Abstract
As their populations age, many countries are facing the increasing economic pressure of providing healthcare to their people. In Taiwan, this problem is exacerbated by an increasing rate of obesity and obesity-related conditions. Encouraging the adoption of personal health management services is one way to maintain current levels of personal health and to efficiently manage the distribution of healthcare resources. This study introduces Mobile Health Management Services (MHMS) and employs the Technology Acceptance Model (TAM) to explore the intention of students in Executive Master of Business Management programs to adopt mobile health management technology. Partial least squares (PLS) was used to analyze the collected data, and the results revealed that “perceived usefulness” and “attitude” significantly affected the behavioral intention of adopting MHMS. Both “perceived ease of use” and “perceived usefulness,” significantly affected “attitude,” and “perceived ease of use” significantly affected “perceived usefulness” as well. The results also show that the determinants of intention toward MHMS differed with age; young adults had higher intention to adopt MHMS to manage their personal health. Therefore, relevant governmental agencies may profitably promote the management of personal health among this population. Successful promotion of personal health management will contribute to increases in both the level of general health and the efficient management of healthcare resources.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In Taiwan, the childbirth rate has dropped to 1.03% (every woman has only 1.03 children), and Taiwan will reach zero population growth in 2017 [1]. The population is also threatened by increasing rates of obesity and obesity-related illnesses. A recent national survey discovered that over 17% of adults in Taiwan are overweight or obese, and half of Taiwan’s top 10 causes of death are related to obesity. Moreover, an estimated one-third of the 2020 national health insurance budget will be spent on treatments related to obesity [2]. Therefore, the public healthcare system is being taxed by the increasing needs of both the elderly and young and middle-aged adults with chronic illnesses.
It is the popular belief that healthcare services are provided only to the ill and aging. In fact, healthcare services also have the task of promoting both good health habits and preventive medicine. “The preservation of mental and physical health by preventing or treating illness through services offered by the health service providers” is a broad definition of healthcare service. Individual health management is a habit, an attitude, and a requirement for daily life [3]. If people form good health management habits, the incidence of disease will decrease.
Denberg et al. [4] pointed out that physician feedback about preventive care and patient and physician reminders have resulted in mixed or modest improvements. Not only are many patients not current on recommended preventive services [5], preventive medicine is often overlooked during clinic visits [6]. Health management is part and parcel of preventive medicine; it helps healthy people stay healthy and aids chronic patients during their convalescence. To encourage people to engage in health management activities is an important task for national health programs as good health management decreases the need for healthcare services.
While nursing and medicine are considered direct-care professions, health systems management is described as the “hidden” health profession [7]. E-health and telemedicine have developed over a number of years. Mobile health (m-health) was introduced as “unwired e-med” in wireless telemedicine systems [8], and can be defined as “mobile computing, medical sensor, and communications technologies for health care” [9]. Mobile computing and wireless technologies benefit healthcare by enabling mobile hand-held or wearable devices that can help patients obtain central healthcare service quickly [10], and may have the potential to deliver healthcare services 24/7. Well-designed e-health and m-health systems act as indirect-care “professionals” caring for their patients and have become integral components of modern healthcare systems.
Mobile healthcare devices currently in use include real-time health monitoring systems [11], decision support systems [12], RFID-based services [13], and weight control services [2]. Although many studies have discussed mobile healthcare issues, few have focused on issues in mobile healthcare management [14, 15]. Moreover, subjects of mobile healthcare studies are often medical professionals [16, 17]; few studies have focused on the general user’s motives [18, 19]. The present study examines the determinants of adopting mobile health management technology among young and middle-aged adults and explores whether determinants of intention toward MHMS vary with age within this group.
In the following pages, MHMS is defined, and the theoretical background and research model are introduced. Next, the material and methods of the study are briefly delineated. Finally, the results of the study are presented and discussed.
Mobile Health Management Service (MHMS)
The lack of sufficient healthcare resources is creating increased pressure on government agencies, healthcare providers, and families; innovation and advancement in MHMS could alleviate that pressure significantly. Continued improvement in MHMS and the concomitant increase in MHMS use would make the saying, “prevention is better than cure” a reality as young and middle-aged people begin to use MHMS to manage their good health.
