Abstract
Breast milk is a multifunctional biofluid that provides nutrients along with highly diverse non-nutritive bioactive components such as antibodies, glycans, bacteria, and immunomodulatory proteins. Research over the past decade has confirmed the essential role of breast milk bioactives in the establishment a healthy intestinal microbiota within the infant. The intestinal microbiota of an exclusively breastfed baby is dominated by several species of Bifidobacteria - the most influential member of which is Bifidobacterium longum subspecies infantis (B. infantis) - and is referred to as the milk-oriented microbiome (MOM). MOM is associated with reduced risk of infection in infancy as well as a reduced risk of certain chronic illnesses in adulthood. Establishment and persistence of MOM is dependent on the selective digestion of complex sugar structures in breast milk that are otherwise indigestible to the infant by B. infantis and its relatives. This review focuses primarily on the influence of breast milk glycans and glycosylated proteins on the development of the intestinal microbiome, and how maternal phenotype may influence the development of MOM providing a framework to understand how variation in diet shapes a protective intestinal microbiome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A high antigenic load coupled with a naïve system defines immunity in the neonatal period. The importance of the gut microbiota in the development and activation of the immune system is well established. Lactation drives a milk-oriented microbiota (MOM) that is characterized by the simultaneous promotion of protective bacteria and suppression of pathogenic bacteria [1]. The development of the microbiota is dictated by complex interactions between the mother, the infant, and their environment (Fig. 1). At birth, the intestinal microbiota is extremely variable, and undergoes several transitions before stabilizing during the first few years of life [2, 3]. The initial environment-derived microbial community is succeeded by microbes that are capable of exploiting and colonizing various niches within the intestine and these niches are largely driven by diet [4]. The exclusive breast feeding period constitutes a rare opportunity to manipulate gut microbiota in favor of health. The components of human milk uniquely support the development of specific microbiota with particular functions and health effects. Lactation protects the infant by delivering bioactive molecules such as growth factors, proteins, antibodies, bacteria, and glycans, which collectively help select the composition and function of the intestinal microbiota [5].
The mother infant-dyad is a complex system with a variety of inputs and outputs that can affect infant health outcomes. Both genotype and phenotype of the mother influences the composition and potentially the function of the breast milk that is ingested by the infant. How that infant is able to use the various components of the breast milk for both nutritive and non-nutritive functions will affect the health status of the infant. Health is a spectrum with green representing good health and red representing poor health and/or disease
The overall importance of the intestinal microbiota for host physiology and metabolism is well-documented in the scientific literature [6–9]. The intestinal microbiome (the full complement of bacterial genes that are active in the intestinal microbiota) plays an important role in nutrient availability and the absorption of dietary components [10–12] as well as immune function [13–15]. For example, early research with gnotobiotic mice demonstrated the immune and metabolic consequences of a sterile gut such as hypoplastic Peyer’s patches, poorly formed lymph nodes, and abnormal quantities of immune cells [16, 17]. Subsequent investigations involving inoculation of germ-free mice with fecal microbes obtained from conventionally raised animals confirmed many of the functional implications of the microbiota at large [6, 8, 18]. Although we know that the intestinal microbiome is essential and key to human health, relatively little is known about what constitutes a “healthy” microbiome and the mechanisms that underlie development.
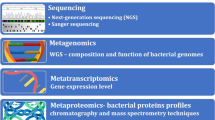
Increased rates of Cesarean section, exposure to antibiotics, and the increased use of disinfectants in the environments coupled with variable early feeding practices (breast feeding, formula, mixed feeding and complementary feeding) over the last few decades have changed the environment surrounding the newborn infant and are jeopardizing the evolutionarily established MOM. The long-term effects of not achieving MOM in the first 3–4 months of life before complementary feeding is started are underappreciated and understudied. The increased rates of obesity, inflammation-associated diseases such as irritable bowel syndrome and Crohn’s disease, and allergies may be attributed to factors that disrupt the development of MOM [19–21]. However, mechanistic studies are lacking and key questions about the early introduction infant formula and/or solid foods that lead to a more diverse adult-like microbiota in early infancy remain unanswered [4]. High-throughput ‘omic’ technologies are providing an unprecedented opportunity to define the inputs and outputs of the mother-infant dyad, which researchers can use to better understand the impact of diet on health outcomes. To achieve this comprehensive view of lactation and the intestinal microbiome, we must understand the maternal factors that influence milk composition and function, and how these factors, in turn, impact MOM and infant health. This review focuses primarily on the influence of breast milk glycans and glycosylated proteins on the development of the intestinal microbiome, and how maternal genotype and phenotype may influence the development of MOMproviding a framework to understand how variation in diet shapes the intestinal microbiome.
