Abstract
A worldwide demographic shift is in progress and the aged population proportion is projected to more than double across the next four decades. Our current healthcare models may not be adequate to handle this shift in demography, which may have serious consequences for the ageing population who are more prone to chronic diseases. One proposed remediation is to provide in-home assisted healthcare with technology-intervened approaches. Telemedicine, telehealth, e-health are paradigms found in scientific literature that provide clinical treatment through a technology intervention. In evidence-based medical science, these technology interventions are evaluated through clinical trials, which are targeted to measure improvements in medical conditions and the treatment’s cost effectiveness. However, effectiveness of a technology also depends on the interaction pattern between the technology and its’ users, especially the patients. This paper presents (1) a meta-synthesis of clinical trials for technology-intervened treatments of type 2 diabetes and (2) the Clinical User-Experience Evaluation (CUE). CUE is a recommendation for future telemedicine clinical trials that focuses on the patient as the user from Human-Computer Interaction (HCI) perspective and was developed as part of this research. The clinical trials reviewed were interpreted from a technology perspective and the non-medical or non-biological improvements of the users (patients) rather than the medical outcome. Results show that technology-intervened treatments provide positive behavior changes among patients and are potentially highly beneficial for chronic illness management such as type 2 diabetes. The results from the CUE method show how it complements clinical trials to capture patients’ interaction with a technology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The next four decades will see a demographic shift in the aged population where older generations retire while the proportion of working population comparatively decreases, sometimes termed a demographic time-bomb. Chronic illnesses such as diabetes, heart disease, Chronic Obtrusive Pulmonary Disease (COPD), obesity, etc. are more common in the ageing so hospital visits will increase accordingly [1]. This change in demography will negatively impact the patient/doctor, patient/nurse and patient to hospital bed ratios, which will consequently increase the overall costs of healthcare for society, possibly to unsustainable levels [2].
Type 2 diabetes is a chronic disease that continues to grow worldwide, constantly increasing the demand on future healthcare systems. This disease needs close monitoring and long-term management to prevent complications and expensive medical interventions, or even fatality [3]. Intensive management of blood glucose levels has been proven to reduce complications in both type 1 and type 2 diabetes [4]. However, the demographic shift, rising healthcare costs, health complications associated with type 2 diabetes and the cost of treatments raise concern about effective ways to manage the illness.
Technology-intervened treatments present one possible way to provide care for type 2 diabetes patients. Technology-intervened treatments have been used mostly for chronic illnesses such as cardiopulmonary disease, asthma and heart failure and are now increasingly used for diabetes monitoring [5]. In the medical literature, the technology-intervened treatments are referred as telemedicine, telehealth, telemonitoring, telecare and e-health.
Currently, the benefits of technology-intervened treatments of diabetes, such as telemedicine, are investigated and presented based on the results obtained from clinical trials. The focus of these clinical trials is to compare blood glucose and other medical conditions at the beginning with the results. In the literature, the trials are concluded to be effective based on evidence of the improvement in the medical condition only and not the combination of technology applied in the treatment. Importantly, patients must interact with the technology, which strongly determines the effectiveness of the treatment. However, if there are interaction barriers patients may have with a technology they are not reported, which indicates the results on the degree of effectiveness are incomplete. This information is important for future clinical trials in technology-intervened treatments that should also investigate the Human-Computer Interaction (HCI) between the patient and the technology.
This paper is a meta-synthesis that systematically reviews the use of technology from the patient’s perspective with a focus on Human Computer Interaction (HCI) and not the medical outcomes. Meta-synthesis generally refers to examination and synthesis of findings, across multiple reports to explore new interpretations [6]. Information was collected from a comprehensive list of clinical trials conducted on type 2 diabetes that applied technology-intervened treatments for comparison and analysis. Notably, the focus is on the patient as the user in a HCI environment, where information is gathered about the non-medical conditions of improvement and influence of telemedicine on patient’s behavior, rather than medical results. This study examines the results of clinical trials, which are interpreted from a technology perspective and the non-medical or non-biological improvements of the users (NB. the terms “user”, “patient” and “participant” are used interchangeably in the context of this paper). The results imply technology-intervened treatments would highly benefit chronic disease management as every trial reviewed recorded significant behavior changes among patients linking persuasive technology and current telemedicine. A Clinical User-Experience Evaluation (CUE) was developed based on the results of the meta-synthesis that proposes a recommendation for future investigations and/or clinical trials of technology-intervened treatments.
This paper is organized as follows: section 2 provides background information on the management of type 2 diabetes and the technologies involved in technology-intervened treatments; section 3 provides the methodology applied in the meta-synthesis of literature; section 4 presents the outcome of the meta-synthesis; section 5 describes the CUE and its use in a clinical trial as a recommendation for future trials; section 6 provides a discussion of findings and section 7 concludes the paper.
Background
The demographic shift
Four challenges may arise from the increase in the ageing population: the demand for healthcare; the retired population versus working population ratio; the patient versus available healthcare ratio; and healthcare costs. The current ageing population in the United States is approximately 8 %, which is expected to rise to 17 % by the year 2050 [7]. In contrast, Australia’s aged population will rise from 13 to 25 % by 2056 [8]. The first challenge, the demand on healthcare, will occur because the ageing population is more prone to chronic diseases, which require higher levels of medical care. The second challenge, the retired population/working population ratio, will adversely influence the government’s economic and financial plans. The third challenge, the patient/healthcare ratio, is the demographic shift toward an aged population that will negatively influence the patient/doctor, patient/nurse and patient/hospital bed ratios, which will decrease available healthcare. Finally, as the demand increases, healthcare costs will continue to rise and eventually become unfeasible.
Diabetes types and economic cost
Type 2 diabetes is one of the most dangerous chronic diseases that cause serious complications in elderly patients. Although younger populations of first world countries are at risk, the prevalence of type 2 diabetes is now increasing in older populations at alarming rates, which poses a growing threat for the future well-being of the projected aged population.
Healthcare systems have struggled with the overwhelming number of patients suffering from diabetes [9]. Diabetes is one of the most dangerous widespread chronic diseases that create serious complications that can lead to additional disease states. In 2000, medical studies projected the total number of people to suffer from diabetes would rise from 171 million in 2000 to 366 million in 2030 worldwide [10]. However, current figures show this increase reached the earlier predicted figures in only 10 years. In fact, as at 2012, approximately 371 million people worldwide already have diabetes, a total of 4.8 million deaths were due to diabetes and treatment costs were approximately 471 billion dollars [9]. This significant increase is attributed to the demographic shift in the proportion of people over 64 years of age [11] where 2.5 million of the diabetes related deaths were from the 60 to 79 age group [9].
There are two forms of diabetes: type 1 and type 2. Type 1 diabetes causes the pancreas to cease producing insulin. Without insulin, the body’s cells cannot regulate glucose (sugar) uptake into cells and the body burns its own fats as a substitute, which is potentially life threatening if not treated [12]. Patients with type 1 diabetes accumulate dangerous chemical substances in their blood from the burning of fat if not treated with daily injections of insulin. Type 2 diabetes is more common than type 1 and is the most common chronic illness that threatens the well-being of the ageing population. Type 2 diabetes affects 85–90 % of all people with diabetes [12]. While it usually affects older adults, younger people, even children, are now developing type 2 diabetes. The pancreas makes some insulin in type 2 diabetes patients but the body essentially develops immunity to insulin and the amounts produced are not enough to regulate blood glucose. This affliction can initially be managed with healthy eating and regular physical activity but over time, many patients also need medication or insulin injection.
There is currently no cure for type 2 diabetes so the recommended treatment is day to day management [12]. Type 2 diabetes treatments involve diet control, exercise, home blood glucose testing, and in some cases, oral medication with or without insulin. Effective individualized treatments may also incorporate psychosocial, lifestyle and other medical interventions [13]. Diabetes needs strict control of the blood glucose level by balancing within a triangle known as the diabetes triangle (Fig. 1), which consists of food, exercise and insulin (or medication) as the three corners [15]. Patients’ decisions sway in this triangle during their daily activities and if there is an imbalance, fluctuations in glucose level occur [14]. These fluctuations in the blood can cause hypoglycemia, a lack of blood sugar, or hyperglycemia, which is an excessive blood sugar ratio. Both hypoglycemia and hyperglycemia are acute conditions because they can cause physical and psychological effects that could range from mild to life threatening. Education, awareness and involvement of patients can help to prevent potential effects [16].
The diabetes triangle: clinical model of diabetes management. In real this model behaves more plastic and dynamic than the triangle shape envisages [15]
According to Zhang et al. [17], the total annual global health expenditure for diabetes in 2010 was estimated to fall between $376.0 billion USD and $672.2 billion USD. This accounted for 12 % of the world’s total health expenditure. In 2010, the global average expenditure related to diabetes per capita was $1330.00 USD [17]. Significantly, the economic cost of diabetes varies in different parts of the world. For example, in Bangladesh, the cost of one diabetic patient for one year is $28 USD, in China $193 USD compared to the high costs of $8,478 USD cost in the United States and Norway $9,208 USD [9]. Notably, the treatment quality differs vastly depending on the country’s healthcare system.