MHMS refers to the ability of the mobile health management systems to support medical care or healthcare and health promoting self-care. A mobile healthcare management system must be able to capture complete and accurate information of a patient’s medical history and current medical conditions [15]. As Fig. 1 shows, mobile health management services are designed for use during two distinct periods, the Healthy Period and the Convalescent period. During the Healthy Period, “health promotion” and “self-care” are the primary MHMS services. The “health promotion” movement originated in Canada in 1974 [20] with the goal of improving Canadians’ general health and decreasing healthcare costs. Mobile health management contributes to health promotion by providing health education, access to health records, and other services to physicians and patients through their cell phones. “Self-care” has been defined as the processes of personal health maintenance, e.g., the intention of improving/restoring health or treating/preventing diseases [21]. Mobile health management systems increase self-care program effectiveness by using cell phones to provide encouragement and timely health reminders (e.g. to take medications or to exercise) to participating patients [2].
During the “Convalescent Period”, “medical care” and “healthcare” are the primary MHMS services provided patients currently under a physician’s care. All services, such as outpatient services and RFID tagging in emergency rooms, are provided by hospitals. During this period, personal health management records integrate with “telemedicine systems” by which physicians may access patient records and patient status information. Upon recovery, the individual patient’s healthcare information will integrate with his/her personal “mobile healthcare management” services.
Individual lifestyles, both at work and in personal life, influence health. Personal health impacts not only individuals, but families and societies, as well. Also, as Zwetsloot and Pot [22] pointed out, health management has a strategic and economic impact on business. Healthy people participating in health-promoting self-care activities define a successful a preventive medicine program, and the more participants there are in such programs, the fewer healthcare resources are required. A paradigm shift from traditional illness treatment toward active and progressive health management is a change that service providers and service consumers can both look forward to.
Theoretical foundations
Theoretical models that have been used to explain human behavior in the process of adoption include Diffusion of Innovations Theory (DIT) [23], Theory of Reasoned Action (TRA) [24], Theory of Planned Behavior (TPB) [24], and Technology Acceptance Model (TAM) [25, 26]. Theory of Reasoned Action regards behavior as a direct function of behavioral intention and indentifies the antecedents of behavioral intention as attitude and subjective norms. Theory of Planned Behavior adds perceived behavioral control to TRA’s attitude and subjective norms as another antecedent of behavioral intention [24]. Diffusion of Innovations Theory focuses on the rate of adoption, which is the relative speed with which innovative technology is adopted by the members of a social system [23].
In the m-healthcare context, Chau and Hu [27] found that TAM is a more suitable model than TRA and more appropriate than TPB for examining technology adoption. Furthermore, TAM has been evidenced and supported by many studies and widely used for explanation of the determinants of innovative technologies in tele-healthcare context [28]. Rahimpour et al. [28] used focus group interviews to draw out the tele-healthcare themes and classify them into four major themes and 16 sub-themes identified from the participants’ comments. Those four major themes are “intention to use the Home Telecare Management System (HTMS),” “the impact on patients’ health management,” “concerns associated with using the HTMS,” and “the impact on health care services.” The study further identified the sub-themes of “intention to use HTMS” as -self-efficacy, users’ anxiety, and TAM based variables. It was noted that the easy use of HTMS may reduce the users’ anxiety and strengthen users’ confidence regarding their self-efficacy [28]. Hence, this study considers that the TAM model is suited to the investigation of MHMS issues.
In e-healthcare and m-healthcare research, TAM is the preferred attitude-behavior model. Davis [25] and Davis et al. [26] developed TAM to predict and explain personal acceptance of computer technology. The TAM is composed of five constructs, “perceived usefulness,” “perceived ease of use,” “attitude,” “behavioral intention to use,” and “actual system use.” In TAM, “perceived usefulness” and “perceived ease of use” are the most dominant determinants of a user’s “attitude,” and “perceived usefulness” has a direct effect on a user’s behavioral intention to use the technology. Previous studies [29, 30] have suggested removing “attitude” from this model. The studies argued that attitude didn’t appear to fully mediate the effect of either perceived ease of use or perceived usefulness on behavioral intention. Because of this perceived weakness, a revised TAM (without the attitude construct) was devised and empirically tested. It was found that behavioral intention to use was determined jointly by “perceived usefulness” and “perceived ease of use.” Wu, et al. [16] subsequently adopted the revised TAM to measure medical professionals’ intention to use a mobile healthcare system.
