Abstract
Breast cancer is the most cause of death for women above age 40 around the world. In this paper, we propose a method to detect microcalcifications in digital mammography images using two-dimensional Discrete Wavelets Transform and image enhancement techniques for removing noise as well as to get a better contrast. The initial step is applying a preprocessing techniques to improve the edge of the breast and then segmentation process (Region of interest) for eliminating some regions in the image, which are not useful for the mammography interpretation. Then unsharp masking and histogram modification technique has used to enhance the contrast of the image and to clarify some details like microcalcifications. Lastly, Discrete Wavelets Transform applied for detecting the abnormality. The proposed method has evaluated using the Mammographic Image Analysis Society (AS) mammography databases. The proposed method has achieved acceptable results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A malignant tumor that commence in the cells of the breast is named breast cancer [1]. In modern countries, medical statistics have estimated that one woman in eight will contract a breast cancer. Malignant tumors are more probable to appear in breast tissues of women age up to 40, and they represent 35% of the abnormalities detection in a woman’s breasts. Breast cancer is presently accountable for more than 30% of death by cancer in women, which is about 1% of all deaths worldwide. Breast cancers also concern men since it represents 1.5% of all cancer deaths in men [2, 3].
The early detection of breast cancer is remarkable effort because of the treatment of an undeveloped and non-metastasized tumor will not require massive surgical inter-ventions.
Microcalcifications are deposits of calcium in breast tissue [4]. It is small size lesions, typically range in size from 0.05 to 1 mm in diameter. With these dimensions, microcalcifications are comparatively hard to detect [1, 5].
There is a high correlation between the presences of microcalcifications, breast cancer, particularly when a number of microcalcifications collected together is labeled a cluster, and it may be a good sign of cancer. A cluster is well-defined as at least three microcalcifications within a 1-cm2 area. As a result, an correct detection of microcalcifications is necessary to any early detection of the common of breast cancers [6, 7].
In the literature, various numbers of techniques has described to detect and classify the presence of microcalcifications in digital mammograms as benign or malignant.
Computer-based methods for the detection of microcalcifications in digital mammograms have designed [8–11]. These methods based on different image technique in which a signal-suppressed image has subtracted from a signal-enhanced image to remove structured background in the mammogram. Global and local thresholding techniques have used to extract potential microcalcifications signals. Subsequently, signal extraction criteria have imposed on the potential microcalcifications to make a distinction true positives from noise and speckles.
Karssemeijer [12, 13] developed a statistical method for detection of microcalcifications in digital mammograms. The method based on the use of statistical models and the general framework of Bayesian image analysis.
Many researchers have used 2D wavelet coefficients for microcalcifications detection in mammography images [14–17].
A malignant tumor that commence in the cells of the breast is named breast cancer [1]. In modern countries, medical statistics have estimated that one woman in eight will contract a breast cancer. Malignant tumors are more probable to appear in breast tissues of women age up to 40, and they represent 35% of the abnormalities detection in a woman’s breasts. Breast cancer is presently accountable for more than 30% of death by cancer in women, which is about 1% of all deaths worldwide. Breast cancers also concern men since it represents 1.5% of all cancer deaths in men [2, 3].
The early detection of breast cancer is remarkable effort because of the treatment of an undeveloped and non-metastasized tumor will not require massive surgical inter-ventions.
Microcalcifications are deposits of calcium in breast tissue [4]. It is small size lesions, typically range in size from 0.05 to 1 mm in diameter. With these dimensions, microcalcifications are comparatively hard to detect [1, 5].
There is a high correlation between the presences of microcalcifications, breast cancer, particularly when a number of microcalcifications collected together is labeled a cluster, and it may be a good sign of cancer. A cluster is well-defined as at least three microcalcifications within a 1-cm2 area. As a result, an correct detection of microcalcifications is necessary to any early detection of the common of breast cancers [6, 7].
In the literature, various numbers of techniques has described to detect and classify the presence of microcalcifications in digital mammograms as benign or malignant.
Computer-based methods for the detection of microcalcifications in digital mammograms have designed [8–11]. These methods based on different image technique in which a signal-suppressed image has subtracted from a signal-enhanced image to remove structured background in the mammogram. Global and local thresholding techniques have used to extract potential microcalcifications signals. Subsequently, signal extraction criteria have imposed on the potential microcalcifications to make a distinction true positives from noise and speckles.