Technology-intervened treatments: Telemedicine, telehealth and e-health
Technologies that are applied in health services and medicine go through a process known as Health Technology Assessment (HTA), which consists of:
-
The product life cycle;
-
The quality standards and regulations;
-
Evidence Based Practice (EBP);
-
Reimbursement processes; and
-
Other HTA processes that are regulated by national HTA bodies such as the Food and Drug Administration (FDA), USA, the National Health Service (NHS), UK, etc.
To provide evidence for EBP, the technologies need to go through rigorous testing methods to prove their efficacy, which is done through clinical trials. Clinical trials are formal procedures that are followed during drug development to check safety and efficacy, which refers to the “capacity of a beneficial effect”, and data for health intervention (drugs, devices etc.). Medical practitioners follow EBPs that aim to find best available evidence from medical science literature before a treatment decision is made by a clinician [18]. EBP supports the clinician in their decision on the risk and beneficial factors of a treatment for a particular patient [19, 20].
“Telemedicine” was introduced in the 1920s [21] but not initially used until the 1970s [22]. Telemedicine is the use of Information and Communications Technology (ICT) to provide clinical treatments over distances [23]. Rapid development in ICT has contributed to the growth in telemedicine initiatives, which continues to evolve. There is now a wide range of communication technologies available for telemedicine [24–26]. For example, after [23] collecting 104 peer reviewed definitions of telemedicine, Sood et al. [23] determined:
“Telemedicine being a subset of telehealth, uses communications networks for delivery of healthcare services and medical education from one geographical location to another, primarily to address challenges like uneven distribution and shortage of infrastructural and human resources.”
“Telehealth” is defined by the American Telemedicine Association (ATA) as closely associated with telemedicine but also encompasses a broader range of remote healthcare methods not always involved in clinical services. These technological methods include videoconferencing, still image transmission of, e-health including patient portals, remote monitoring of vital signs, continuing medical education and nursing call centers [27].
The term “e-health” emerged with the growth of the Web and can be viewed as a type of e-commerce [28]. According to Eysenbach [28], e-health was used more by industry and commerce people than academics and was created to be aligned with other “e” words such as e-commerce, e-business, e-solutions etc. His definition is:
“e-health is an emerging field in the intersection of medical informatics, public health and business, referring to health services and information delivered or enhanced through the Internet and related technologies. In a broader sense, the term characterizes not only a technical development, but also a state-of-mind, a way of thinking, an attitude, and a commitment for networked, global thinking, to improve health care locally, regionally, and worldwide by using information and communication technology” [28].
Human computer interaction (HCI)
Computer systems are developed through a User-Centered Design (UCD) in HCI as opposed to the traditional software engineering and computer science approach where the technologies or functionality are the initial concentration. UCD keeps the human users and their goals central to design and evaluation [29].
Qualitative research methods, which are common practice in HCI, aim to generate richer knowledge about users. According to Boulding (1956), “knowledge does not grow in abstract and knowledge does not exist by itself, it is a property of interaction between agents and the environment and is tied to perspectives, intentions and perceptions”. A message may have a meaning but the meaning depends on the code or set of alternatives from which the message has originated [30]. Qualitative research has been used by Dalcher [31] to understand major ICT and Information System (IS) failures in the United States. Dalcher [31] practices qualitative research in software engineering processes and argues that “knowledge is deeply bound to its original context and thus enables for a contextually correct understanding”. Effective capturing of a precise context is the only way to discover information about the informer’s position, perspective and relationship with the environment. To understand IS failures, Dalcher urges that any useful information must therefore be accompanied by additional contextual information that will shed light on its utility, validity and relevance and any methods adopted need to identify such contextual knowledge [31, 32].
HCI techniques have many methods of evaluation, some are analytical and focus on the system with a set criteria while others are empirical and involve people using the system. Contextual design, interviews, observations, participatory design, ethnography are effective techniques in performing empirical evaluations. HCI mandates anyone who uses a system be classed as a user, so transcending the HCI empirical evaluation methods to technology-intervened treatments, the “user” classification includes doctors, nurses, care providers as well as the patients. This paper focuses predominantly on patients as the most important users because their well-being depends on the proper use of the technology. Patients’ feelings, comfort, partiality, ease of use are very important factors to gauge the success rate of a technology. This paper focuses on the patients’ perspective and the non-medical factors of improvement through telemedicine, telehealth and e-health for the treatment of type 2 diabetes.
Comparison with related works
Ekeland et al. [33] established that besides the traditional questions of clinical benefits and the cost-efficiency of telemedicine, there are “new questions rising in telemedicine”. There are a resurgence of new questions arising in telemedicine such as patients’ perspectives and ongoing collaborative achievements. Ekeland et al. [33] performed a systematic review of other reviews in telemedicine, which provided a strong direction to show the effectiveness of telemedicine for different illnesses in general. Methodologies of the clinical trials of telemedicine are heterogeneous, which makes comparisons of different systematic reviews difficult. However, evidence of an aspect of telemedicine (e.g., effectiveness on patients or cost efficiency) is built through systematic reviews of clinical trials. These reviews support the EBP for medical science.
Verhoeven et al. [34] and Verhoeven et al. [35] presents a diabetes-specific systematic review of telemedicine from technology perspective. Both of Verhoeven et al’s reviews thoroughly explored the technologies for diabetes care in general and concluded that telemedicine is practical, cost-effective and reliable. The authors found that clinical, behavioral and care coordinator outcomes provided a strong basis of data on technology intervened treatments of telemedicine and diabetes.
This paper extends and expands the above works and the approach differs in three ways:
-
1)
This paper separates type 2 diabetes technologies from other types of diabetes. Verhoeven et al. [34] and Verhoeven et al. [35] included diabetes types (i.e., type 1, type 2 and gestational diabetes). However, the daily management and effects on the patient differ depending on which type. Gestational diabetes occurs among women during pregnancy and if untreated may cause serious health problems and future diabetes risks to both the mother and child. Type 1 diabetes is fatal; the patient needs to take an insulin dosage to stay alive. Type 1 diabetes is prevalent in the population younger than 40 and often known as “juvenile diabetes”. In contrast, type 2 diabetes is not fatal during the initial stages and with proper management the patient can enjoy a normal and healthy life. Due to the differences in types of diabetes, the technology interventions differ in the urgency and interaction patterns for the varied types of diabetes.
-
2)
This paper proposes a method, Clinical User-Experience Evaluation (CUE) to capture individual patient perspectives. The CUE aims to expand and explore the findings of Verhoeven et al. [34] and Verhoeven et al. [35] who stated some patients benefited more than others. This paper proposes the method CUE, which will help to further understand these reasons in detail to better inform research in persuasive technology that finds one design does not fit all [36, 37];
-
3)
Verhoeven et al. [34] and Verhoeven et al. [35] noted that patients found the technology too complex, costly and time consuming with some patients needed greater assistance with self-care than they received in the intervention settings. In these ICT-based care cases, online training and personal assistance might be necessary and this paper extends from that to provide analysis in two criteria:
-
a.
The degree of setup, maintenance and training; and
-
b.
Patient withdrawals.
-
a.
The CUE methodology is aimed to unpack the variations in outcome of individual patients using the technology.
Persuasive technologies and the diabetes triangle
Persuasive technology is a type of technology that is intentionally designed in a way to change a person’s attitude or behavior [38]. Alternately, these technologies are also referred to as Behavior Change Support Systems (BCSS) due to the support provided to an individual to make behavioral changes [39]. The use of force (coercion) or misinformation (deception) is outside of the scope of persuasive technology because persuasion is a voluntary change of behavior or attitude or both. Just-in-time persuasive interfaces can be created to motivate behavior change [40]. Several frameworks exist for designing [41] and evaluating [37, 42] persuasive technology interventions. For example, Intille [43] reviewed that there are four components to effective just-in-time information that include:
-
1)
A simple, tailored message that is easy to understand;
-
2)
The message occurs at an appropriate time;
-
3)
The message is given at an appropriate place; and
-
4)
The message uses a non-irritating strategy [44].
Evidence of effectiveness of persuasive technology to control behavior about food and exercise started approximately two decades ago. An example of persuasive technologies for better eating habits is the USA’s Food and Drug Administration (FDA) successful recommendation for eating fruits and vegetables. They promoted better habits via the “5-A-Day Adventures” multimedia application produced on CD-ROM by Dole Food Corp [45]. This “edutainment” application uses animated characters, music, and games to encourage children to eat the number of daily servings of fruits and vegetables. Examples of persuasive technologies for better exercise habits include
-
Nintendo’s Pocket Pikachu with pedometer is designed to persuade children to do more physical activities consistently [46]. The pet that lives inside the device requires the owner to walk, run, or jump each day to keep the pet alive. This persuasion was very effective due to the popularity the Pokémon animation series and children’s affinity with the characters; and
-
Nike’s “Fuelband” is an all-day activity monitor/pedometer bracelet that tracks total daily steps and reward a person for being active based on a goal known as “NikeFuel” goal.
Research objectives and rationale
Medical science practitioners and healthcare professionals conduct the clinical trials that gather evidence on efficacy and cost-effectiveness of telemedicine interventions. The evidence that is gathered from clinical trials in medical science is through a systematic review for EBP. These systematic reviews aim to ask one (and sometimes more) specific question(s) to gather all supporting evidence from the answer(s).