What is the Milk-Oriented Microbiota and Why is it Important?
Exclusive breast feeding fosters a Bifidobacteria-dominated microbiota that is distinct from those resulting from other infant feeding strategies, and which accounts for a substantial proportion of the benefits ascribed to breast feeding [22]. Bifidobacteria can account for 70–80 % of the total bacteria in feces from breast fed babies. B. longum and B. breve are the most frequently observed species in the breast-fed infant intestine; B. bifidum, B. pseudocatenulatum, and B. catenulatum may also be found [22]. Studies focusing on the genomes of Bifidobacteria suggest that specific species have co-evolved with human lactation [12–16]. Several gene clusters have been identified that are responsive to human milk and confer the ability to sequester and breakdown specific linkages in complex sugar structures that are indigestible to the infant, but are an important food source for these bacteria [23]. Early studies demonstrated that one such microbe is B. longum subspecies infantis (B. infantis) outcompetes other Bifidobacteria strains when allowed to grow in cultures where milk glycans are the sole carbon sourse [24–26]. Sequencing this subspecies uncovered a collection of genes involved in the catabolism of complex carbohydrates, including a 43-kb gene cluster encoding a variety of glycosyl hydrolases as well as transport proteins that were not found in closely-related species [27, 28]. In addition, B. infantis is the only known Bifidobacteria strain capable of digesting every type of prebiotic glycan (i.e., neutral, fucosylated, and sialylated) present in human milk [29]. Differences such as these help explain why B. infantis is capable of out-competing other colonic bacteria when given a steady supply of milk glycans.
Evidence suggests that B. infantis provides for a substantial portion of the benefits normally ascribed to breast feeding [22]. The relative abundance of B. infantis measured from the stool of infants 15 weeks of age was found to correlate with their vaccination responses to 4 vaccines: oral polio virus (OPV), bacille Calmette-Guérin (BCG), tetanus toxoid (TT), and hepatitis B virus (HBV). Vaccination responses were measured by vaccine specific T-cell proliferation and skin tests or vaccine specific immunoglobulin G levels for each of the vaccines. Positive correlations were observed between abundance of fecal B. infantis and CD4 stimulation responses to OPV, PPD, and TT. Furthermore, fecal B. infantis was positively associated with thymus index which was independent of length-for-age, a typical marker of nutrition status [30]. While the aforementioned correlation does not guarantee causation, it does support the notion that the composition of the infant microbiota is a crucial factor for immune system development. More evidence supporting this hypothesis is the fact that probiotics containing B. infantis decreased the relative risk of developing necrotizing enterocolitis (NEC) in premature infants [31]. In fact, five of six published randomized clinical trials of B. infantis alone or in combination when administered to premature infants showed decreased incidence of NEC compared to control [32–37]. In contrast, administration of B. lactis to premature infants did not affect the incidence of NEC [38].
The Early Microbial Environment: From Birth to MOM
Two key questions regarding the role of high levels of B infantis in MOM remain unanswered: 1) where does the B. infantis inoculum come from; and 2) how do Bifidobacteria interact with other bacteria in a background of a strictly human milk diet? There is some evidence to suggest that the early colonizers prepare the infant intestine by reducing the pH of the environment to make way for strict anaerobes like Bifidobacteria spp. [29]. Therefore, it is imperative that we begin to focus research on the mechanisms by which the perinatal environment influences the development of the infant’s intestinal microbiome.
Babies acquire bacteria from their environment so initial seeding of their intestine is strongly influenced by gestational age (pre-term vs. term) [39–42], mode of delivery (vaginal vs. Cesarean section) [43] and, potentially, delivery environment (hospital vs. hospital; hospital vs. home) [40, 44]. Vaginally delivered infants acquire bacterial communities resembling their mother’s vaginal microbiota, which is dominated by Lactobacillus, Prevotella, or Sneathia spp., while infants born by Cesarean section harbor bacterial communities similar to those found on the skin surface, predominantly composed of Staphylococcus, Corynebacterium, and Propionibacterium spp. [43]. Additionally, vaginal delivery invariably leads to contact with maternal fecal matter, thereby exposing the infant to maternal gut bacteria [45]. However, maternal fecal transfer of anaerobic bacteria to the infant is not well understood. In a study comparing the prevalence of ten key species of Bifidobacteria, babies born by Cesarean section did not have Bifidobacteria, while the guts of vaginally delivered neonates were dominated by Bifidobacteria spp. such as B. longum and B. catenulatum [46]. Premature infant microbiomes are less diverse than full term infants, possibly due to the hospital environment, high rate of C-section and routine use of antibiotics [47, 48]. As a result, premature infants follow a specific gut microbial trajectory that is characterized by abrupt and unpredictable changes in microbial composition [49]. Birth introduces a number of different organisms to the infant as a bolus, and is a distinct, trackable event in the history of that baby providing a piece of the puzzle of how we acquire microbial communities.