Karssemeijer [12, 13] developed a statistical method for detection of microcalcifications in digital mammograms. The method based on the use of statistical models and the general framework of Bayesian image analysis.
Many researchers have used 2D wavelet coefficients for microcalcifications detection in mammography images [14–17].
Mammogram database
The Mammography Image Analysis Society (MIAS), which is an organization of UK research groups interested in the understanding of mammograms, has created a digital mammography database (ftp://peipa.essex.ac.uk).
The database used in experiments of this work has taken from the MIAS because it contains complete information about abnormalities of each mammography image. The X-ray films in the database have been carefully selected from the United Kingdom National Breast Screening Program and digitized with a Joyce-Lobel scanning microdensitometer with a resolution of 50 μm × 50 μm, 8bits represent each pixel with 1024 × 1024 pixel size and at 256 Gy levels.
The images are in the grayscale file format (.pgm) (Portable Gray map). The used database contains left and right breast images for 161 patients. Its quantity consists of 322 images, which belong to three types such as Normal, benign and malignant. There are 208 normal, 63 benign and 51 malignant (abnormal) images.
Proposed method
Briefly, Fig. 1 depicts the flowchart steps of this method.
Preprocessing
This step enhances the breast’s edge before segmenting the region of interest (ROI) from the mammography images; this process has performed by the Logarithm transformation tool for dynamic range manipulation.
Segmentation
The aim of image segmenting is to decrease the data volume, decrease the complexity of time, and the procedure searching for (ROI) that includes a lesion with high probability. This phase removes the parts of the image that aren’t beneficial for the mammography interpretation and extract only the area of the image that relates to the breast. This step has completed by binarization the image with automatic threshold for locating a binary image and morphological operations for the extract the area of the breast.
Enhancement
Enhancement step divides into two stages:
Unsharp masking
The unsharp masking is used for enhancing the quality of mammography image, emphasizing the high frequency contents, improving strong edges, and the detailed information. Technique of Laplacian linear high pass filter has employed. This technique is a simple, effective and extensively applied in some of applications, on the other hand, it has the drawback that the linear high pass filter is sensitive to the noise. The output image from this stage has obtained by Eq. (1).
Where g 1 (x, y) are output image, g (x, y) is the input image (output of preprocessing step), α is the factor of improvement that controls the level of improvement of contrast and f 1(x, y) is the filtered image by linear high pass filter.
As mentioned above, we used Laplacian linear high pass filter for obtaining thef 1(x, y), Eq. (2) describes this process:
This equation has implemented by the convolution mask below:

Additional putting into digital practice of the Laplacian takes in consideration all eight neighbors of the mention pixel in the input image and has executed by the convolution mask below:

There is another expression for Laplacian that has implemented by the convolution mask below:

In this work, we used the three types of Laplacian when implementing the experiments.
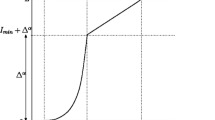
Histogram modification
Image histogram represents the relative frequency of occurrence of different gray levels in the image. Histogram modification techniques are good-looking due to their effortlessness and speed. Firstly, a transform function has derived from a chosen histogram and the histogram of an input image. The transform function is regularly nonlinear and for continuous functions, a unenthusiastic transform has accomplished.
Once the unsharp mask is applied, proceeds to modify the levels of gray to generate a better visualization of the microcalcifications in the image. Here it needs to select a threshold, which allows separating the values from the intensity of the corresponding pixels to the microcalcifications and the rest of the image. In this stage, we used two approaches for histogram modification:
-
A: Exponential Modification Approach
Mathematically, this approach has described in Eq. (3).
where g 2 is output image, g 1 is image from the unsharp mask stage, T is a threshold, c is a positive integer and m represents the mean values in the mammography image.
-
B: Linear Modification Approach
Mathematically, this approach has described in Eq. (4).
where g 2 is output image, g 1 is image from the unsharp mask stage, T is the threshold and c is a positive integer number.
Detection
Detection step involves many processes to detect in result the microcalcifications, these processes has described as:
Wavelets analysis
A significant branch of CADe approaches in mammography utilizes wavelet transforms for feature improvement. This study applies the 2-Dimensional Discrete Wavelet Transform, which has appeared in Eq. (5).