This paper adopts an approach similar to a systematic review that uses a keyword search to choose papers to review the effectiveness of clinical trials for type 2 diabetes. Evidence in diabetes research shows that intensive treatment with frequent monitoring of the blood glucose helps to reduce further complications. There are many cases in the literature of clinical trials that examined the use of telemedicine for diabetes treatments to determine the efficacy of such treatments. However, new technologies emerge so rapidly there are many that have not yet been evaluated in clinical trials and without these formal evaluations will never be used in common practice. Because this paper reviews past clinical trials of telemedicine treatments for type 2 diabetes patients, the focus is on the technologies that have been assessed in a clinical trial and not new technologies.
This study is carried out from the perspective HCI because there are significant differences between a drug treatment and a technology treatment, such as telemedicine. The scope of telemedicine technologies is non-pharmacological, non-immunological and non-biological. Instead, the capability of usage is important because results may vary depending on the technological skills of the patients. In many cases, some training is required with technology-intervened treatments to ensure patient’s capability and engagement. Contrarily, there are no training required with a drug and their effects are at the pharmacological, immunological and metabolic levels. Because the user has frequent or regular interaction with the technologies, especially in the case of type 2 diabetes interventions, the feelings of these users towards the technologies are almost as important to successful outcomes as the drug treatments.
Research questions
Technology-intervened treatments fall into two domains; the domain of medical science for their utilization in healthcare and the domain of IT for the technology design and user evaluation. The term “user” in telemedicine would refer to doctors, nurses, patients, caregivers who all use the technology and make up the user group. However, only the patients use telemedicine methods as a form of treatment for life altering illnesses, all others use the technologies for the purpose of job requirements. Therefore, throughout the rest of this paper the term “user(s)” are referring to patients. The following two questions were the focus of this review:
-
1.
How effective have telemedicine services been for the treatment of type 2 diabetes?; and
-
2.
What improvements did telemedicine provide for type 2 diabetes patients from technology use perspective?
Methodology of the meta-synthesis
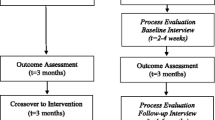
The methodology of the meta-synthesis involved a systematic review that comprised of four iterative steps (Fig. 2):
-
Step 1
Literature search - Pubmed, Science Direct and Google scholar were the databases used to search for literature on clinical trials of type 2 diabetes telemedicine. No limits were posed on sample population size, intervention type and clinical trial design. The search keywords used were - “type 2 diabetes”, “clinical trial”, “telemedicine”, “ehealth”, “telehealth”, “telecare”, “telemonitoring”, “technology”.
-
Step 2
Intervention types - All variations of technology intervention for diabetes type 2 treatments were included with no limits on the type of technology.
-
Step 3
Content Extraction - Each paper was analyzed systematically in the following order:
-
1.
Methodology;
-
2.
Conclusion;
-
3.
Discussion; and
-
4.
Results.
The contents extracted from the literature (Table 3) included:
-
The type of diabetes (type1 and/or 2);
-
The behavioral outcomes;
-
The patient dropouts;
-
The type of technology used;
-
The contents about patients’ non-medical conditions;
-
The patients’ feelings comments about the technology; and
-
The patients’ difficulty or ease with the technology.
Notably, not all papers contained contents of the above bullet list.
-
-
Step 4
Exclusion criteria – Because search results most often yielded type 1 diabetes, clinical trial design and clinical trial planning for telemedicine, the following exclusion criteria were used to filter the results (Fig. 2):
-
Criteria 1)
Papers that were about ICT and diabetes-care but were not clinical trials were excluded since this is not a review of the available technology;
-
Criteria 2)
Only papers on type 2 diabetes were included. Papers on telemedicine clinical trials on type 1 diabetes were excluded. However, papers that considered both types 1 and 2 diabetes patients were included but only information on type 2 diabetes were analyzed;
-
Criteria 3)
Papers that only published the plan, proposal or study design of a clinical trial that has not yet commenced were excluded; and
-
Criteria 4)
Papers that were published in languages other language than English were also excluded from this review.
-
Criteria 1)
-
1.
A number of prominent diabetes clinical trials were excluded from this meta-synthesis because they did not align with one or more of the criteria (Fig. 2). For example, the vast French IDEATEL diabetes project [47–49] and the telemedicine clinical trial of diabetes conducted by Leichter et al. [50], [51] and Shultz et al. [52] were excluded because they all incorporated both type 1 and type 2 diabetes. Studies by McFarland et al. [53], Stone et al. [54], Estrada et al. [55] and Rodriguez-Idigoras et al. [56] did not report anything about dropout numbers, reasons for dropout and behavioral changes but only presented data of medical conditions improvements. Other exclusions included, for example, Watson et al. [57] who presents a pilot study, Eakin et al. [58] who presents a preliminary trial plan and Davis et al. [59] who presents the technology used at a remote clinic for low-income community. Figure 2 presents the workflow used in the paper selection process and the number of actual papers excluded and included.
The meta-synthesis findings and discussion
Nineteen clinical trials of technology intervened treatments of type 2 diabetes were selected to be included in the meta-synthesis based on the methodology described in section 3.3. Five criteria were used to review the selected trials shown in Table 3, which include:
-
Criteria 1)
The technology type;
-
Criteria 2)
The degree of setup, maintenance and training;
-
Criteria 3)
Patient withdrawals;
-
Criteria 4)
The effectiveness of the telemedicine; and
-
Criteria 5)
The behavioral improvements.
Technology type
Figure 3 presents a classification diagram of telemedicine technology that has been used in a clinical trial for type 2 diabetes. The technologies range from uncomplicated, where patients and clinicians communicate through phone, email or SMS (short message service), to complex web based frameworks that require connection to the Internet. The different technology categories include:
-
Handheld portable devices - devices that are easy for the patient to carry and automatically record time, date and blood glucose levels [60, 61]. For example, sample recommendations such as “Please, decrease the long acting insulin by two units”, “Please add one tablet of sulfonylurea in the evening”, “Lack of exercise may be the cause of the aggravated glucose level” and “Your glucose control seems to be good” etc., can be sent using the mobile phone SMS service [62];
-
Transfer of data via modem followed by telephone counseling - methods used in earlier periods before the Internet was widely available [63];
-
Automated Telephone Disease Management (ATDM) – a telephone-based system where patients receive calls at predetermined times and listen to self-management tips navigated via the telephone keypad [64] and the modern version where phone calls are automated to emulate the conversation with a physician [65];
-
Glucometer modem transfer followed by graphical report generation [52];
-
Data entry of touch tone telephone followed by voice message from clinicians [66];
-
Interactive programs on CD Rom to educate on self-management [67];
-
Web-based programs on self-management including chat room forums to enlist strangers as supporters [68] the iCare Desktop, the Health Buddy appliance web interfaces [69], web-based diabetes management systems [70] and the Internet Based Glucose Monitoring System (IBGMS) [71],;
-
Teleconferencing - a person to person connection via telephone [72]; and
-
Pro-active call center treatment support - a telephone-based system where conversation is not automatic like the ATDM. The conversation takes place with trained non-medical operators [73]
Training, setup and maintenance of the clinical trial technologies
To determine the success or failure of technology development, understanding users’ needs is important [74]. Bardram [75] stated that “the clinical benefit of a healthcare technology might be diluted significantly if the patients find the technology hard to use”. System complexity and poorly crafted interfaces can cause negative emotional responses in the user, which lead to experiences of confusion, frustration, and failure [76]. Further, errors can be frustrating experiences for novice users who are unable to fully understand its cause. In fact, if a user is unable to understand how to appropriately respond to an error, they may perform actions that compound its severity, which invariably compounds feelings of frustration [77, 78].
User training can help to alleviate errors made by users and to help them to understand the system. Ideally, patients should have the knowledge to operate the technology in the appropriate way. However, technology skills vary and patients that fail to use the technology efficiently often experience dissatisfaction, which can ultimately cause the patients to not engage in the treatment and indirectly hamper medical improvements. For this reason, most clinical trials provide a training and instruction manual on how to use the technology. Notably, the trials reviewed in this paper did not all report the specifics of the technology training applied for the study. Tsang et al. [61] investigated technical issues of patients in their trial. Bujnowska-Fedak et al. [79] found that patients did not find the technology in their trial to be intuitive enough; only 35 % of patients could use the technology alone, 24 % required family support and 41 % were unable to use the system and required constant family assistance. The results found that patients who operated the equipment by themselves benefited more than those that could not or those that required assistance, which shows the importance of investigations of the technology from the HCI (albeit the patients’) perspective. Table 3 presents a summary about technology training, setup, maintenance issues of the reviewed trials.
Users often respond to technology as if the device were another person in a social context [80]. An experiment on the “rule of reciprocity” was demonstrated where users were happier to provide helping behavior to a computer that had assisted helped them previously than to a different computer [40]. Further laboratory experiments examined how users are susceptible to flattery from computers and this flattery has the same effects as if given by a human [44].