Consuming breast milk provides a small, but continuous source, of viable bacteria (103colony forming units/mL) as measured in aseptically collected milk [50–53]. With this in mind one could postulate that milk delivers specific organisms to preferentially seed the infant intestine. Martin et al. (2003) suggested that breast milk was a source of endogenous lactic acid bacteria not resulting from skin contamination [54]. The hypothesis that breast milk is in part responsible for seeding the infant gut further emphasizes the need to understand the mother’s health status as it relates to both the exogenous and endogenous microbial environments. One example of a known perturbation to milk microbiota occurs with infectious mastitis. Staphylococcus epidermidis is the major microorganism present in breast milk collected from mothers suffering with mastitis [55]. The fate of these organisms and their ability to interfere with the development of a healthy infant microbiota requires additional research particularly since it was also demonstrated that the strains of staphylococcus isolated from mothers with mastitis were antibiotic resistant compared to strains isolated from healthy mothers [56]. The dynamic nature of the mother-infant pair requires careful monitoring and interpretation of the data to fully understand the relationship between maternal intestine, mammary gland and the infant intestinal microbiome.
Cabrera-Rubio et al. (2012) discovered lactic acid bacteria from the order Lactobacillales and genera Staphylococcus were dominant in both colostrum, and mature milk (mature milk samples at 1 and 6 months postpartum). In another prospective study, Hunt et al. 2011 [57] discovered that nine core bacterial genera (Staphylococcus, Streptococcus, Serratia, Pseudomonas, Corynebacterium, Ralstonia, Propionibacterium, Sphingomonas, and Bradyrhizobiaceae) represented approximately 50 % of total bacteria in breast milk. The most abundant genera found (Streptococcus and Staphylococcus) were also discovered in the oral cavity; skin and breast tissue, respectively [43, 58]. There are several culture-based studies that have isolated obligate anaerobes from breast milk typical of the lower gastrointestinal tract such as Bacteroides, Clostridia, Bifidobacterium, Veillonella [51, 53, 59]. Using PCR denaturing gradient gel electrophoresis, Martin et al. (2009), identified Bifidobacteria spp. across the majority of early milk samples from 23 mothers. However, this genera was only a minor member of the milk microbiota, averaging 2.8 % of total bacterial abundance and ranging from 0 to 16 % across samples [51]. Using both culture-independent and dependent methods, Jost et al. (2013) identified that the highest potential for vertical mother–infant transfer via breast milk was observed for the genus Bifidobacterium which was consistently detected in all samples at mean relative abundances of 8.4, 1.3 and 51.8 % in maternal feces, breast milk, and infant feces, respectively. However, the presence of identical isolates must be confirmed on the subspecies or strain level within mother–infant pairs to support the hypothesis of vertical transfer via breast milk. Only the strain B. breve was shared within one mother–infant dyad, therefore no conclusions can be made about whether this transfer is a common event during lactation. Similarly with vaginal microbial environment, the dominance of lactic acid bacteria in breast milk may function to maintain an acidic environment in the intestine that supports the growth of obligate anaerobes.
