJ, Burton WN. The economic impact of depression in a workplace. J Occup Environ Med 1994;36(9):983–8.
Schoenbaum M, Unutzer J, McCaffery D, Duan N, Sherbourne C, Wells KB. The effects of primary care depression treatment on patients’ clinical status and employment. Health Serv Res 2002;37(5):1145–58.
Waghorn G, Chant D. Labour force activity by people with depression and anxiety disorders: a population level second order analysis. Acta Psychiatr Scand 2005;112:415–24.
Waghorn G, Chant D. Employment restrictions among persons with ICD-10 anxiety disorders: characteristics from a population survey. J Anxiety Disord 2005;19:642–57.
Waghorn G, Chant D, White P, Whiteford H. Disability, employment and work performance among persons with ICD-10 anxiety disorders. Aust N Z J Psychiatr 2005;39:55–66.
Sullivan MJL, Feuerstein M, Gatchel R, Linton SJ, Pransky G. Integrating psychosocial and behavioral interventions to achieve optimal rehabilitation outcomes. J Occup Rehabil 2005;15:475–89.
Feuerstein M, Berkowitz SM, Haufler AJ, Lopez MS, Huang GD. Working with low back pain: workplace and individual psychosocial determinants of limited duty and lost time. Am J Ind Med 2001;40:627–38.
Feuerstein M, Harrington CB, Lopez M, Haufler A. How do job stress and ergonomic factors impact clinical visits in acute low back pain? A prospective study. J Occup Environ Med 2006; in press.
Shaw WS, Feuerstein M, Haufler AJ, Berkowitz SM, Lopez MS. Working with low back pain: problem solving orientation and function. Pain 2001;93:129–37.
Feuerstein M, Shaw WS, Lincoln AE, Miller VI, Wood PM. Clinical and workplace factors associated with a return to modified duty in work-related upper extremity disorders. Pain 2003;102:51–61.
Andrews G, Hall W, Teesson M, Henderson S. The Mental Health of Australians. National Survey of Mental health and Wellbeing. Report 2. Canberra: Commonwealth Department of Health and Aged Care, 1999.
Henderson S, Andrews G, Hall W. Australia's mental health: an overview of the general population survey. Aust N Z J Psychiatr 2000;33:197–205.
Kessler RC, McGonagh KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen U, Kendler KS. Lifetime and 12-month prevalence of DSM-II-R psychiatric disorders in the United States. Arch Gen Psychiatr 1994;51:8–19.
Andrews G, Hunt C. Treatments that work in anxiety disorders. Med J Aust 1995;168:628–34.
Issakidis C, Sanderson K, Corry J, Andrews G, Lapsley H. Modeling the population cost-effectiveness of current and evidence based optimal treatment for anxiety disorders. Psychol Med 2004;34:19–35.
Australian Bureau of Statistics. Survey of disability, ageing and carers, Australia. Summary of findings, Cat. 4430.0. Canberra: Australian Government; 1998.
Australian Bureau of Statistics. Survey of Disability, Ageing and Carers, Australia. Technical Paper. Confidentialised Unit Record File. Canberra: Australian Government, 1998.
World Health Organization. International classification of diseases. 10th ed. (ICD-10). Geneva: World Health Organization; 1993.
World Health Organization. International classification of impairments, disabilities and handicaps. Geneva: World Health Organization; 1980.
SAS Institute. User's guide 8.02. Cary, NC: SAS Institute; 2003.
Kish L, Frankel MR. Balanced repeated replications for standard errors. J Am Stat Assoc 1970;65:1071–94.
Särndal CE, Swensson B, Wretman J. Model assisted survey sampling. New York: Springer-Verlag; 1992.
Waghorn G, Chant D, White P, Whiteford H. Delineating disability, labour force participation and employment restrictions among persons with psychosis. Acta Psychiatr Scand 2004;109:279–88.
Meijer EM, Sluiter JK, Frings-Dresen MHW. Evaluation of effective return-to-work treatment programs for sick-listed patients with non-specific musculoskeletal complaints: a systematic review. Int Arch Environ Health 2005;78:523–32.
Bond GR. Supported employment: evidence of an evidence-based practice. Psych Rehab J 2004;27:345–59.
Meltzer H, Gill B, Pettigrew M, Hinds K. OPCS Surveys of psychiatric morbidity in Great Britain. Report 1. The prevalence of psychiatric morbidity among adults living in private households. London: OPCS Social Surveys Division, HMSO; 1995.
Robins LN, Regier DA, editors. Psychiatric disorders in America: The epidemiological catchment area study. New York: The Free Press; 1991.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Waghorn, G., Chant, D. & Lloyd, C. Labor force activity among Australians with musculoskeletal disorders comorbid with depression and anxiety disorders. J Occup Rehabil 16, 235–246 (2006). https://doi.org/10.1007/s10926-006-9018-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-006-9018-3