Important functions in telemedicine are the setup and maintenance of the devices in the users’ home because patients should not be expected to have this knowledge. Generally, technical support is usually provided to assist with these functions as well as troubleshooting any technological problems that arise. Problems and negative experiences can alter a user’s trust in a technology. These results show that if patients have to troubleshoot the telemedicine technology, the effectiveness of the treatment can decrease indirectly as users (patients) stop using the technology due to frustration. Because the focus was predominantly on the medical data and not the technology used, the majority of clinical trials reviewed, did not report any technical problems or maintenance information. Yet one study by Faridi et al. [81] reported that the technology barrier, which was the difficulty of using a mobile phone, had caused lack of adherence to a mobile phone based system.
Participant withdrawal and/or dropouts
The reasons for participant withdrawal, shown in Table 3, were not reported in the majority of the nineteen reviewed trials reviewed. There were two withdrawals reported by Rutten et al. [60] due to lack of motivation to adhere to the self-monitoring. The studies by Lavery et al.[82], Cherry et al. [69] and Biermann et al. [63] did not report any dropouts. Izquierdo et al.[72] reported several patients who did not send the data in time so were withdrawn by default. There were a large number of dropouts in the following studies: 10 by Shultz et al. [52], 43 by Glasgow and Toobert [67] and 37 by McKay et al. [68], but the reasons were not reported. Williams et al. [65] found four dropouts from 60 patients, due to patients’ inability to use the blood glucose meter and disappointment with the intervention. The study by Meneghini et al. [66], which had 77 withdrawals, was the only one that posed the question for future research to investigate reasons for not using the system in the trial.
The lack of data about withdrawal and/or dropouts led to three assumptions:
-
1)
The reasons were not investigated;
-
2)
The reasons were investigated but not published; or
-
3)
The reasons were out of the scope of the clinical trials.
Based on these assumptions, the authors of the reviewed clinical trials were emailed and responses were received from three. Two authors stated that withdrawal reasons were not recorded. However, one stated although the reasons for withdrawals were not in the research scope, they were discussed and provided information about patient behavior for this analysis.
The study by Young et al. [73] recorded and published the reasons for dropout and withdrawal. There were 83 dropouts in the intervention group with an additional 22 for call center–related reasons. The reasons reported included: eight participants were not able to cope with the calls; four participants were unhappy with the advice given; three due to the travel required; three changed their minds; and two were too busy to use the intervention.
The tendency for participants to withdraw from a trial would be of great interest from the ICT and HCI perspective. Some patients possibly dropout or withdraw (unless for medical reasons) due to the technology involved. The reasons could be found to relate to usage and interaction issues such as difficulty of use, technical problems, the complexity higher than the patients’ skill level and/or the patients’ confidence level in, and willingness to adopt, a technology. For example, a publication by Steele et al. [83], proposed that patients’ willingness to adopt a technology-intervened treatment could be influenced by independence, perceived improvement in life and ease of use. All participants believed that independence is of paramount importance to them and they would prefer to remain home and use technology rather than being in a nursing home. If benefits of the technology were explained to the participants most of them had shown willingness to adopt the technology even though they had concerns about change of lifestyle due to its use. Participants commented that they would consider using the system if it is deemed useful, reliable and provides benefits to their current lifestyle. Each participant had different levels of skills to use the technology but they stated that the ease of use was one factor of choosing the technology. Participants mentioned that availability of training, the available quality of support for training would let them use the technology if it was not easy to use.
Patients’ withdrawal from clinical trials is common in most clinical trials [84]. Jadad [84] presented a scale that independently assesses the quality of methodology of a clinical trial. The Jadad Scale, also known as the Oxford Quality Scoring System, shows the importance of quantifying the number of withdrawals and dropouts in a clinical trial to assess the effectiveness of the employed methodology [85]. Notably, the reasons for patient withdrawals are often not collected or published even though the number of withdrawals affects the outputs and statistics of the clinical trial. This practice is common because the objective of the clinical trials is to find out improvements in particular medical conditions and cost effectiveness of a telemedicine. However, to create sustainable telemedicine practice, data on withdrawals are significantly important in understanding the reasons why patients dropout and especially if caused by the technology.
Effectiveness of telemedicine for type 2 diabetes patients
The clinical trial results were used to assess the effectiveness of telemedicine for type 2 diabetes patients. Most of the reviewed papers are randomized clinical trials where the blood glucose is measured initially as a baseline and then measured after a certain period after the intervention. The baseline and post-intervention results are then compared between control groups.
This review relied solely on the publications about the clinical trials to extract information, regardless of the specific applied design method so only available results and conclusions were assessed about the effectiveness of telemedicine treatment. Surprisingly, the results were mixed where not all trials agreed that telemedicine for type 2 diabetes treatment was effective. Our results are consistent with the results from [33] who conducted a systematic review of reviews on the impacts and costs of telemedicine service. They found that out of eighty heterogeneous reviewed studies only twenty-one stated telemedicine was effective, eighteen stated it was promising and others raised questions for further analysis.
Behavioral improvements
Significantly, our results found that every clinical trial showed noteworthy positive behavioral outcomes of telemedicine. The trials conclude that even though telemedicine does not improve medical conditions for certain, it does invoke positive behavioral change. However, the literature urges for further investigations due to limited evidence. In addition, when authors found behavioral improvements, which were not the main scope of clinical trial, they mentioned those worth investigating in future to determine conclusive results. Some authors also mentioned the study design was limited. Table 1 summarizes the effectiveness in terms of physical and behavioral improvements.
The three specific behavioral outcomes to show improvement (Fig. 4) are classified as actions, changes in awareness about managing type 2 diabetes and satisfaction with the telemedicine healthcare. Actions entail activities that the participant adopts due to the technology intervention. Awareness is the informed state of mind the participant achieves after using the telemedicine intervention. Satisfaction involves the participants’ satisfaction from using the technology intervention. The nineteen studies revealed the following findings of behavioral improvements:
-
Rutten et al. [60] reported overall improvement in personal health care and quality of life for all patients. The participation stimulated the patients to keep closer control of blood glucose levels and increased their motivation of maintaining good levels;
-
Shultz et al. [52] showed that using telemedicine helped patients adhere to a dietary plan and other healthy habits;
-
Meneghini et al. [66] found patients became an active participant and got involved in metabolic control. Technology-intervened systems empowered case managers to increase intervention and improve metabolic control. In addition, Meneghini et al. [66] have urged the importance of the psychological foundation, possible system dependencies, and personality traits are contributing factors in the various behaviors that require further study;
-
Piette et al. [64] stated the automated telephone assessment resulted in improved self-care, weight monitoring for patients even though the interaction with the nurse was less than six minutes per month. It also allowed patients with behavior reinforcement;
-
Glasgow and Toobert [67] found improvements in dietary behavior of the patients. This clinical trial is first of its kind to consider social cognitive-environmental model in an intervention;
-
Biermann et al. [63] observed that patients were enthusiastic about sending data and preferred telemanagement rather than daily logging with pen and book;
-
Montori et al. [70] work also showed similarly a better way of self-reporting and documenting to improve well-being;
-
Izquierdo et al. [72] measured stress levels of diabetes patients through teleconferencing. They found patients’ quality of life improved by reducing the diabetes related stress, which helped the patients better manage the illness;
-
Cherry et al. [69] showed that overall quality of life was improved, which is evidenced by the SF-12 survey, which indicated a change of self-management behavior;
-
McKay et al. [68] showed social support is also important for self-management and awareness, where improvements in patients’ perceived availability of social support was relative to participants who only had computer access to information about diabetes. Connecting with other type 2 diabetes patients helped patients to engage better in self-management;
-
Tsang et al. [61] reported that dietary awareness was generated after use of the technology;
-
Young et al. [73] published the behavioral outcomes in a companion article and reported participants receiving the intervention continued to report high levels of satisfaction with their treatment after a year and more than 90 % strongly agreed or agreed that the telecarer approach was acceptable. Qualitative comments pointed to the importance of a personalized service; increased feelings of well-being, including confidence and self-control; help with problem-solving; and patients developing rapport and a strong bond with the telecarers [86].
-
Cho et al. [71] expected a majority of patients’ questions to be about drug dosage during the 30 month trial. However, they concluded that the contrary was true because only 20 % times patients actually sought for glucose dose adjustment of the drug. Instead, the authors found 41 % of the recommendations made were for patients seeking encouragement and problem assessment and 30 % of patients asked for some sort of counseling.
-
Kim, Kim [62] attributed the significant physical improvement of patients was due to their behavioral changes. Patients were found to have more contact with caregivers through SMS and internet based messages, which improved their enthusiasm, motivation and engagement in blood glucose monitoring.
-
Bujnowska-Fedak et al. [79] found that patients who used the system alone benefited with an increased quality of life score shown in the surveys that indicates better mental health and higher prevention against depression.
-
Zolfaghari et al. [87] found that both SMS and telephone intervention found significant improvements in behavior.
-
Tang et al.[88] found physical improvements through behavior change and attributed it to the Hawthorne effect, where patients are influenced by awareness of being observed. The authors intended to understand factors that might predict patient engagement.
The findings on behavioral improvements in this meta-synthesis show positive results in type 2 diabetes treatments and comply with the diabetes treatment based on diabetes triangle in Fig. 1. The compliance is only towards two corners of food and insulin since the technology interventions did not have physical activity monitoring functions. Yet there were awareness of weight management. Improvements in dietary behavior and medicine are positive indicators that these telemedicine technologies are moving towards patient improvement. Furthermore, the satisfaction with the technology by patients in the trial shows promises for these kinds of interventions. The behavioral outcomes are positive although the medical outcomes in terms of blood glucose are not always positive.
