Abstract
Many medical organizations have deployed electronic medical record (EMR) information systems (IS) to improve medical decision-making and increase efficiency. Despite their advantages, however, EMR IS may make less of a contribution in the stressful environment of an emergency department (ED) that operates under tight time constraints. The high level of crowdedness in the EDs itself can cause physicians to make medical decisions resulting in more unnecessary admissions and fewer necessary admissions. Thus this study evaluated the contribution of an EMR IS to physicians by investigating whether EMR IS leads to improved medical outcomes in points of care in EDs under different levels of crowdedness. For this purpose a track log-file analysis of a database containing 3.2 million ED referrals in seven main hospitals in Israel (the whole population in these hospitals) was conducted. The findings suggest that viewing medical history via the EMR IS leads to better admission decisions, and reduces the number of possibly avoidable single-day admissions. Furthermore, although the ED can be very stressful especially on crowded days, physicians used EMR IS more on crowded days than on non-crowded days. These results have implications as regards the viability of EMR IS in complex, fast-paced environments.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction and background
Emergency departments (EDs) are traditionally associated with inefficiency and long waits [1]. Overcrowding is a common phenomenon in EDs globally. Schneider et al. [2] found that 91 % of hospital ED heads in the USA reported overcrowding as a problem. They showed that severe overcrowding in EDs has become the accepted standard of care [2] and that overcrowding in EDs is not related to a particular season, since a high volume of referrals were found for different periods of the year and for different months.
Overcrowding is hard to define but easy to recognize in an ED [3]. A stroll through an ED with patients in stretchers or beds in the corridors, conference rooms and offices converted into patient-care space, a crowded waiting room, and harried nurses and physicians are clearly the sign of an overcrowded department. ED crowding is one consequence of the growing demand for health care and a deficit in available hospital and ED beds, and has become an increasingly significant public health problem [4]. Bair et al. [4] studied patients who leave without being seen; this situation is commonly used as an indicator of ED efficiency. According to McCabe [3], many factors contribute to ED overcrowding. The numbers of EDs and hospital beds have decreased as a result of downsizing, closing, and merging of health care institutions. This has led to an increase in patient volume. Because of the shift to outpatient services, sicker patients reach the ED. This leads to longer evaluation and treatment times. Similarly, referrals of uninsured and nursing home patients result in more complex and longer use of the ED, due to delays in seeking needed medical information.
Many hospitals are choosing to admit elective cases rather than allocating available beds to waiting ED patients. Emergency physicians often find it difficult to obtain timely consultations from the hospital medical staff and must make alternate arrangements or transfer patients to other facilities for care. This is further exacerbated by the current nursing shortage. Finally, emergency medicine has evolved as an intensively diagnosis-oriented specialty that relies heavily on ancillary services such as radiology and clinical pathology that lead to (additional) long delays for patients.
Although ED overcrowding has been a topic of frequent investigation, recent studies have tended to focus on factors outside of the ED itself. Hwang & Concato [5] examined how ED overcrowding is defined in the medical literature. They found that the majority of articles with explicit definitions had criteria that were based on hospital factors (e.g., number of referrals, availability of beds elsewhere in the hospital), external factors (e.g., status regarding ambulance diversion), or a combination of categories. In addition, factors used to define overcrowding need to be distinguished from possible causes (e.g., a shortage of nurses for available positions) and effects (e.g., decreased efficiency of care) of overcrowding. Gillies and Howard [6] claimed that some of the overcrowding effect could be overcome by increasing points of care in the community. Nursing hours are also an indication of the time nurses have to care for each patient, which thus impacts the quality of service; i.e., longer nursing hours mean that patients receive better quality medical care [7].
