Abstract
Previous studies have suggested that electronic medical records (EMR) can lead to a greater reduction of medical errors and better adherence to regulatory compliance than paper medical records (PMR). In order to assess the organizational performance and regulatory compliance, we tracked different clinical pertinence indicators (CPI) in our anesthesia information management system (AIMS) for 5 years. These indicators comprised of the protocols from the Surgical Care Improvement Project (SCIP), elements of performance (EP) from The Joint Commission (TJC), and guidelines from the Centers for Medicare and Medicaid Services (CMS). A comprehensive AIMS was initiated and the CPI were collected from October 5, 2009 to December 31, 2010 (EMR period) and from January 1, 2006 to October 4, 2009 (PMR period). Fourteen CPI were found to be common between the EMR and PMR periods. Based on the statistical analysis of the 14 common CPI, there was a significant increase (p < 0.001) in overall compliance after the introduction of EMR compared to the PMR period. The increase in overall compliance was significantly progressive (p = 0.013) from year to year over 2006 and 2010. Of the 14 CPI, Documentation of a) medication doses, and b) monitoring of postoperative physiological status, mental status, and pain scores showed significant improvement (p < 0.001) during the EMR period compared to the PMR period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Electronic medical records (EMR) have been increasingly used by healthcare professionals to minimize the space required to store paper medical records (PMR), improve workflow efficiency, provide faster retrieval of patient documents, and to facilitate speedy sharing of patient information among care givers [1–4]. The Centers for Medicare and Medicaid Services (CMS) specified a set of standards for the meaningful use of EMR. CMS further provided monetary incentives to healthcare providers and hospitals using EMR, through the Health Information Technology for Economic and Clinical Health (HITECH) Act [5,6].
Specifically for anesthesia practice, an anesthesia information management system (AIMS) was developed to facilitate completeness of documentation for patient safety, audit trails for accurate record keeping, medico-legal litigations, and health insurance reimbursements [7–10]. To enhance data completeness, accuracy and capture, we implemented mandatory structured data entry (SDE) fields in different anesthesia scripts of the AIMS used at our institution. This ensures compliance with documentation since the practitioners cannot lock the system without completing these mandatory SDE fields. This facilitates the capture of events in a time-stamped sequence [11].
Hospitals are expected to implement procedures to determine when anesthesia and analgesia are administered, and to specify the requirements for the practitioners who administer anesthesia and analgesia. CMS specified the following 7 sets of details to be incorporated into the anesthesia care records: (1) preanesthesia examination and evaluation; (2) type of anesthesia or analgesia assessed, planned, and administered; (3) was a licensed practitioner present during induction, administration of anesthesia or analgesia, and emergence; (4) did a qualified individual administered the anesthesia or analgesia; (5) values of vital signs monitored during anesthesia or analgesia; (6) was a licensed practitioner available to diagnose and treat immediate emergencies; and (7) postoperative anesthesia care provided [12].
The Joint Commission (TJC) standardized the elements of performance (EP) and these were adopted by our department as clinical pertinence indicators (CPI). The main goal of the present study was to closely track the CPI in order to monitor patient safety, improve regulatory compliance, and reduce surgical complications as part of the Surgical Care Improvement Project (SCIP). Our hypothesis was that documenting the patient data with EMR in AIMS would lead to higher regulatory compliance than recording the patient data with PMR.
Methods
This study was conducted at Maimonides Medical Center, a 705-bed university affiliated teaching hospital, in Brooklyn, New York. This was a retrospective chart review study approved by the institutional review board. Following was the process for chart review: A convenient sample of 60–80 charts were reviewed every month. About 3 charts were reviewed by each Anesthesia resident. Data pertaining to preoperative screening, preanesthesia evaluation, perioperative care, and postoperative phases were collected according to SCIP and TJC standards. The PI committee evaluated the aggregate report from the chart review and areas of deficiency/noncompliance were identified. We tabulated the CPI results from January 1, 2006 to October 4, 2009 for our PMR, and from October 5, 2009 to December 31, 2010 for our EMR periods.