With a = 2j , b = k.2j, j, k ∈ N.
where f is the original image, g is the wavelet function, a is a scale factor of the wavelet function, b is a position parameter of the wavelet function, and C (a, b) is the set of obtaining coefficients. Inverse process has considered in Eq. (6).
where ψ is the inverse wavelet function used to rebuild the image.
The multiresolution demonstration has accomplished by 2-D discrete wavelet transform, segment the frequency spectrum of an image f(x,y) into a lowpass subband image cAj and a set of band-pass subband images cDHj, cDVj, cDDj, j = 1,…,L, where L denotes the number of levels for a representation, cDHj is molded by lowpass filtering the rows tracked by highpass filtering the columns, and is consequently sensitive to horizontally oriented features.
In the same manner, the cDVj covers vertically oriented structure, and cDDj includes primarily diagonal structure.
A waterfall of analysis/synthesis (A/S) filter banks puts through multiresolution representations. The discrete wavelet transform utilized 2-different wavelet mothers: h (x) for multiresolution decomposition (analysis) and g (x) for reconstruction (synthesis) of the original image from its multiresolution representation.
Fig. 2 demonstrations the execution of one-level (L = 1) multiresolution representation of the discrete wavelet transform, which splits orientations into three bands.
As shown in Fig. 2, the forward 2-D wavelet transform is executed using a bank of the 1-D lowpass (h1 (x)) and highpass (h2 (x)) analysis filters. The restoration progression, or reverse wavelet transform, is similarly calculated via 1-D synthesis filters, g1 (x) and g2 (x).
Wavelet-based image decomposition reads as an image filtering process. For input image I of size 2n x 2n, wavelet-based subband decomposition has achieved as follows: The wavelet filters h1 (x) and h2 (x) have implemented to the rows of the image I. The filter h1 (x) is a lowpass filter with frequency response H1 (w) and h2 (x) is a high pass filter with frequency response H2 (w). By filtering the image I with H1 (w), lowfrequency is attained information.
By way of filtering the image with H2 (w), the highfrequency information has gotten (edges). After down_sampling by a factor of two, two subbands have found H1rI and H2rI (the subscript r proposes that the filters have been stratified to the rows of the image I). At that point the filters H1 (w) and H2 (w) have used to the columns of the subbands H1rI and H2rI, tracked by down_sampling by a factor of two, and the following four subbands have attained cAj, cDHj, cDVj, and cDDj. The subband cAj covers the smooth information of the image, and the subbands cDHj, cDVjand cDDj cover the detail information of the image. At that point, the cAj subband of the frequency domain is splitted into four subbands at the second level decomposition, and thus along.
By way of filtering the image with H2 (w), the highfrequency information has gotten (edges). After down_sampling by a factor of two, two subbands have found H1rI and H2rI (the subscript r proposes that the filters have been stratified to the rows of the image I). At that point the filters H1 (w) and H2 (w) have used to the columns of the subbands H1rI and H2rI, tracked by down_sampling by a factor of two, and the following four subbands have attained cAj, cDHj, cDVj, and cDDj. The subband cAj covers the smooth information of the image, and the subbands cDHj, cDVjand cDDj cover the detail information of the image. At that point, the cAj subband of the frequency domain is splitted into four subbands at the second level decomposition, and thus along.
Image normalization
Normalization involves a 2D matrix (output of Wavelet Analysis), and returns it as an image (uint8 and values from 0 to 255). This procedure has performed by:
-
1.
Find max value in the matrix.
-
2.
Find min value in the matrix.
-
3.
Subtract the min value from max value.
-
4.
Subtract the min value of a matrix, multiply the result by 255, and finally divided the result by the difference between max value and min value
Thresholding
The responses of the single wavelet identified filters required to be joint to make a detection choice. The easiest lest methodology is a threshold model, to find a binary image that demonstrates the detected microcalcifications the universal threshold technique is applied.
Result and evaluation
In this section, we have tried out the detection method and showed the outcomes of applying these methods to a set of mammogram images.
Detection method testing
We have run experiments using wavelet family Daubechies, Symlets, and Coiflet.