Currently, overcrowding in EDs often results in inferior clinical outcomes and medical errors in almost every facet of emergency care, including diagnostic errors, malfunctioning administrative procedures, erroneous documentation, and wrong pharmacotherapy [8]. The availability of patients’ long term health records, including information about medications, diagnoses, recent procedures, and recent laboratory tests, is critical to forming an appropriate plan of care [9]. Studies have demonstrated a clear association between reviewing of medical history and improved medical care, including admission decisions [10, 11]. For instance, it was suggested that experts are vulnerable to heuristics such as premature closure, where they reach a conclusion rapidly and disregard evidence for competing hypotheses. Reasoning is further taxed when there are large numbers of patients and a high degree of medical uncertainty [12, 13]. Lack of easy access to a full medical history may contribute to poor heuristics, although it has been claimed that a physician can reach valid, reasonable conclusions regarding medical treatment despite imperfect information about the patient [14]. It is sometimes argued that the introduction of extended information and care options compounds rather than simplifies decision complexity [15].
The aim of this study
The main objective of this study was to assess the impact of EMR IS on admission decisions by physicians in the high-stress environment of EDs as a function of level of crowdedness.
Specifically, we examined the impact of viewing medical information from a very large EMR IS on admission decisions. One of the most important decisions in an ED is whether or not to admit a patient. It was suggested that about one out of seven admissions to an ED is due to missing information [16]. Recently it was suggested that EMR availability was associated with a lower likelihood of hospitalization, though the evidence is not inclusive [17]. Finally, viewing medical history may encourage stricter adherence to medical guidelines, which have been shown to be associated with reduced ED visits and hospitalizations [18].
In addition to the proportion of admissions, we examined how the proportion of single-day admissions fluctuates when a patient’s medical history is inspected via EMR IS. We assumed that part of the single-day admissions are uncalled for, and could be prevented if a comprehensive medical history were available. These measures have been used in previous studies [8, 19].
The database for this study comes from the main health maintenance organization (HMO) in Israel, which is also one of the world’s largest non-governmental HMOs. This HMO is a non-profit organization that serves over 3.8 million customers and employs more than 9,000 physicians. The HMO owns seven general hospitals (all surveyed in this research), and seven other hospitals, including geriatric and pediatric facilities, and more than 1,300 community clinics.
In 2004, the HMO deployed the EMR IS analyzed here. The EMR IS retrieves data from many medical systems. This data retrieval architecture provides a comprehensive, integrated and real time virtual patient record available at all points of care of the HMO. The system gathers historical patient data from the other healthcare information systems at the HMO’s hospitals and clinics. The data in this study included patients’ demographics, chronic medication, adverse reactions, detailed lab and imaging results, past diagnoses, healthcare procedures, etc. Actual usage of the system at each of the seven hospitals is idiosyncratic because of differences in management policy relating to the system, electronic order entry in general, and the influence of other technologies on cooperation among physicians within each hospital. The database for this study covered 2004 to 2007 (after the EMR IS had been integrated into all hospitals) from all seven hospitals.
This paper is organized as follows: Section 3 describes the methodology, section 4 reports the research findings, section 5 presents the conclusions and discusses the findings, section 6 states the research contribution, and section 7 analyzes the research limitations with some suggestions for future research.
Methodology
The research method selected for this study was track log-file analysis. Track log-file analysis uses statistical tools such as multivariate logistic regression. The log-files were based on data from seven main hospitals owned by the main HMO in Israel, which uses an EMR IS to share medical information from distributed health suppliers. We drew the research variables from this log file in a way comparable to methodologies in similar studies.
The dependent variables
Admission decision
Admission decision was defined as a dichotomous variable to admit a patient to the ED or not (1 for admit decision and 0 for discharge decision). This variable has been used in previous research [20].
Single-day admission
This variable quantified whether a patient, as a result of the decision to admit, was admitted for a single day (coded 1) or for a longer period of time (coded 0). Previous works have shown that such short-term admissions can be reduced using medical information [19, 21].
The definition of single day admissions filtered out patients who intentionally sought and received treatment involving a single day admission. Only admissions from an ED to a specific hospital department were recorded and included. In addition, similar to many EDs around the world, hospitals in Israel maintain observation wards in which patients are monitored for a period of 12–24 hours. This period of observation was not included in the calculations. To assess the impact of interoperability on admission decisions, medical history which existed at the local EMR in certain hospitals was differentiated from the medical history which was exclusively provided online from several decentralized health suppliers.