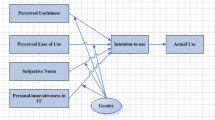
When healthcare organizations decide to implement mobile healthcare systems, their medical professionals are merely asked to adopt the technology. In such cases it is perhaps reasonable not to be overly concerned with these professionals’ attitudes toward employing the new technology. However, users of Mobile Health Management Systems adopt the system voluntarily, and their attitudes are important. Thus, the original TAM, which includes the “attitude” construct, may be more appropriate for measuring MHMS intention. There are two reasons why this might be the case: First MHMS users decide for themselves whether to use the technology, and this decision reflects their attitude toward the technology, which is influenced by “usefulness” and “ease of use” as the original TAM suggested [25, 26]. As Rahimpour et al. [28] pointed out, ease of use was one critical factor related to the use of the home telecare management system. Second, in related e-heath literature, “attitude” facilitated the intended conceptual response of studies [27, 31], all of which retained the “attitude” construct in their administration of the TAM. In order to explore the determinants of adopting MHMS based on TAM, an original TAM was administered in the current study, as depicted in Fig. 2.
This research model posits that the level of user intention to use MHMS can be explained by both the user’s perception about MHMS usefulness and his/her attitude toward MHMS use. This study explores the determinants of the intention to use MHMS and examines the following hypotheses:
-
H1: Perceived ease of use has a positive effect on perceived usefulness of MHMS.
-
H2: Perceived ease of use has a positive effect on attitude toward MHMS.
-
H3: Perceived usefulness has a positive effect on attitude toward MHMS.
-
H4: Perceived usefulness has a positive effect on behavioral intention toward MHMS.
-
H5: Attitude has a positive effect on behavioral intention toward MHMS.
In the past, most mobile healthcare services focused on the elderly and on chronically ill patients. Previous healthcare management literature also often focused on the elderly; fewer studies explored the intention of adopting health management service by the young and middle-aged. Because the numbers of chronically ill in the young and middle-aged groups seems to be increasing, this study will also explore different age groups’ intentions in adopting MHMS. The study’s last hypothesis will be:
-
H6: The determinants of intention toward MHMS will vary depending on age group.
Material and methods
The study survey instrument was developed based on the TAM. The first part of the survey collects respondents’ personal information, and the second part consists of 15 items suggested by Davis [25], Davis et al. [26], and Taylor and Todd [32] to measure perceived ease of use, perceived usefulness, attitude, and behavioral intention of adopting the MHMS. The scale items used in the survey instrument were adapted from previous studies to ensure content validity. In addition, medical professionals and mobile service researchers were enlisted to assess the face validity of the instrument. After discussion, the initial survey was revised to ensure that the scale items would measure intention of adopting MHMS. The survey instrument was composed of four variables, Perceived Ease of Use (PEU), Perceived Usefulness (PU), Attitude (ATT), and Behavioral Intention toward MHMS (BI) (Table 1). Each variable was taken from previously validated instruments [25–27, 32]. Likert scales (ranging from 1 to 5), with anchors ranging from “strongly disagree” and “strongly agree” were used for all scale items. The survey items are listed in Table 2.
As they are assumed to be of higher economic standing and to have elderly family members at home, students in Executive Master of Business Administration (EMBA) programs were invited to participate in the study. One-hundred-and-eighty-five respondents were recruited from three universities in Taiwan. In this sampling, most of the “EMBA” program students were managers, and their ages were in the range of 25–65. A total of 170 valid surveys were returned, a response rate of 92%. Of the respondents, 64% were married, 54% were female, and 102 were 40 years of age or younger. Table 1 shows the respondent diversity.
The definition of “middle age” varies, being identified on different occasions as 40–60, 45–60 or 40–65 years of age. Because chronically ill patients have been getting younger, this study adopts the broader definition of middle age as “beginning after age 40.” In this study, respondents were split into two sub-groups, those 40 years of age and younger (S1), and those over 40 (S2). These two groups were used to evaluate hypothesis six, which explored the effect of age on intention to adopt technology.
Results
Partial least squares (PLS) is a powerful second-generation multivariate technique used to analyze causal models involving multiple constructs with multiple observed items [33]. In this study, two age-group samples, S1 (n = 102) and sample S2 (n = 68), were examined. Because PLS does not require a large sample size [34, 35], the technique is the most suitable for testing the hypotheses in this study.