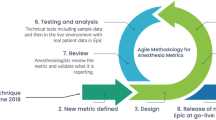
Deployment of AIMS occurred in phases in order to ensure allocation of appropriate information technology support, minimize system malfunction, and facilitate software troubleshooting [9]. Our AIMS was designed by Centricity® Perioperative Anesthesia, GE Healthcare, Barrington, IL. It uses a graphical user interface icon to allow user to click on a custom-made anesthesia script for a specific or common surgical procedure. The script contains a systematic sequence of critical core events that must be selected and completed by the providers in order for the case to end (Table 1). Under these core events, SDE fields consist of drop-down menus such as documenting prophylactic antibiotic and beta blocker administration, tracheal intubation grade, patient’s positioning, and postanesthesia pain score and vital signs that are charted in a time-stamped sequence to facilitate accuracy of data entry. Figure 1 shows a typical anesthesia template for our AIMS.
The number of specific CPI fields collected between 2006 and 2009 were 42 (Table 2). In 2010, the data collection was greatly streamlined, so that only 27 data fields covered all of the CPI attributes. We identified 14 data fields that were common to both PMR and EMR, and these are highlighted in gray in Table 2. Although the specific codes given to these data fields were slightly different between the EMR and PMR years, the descriptive labels for the respective fields were almost the same.
Statistical analysis of the data was performed using SPSS (SPSS, Chicago, IL). Descriptive statistics were used to calculate the mean and standard deviation values for the 14 common CPI fields. Mann–Whitney rank sum test was used to assess the significance of differences in CPI compliance between the EMR and PMR periods. Significance of differences in compliance among different years was compared using the Kruskal-Wallis one-way analysis of variance on ranks. Multiple comparison tests for the EMR and PMR years were performed using the Bonferroni-Dunn test. A p < 0.05 was considered to be statistically significant.
Results
In order to assess the overall increase in compliance during the EMR compared to PMR periods, the percent compliance for all of the 14 CPI data fields for EMR and PMR were separately added, and the mean and standard deviation values were calculated. Mann–Whitney rank sum test showed that there was a significant increase (p < 0.001) in the overall percent compliance with the introduction of the EMR compared to the PMR period (Fig. 2).
The overall regulatory compliance with 14 CPI parameters during the PMR years (2006–2009) and EMR year (2010). The bars represent mean values and the vertical lines represent standard deviation values. The significance of difference between EMR and PMR periods was evaluated using Mann–Whitney rank sum test
To track the yearly increase in overall compliance between 2006 and 2010, the percent compliance of all the 14 data fields was added and the mean and standard deviation values were calculated. There was an increasing trend in the overall percent compliance from 2006 to 2010 (Fig. 3). Kruskal-Wallis one-way analysis of variance on ranks revealed that the difference in percent compliance among the 5 yearly periods was statistically significant (p = 0.013). Bonferroni-Dunn multiple comparison test showed that there was significant increase (p < 0.05) in overall percent compliance in 2010 compared to 2008 and 2009, but not compared to 2006 or 2007, probably because of the large variations in overall percent compliance in 2006 and 2007. Similar comparisons between 2009 and each of the other PMR years did not show any significant differences.
Annual changes in the overall regulatory compliance with 14 CPI parameters during the PMR years (2006–2009) and EMR year (2010). The closed circles represent mean values and the vertical lines represent standard deviation values. The significance of change in compliance between EMR and PMR periods was evaluated using Kruskal-Wallis one-way analysis of variance
To identify the specific CPI parameters which showed significant increase in compliance during the PMR to EMR periods, the mean and standard deviation values for each of the 14 CPI parameters for each of the 5 years were calculated, and shown in Table 3. Kruskal-Wallis one-way analysis of variance on ranks in the PMR and EMR years showed that there was a significant improvement in documentation of all medication dosages (p < 0.001) during the EMR compared to the PMR years (Fig. 4). Monitoring of patient’s physiological status, mental status, and pain also showed significant improvement in documentation (p < 0.001) during the EMR compared to the PMR years (Fig. 4). There was a progressive increase in compliance with antibiotic administration within 60 min during EMR compared to PMR period, but the difference was not statistically significant (p = 0.220). There were no significant differences in the other CPI parameters during the EMR compared to the PMR years.