The dependent variables ‘admission decision’ and ‘single-day admission’ are connected since a ‘single-day admission’ is a subset of ‘admission decision’. However, we were careful not to use these two variables in the same statistical test or regression but rather in separate tests and regressions.
The independent variables
Viewed medical history
The patients in our study were divided into two groups: patients whose medical history was viewed via the EMR IS and patients whose medical history was not viewed via the EMR IS. Vest [22] recently found that system access is not random, and that specific patient factors increased the likelihood of information access. Vest’s [22] findings show that the more a person’s data were examined, the more likely that person was to have more ED visits and inpatient hospitalizations.
The term ‘viewed medical history’ refers to access to at least one of several medical history components in the EMR IS (see Table 1). This was measured as a dichotomous variable (1 = history viewed, 0 if not).
Crowdedness level
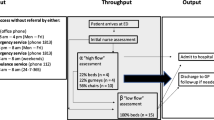
One of the main independent variables in this study was the crowdedness level of the ED. Richardson [20] distinguished between the volume of crowdedness in EDs on weekdays and weekends, and found different levels of referrals (the number of referrals on weekdays was higher than the number of referrals on weekends). He divided the days in EDs into “Busy weekday” vs. “Non-busy weekday” and “Busy weekend day” vs. “Non-busy weekend day” to capture different levels of referrals. We chose to extend this suggested division. We defined a “Crowded day” according to the data for each day individually, corresponding to a specific hospital, i.e. we tailored a specific “Crowded day” measurement to a specific healthcare facility on a given weekday. For instance, the average number of referrals per day was calculated separately for Sundays (considered the first day of the week in Israel) for each hospital (controlling for the differences between hospitals such as facilities, beds and medical staff members and controlling for the differences between days such as weekdays, weekend days and holidays). If the number of referrals in hospital N on a certain Sunday exceeded the average number of referrals on Sundays in this hospital, we termed this one Sunday a “Crowded day”. This yielded 49 distinct “Crowded day” classifications—matched for each weekday and for each hospital’s average number of referrals. See Table 2 for the 49 classifications.
For each referral, we assigned the day of the week and the name of the hospital. Thus here we formulated the independent variable representing “crowded day” for each referral in our study as a dichotomous variable (value = 1 for a crowded day and value = 0 for a non-crowded day). This main variable (crowded day) was assigned a value of 1, if the number of referrals on that day was above the average number of referrals per day in the same hospital on the same day of the week (otherwise the value assigned was 0).Footnote 1
Health maintenance organization
The EMR IS chosen for this study provides full integrative information only on patients belonging to the main HMO. To control for major discrepancies in the quality and the amount of medical information between the main HMO patients and other HMO patients, a dichotomous variable was created (1—if the patient was a member of the main HMO, for whom full medical history was available via the IS or 0—if the patient was not a member of the main HMO).
ED department
This variable represented the specific type of unit where the patient was evaluated in the ED. The EDs in the log-file were internal medicine, surgery, obstetrics, orthopedics, gynecology, ENT (ear, nose & throat), primary, and dermatology.
Hospital
This variable represented the specific hospital where the patient was evaluated. Each one of the seven hospitals had a different code represented by this variable (due to specificities such as policies).
Patient age
Continuous variable representing the age of the patient.
Patient gender
Male/Female.
Research findings
Descriptive statistics
The log-file consisted of 3,219,910 referrals. The names of the hospitals are not disclosed for reasons of confidentiality and privacy.
First, there were slightly more referrals to the hospitals’ EDs during crowded days, which is consistent with the literature (about 52.4 % of the referrals and 51.8 % of the admissions). Second, as shown in Table 3 the distributions of crowded days as compared to non-crowded days were quite similar for all referrals, suggesting that there were no differences in the crowdedness levels between different types of gender or insurance. Third, and most strikingly, patients’ medical histories were viewed in the ED in only 16.12 % of all referrals to all hospitals. Thus, 83.88 % of all referrals and 76.27 % of all admissions did not involve any use of medical history. Finally, and contrary to expectations, physicians used medical information on crowded days more than on non-crowded days (17.17 % vs. 14.97 % respectively of all referrals).