Recommendation for future clinical trials
A lack of data exists on user (patient) experience with technology-intervened treatments in clinical trials of type 2 diabetes, as discussed in section 4. In-home telemedicine technologies will not serve their purpose if they are not adopted by the users. Information can be collected via the users’ experience and interaction to find out reasons that influence effectiveness of telemedicine technologies. Bardram [75] claimed the results of failure to use a technology can be diluted in the end results of a clinical trial. Early evaluations during clinical trials can help technology and medical researchers learn more about user experience to identify the positive and negative user interactions. To remediate this situation this paper proposes the Clinical User-Experience Evaluation (CUE) method to complement clinical trials in EBP. The name CUE was inspired by Bardram’s [75] Clinical Proof-of-Concept (CPOC), which is a prototype evaluation phase with a few patients prior to a full-scale clinical trial.
The clinical user-experience evaluation (CUE) project
The CUE was conducted in conjunction with a clinical trial of a telemedicine in-home monitoring device for type 2 diabetes administered by the Townsville-Mackay Medicare Locals (TMML) in North Queensland, Australia. The TMML trial used a randomised controlled method to explore whether remote access to clinical care, supported by telehealth technologies over high speed broadband, leads to improved diabetes control [89]. Patients were randomly selected to assign participants to an intervention group and to a control group. The intervention group received additional diabetes care from a care coordinator nurse via an in-home broadband communication device that comprises of a tablet computer, an automatic glucometer, which is a blood glucose measuring device, and an automatic sphygmomanometer, which is a blood pressure measuring device. The device captures clinical measures, provides regular health assessments and videoconference with other health professionals when required [89].
To distinguish the CUE from the TMML randomized clinical trial, the CUE methodology was developed as a three stage process:
-
1.
A contextual inquiry that is performed in-situ in a patient’s home. During this stage the patient uses the device while using the “think-aloud” method as the observer takes notes. Then, the observer interviews the patient regarding the process of using the device. The questions are based on the actions that were observed while the patient was using the device. This process is conducted during a patient’s regularly scheduled time for using the device.
-
2.
A semi-structured qualitative inquiry (interview) to understand patients’ experience and expectations. The questions are predominantly developed during stage one. The interview takes place directly after stage one, while perceptions are still fresh in the mind of the user. The questions are structured around the patient’s perceived benefits of the device, the patient’s choice of locations, their expectations of the device, their impressions about the design of the current device and the patients’ thoughts of how the device should be.
-
3.
An anonymous survey to encourage free expression without reservations. During the first two stages, the CUE allows for observation of certain behaviour of the participants in person. To verify these observations, an anonymous survey is conducted in the third stage to obtain patients’ feedback and opinions on the observations from the previous stages. This survey was administered 8 months after stage two to allow for reflection and was anonymous to uncover thoughts that may not have emerged in the in-person interviews.
Implementation of CUE
The CUE does not interfere nor impede in the traditional clinical trials but is an additional activity that is carried out concurrently by non-medical staff. Table 2 describes alignment of activities of the clinical user evaluation to the activities of the full medical clinical trial.
Participation in the CUE was voluntary and nine patients were selected based on a subset of intervention group within the TMML clinical trial. The CUE contextual inquiry (stage one) and the qualitative inquiry (stage two) were completed after a 3 months period from when the patient was given the initial training by the nurses on how to use the in-home monitoring device. This time period allowed the patients to become accustomed to the device to ensure the data from the CUE was not influenced by the initial novelty or unfamiliarity with the device [90, 91]. Two of the nurses who went to the patients’ homes during setup of the technology, training with the technology and provided support through telephone communication with these patients were also interviewed.
Data analysis of the CUE
All contextual inquiry and qualitative inquiry sessions were audio-recorded, then transcribed. Photographs and field notes were taken at the time of the sessions. The contextual inquiry was analyzed to recommend patient-centered system design by following steps from contextual design [92]. The qualitative inquiry transcripts were open-coded and themes were developed from patients’ answers. NVivo software was used to manage the codes and themes. During the contextual inquiry patients were observed while they uploaded their blood glucose and blood pressure. The patients led each session and talked about the device like an instructor while the researcher listened and took notes.
Preliminary results from the CUE
Results from CUE provided deep insights into how patients perceive the device and how to improve the device.
Types of users (patients)
All patients do not interact with the device the same way. Individual variations of their interaction were noted through CUE. The patients could be grouped as the following:
-
Proactive patients are very proactive and used the technology to upload their regular blood glucose and blood pressure regularly. In addition, the proactive patients also used diabetes awareness information that was available on the tablet PC.
-
Accepting patients welcome the use of the technology but did not spend extra time to explore the features for diabetes awareness.
-
Indifferent patients use the technology because they are told they have to. They do not resist and do not seem to care either way.
-
Resistant patients are opposed to using any technology. For example, one patient was resistant due to their lack of experience in technology use and lack of ownership of a computer or mobile-phone. This patient was in the clinical trial intervention group due to the random participation for recruitment (i.e., a lottery method). Notably, although resistant, the patient used the technology because they felt they had to commit to the clinical trial.
Ease of use
All patients were given training to use the technology by their nurse. A nurse went to a patient’s home during set up and trained the patients for approximately one hour. The training consisted of demonstration by the nurse followed by practice sessions in the presence of the nurse. Two nurses were also available during the rest of the clinical trial to answer questions about problems with the technology. In cases when the guidance through phone was unable to resolve the problems, the nurse would visit a patient’s home personally or send a technician.
Two patients were not as comfortable with the technology as the others despite having used the devices for more than 13 weeks before participation in the CUE. One was a patient from technology “resistant” group while the other was from the “indifferent” group. The user types of section 5.2.1 could be related to a patient’s ease of use with the technology. According to the nurses, “What patients describe as a problem with the technology is often not what the real problem is”. The nurses went on to state that “often it is a step that the patients forgot but they thought the technology had problems”.
Other significant results
The implementation of the CUE during this clinical trial revealed further rich information including:
-
Patients’ perceived benefits;
-
Patients’ future decision to use the technology;
-
Patients’ feedback about the technology [93]; and
-
Recommendations of the technology design
These results are very detailed and would be reported in future publications.
Discussion
Although numerous clinical trials have been conducted that examine the effectiveness of technology-intervened treatments, the results and conclusions are not absolute. The business and technology communities continue research and development of these treatments. TechCast [94] performed a study to determine the future of medicine to be telemedicine, telehealth and e-health services. This study found the global telemedicine market grew from $9.8 billion USD in 2010 to $11.6 billion USD in 2011 and was expected to reach $27.3 billion USD in 2016, which is an additional 15 % global rise in adoption. Conversely, technology-intervened treatments expect patients to have a more proactive role in comparison to the traditional healthcare methods [95]. Even if patients are provided with the latest state-of-the-art technology at home, the technology-interventions will not benefit the future healthcare systems if they do not use them. For this reason, research into the technology interventions through a HCI perspective is important.
Benefits of telemedicine could be lost due to the problems faced in the use of the technologies. A clinical trial study by Bujnowska-Fedak et al. [79] reported that patients who operated the device by themselves gained greater benefits of the medical treatments than those that could not or would not use the technology. The study reported only 35 % of patients could use the technology without assistance and they gained more benefits from the technology-intervened treatment.
The importance of user-experience of patients is valuable in a clinical trial. A study by Cho et al. [71] reported that during telecare support, the researchers expected a majority of patients’ questions to be about drug dosage. Unexpectedly, the study discovered approximately 80 % of patients sought encouragement and counseling while only 20 % of patients sought information on drug dose adjustment. This discovery showed the potential telemedicine could have towards patients’ well-being through the information dissemination, support and influence.
Generally, user-centric design for assistive health technologies is carried out on users who are not patients due to ethical reasons or strong regulations by HTA. The inclusion of CUE as a part of an overarching clinical trial with real patients in real situations can be beneficial to the design process of these technologies because it explores and extracts knowledge on patient perceptions of the technology.
Promise of persuasive technology in telemedicine for type 2 diabetes treatment
Persuasive technology intervention in telemedicine is beneficial for diseases like type 2 diabetes where the only cure is through behavioral management [96]. Diabetes needs strict control of the blood glucose level by balancing food, exercise and insulin (or medication) within the diabetes triangle (Fig. 1) [13]. To educate and motivate a change in eating behavior the persuasive techniques would be an initial recommendation to inform diabetes patients of good food and food to avoid. There exists already multimedia applications via CD-ROM for diabetes self-management counseling that are educational and showed behavior improvements [97]. These applications were simply educational; they could potentially be even more effective by employing persuasive technologies. Motivation and awareness to build better habits for exercise and medication could also be accomplished through persuasion. For example, just-in time messages or triggers can be setup with the appropriate device reminders to take insulin injection or medication.