Experiment
In the experiment, we have tested our method on the mammographic image contains one location of microcalcifications and malignant.
-
Step 1: Read a mammogram image, Fig. 3 shows this step.
-
Step 2: preprocessing, Fig. 4 shows this step.
-
Step 3: ROI, Fig. 5 shows this step.
In this step, we observed that, not using the preprocessing step, made the edge of the breast not clear and jagged. Therefore, the preprocessing step is important and must perform before extracting the breast and the Fig. 6 explains that. Fig. 7 shows the result of ROI step.
-
Step 4: Enhancement
-
Step 5: Detection
Figures 10, 11, 12 show this step using db4, coif4, and sym4 respectively:
Performance methods
In clinical practice the problem is to determine the efficiency of a diagnostic system detecting the presence of pathology, therefore in the proposed system the efficiency can be classified in four perspectives [18]:
-
1.
True Positive (TP) (correct), when the suspected abnormality is in fact malignant;
-
2.
True negative (TN) (correct), when there is no detection of abnormality in a healthy person;
-
3.
False positive (FP) (incorrect), when occurs detection of abnormality in a healthy Person;
-
4.
False negative (FN) (incorrect), when there is no detection of a malignant lesion.
The last two classifications are critical situations. The false positive requires an invasive examination which implies patient anxiety, stress and unnecessary costs. The false negative is an even worse situation as it compromises the health of the patient and the disease treatment.
The evaluation of mammography images is performed by expert radiologists, by histological examination, in the pathological cases and by three-year follow-ups in the negative results.
The performance criterion of a radiologist or a diagnostic system is generally appraised by two indices: sensitivity and specificity. The sensitivity (TRUE POSITIVE )of a recognized test is the fraction of positively diagnosed cases over the total of afflicted cases, which can be expressed by:
A test with a high value of sensitivity must have a minimal number of false negatives and is therefore useful in order to characterize the disease.
The specificity (TRUE NEGATIVE) of a test is the fraction of healthy cases over the total of un-afflicted cases, which can be expressed by:
A test with a high value of specificity must have a minimal number of false positives and is therefore useful to exclude the disease [18]. There are other criteria that include those four perspectives, such as accuracy that is the measure of the global performance of the algorithm about the correct decisions and precision which corresponds to the fraction of relevant detections:
Results
The detection method was proven with 65 images from the MIAS database (40 normal and 25 abnormal) and the number of microcalcifications locations in all abnormal images was (29) agreeing to the information offered about the database. The results from this method were as follows:
-
True Positive Number (TP) =27;
-
True Negative Number (TN) =36;
-
False Positive Number (FP) =4;
-
False Negative Number (FN) = 2.
The evaluation of our method was 93.1% of true positives, this result is computed by ((27/29) *100) and 10% of false positives ((4/40) *100) of the sum of detected objects on the image managed. In unsharp masking stage, we have tested the method using every one of three expressions for the Laplacian and obtained the best enhancement with the type two, and α equal (0.5) value of contrast, whereas the histogram modification was best with exponential modification approach, c equal 3, and 210 threshold value. Finally the best performance for the method was found with the family wavelet Daubechies order 4 (db4) with level one of decomposition.
Conclusions
In this article, a method for microcalcifications detection in mammograms of the breast has planned. After applying this method, we concluded the following:
-
1.
In spite of the great quantity of theoretical works in this major, computerized microcalcifications detection and diagnosis is extremely important things that need a good deal of effort and practice. This is to be appropriated to many reasons. Those arise from the great unevenness in the database mammograms, the profit of low resolution microcalcifications mammograms, small number of the existing database, some mammograms are still film-based and are read by way of a light box thus commercial (CADx) systems digitize the film and put markers on a small display or on a separate sheet, for the target of detection and classification the image is, in simple way, partitioned to produce features for a classifier and the functionality of enhancement is complicated as it also requires an image reconstruction.
-
2.
Microcalcifications are skilled marks of breast cancer and are very problematic to detect and diagnose in the mammography images due to their small size, low contrast with respect to the regular breast tissue and closeness to the surrounding tissues.
-
3.
For the reason of the importance of the information in medical images, the objective is to hold onto this information. Possibly the uses of wavelet transform appearances have had a significant impact in achieving this goal.