Table 3 shows the average referrals per day and hospital. These averages were used to determine whether a referral occurred on a crowded day in the ED (if the number of referrals exceeded the average number of referrals on the same day in the same hospital) or not. For instance, if on a specific Sunday in Hospital1 the total number of referrals was above 643.4 (the average number of referrals per Sunday in Hospital1) that day was defined as a Crowded Day (otherwise it was defined as an non--crowded day).
Table 4 suggests that there were some differences in the level of crowdedness between hospitals.
Table 5 shows the total rate of admissions for the 9 main ED departments in terms of their different crowdedness levels. It shows that there were very similar distributions of crowded days vs. non-crowded days. The percentage of admissions during crowded days in the Internal medicine departments was higher than the percentage of admissions in the surgical departments.
To sum up, there were no striking differences in the levels of crowdedness for the different EDs, gender or medical insurance. However, there were minor differences between distributions for crowded days vs. non-crowded days by hospital.
The outcomes of the regressions
Logistic regression is a statistical tool which is used extensively in the medical field and the social sciences. The logistic regression function has a number of advantages [23]. For example, while not all statistical tools are applicable to the specific dichotomous nature of outcome measures such as enrollment, persistence and attainment, the logistic regression can deal with these types of data. The logistic regression adjusts the outcomes so that each independent variable is assigned its own true weight in the equation [24–29].
We ran the logistic regressions using three blocks of variables: 1) Treatment variables (history viewing, age, insurance provider, gender and crowdedness), 2) Control variables for type of department (for example, example internal medicine and surgery), and 3) Control variables for different hospitals (due to various differences such as policies). These regressions reflect the pure contribution of previous information to the rate of admissions and single day admissions (Block 2 and Block 3 are not shown here, but were included in these regressions).
As shown in Table 6, when history is viewed the likelihood of being admitted to the ED increases by 42.6 % (95 % CI = 1.416–1.436, adjusted OR = 1.426).
When the age of the patients increases by 1 year, the likelihood of admission to the ED increases by 3.3 % (95 % CI = 1.033–1.033, adjusted OR = 1.033).
When the insured patients are not members of the main HMO, the likelihood of admissions increases by 9.3 % (95 % CI = 0.902–0.913, adjusted OR = 0.907).
For male patients, the likelihood of admissions to the ED increases by 16.2 % in comparison to female patients (95 % CI = 1.155–1.169, adjusted OR = 1.162).
When the current day in the ED is crowded, total admission likelihood decreases by 3.5 % (95 % CI = 0.960–0.970, adjusted OR = 0.965).
All values were significant at p < 0.001.
As shown in Table 7, when history is viewed, the likelihood of single-day admissions to the ED decreases by 16.2 % (95 % CI = 0.826–0.850, adjusted OR = 0.838) adjusted to the remaining variables.
When the age of the patients increases by 1 year, the likelihood of a single-day admission decreases by 2.1 %) 95 % CI = 0.979–0.980, adjusted OR = 0.979) adjusted to the remaining variables.
When the insured patients are members of the main HMO, the likelihood of a single-day admission decreases by 6.4 % (95 % CI = 0.924–0.948, adjusted OR = 0.936) adjusted to the remaining variables.
For male patients, this likelihood increases by 5.2 % in comparison to female patients (95 % CI = 1.040–1.065, adjusted OR = 1.052).
When the current day in the ED is crowded, the likelihood for single-day admissions to the ED increases by 6.6 % (95 % CI = 1.055–1.077, adjusted OR = 1.066).
All values were significant at p < 0.001.
In order to extend the validation of these results, we tested all the regressions on many subsets of all various ED units, all hospitals and all HMOs. The findings were very similar for almost every subset (data not shown). We also tested these regressions on a smaller random sample within our whole population. Very similar results were found in this random sample as well.
Summary of the main findings
Contrary to expectations, physicians in this study used information from EMR IS on crowded days more than on non-crowded days, despite the time pressure. Viewing history may thus assist physicians in coming to more rapid decisions, which is probably much more necessary on crowded days.
Another major finding concerns the use of medical history available on the EMR IS. When patient history is viewed, the total number of admissions increases (adjusted to the remaining variables including crowdedness level) whereas the number of single-day admissions decreases. Additionally, EMR IS was consulted more for patients who were members of the main HMO health services, for whom more extensive data were collected.