Persuasive in-home monitoring can make the management of blood glucose levels timely and provide an efficient day-to-day management of diabetes to prevent complicated stages. Interventions for behavior change has been identified as a major cornerstone for changing dietary behaviors [98]. A US study of over 17,000 patients enrolled in a home telehealth program reported a 20 % reduction in hospital admissions and 25 % reduction in bed days of care for chronic health condition management [99]. Recent work has conceptually explored the promises of persuasion techniques if added in existing telemedicine type 2 diabetes in-home monitoring interventions [96].
Pervasive technology and telemedicine
The advent of pervasive technologies (mobile devices, wireless sensor networks) provides a great future for telemedicine in general and specifically for chronic diseases like type 2 diabetes. Telemedicine through the use of pervasive technologies have the potential to change the paradigm of current healthcare models [95, 100].
Two potential challenges may arise. First, a new technology must show enough clinical evidence of improvement of health conditions compared to alternative therapies that have existed before, which is challenging and may slow down the use of pervasive technologies in telemedicine and healthcare. Bardram and Mihailidis [100] called this phenomenon the antithesis of the technology-push mindset found in consumer technologies. Second, how welcoming/resisting will the doctors and nurses be to the new technologies that require changes in the existing healthcare services?
Conclusion
This paper is a meta-synthesis that systematically reviewed a comprehensive list of clinical trials of technology-intervened treatments for the care of type 2 diabetes from HCI perspective. This paper identifies patients as the most important focus of technology-intervened treatments. The meta-synthesis determined there is a need for a new method that could capture the experience of users (patients) in a clinical trial of technology-intervened treatments for type 2 diabetes. To satisfy this need, this paper describes the CUE, which was developed to complement clinical trials in EBP. The CUE was implemented concurrently in a clinical trial and provided insights about the patients as technology users.
The objective of this paper was to assess the types of technology applied and their effectiveness in technology-intervened treatments, which led to two important conclusions to inform future exploration of telemedicine and persuasive technology. First, the reasons for dropout or withdrawal of patients can significantly inform the future development and design of information technology used in technology-intervened treatments. Improvements in telemedicine require knowledge and understanding of how users (patients) physically and emotionally act and react with the technologies. However, currently, the reasons for withdrawal have not been investigated in clinical trials. Second, all of the reviewed papers reported patients had significant behavioral changes via telemedicine techniques although improvements in the physical conditions were not consistent. The outcomes show the potential of telemedicine in the treatment of diseases like type 2 diabetes where the key to success is behavioral change and continuous management.
This paper showed that telemedicine have been effective in providing the education and awareness in the patients’ own well-being. The key to surviving diabetes involves a long-term management of the diabetes triangle model, which includes a balanced control of diet and exercise, home blood glucose testing and insulin (or medication) if required. The majority of the studies reviewed concluded that telemedicine provided significant health improvements in weight management and blood glucose levels.
In-home technology intervened healthcare such as telemedicine and other pervasive healthcare technologies will increase with the demographic shift. Currently, there is a disjuncture between telemedicine and persuasive technology for type 2 diabetes. The technologies used in the clinical trials this paper investigated did not have a persuasive design consideration, yet they had positive behavioral changes to affect well-being. Recent studies suggest that persuasive technology could change behavior in patients with in-home technology intervened treatments. The combination of telemedicine and persuasive technology can provide better solutions for type 2 diabetes treatments.
The full results of CUE project with in-depth analysis will be published in future work. Both the technological and medical reasons for patient withdrawal from clinical trials is important to understand. During future trials, researchers are urged to take an approach towards data collection that would include patients’ physical and emotional actions/reactions with the technologies. Future work will conduct further investigations of measuring effectiveness and integration of telemedicine technology.
References
Bloom, D. E., Canning, D., and Fink, G., The economics of ageing: an editorial introduction - Implications of population ageing for economic growth. Oxford Review of Economic Policy 26(4):581–582, 2010. doi:10.1093/oxrep/grq038.
Lunenfeld, B., and Stratton, P., The clinical consequences of an ageing world and preventive strategies. Best Practice & Research Clinical Obstetrics & Gynaecology 27(5):643–659, 2013. doi:10.1016/j.bpobgyn.2013.02.005.
Jaana, M., and Paré, G., Home telemonitoring of patients with diabetes: a systematic assessment of observed effects. Journal of Evaluation in Clinical Practice 13(2):242–253, 2007.
Wai AAP, Foo SF, Jayachandran M, Biswas J, Nugent C, Mulvenna M, Zhang D, Craig D, Passmore P, Lee JE (2010) Towards developing effective Continence Management through wetness alert diaper: Experiences, lessons learned, challenges and future directions. Paper presented at the 4th International Conference on-NO PERMISSIONS, Munich, Germany, 22–25 March
Meystre, S., The current state of telemonitoring: a comment on the literature. Telemedicine Journal & e-Health 11(1):63–69, 2005.
Finfgeld, D. L., Metasynthesis: The state of the art—so far. Qualitative Health Research 13(7):893–904, 2003.
United States Sensus Bureau (2013) United States Census Bureau. http://www.census.gov/ipc/www/idbpyr.html. Accessed August 16 2013
Australian Bureau of Statistics (2013) Australian Bureau of Statistics. http://www.abs.gov.au. Accessed October 16, 2012
International Diabetes Federation (2013) Diabetes Atlas. http://www.idf.org/diabetesatlas/. Accessed October 29 2013
Buttler D, Liu L, Pu C (2001) A fully automated object extraction system for the World Wide Web. Paper presented at the 21st International Conference on Distributed Computing Systems, Mesa, AZ, USA, April 16–19
Harjumaa M, Isomursu M, Muuraiskangas S, Konttila A (2011) HearMe: A touch-to-speech UI for medicine identification. Paper presented at the 5th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth), Dublin, UK, May 23–26
Diabetes Australia Limited (2013) Diabetes Australia. http://www.diabetesaustralia.com.au/. Accessed 20 July 2013
Benocci M, Bächlin M, Farella E, Roggen D, Benini L, Tröster G (2010) Wearable assistant for load monitoring: recognition of on—body load placement from gait alterations. Paper presented at the 4th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth), Munich, Germany, 22–25 March
Matic A, Mehta P, Rehg JM, Osmani V, Mayora O AID-ME: Automatic Identification of Dressing failures through Monitoring of patients and activity Evaluation. In, 2010. IEEE, pp 1–8
Kanstrup AM, Bertelsen P, Glasemann M, Boye N Design for more: an ambient perspective on diabetes. In: Proceedings of the 10th Anniversary Conference on Participatory Design (PDC08), Indiana, USA, 30 September – 4 October 2008. Indiana University, pp 118–127
Markow T, Ramakrishnan N, Huang K, Starner T, Eicholtz M, Garrett S, Profita H, Scarlata A, Schooler C, Tarun A (2010) Mobile music touch: Vibration stimulus in hand rehabilitation. Paper presented at the 4th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth), Munich, Germany, 22–25 March
Zhang, P., Zhang, X., Brown, J., Vistisen, D., Sicree, R., Shaw, J., and Nichols, G., Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Research and Clinical Practice 87(3):293–301, 2010. doi:10.1016/j.diabres.2010.01.026.
Guyatt, G., Cairns, J., Churchill, D., Cook, D., Haynes, B., Hirsh, J., Irvine, J., Levine, M., and Nishikawa, J., Evidence-based medicine. JAMA: The Journal of the American Medical Association 268(17):2420–2425, 1992.
Sackett, D. L., Rosenberg, W., Gray, J., Haynes, R. B., and Richardson, W. S., Evidence based medicine: what it is and what it isn’t. BMJ 312(7023):71–72, 1996.
Sackett, D. L., Evidence-based medicine. Seminars in perinatology 21(1):3–5, 1997.
Winters, S., Diagnosis by wireless. Scientific American 124:465–465, 1921.
Moore, M., The evolution of telemedicine. Future Generation Computer Systems 15(2):245–254, 1999.
Sood, S., Mbarika, V., Jugoo, S., Dookhy, R., Doarn, C. R., Prakash, N., and Merrell, R. C., What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemedicine and e-Health 13(5):573–590, 2007.
Tachakra, S., Wang, X., Istepanian, R. S. H., and Song, Y., Mobile e-health: the unwired evolution of telemedicine. Telemedicine Journal and E-health 9(3):247–257, 2003.
Orlov, O. I., Drozdov, D. V., Doarn, C. R., and Merrell, R. C., Wireless ECG monitoring by telephone. Telemedicine Journal and E-health 7(1):33–38, 2001.
Anvari, M., Telesurgery: remote knowledge translation in clinical surgery. World journal of surgery 31(8):1545–1550, 2007.
American Telemedicine Association (2013) American Telemedicine Association. www.americantelemed.org. Accessed August 11 2013
Eysenbach G (2001) What is e-health? Journal of medical internet research 3 (2)
Braiterman, J., Verhage, S., and Choo, R., Business: designing with users in Internet time. Interactions 7(5):23–27, 2000.
Lissack, M., and Roos, J., The next common sense: Mastering corporate complexity through coherence. Nicholas Brealey Publishing, London, 1999.
Dalcher D, Drevin L Learning from information systems failures by using narrative and ante-narrative methods. In: Proceedings of the annual research conference of the South African institute of computer scientists and information technologists on: Enablement through technology (SAICSIT ’03), 2003. South African Institute for Computer Scientists and Information Technologists, Republic of South Africa, pp 137–142
Dalcher, D., Software project success: moving beyond failure. The European Journal for the Informatics Professional 10(1):42–50, 2009.