Annual changes in percent regulatory compliance of two CPI parameters during the PMR years (2006–2009) and EMR year (2010). The circles represent the mean values and the vertical lines represent standard deviation values. The significance of change in compliance between EMR and PMR periods for each CPI parameter was evaluated using Kruskal-Wallis one-way analysis of variance
Discussion
The introduction of the AIMS increases the time efficiency in the workplace. Studies have shown that AIMS records require less time to complete the required documentation and these are better quality records than manual anesthesia records [1]. Illegible handwriting, ambiguous and incomplete data, and poor accessibility have made PMR an unfavorable medium in which health records can be effectively collected, stored, and disseminated. AIMS has the ability to capture real-time intraoperative data electronically and preserve case information as reliably and securely as possible.
In three case reports, analysis of the automatic data capturing from inhalational gas concentration facilitated in identifying the cause of intraoperative awareness during general anesthesia [13]. Furthermore, handwritten anesthesia records are less reliable and often subject to “data smoothing” where extremes of vital signs (e.g., arterial blood pressure and heart rate) are exaggerated to make data look more homogenous [14]. However, further studies are warranted to establish that AIMS increases the regulatory compliance, and thus indirectly leads to improvement in patient safety and better outcomes.
Our present study showed a significantly higher (p < 0.001) rate of compliance in the year we initiated the EMR (99.0 %) compared to the PMR period (96.2 %). Reasons could be that AIMS software has mandatory SDE function that forces users to enter information without fail (for example: EMR cannot be closed without completion of the mandatory SDEs in the script), and sends a reminder to the provider if the tasks are not completed before the case is closed. When we used an earlier version of AIMS during the last 3 months of 2009, some of the customized SDE fields allowed users to end a case without completion of the mandatory fields. This affected the overall compliance when we tabulated the EMR results. It is important to note that introduction of the mandatory SDE function increased the compliance significantly. However we could not achieve 100 % compliance because there were some CPI elements which were not part of the intraoperative script but, were part of the preoperative or postoperative charts.
Of the 14 common fields between the EMR and PMR periods, significant improvement was reported in documenting all medications used (98.5 % vs. 75.6–92.3 %). Significant improvement also occurred in documentation of the monitoring of patient’s physiological status, mental status, and pain level postoperatively (96.2 % vs. 55.9–86.6 %) after AIMS implementation. One possibility could be that EMR allowed for more accurate and legible recording of all medications administered and documentation of patient’s vital signs and pain scores as compared to PMR. A recent study by Wrightson showed electronic anesthetic records were more complete in recording intravenous drugs and medications used during surgical procedures than handwritten records [15].
Compliance for antibiotic administration within 60 min was slightly higher for EMR than the PMR period (95.3 % vs. 91.6 %), but the difference was not significant. Compliance of antibiotic administration can be greatly improved if an interactive visual reminder is integrated into AIMS, so that it will keep reminding the anesthesiologist to prophylactically administer the antibiotic from the beginning of the case, until it is given and documented [16]. Introducing such interactive prompts into AIMS, would significantly improve the compliance for timely administration of prophylactic antibiotics. This could help prevent surgical site infections (SCIP criteria), and thus indirectly lead to better patient outcomes. Similarly, introduction of the point-of-care electronic prompts was reported to be an effective means of increasing compliance and improving outcome [17].
In order to further improve the overall compliance, our department mandates the completion of the EMR within a specified time, and checks for compliance on a monthly basis. Every quarterly, the department sends out a list of documentation deficiencies to the delinquent faculty and residents in order to improve compliance. For residents, it is a measure of their professionalism as part of the Accreditation Council for Graduate Medical Education (ACGME) core competencies. For faculty, it translates into monetary incentives as part of their year-end bonus.