Discussion and conclusion
One of the most important decisions in an ED is whether or not to admit a patient. The current literature on the usefulness of an ED EMR IS is somewhat ambiguous. On one hand, it is argued that a patient’s full data are necessary and even critical for an appropriate plan of care [9], and that crowdedness and high levels of uncertainty invite premature conclusions while ignoring invaluable evidence [12]. On the other hand, it is claimed that physicians can reach valid, reasonable conclusions regarding medical treatment despite imperfect information [14]. Extended information can also promote decision complexity [15].
Our findings suggest that viewing medical history via an EMR IS contributes to improved admission decisions. When EMR data were examined, a decision to admit was more probable. In addition, viewing medical records led to a significant reduction in the number of unnecessary single-day admissions. This finding confirms previous studies showing that such short-term admissions can be reduced using medical information [19, 21].
One possible explanation for the admission results is that the decision to admit to an ED following the use of EMR is that the medical problems tend to be more severe. However, short unnecessary admissions which are more closely related to a lack of viewing information can be prevented, in significant percentages, by using EMR IS during the evaluation time in the ED.
The second striking finding emerging from this study is the very low use of the EMR IS in the EDs. A possible explanation is that the harried environment of an ED curtails opportunities to view the medical history within the given time frame of treatment. In fact, there is no need for a medical history in many ED cases. Viewing medical history is less frequent when patients present with less serious problems, and the percentage of medical histories viewed was greater for the severe cases.
Finally, when the ED is crowded, the total number of admissions decreases and the number of single-day admissions increases. These results imply that at least some of the unnecessary admissions may have been prevented by using EMR IS in the medical decision process. However, the causal link should be researched in a further research
Interestingly, contrary to our expectations, physicians appeared to use information on crowded days more than on non-crowded days. The results show that EMR IS was used more for patients who were admitted to hospitals on crowded days at the ED, although the ED can be highly stressful at those times. Viewing medical history may thus assist the physicians in managing stressful medical scenarios.
Research contribution
In recent years, the adoption of EMR IS in the healthcare sector has increased substantially as more organizations recognize its importance and usability. In the field of healthcare, physicians need information to help them accomplish the task of providing medical services. One of the major questions in this context is how information regarding patients, as supplied by EMR IS under the serious time constraints and overcrowding of an ED can improve decision-making and its outcomes. This study attempted to answer this question and hence provides further insights into the field of medical informatics.
The main conclusions of this study allow us to better understand the importance of using EMR IS in EDs. Physicians take advantage of medical history, and are apparently aware of its importance in crowded situations. Although medical history may not always be available or relevant, our research provides insights into the common errors that may occur in ED without the existence of such data.
In this study, we dealt with the critical question of whether or not to admit a patient to the ED, which has been raised in previous research [20]. We expanded our analysis to other outcomes and showed a reduction in the volume of short-term admissions and particularly single day admissions (as compared to Cooke et al. [8] and Shabtai et al. [19]). In addition, we complement findings by Denman-Johnson et al. [21] (in which the lack of proper information lengthened hospitalization time) by exploring the important aspect of crowdedness.
We analyzed a unique and vast DB with a single EMR IS. This study has its advantages since our sample population of patients consisted of all the relevant population sectors, rather than smaller samples as found in other studies.
We investigated the advantages of EMR in the most critical decision in the ED, whether to admit or discharge the patient. Other studies have discussed the implementation of technology in EDs such as the MET system for the triage of patients [30]. This research contributes by focusing on the entire sequence of steps comprising the process of providing medical care in the ED (not only the triage), and by using an integrative EMR IS from decentralized medical suppliers.
We showed that physicians retrieve only a certain amount of information via the system during referrals in the EDs. This finding is consistent with a study that showed that physicians retrieve limited information even without any time constraints [31]. We extended this conclusion to a time pressured environment and found that medical information is used to a greater extent in more severe cases and on more crowded days.