Future works
We would like to recommend the following points for further research:
-
1.
Apply these methods on local mammographic images.
-
2.
Add the removal process step in the preprocessing to pectoral muscle region in the Medio-Lateral Oblique (MLO) for reducing false positives. The pectoral muscle appears as a bright triangular patch in the mammographic image.
-
3.
Use of hybrid methods for process of classification such as fuzzy logic with Nearest Neighbor classifier.
References
American Cancer Society, Breast cancer. American Cancer Society, Atlanta, Ga, 2011.
Zimmerman, B.T., Understanding breast cancer genetics. University Press of Mississippi, United States of America, 2004.
B. E. Denarie, Using SURF imaging for efficient detection of micro-calcifications. M.Sc. Thesis, Department of Engineering Cybernetics, Mathematics and Electrical Engineering, Faculty of Information Technology, Norwegian University of Science and Technology, Norway, 2010.
Oliver, A., Torrent, X., Lladó, M., and Tortajada, L., Tortajada. Automatic microcalcifications and cluster detection for digital and digitised mammograms. Knowledge-Based Systems. 28:68–75, 2012.
Sankar, D., and Thomas, T., A new fast fractal modeling approach for the detection of microcalcifications in mammograms. J Digit Imaging. 23(5):538–546, 2010.
N. Uchiyama, and M. Nascimento, Mammography-recent advances. InTech, 2012.
Li, H., Liu, R., and Lo, S., Fractal modeling and segmentation for the enhancement of microcalcifications in digital mammograms. IEEE Trans on Medical Imaging. 16(6):785–798, 1997.
Kalra, P.K., and Kumar, N., A novel automatic microcalcifications detection technique using Tsallis entropy & a type II fuzzy index. Computers & Mathematics with Applications. 60(8):2426–2432, 2010.
Jiang, J., Yao, B., and Wason, A.M., A genetic algorithm design for microcalcifications detection and classification in digital mammograms. Computerized Medical Imaging and Graphics. 31(1):49–61, 2007a.
Cheng, H.D., Cai, X., Chen, X., Hu, L., and Lou, X., Computer-aided detection and classification of microcalcifications in mammograms: a survey. Pattern recognition. 36(12):2967–2991, 2003.
Yu, S., and Guan, L., A CAD system for the automatic detection of clustered microcalcifications in digitized mammogram films. IEEE transactions on medical imaging. 19(2):115–126, 2000.
N. Karssemeijer, A stochastic model for automated detection of calcifications in digital mammograms. in Proc. 12th Int. Conf. Information Processing Medical Imaging, Wye, U.K., 1991, 227–238.
N. Karssemeijer, Recognition of clustered microcalcifications using a random field model, biomedical image processing and biomedical visualization. In SPIE Proc., vol. 1905, San Jose, CA, 1993, 776–786.
Rizzi, M., D'Aloia, M., and Castagnolo, B., Computer aided detection of microcalcifications in digital mammograms adopting a wavelet decomposition. Integrated Computer-Aided Engineering. 16(2):91–103, 2009.
Yu, S.-N., Li, K.-Y., and Huang, Y.-K., Detection of microcalcifications in digital mammograms using wavelet filter and Markov random field model. Computerized Medical Imaging and Graphics. 30(3):163–173, 2006a.
Yu, S.N., Li, K.Y., and Huang, Y.K., Detection of microcalcifications in digital mammograms using wavelet filter and Markov random field model. Computerized Medical Imaging and Graphics. 30(3):163–173, 2006b.
Jiang, J., Yao, B., and Wason, A.M., A genetic algorithm design for microcalcifications detection and classification in digital mammograms. Computerized medical imaging and graphics. 31(1):49–61, 2007b.
Thangavel, K., Karnan, M., Sivakumar, R., and Mohideen, A., Automatic detection of Microcalcification in mammograms– a review. ICGST International Journal on Graphics, Vision and Image Processing, pp. 31–61, 2005.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Image & Signal Processing
Rights and permissions
About this article
Cite this article
Alasadi, A.H.H., Al-Saedi, A.K.H. A Method for Microcalcifications Detection in Breast Mammograms. J Med Syst 41, 68 (2017). https://doi.org/10.1007/s10916-017-0714-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-017-0714-7