Ekeland, A. G., Bowes, A., and Flottorp, S., Effectiveness of telemedicine: a systematic review of reviews. International journal of medical informatics 79(11):736–771, 2010.
Verhoeven, F., van Gemert-Pijnen, L., Dijkstra, K., Nijland, N., Seydel, E., and Steehouder, M., The contribution of teleconsultation and videoconferencing to diabetes care: a systematic literature review. Journal of Medical Internet Research 9(5), e37, 2007. doi:10.2196/jmir.9.5.e37.
Verhoeven, F., Tanja-Dijkstra, K., Nijland, N., Eysenbach, G., and van Gemert-Pijnen, L., Asynchronous and synchronous teleconsultation for diabetes care: a systematic literature review. Journal of diabetes science and technology 4(3):666–684, 2010.
Orji R, Mandryk RL, Vassileva J, Gerling KM Tailoring persuasive health games to gamer type. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, 2013. ACM, pp 2467–2476
Orji R, Vassileva J, Mandryk RL (2014) Modeling the efficacy of persuasive strategies for different gamer types in serious games for health. User Modeling and User-Adapted Interaction:1–46
Fogg B, Nass C How users reciprocate to computers: an experiment that demonstrates behavior change. In: Proceeding of CHI EA ’97 - CHI ’97 extended abstracts on human factors in computing systems: looking to the future, 1997. ACM, pp 331–332. doi:10.1145/1120212.1120419
Oinas-Kukkonen H (2010) Behavior change support systems: A research model and agenda. In: Persuasive Technology. Springer, pp 4–14
Fogg B, Nass C How users reciprocate to computers: an experiment that demonstrates behavior change. In: CHI’97 extended abstracts on Human factors in computing systems: looking to the future, 1997. ACM, pp 331–332
Oinas-Kukkonen, H., A foundation for the study of behavior change support systems. Personal and ubiquitous computing 17(6):1223–1235, 2013.
Orji R, Vassileva J, Mandryk R (2012) Towards an effective health interventions design: an extension of the health belief model. Online journal of public health informatics 4 (3)
Intille, S. S., A new research challenge: persuasive technology to motivate healthy aging. Information Technology in Biomedicine, IEEE Transactions on 8(3):235–237, 2004.
Fogg, B. J., and Nass, C., Silicon sycophants: the effects of computers that flatter. International Journal of Human-Computer Studies 46(5):551–561, 1997. doi:10.1006/ijhc.1996.0104.
Fogg, B. J., Persuasive technologie301398. Communications of the ACM 42(5):26–29, 1999.
Grimes A, Grinter RE (2007) Designing persuasion: Health technology for low-income African American communities. In: Persuasive Technology. Springer, pp 24–35
Hilliman, C. A., Cimino, J. J., Lai, A. M., Kaufman, D. R., Starren, J. B., and Shea, S., The effects of redesigning the IDEATel architecture on glucose uploads. Telemedicine journal and e-health : the official journal of the American Telemedicine Association 15(3):248–254, 2009. doi:10.1089/tmj.2008.0101.
Shea, S., The Informatics for Diabetes and Education Telemedicine (IDEATel) project. Transactions of the American Clinical and Climatological Association 118:289–304, 2007.
Weinstock, R. S., Teresi, J. A., Goland, R., Izquierdo, R., Palmas, W., Eimicke, J. P., Ebner, S., and Shea, S., Glycemic control and health disparities in older ethnically diverse underserved adults with diabetes: five-year results from the Informatics for Diabetes Education and Telemedicine (IDEATel) study. Diabetes Care 34(2):274–279, 2011. doi:10.2337/dc10-1346.
Leichter, S. B., Bowman, K., Adkins, R. A., and Jelsovsky, Z., Impact of remote management of diabetes via computer: the 360 study–a proof-of-concept randomized trial. Diabetes Technol Ther 15(5):434–438, 2013. doi:10.1089/dia.2012.0323.
Biermann, E., Dietrich, W., and Standl, E., Telecare of diabetic patients with intensified insulin therapy. A randomized clinical trial. Studies in health technology and informatics 77(1):327–332, 1999.
Shultz EK, Bauman A, Hayward M, Rodbard D, Holzman R Improved diabetic prognosis following telecommunication and graphical processing of diabetic data. In: Proceedings of the Annual Symposium on Computer Application in Medical Care, 1991. American Medical Informatics Association, p 53
McFarland, M., Davis, K., Wallace, J., Wan, J., Cassidy, R., Morgan, T., and Venugopal, D., Use of home telehealth monitoring with active medication therapy management by clinical pharmacists in veterans with poorly controlled type 2 diabetes mellitus. Pharmacotherapy 32(5):420–426, 2012. doi:10.1002/j.1875-9114.2011.01038.x.
Stone, R. A., Rao, R. H., Sevick, M. A., Cheng, C., Hough, L. J., Macpherson, D. S., Franko, C. M., Anglin, R. A., Obrosky, D. S., and Derubertis, F. R., Active care management supported by home telemonitoring in veterans with type 2 diabetes: the DiaTel randomized controlled trial. Diabetes Care 33(3):478–484, 2010. doi:10.2337/dc09-1012.
Estrada, C. A., Safford, M. M., Salanitro, A. H., Houston, T. K., Curry, W., Williams, J. H., Ovalle, F., Kim, Y., Foster, P., and Allison, J. J., A web-based diabetes intervention for physician: a cluster-randomized effectiveness trial. International journal for quality in health care : journal of the International Society for Quality in Health Care / ISQua 23(6):682–689, 2011. doi:10.1093/intqhc/mzr053.
Rodriguez-Idigoras, M. I., Sepulveda-Munoz, J., Sanchez-Garrido-Escudero, R., Martinez-Gonzalez, J. L., Escolar-Castello, J. L., Paniagua-Gomez, I. M., Bernal-Lopez, R., Fuentes-Simon, M. V., and Garofano-Serrano, D., Telemedicine influence on the follow-up of type 2 diabetes patients. Diabetes Technol Ther 11(7):431–437, 2009. doi:10.1089/dia.2008.0114.
Watson, A. J., Kvedar, J. C., Rahman, B., Pelletier, A. C., Salber, G., and Grant, R. W., Diabetes connected health: a pilot study of a patient- and provider-shared glucose monitoring web application. J Diabetes Sci Technol 3(2):345–352, 2009.
Eakin, E. G., Reeves, M. M., Marshall, A. L., Dunstan, D. W., Graves, N., Healy, G. N., Bleier, J., Barnett, A. G., O’Moore-Sullivan, T., Russell, A., and Wilkie, K., Living Well with Diabetes: a randomized controlled trial of a telephone-delivered intervention for maintenance of weight loss, physical activity and glycaemic control in adults with type 2 diabetes. BMC public health 10:452, 2010. doi:10.1186/1471-2458-10-452.
Davis, R. M., Hitch, A. D., Salaam, M. M., Herman, W. H., Zimmer-Galler, I. E., and Mayer-Davis, E. J., TeleHealth improves diabetes self-management in an underserved community: diabetes TeleCare. Diabetes Care 33(8):1712–1717, 2010. doi:10.2337/dc09-1919.
Rutten, G., Van Eijk, J., de Nobel, E., Beek, M., and Van der Velden, H., Feasibility and effects of a diabetes type II protocol with blood glucose self-monitoring in general practice. Family practice 7(4):273–278, 1990.
Tsang, M., Mok, M., Kam, G., Jung, M., Tang, A., and Chan, U., Improvement in diabetes control with a monitoring system based on a hand-held, touch-screen electronic diary. Journal of Telemedicine and Telecare 7(1):47–50, 2001.
Kim, S. I., and Kim, H. S., Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Inform 77(6):399–404, 2008. doi:10.1016/j.ijmedinf.2007.07.006.
Biermann, E., Dietrich, W., and Standl, E., Telecare of diabetic patients with intensified insulin therapy. Stud Health Technol Inform 77:327–332, 2000.
Piette, J. D., Weinberger, M., McPhee, S. J., Mah, C. A., Kraemer, F. B., and Crapo, L. M., Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? American Journal of Medicine 108(1):20–27, 2000.
Williams, E. D., Bird, D., Forbes, A. W., Russell, A., Ash, S., Friedman, R., Scuffham, P. A., and Oldenburg, B., Randomised controlled trial of an automated, interactive telephone intervention (TLC Diabetes) to improve type 2 diabetes management: baseline findings and six-month outcomes. BMC public health 12:602, 2012. doi:10.1186/1471-2458-12-602.
Meneghini, L. F., Albisser, A. M., Goldberg, R. B., and Mintz, D. H., An electronic case manager for diabetes control. Diabetes care 21(4):591–596, 1998.
Glasgow, R. E., and Toobert, D. J., Brief, computer-assisted diabetes dietary self-management counseling: effects on behavior, physiologic outcomes, and quality of life. Medical care 38(11):1062–1073, 2000.
McKay, H. G., Glasgow, R. E., Feil, E. G., Boles, S. M., and Barrera, M., Jr., Internet-based diabetes self-management and support: Initial outcomes from the Diabetes Network project. Rehabilitation Psychology 47(1):31, 2002.