References
Edsall, D. W., Deshane, P., Giles, C., et al., Computerized patient anesthesia records: less time and better quality than manually produced anesthesia records. J. Clin. Anesth. 5(4):275–283, 1993.
Tang, P. C., LaRosa, M. P., and Gorden, S. M., Use of computer-based records, completeness of documentation, and appropriateness of documented clinical decisions. J. Am. Med. Inform. Assoc. 6(3):245–251, 1999.
Devitt, J. H., Rapanos, T., Kurrek, M., Cohen, M. M., and Shaw, M., The anesthetic record: accuracy and completeness. Can. J. Anaesth. 46(2):122–128, 1999.
Roukema, J., Los, R. K., Bleeker, S. E., et al., Paper versus computer: feasibility of an electronic medical record in general pediatrics. Pediatrics 117(1):15–21, 2006.
Blumenthal, D., Launching HITECH. N. Engl. J. Med. 362(5):382–385, 2010.
Classen, D. C., and Bates, D. W., Finding the meaning in meaningful use. N. Engl. J. Med. 365(9):855–858, 2011.
Vigoda, M. M., and Lubarsky, D. A., The medicolegal importance of enhancing timeliness of documentation when using an anesthesia information system and the response to automated feedback in an academic practice. Anesth. Analg. 103(1):131–136, 2006.
Driscoll, W. D., Columbia, M. A., and Peterfreund, R. A., An observational study of anesthesia record completeness using an anesthesia information management system. Anesth. Analg. 104(6):1454–1461, 2007.
Muravchick, S., Caldwell, J. E., Epstein, R. H., et al., Anesthesia information management system implementation: a practical guide. Anesth. Analg. 107(5):1598–1608, 2008.
Jang, J., Yu, S. H., Kim, C. B., Moon, Y., and Kim, S., The effects of an electronic medical record on the completeness of documentation in the anesthesia record. Int. J. Med. Inform. 82(8):702–707, 2013.
Avidan, A., and Weissman, C., Context-sensitive mandatory data-entry fields for data completeness and accuracy in anesthesia information management systems. Can. J. Anaesth. 60(3):325–326, 2013.
CMS Manual System. §482.52 Condition of participation: Anesthesia services. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R74SOMA.pdf Accessed: 8/9/13
Driscoll, W. D., Columbia, M. A., and Peterfreund, R. A., Awareness during general anesthesia: analysis of contributing causes aided by automatic data capture. J. Neurosurg. Anesthesiol. 19(4):268–272, 2007.
Reich, D. L., Wood, R. K., Jr., Mattar, R., et al., Arterial blood pressure and heart rate discrepancies between handwritten and computerized anesthesia records. Anesth. Analg. 91(3):612–616, 2000.
Wrightson, W. A., A comparison of electronic and handwritten anaesthetic records for completeness of information. Anaesth. Intensive Care. 38(6):1052–1058, 2010.
Wax, D. B., Beilin, Y., Levin, M., et al., The effect of an interactive visual reminder in an anesthesia information management system on timeliness of prophylactic antibiotic administration. Anesth. Analg. 104(6):1462–1466, 2007.
Schwann, N. M., Bretz, K. A., Eid, S., et al., Point-of-care electronic prompts: an effective means of increasing compliance, demonstrating quality, and improving outcome. Anesth. Analg. 113(4):869–876, 2011.
Acknowledgments
The authors would like to thank Murali Pagala, Ph.D. for providing statistical analysis of the data and critically reading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Choi, C.K., Saberito, D., Tyagaraj, C. et al. Organizational Performance and Regulatory Compliance as Measured by Clinical Pertinence Indicators Before and After Implementation of Anesthesia Information Management System (AIMS). J Med Syst 38, 5 (2014). https://doi.org/10.1007/s10916-013-0005-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-013-0005-x