To ensure reliability, the scores of each construct were used to calculate Cronbach’s α values. Cronbach’s α values range from zero (unreliable) to one (perfect reliability), with a value of 0.5 indicating acceptable reliability [36], 0.6 indicating acceptability for exploratory studies [37], and 0.7 indicating good reliability [36, 37]. In this study, the Cronbach’s α value for each construct was higher than 0.6, indicating its acceptability for use in this exploratory study of MHMS applications.
This study used Exploratory Factor Analysis (EFA) to verify the construct validity of the instrument. In Table 3, EFA with varimax rotation was performed to assess the underlying factor structures of the measured scales. The results of the EFA revealed that each of the measures showed sufficient construct reliability as the factor loading of each item in the instrument was above the suggested 0.5 [37].
Three criteria are commonly used to assess the convergent validity of measurement models [38]. First, it is suggested that the factor loadings of all standardized items be higher than 0.5; second, it is suggested that the composite reliability (CR) be higher than 0.6; and three, that the average variance extracted (AVE) should be higher than 0.5. An analysis of the survey instrument used in this study is shown in Table 3. All scale items in the instrument showed reasonable reliability and validity for the measurement model.
Table 4 shows the results of path analysis, with path coefficients and t-values, and Table 5 lists the explanatory powers. Tables 4 and 5 show the relative strengths of each path specified by the research model and the variance (R 2) explained by each path. The analyzed results of the 170 valid surveys indicated that ATT and PU significantly determine the adoption of MHMS, and R 2 is 57.8%. For the antecedents of ATT, both PEU and PU affected ATT, accounting for 64.5% of the variance in ATT. Additionally, PEU significantly impacted PU, accounting for 44% of the PU variance. After analysis of the 170 valid survey instruments in the two samples, H1, H2, H3, H4, and H5 were confirmed in this TAM-based research model.
Hypothesis 6 explores the determinants of intention toward MHMS that might vary depending on age. Table 4 shows the path coefficients among the research variables in both S1 and S2 samples. In the S1 (young adult) sample, only ATT significantly determines the adoption of MHMS, and R 2 is 59.5%. As for the antecedents of ATT, both PEU and PU affected ATT, accounting for 71.7% of the ATT variance. PEU also significantly impacted PU, accounting for 50.8% of the PU variance. For this group, H1, H2, H3, and H5 are supported. In the middle-aged sample (S2), ATT and PU significantly determine the adoption of MHMS (R 2 = 54.0%). For the antecedents of ATT, only PU affected ATT, accounting for 48.7% of the ATT variance. PEU also significantly impacted PU, accounting for 27.4% of the PU variance. For the middle-aged group, H1, H3, H4, and H5 are supported. Comparing the two samples, there is within each sample one path coefficient that is not significant. In other words, the determinants of intention toward adopting MHMS differ with age.
Limitations
This empirical study has its limitations. MHMS is a new issue; moreover, these research findings and implications were obtained from a single study. Hence, readers should exercise caution when generalizing the findings and implications to other mobile healthcare management service user groups.
Discussion and suggestions
Previous literature shows that TAM is the preferred model in evaluating the adoption of innovative technology. Consistent with Rahimpour et al. [28], this study found that all variable relationships of the TAM model are significant. This implies that intention to use MHMS can be well explained through the TAM model. However, the findings of this study differ from those of Chau and Hu [27], who point out that perceived usefulness was more important than perceived ease of use for their physician users. The current study found that the effects of perceived ease of use and perceived usefulness are not only different for different technology adopters, but are also different for technology adopters of different ages.
MHMS is a growing area of telemedicine research. In the past, MHMS was considered most valuable to the elderly [39] or as a support system for healthcare professionals [40]. However, as this study shows, MHMS could prove acceptable to a younger population. Utilizing TAM, the current study has identified important determinants of intention to adopt MHMS. This information will be important in the design and implementation of future mobile healthcare services. As the use of personal electronic health records expands with the advance of e-health services [40], the use of MHMS by young and middle-aged adults will contribute to efficient allocation of healthcare resources and an improvement in general health.