Cherry, J. C., Moffatt, T. P., Rodriguez, C., and Dryden, K., Diabetes disease management program for an indigent population empowered by telemedicine technology. Diabetes technology & therapeutics 4(6):783–791, 2002.
Montori, V. M., Dinneen, S. F., Gorman, C. A., Zimmerman, B. R., Rizza, R. A., Bjornsen, S. S., Green, E. M., Bryant, S. C., and Smith, S. A., The Impact of Planned Care and a Diabetes Electronic Management System on Community-Based Diabetes Care The Mayo Health System Diabetes Translation Project†. Diabetes care 25(11):1952–1957, 2002.
Cho, J. H., Chang, S. A., Kwon, H. S., Choi, Y. H., Ko, S. H., Moon, S. D., Yoo, S. J., Song, K. H., Son, H. S., Kim, H. S., Lee, W. C., Cha, B. Y., Son, H. Y., and Yoon, K. H., Long-term effect of the Internet-based glucose monitoring system on HbA1c reduction and glucose stability: a 30-month follow-up study for diabetes management with a ubiquitous medical care system. Diabetes Care 29(12):2625–2631, 2006. doi:10.2337/dc05-2371.
Izquierdo, R. E., Knudson, P. E., Meyer, S., Kearns, J., Ploutz-Snyder, R., and Weinstock, R. S., A comparison of diabetes education administered through telemedicine versus in person. Diabetes care 26(4):1002–1007, 2003.
Young, R. J., Taylor, J., Friede, T., Hollis, S., Mason, J. M., Lee, P., Burns, E., Long, A. F., Gambling, T., and New, J. P., Pro-active call center treatment support (PACCTS) to improve glucose control in type 2 diabetes a randomized controlled trial. Diabetes care 28(2):278–282, 2005.
Cahill, D. J., Thach, S. V., and Warshawsky, R. M., The marketing concept and new high-tech products: is there a fit? Journal of Product Innovation Management 11(4):336–343, 1994.
Bardram JE (2008) Clinical proof-of-concept–A evaluation method for pervasive healthcare systems. Paper presented at the Ubiquitous Systems Evaluation (USE ’08), Seoul, Korea, 21–24 September
Baecker R, Booth K, Jovicic S, McGrenere J, Moore G Reducing the gap between what users know and what they need to know. In: Proceedings on the 2000 conference on Universal Usability, 2000. ACM, pp 17–23
Carroll, J. M., and Carrithers, C., Training wheels in a user interface. Communications of the ACM 27(8):800–806, 1984.
Lazar, J., User-centered Web development. Jones & Bartlett Learning, Sudbury, MA, USA, 2001.
Bujnowska-Fedak, M. M., Puchala, E., and Steciwko, A., The impact of telehome care on health status and quality of life among patients with diabetes in a primary care setting in Poland. Telemedicine journal and e-health : the official journal of the American Telemedicine Association 17(3):153–163, 2011. doi:10.1089/tmj.2010.0113.
Reeves, B., and Nass, C., The media equation: how people treat computers, television, and new media like real people and places. Cambridge University Press, United Kingdom, 1996.
Faridi, Z., Liberti, L., Shuval, K., Northrup, V., Ali, A., and Katz, D. L., Evaluating the impact of mobile telephone technology on type 2 diabetic patients’ self-management: the NICHE pilot study. J Eval Clin Pract 14(3):465–469, 2008. doi:10.1111/j.1365-2753.2007.00881.x.
Lavery, L. A., Higgins, K. R., Lanctot, D. R., Constantinides, G. P., Zamorano, R. G., Armstrong, D. G., Athanasiou, K. A., and Agrawal, C., Home monitoring of foot skin temperatures to prevent ulceration. Diabetes care 27(11):2642–2647, 2004.
Steele, R., Lo, A., Secombe, C., and Wong, Y. K., Elderly persons’ perception and acceptance of using wireless sensor networks to assist healthcare. International journal of medical informatics 78(12):788–801, 2009. doi:10.1016/j.ijmedinf.2009.08.001.
Jadad, A. R., Moore, R. A., Carroll, D., Jenkinson, C., Reynolds, D. J. M., Gavaghan, D. J., and McQuay, H. J., Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled clinical trials 17(1):1–12, 1996.
Olivo, S. A., Macedo, L. G., Gadotti, I. C., Fuentes, J., Stanton, T., and Magee, D. J., Scales to assess the quality of randomized controlled trials: a systematic review. Physical therapy 88(2):156–175, 2008.
Long, A. F., Gambling, T., Young, R. J., Taylor, J., and Mason, J. M., Acceptability and satisfaction with a telecarer approach to the management of type 2 diabetes. Diabetes care 28(2):283–289, 2005.
Zolfaghari, M., Mousavifar, S. A., Pedram, S., and Haghani, H., The impact of nurse short message services and telephone follow-ups on diabetic adherence: which one is more effective? Journal of clinical nursing 21(13–14):1922–1931, 2012. doi:10.1111/j.1365-2702.2011.03951.x.
Tang, P. C., Overhage, J. M., Chan, A. S., Brown, N. L., Aghighi, B., Entwistle, M. P., Hui, S. L., Hyde, S. M., Klieman, L. H., Mitchell, C. J., Perkins, A. J., Qureshi, L. S., Waltimyer, T. A., Winters, L. J., and Young, C. Y., Online disease management of diabetes: engaging and motivating patients online with enhanced resources-diabetes (EMPOWER-D), a randomized controlled trial. Journal of the American Medical Informatics Association : JAMIA 20(3):526–534, 2013. doi:10.1136/amiajnl-2012-001263.
Carlisle, K., Warren, R., Scuffham, P., and Cheffins, T., Randomised Controlled Trial of an In-Home Monitoring Intervention to Improve Health Outcomes for Type 2 Diabetes: Study Protocol. Studies in Health Technology and Informatics 182(1):43, 2012. doi:10.3233/978-1-61499-152-6-43.
Wells, J. D., Campbell, D. E., Valacich, J. S., and Featherman, M., The effect of perceived novelty on the adoption of information technology innovations: a risk/reward perspective. Decision Sciences 41(4):813–843, 2010.
Clark RE, Craig TG (1992) Research and theory on multi-media learning effects. In: Interactive multimedia learning environments. Springer, pp 19–30
Beyer, H., and Holtzblatt, K., Contextual design: defining customer-centered systems. Morgan Kaufmann, Burlington, MA, USA, 1997.
Jalil S, Myers T, Atkinson A Design Implications from the Preliminary Results of a Telemedicine Patient-Technology Interaction Study. In: The 7th International Symposium on Visual Information Communication and Interaction (VINCI’ 2014), Sydney, Australia, 6–8 August 2014 2014. ACM,
TechCast Global (2013) TechCast a virtual think tank tracking the technology revolution. http://www.techcast.org/BreakthroughAnalysis.aspx?ID=52. Accessed 17 June 2013
Bardram, J. E., Pervasive healthcare as a scientific discipline. Methods of Information in Medicine 47(3):178–185, 2008.
Jalil S (2013) Persuasion for in-home technology intervened healthcare of chronic disease: Case of diabetes type 2. Paper presented at the Adjunct Proceedings of 8th International Conference on Persuasive Technology (Persuasive-2013), Sydney, Australia, April 3–5
Trossen, D., and Pavel, D., Sensor networks, wearable computing, and healthcare Applications. Pervasive Computing, IEEE 6(2):58–61, 2007.
Lau, D. C., Douketis, J. D., Morrison, K. M., Hramiak, I. M., Sharma, A. M., and Ur, E., 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. Canadian Medical Association Journal 176(8):S1–S13, 2007.
Darkins, A., Ryan, P., Kobb, R., Foster, L., Edmonson, E., Wakefield, B., and Lancaster, A. E., Care coordination/home telehealth: the systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemedicine and e-Health 14(10):1118–1126, 2008.
Bardram JE, Mihailidis A (2006) Pervasive computing in healthcare. CRC
Hassenzahl, M., Diefenbach, S., and Göritz, A., Needs, affect, and interactive products-Facets of user experience. Interacting with computers 22(5):353–362, 2010.
Pressman, A. R., Kinoshita, L., Kirk, S., Barbosa, G. M., Chou, C., and Minkoff, J., A novel telemonitoring device for improving diabetes control: protocol and results from a randomized clinical trial. Telemedicine journal and e-health : the official journal of the American Telemedicine Association 20(2):109–114, 2014. doi:10.1089/tmj.2013.0157.
Acknowledgments
The authors would like to thank the participants who volunteered in the CUE and the Townsville-Mackay Medicare Locals (TMML) who conduct the clinical trials and Dianna Hardy from James Cook University, Australia and Professor Alison Bowes from the University of Stirling, Scotland, for their expertise, interest, helpful discussions and feedback.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Education & Training
Appendix I
Appendix I
Rights and permissions
About this article
Cite this article
Jalil, S., Myers, T. & Atkinson, I. A Meta-Synthesis of Behavioral Outcomes from Telemedicine Clinical Trials for Type 2 Diabetes and the Clinical User-Experience Evaluation (CUE). J Med Syst 39, 28 (2015). https://doi.org/10.1007/s10916-015-0191-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-015-0191-9