There are also some practical implications. According to Wyatt & Spiegelhalter [32], evaluating the contribution of medical IS can provide feedback to the system developers. Our findings can promote EMR IS usage, and thus prove to physicians that these systems can improve the service and care given to patients.
Limitations and future research
The main limitation is that different hospitals have different policies regarding the use of the system. In addition, in different hospitals, there are different admission mechanisms. Thus, the nature of the hospital (type of management, different policy makers, admission policy, vacant beds, users, the deployment of the EMR IS, etc.) has a far-reaching impact on the hospital’s ability to fulfill its potential and utilize a new IS to the maximum. Another limitation is that we could not control the oral information or the hard copy information delivered by patients in the ED.
Many other research avenues could be explored in the future. For instance, the sample could be split into different time shifts (for the medical staff). There are several different shifts in the ED during the day. The hours and the number of the shifts constantly vary across hospitals and between different clinic professionals. In addition, analyzing specific medical scenarios is a powerful tool that could be used to assess end-users’ perceptions and information needs and provide a solid way of explaining workflow features, challenges and solutions related to the specifics of the ED, specifically in the public health context [33]. In particular, the findings together with future research directions could be used by developers and designers of EMR IS to design more user-friendly initial entry screen (minimal dataset) to fit the specific clinical case requirements, and environmental variables in the ED unit and patient attributes.
Notes
We chose the average as the threshold value for determining the crowdedness level over other alternative threshold candidates such as the median (consistent with other studies mentioned above). However, we tested the same regressions with a median threshold and found very similar results. We also tested several of other levels above the average (such as one and two standard deviations) and obtained very similar results.
References
Spaite, D. W., Bartholomeaux, F., Guisto, J., Lindberg, E., Hull, B., Eyherabide, A., Lanyon, S., Criss, E. A., Valenzuela, T. D., Conroy, C., Rapid process redesign in a university-based emergency department: decreasing waiting time intervals and improving patient satisfaction. Annals of emergency medicine 39:168–177, 2002.
Schneider, S., Zwemer, F., Doniger, A., Dick, R., Czapranski, T., Davis, E., A decade of emergency department overcrowding. Academic Emergency Medicine 8:1044–1050, 2001.
McCabe, J. B., Emergency department overcrowding: a national crisis. Academic Medicine 76:672–674, 2001.
Bair, A., Song, W., Chen, Y. C., Morris, B., The impact of inpatient boarding on ED efficiency: A discrete-event simulation study. Journal of Medical Systems 34:919–929, 2010.
Hwang, U., Concato, J. Care in the emergency department: how crowded is overcrowded?. Academic Emergency Medicine 11:1097–1101, 2004.
Gillies, A. C., Howard, J., Information as change agent or barrier in health care reform?. International Journal of Healthcare Information Systems and Informatics 6:19–35, 2011.
Leu, J. D., Huang, Y. T., An application of business process method to the clinical efficiency of hospital. Journal of Medical Systems 35:409–421, 2011.
Cooke, M. W., Higgins, J., Kidd, P., Use of emergency observation and assessment wards: a systematic literature review. British Medical Journal 20:138, 2003.
Hripcsak, G., Sengupta, S., Wilcox, A., Green, R., Emergency department access to a longitudinal medical record. Journal of the American Medical Association 14:235–238, 2007.
Walker, J., Pan, E., Johnston, D., Milstein, J. D., Bates, W. D., Middleton, B., The value of health care information exchange and interoperability. Health Affairs 24:10–18, 2005.
Goldman, D., Crum, D., Bromberg, R., Rogovik, A., Langer, J., Analgesia administration for acute abdominal pain in the pediatric emergency department. Pediatric Emergency Care 22:18–21, 2006.
Patel, V. L., Cohen, T., Murarka, T., Olsen, J., Kagita, S., Myneni, S., Buchman, T., Ghaemmaghami, Recovery at the edge of error: Debunking the myth of the infallible expert. Journal of Biomedical Informatics 44:413–424, 2011.
Junankar, P., Mital, D., Haque, S., Srinivasan, S., A clinical decision support system for managing flexor tendon injuries. International Journal of Medical Engineering and Informatics 1:275–289, 2009.