The present study contributes to the research literature by demonstrating that TAM is a good model for predicting and explaining the intention to adopt MHMS. In the study, the relationships between perceived ease of use, perceived usefulness, attitude, and behavioral intention to adopt MHMS were found to be positive and highly significant. The study also found that while perceived ease of use of MHMS is more important to young adults than to those at middle-age, perceived usefulness is of greater importance to the later group. These differences will inform the future direction of healthcare services policy [39] as providers focus on the needs of different groups of service consumers. By providing demonstrably useful services via a user-friendly interface, both young and middle-aged adults will be attracted to the technology.
The results of the present study will also be of interest to researchers concerned with improving healthcare management and reducing systemic resource waste [41]. As a society ages, preventive medicine becomes increasingly important. While much research in the area of preventive medicine focuses on the health maintenance behaviors of the elderly, the present study suggests that health maintenance behaviors and habits might be profitably addressed in young-adulthood and middle age. Promoting the use of MHMS among these populations might begin with government-sponsored health management activities hosted both at higher education institutions and at private companies. An increase in MHMS use will result in a concomitant improvement in general health and, in the longer run, an increasingly efficient allocation of healthcare resources.
References
China Times: Taiwan will confront zero population growth in 2017, http://tw.news.yahoo.com/article/url/d/a/100514/4/25mjv.html. (in Chinese) (Accessed date on 2011/05/14)
Jen, W. Y., Mobile healthcare services in school-based health center. Int. J. Med. Inform. 78:425–434, 2009.
Hunter, D. J., and Brown, J., A review of health management research. Eur. J. Public. Health. 17:33–37, 2007.
Denberg, T. D., Ross, S. E., and Steiner J. F., Patient acceptance of a novel preventive care delivery system. Prev. Med., 44:543–546, 2007.
Pham, H. H., Schrag, D., Hargraves, J. L., and Bach, P. B., Delivery of preventive services to older adults by primary care physicians. JAMA. 294:473–481, 2005.
Stange, K. C., Woolf, S. H., and Gjeltema, K., One minute for prevention: the power of leveraging to fulfill the promise of health behavior counseling. Am. J. Prev. Med. 22:320–323, 2002.
Haddock, C. C., McLean, R. D., Careers in healthcare management: how to find your path and follow it. Chicago: Health Administration Press, 2002.
Istepanian, R. S. H., and Laxminaryan, S., UNWIRED, the next generation of wireless and internetable telemedicine systems-editorial paper. IEEE T. Inf. Technol. B. 4:189–194, 2000.
Istepanian, R. S. H., Jovanov, E., and Zhang, Y. T., Introduction to the special section on m-health: beyond seamless mobility and global wireless health-care connectivity. IEEE T. Inf. Technol. B., 8:405–414, 2004.
Hameed, K., The application of mobile computing and technology to health care services. Telemat. Inform. 20:99–106, 2003.
Chen, H., Wu, W., and Lee, J., A WBAN-based real-time electroencephalogram monitoring system: design and implementation. J. Med. Syst. 34:303–311, 2010.
Eren, A., Subasi, A., and Coskun, O., A decision support system for telemedicine through the mobile telecommunications platform. J. Med. Syst. 32:31–35, 2008.
Chao, C. C., Jen, W. Y., Patient safety management: RFID technology to improve Emergency Room medical care quality. In T. Shih and Q. Li (Eds.), Ubiquitous Multimedia Computing (pp. 323–339). CRC Press, Taylor & Francis Company, chapter 15, 2010.
Tani, S., Marukami, T., Matsuda, A., Shindo, A., Takemoto, K., and Inada, T., Development of a health management support system for patients with diabetes mellitus at home. J. Med. Syst. 34:223–228, 2010.
Chan, A. T. S., WWW+smart card: toward a mobile health care management system. Int. J. Med. Inform. 57:127-137, 2000.
Wu, J., Wang, S., and Lin, L., Mobile computing acceptance factors in the healthcare industry: a structural equation model. Int. J. Med. Inform. 76:66–77, 2007.
Rafael, A., Wangenheim, A., and Bortoluzzi, M., Wireless and PDA: a novel strategy to access DICOM-compliant medical data on mobile devices. Int. J. Med. Inform. 71:157–163, 2003.
Jen, W. Y., and Hung, M. C., An empirical study of adopting mobile healthcare service: The family’s perspective on the healthcare needs of their elderly members. Telemed. e-Health. 16:1–8, 2010.
Lorenz, A., Oppermann, R., Mobile health monitoring for the elderly: designing for diversity. Perv. Mobil. Comp. 5:478–495, 2009.
Lalonde, M., A new perspective on the health of Canadians. Ottawa: Health and Welfare Canada, 1974.
Levin, L. S., Katz, A. H., and Holst, E., Self care: lay initiatives in health. London: Croom Helm, 1977.
Zwetsloot, G., and Pot, F., The business value of health management. J. Bus. Ethics. 55:115–124, 2004.
Rogers, E. M., Diffusion of innovations. New York: Free Press, 2003.
Ajzen, I., From intention to action: A theory of planned behavior. In J. Kuhl & J. Beckmann (Eds.), Action control: From cognition to behavior. New York: Springer, 1985.
Davis, F. D., Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 13: 318–339, 1989.
Davis, F. D., Bagozzi, R. P., and Warshaw, P. R., User acceptance of computer technology: a comparison of two theoretical models. Manage. Sci. 35:982–1003, 1989.
Chau, P. Y. K., and Hu, P. J. H., Investigating healthcare professionals’ decisions to accept telemedicine technology: an empirical test of competing theories. Inf. Manage. 39:297–311, 2002.
Rahimpour, M., Lovell, N. H., Celler, B. G., and McCormick, J., Patients’ perceptions of a home telecare system. Int. J. Med. Inform. 77: 486–498, 2008.
Venkatesh, V., Determinants of perceived ease of use: integrating control, intrinsic motivation, and emotion into the technology acceptance model. Inform. Syst. Res. 11: 342–365, 2000.
Venkatesh, V., and Davis, F. D., A theoretical extension of the technology acceptance model: four longitudinal field studies. Manage. Sci. 46:186–204, 2000.
Chen, I. J., Yang K. F., Tang F. I., Huang C. H., and Yu S., Applying the technology acceptance model to explore public health nurses’ intentions toward web-based learning: A cross-sectional questionnaire survey. Int. J. Nurs. Stud. 45:869–878, 2008.
Taylor, S., and Todd, P. A., Understanding information technology usage: a test of competing models. Inform. Syst. Res. 6:144–176, 1995.
Fornell, C. A., Second generation of multivariate analysis. Methods: Vol. 1. New York: Praeger, 1982.
Yoo, Y., Alavi., M., Media and group cohesion: relative influences on social presence, task participation, and group consensus. MIS Quart. 25:371–390, 2001.
Fornell, C., Bookstein, F., Two structural equation models: LISREL and PLS Applied to Consumer Exit-Voice Theory. J. Mark. Rese. 19:440–452, 1982.
Jőreskog, K. G, and Sőrbom D., LISREL 8: users’ reference guide. Chicago, IL: Scientific Software International, 1993.
Hair, J. F., Anderson, R. E., Tatham, R. L., and Black, W. C., Multivariate data analysis. Prentice Hall, NJ, 1998.
Fornell, C., and Larcker D. F., Evaluating structural equation models with unobservables and measurement error. J. Market. Res. 18:39–50, 1981.
Farmer, J., Philip, L., King, G., Farrington, J., MacLeod, M., Territorial tensions: Misaligned management and community perspectives on health services for older people in remote rural areas. Heal. and Plac. 16:275–283, 2010.
Chronaki, C. E., Lelis, P., Chiarugi, F., Trypakis, D., Moumouris, K., Stavrakis, H., Kavlentakis, G., Stathiakis, N., Tsiknakis, M., and Orphanoudakis, S. C., An open eHealth platform for health management using adaptable service profiles. Intl. Cong. Seri. 1268: 295–300, 2004.
Tudor, T. L., Marsh, C. L., Butler, S., Van Horn, J. A., and Jenkin, L. E. T., Realising resource efficiency in the management of healthcare waste from the Cornwall National Health Service (NHS) in the UK. Waste. Manage. 28: 1209–1218, 2008.
Acknowledgements
The authors would like to thank Dr. Ralph Grams, M.D. and the anonymous reviewers for their insightful suggestions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hung, MC., Jen, WY. The Adoption of Mobile Health Management Services: An Empirical Study. J Med Syst 36, 1381–1388 (2012). https://doi.org/10.1007/s10916-010-9600-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10916-010-9600-2