Sox, C., Blatt, A., Higgins, C., Medical decision making. Philadelphia: American College of Physicians, 2007.
Redelmeier, A., Shafir, E., Medical decision making in situations that offer multiple alternatives. JAMA 273:302–305, 1995.
Frisse, M. E., Holmes, R. L., Estimated financial savings associated with health information exchange and ambulatory care referral. Journal of Biomedical Informatics 40:S27–S32, 2007.
Connelly, D. P., Park, Y. T., Du, J., Ampornpunt, N. T., Gordon, B. D., Bershow, B. A., Gensinger, R. A., Shrift, M., Routhe, D. T., Speedie, S. M. The impact of electronic health records on care of heart failure patients in the emergency room. Journal of the American Medical Association, doi:10.1136/amiajnl-2011-000271, 2011.
Hoeksema, L. J., Bazzy-Asaad, A., Lomotan, E. A., Edmonds, D. E., Ramírez-Garnica, G., Shiffman, R. N., Horwitz, L. I., Accuracy of a computerized clinical decision-support system for asthma assessment and management. Journal of the American Medical Association 18:243–250, 2011.
Shabtai, I., Leshno, M., Blondheimc, O., Kornbluth, J., The value of Information for Decision-Making in the Healthcare Environment. Medical and Care Compunetics 4:91–97, 2007.
Richardson, D., No relationship between emergency department activity and triage categorization. Academic Emergency Medicine 5:141–145, 1998.
Denman, J. M., Bingham, P., George, S., A confidential enquiry into emergency hospital admissions on the Isle of Wight, UK. British Medical Journal 51:386–390, 1997.
Vest, J. R., Health information exchange and healthcare utilization. Journal of Medical Systems 33:223–231, 2009.
Kleinbaum, D. G., Klein, M., Pryor, E. R., Logistic regression: A self-learning text, Springer New York, Second Edition, 2002.
Cabrera, A. F., Logistic regression analysis in higher education: An applied perspective. Higher education: Handbook of theory and research 10:225–256, 1994.
Kooperberg, C., Petitti, D. B., Using logistic regression to estimate the adjusted attributable risk of low birth weight in an unmatched case–control study. Epidemiology 2:363–366, 1991.
Liao, D., Arnett, D. K., Tyroler, H. A., Riley, W. A., Chambless, L. E., Szklo, M., Heiss, G., Arterial stiffness and the development of hypertension. The ARIC study, American Heart Association 34:201–206, 1999.
Ford, E. S., Does exercise reduce inflammation? Physical activity and C-reactive protein among US adults. Epidemiology 13:561–568, 2002.
Baker, D. W., Parker, R. M., Williams, M. V., Clark, W. S., Health literacy and the risk of hospital admission. Journal of General Internal Medicine 13:791–798, 1998.
Fonarow, G. C., Adams, K. F., Abraham, W. T., Yancy, C. W., Boscardin, W. J., Risk stratification for in-hospital mortality in acutely decompensated heart failure classification and regression tree analysis. Journal of the American Medical Association 293:572–580, 2005.
Michalowski, W., Kersten, M., Wilk, S., Slowinski, R., Designing man–machine interactions for mobile clinical systems: MET triage support using Palm handhelds. European Journal of Operational research 177:1409–1417, 2007.
Hersh, R., Hickam, H., How Well Do Physicians Use Electronic Information Retrieval Systems? A Framework for Investigation and Systematic Review. Journal of the American Medical Association 280:1347–1352, 1998.
Wyatt, J., Spiegelhalter, D., Evaluating medical expert systems: what to test and how?. Informatics for Health and Social Care 15:205–217, 1990.
Reeder, B., Demiris, G., Building the PHARAOH framework using scenario based design: a set of pandemic decision-making scenarios for continuity of operations in a large municipal public health agency. Journal of Medical Systems 34:735–739, 2010.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ben-Assuli, O., Leshno, M. & Shabtai, I. Using Electronic Medical Record Systems for Admission Decisions in Emergency Departments: Examining the Crowdedness Effect. J Med Syst 36, 3795–3803 (2012). https://doi.org/10.1007/s10916-012-9852-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10916-012-9852-0