There are a number of explanations for the origin of milk microbes; for example, it is reasonable to suggest a proportion arise from skin on and around the nipple [60] or through handling breast pump supplies [61]. Another possibility is the transfer of bacteria from the infant oral cavity to the milk ducts, likely reaching steady state equilibrium between the infant and its mother [62]. This is consistent with the fact that retrograde flow back into the mammary ducts can occur during suckling, and the frequent appearance of typical inhabitants of the oral cavity such as Streptococcus, Veillonella, Leptotrichia, and Prevotella in breast milk [63]. However, the breastmilk microbiota species that have been identified to date include not only skin and oral sources, but also contain organisms typically associated with the intestine. Perez and colleagues (2007) proposed that mothers transfer their intestinal microbiota via an enteromammary pathway mediated by her immune system. The authors discovered that aseptically collected milk contained viable bacteria in human mothers. Maternal peripheral blood mononuclear cells and milk cells contained intact bacterial structures. Furthermore, these cells contained ribosomal DNA of a greater biodiversity reflective of enteric bacteria (Perez 2007). However, only some of the bacterial signatures were common to fecal samples of maternal origin and their matched infants. B. longum was identified as common between mother feces, mother’s blood cells and infant feces. It is important to emphasize that only DNA signatures and not viable bacteria were analyzed in these samples. In a second study, it was demonstrated that pregnant and lactating mice had increased bacterial translocation compared to control mice. More research is needed to validate this mechanism of vertical transfer of bacteria from mother to infant.
A conclusive understanding of the origin and importance of microbes in breast milk remains unknown and how their consumption leads to changes in the infant intestinal microbiome. The above studies still represent small sample sizes. There is a need for greater standardization of methods and the creation of large curated databases to understand the composition as well as the contribution of the milk microbiome on infant development. Above methodological issues, differences could also be attributed to the high inter-individual variation for milk microbiota among women. For example, the bacterial communities of breast milk from women who were obese or women who delivered by elective Cesarean section were different from normal weight women or women who delivered by emergent Cesarean or vaginal delivery, respectively [63]. Understanding the composition of, and the role(s) such communities play in maintaining mammary gland health, bacterial colonization of the infant’s gastrointestinal tract, and on short- and long-term indices of maternal and infant health are needed.
Understanding the Impact of Human Milk on the Infant Intestine
Overall, the composition and development of infant gut microbiota are influenced by body mass index, weight, and maternal gestational weight gain. For example, greater maternal weights and BMIs were correlated with higher concentrations of Bacteroides, Clostridium, and Staphylococcus spp. along with lower concentrations of the Bifidobacterium in their infants [64]. Furthermore, infants with older siblings have been found to have slightly higher numbers of Bifidobacteria, compared with infants without siblings [4]. Molecular nutrition and technological advances have provided scientists with the tools necessary to investigate the mechanisms that promote MOM. However, natural variation presents several major challenges. Typical phenotyping research explores the impact of individual variation on personal health. Uniquely, variation in human milk will impact the nursing infant. The remainder of this paper will focus on the glycan components of breast milk that help shape the infant gut microbiome as well as factors that contribute to variation in milk composition.
Direct Effects of Glycans on Intestinal Microbiota
Compositionally, human milk contains an appreciable amount of oligosaccharides that is indigestible to the infant. Human milk glycans (HMG) are a large and diverse group of polysaccharides that include free human milk oligosaccharides (HMO), glycoproteins, glycopeptides, and glycolipids capable of enriching populations of Bifidobacteria. This enrichment is understood to be driven by the prebiotic effect of HMOs. HMOs are superior substrates for B. infantis in additional ways. For example, HMO consumption alters phenotypic expression and subsequent interactions with the host in ways that aid in its colonization and persistence in the infant intestine. Chichlowski et al. (2012) showed that growth of B. infantis ATCC15697 on HMOs compared with lactose increased binding to intestinal epithelial cells in vitro [65]. In a separate study, a similar increase in binding was determined using sialyllactose compared with oligofructose [66]. Compared with lactose, when B. infantis was incubated with HMOs, the production of inflammatory cytokines was diminished and the release of anti-inflammatory cytokines was increased [67]. When delivered in combination with breast milk, B. infantis supplementation led to decreases in γ-Proteobacteria compared with a matched formula fed group [68]. These studies suggest that the specific growth phenotype of milk glycan-enriched Bifidobacteria populations promotes persistence in situ and positively modulates the host epithelium.
HMO concentrations decrease from 23 g/L in colostrum to about 7 g/L in mature milk [69, 70]. The functional implications of the structural diversity of HMO are an important area of research as these complex sugars are indigestible by the infant. HMOs are comprised of glucose, galactose, N-acetylglucosamine, fucose, or sialic acid monosaccharides. The biosynthesis of HMOs in the mammary gland begins with the formation of a lactose core from galactose and glucose catalyzed by β-galactosyltransferase in the presence of α-lactalbumin. With few exceptions, all HMO structures consist of a lactose core [71]. Lactose can be elongated enzymatically by β1-3 linkage to lacto-N-biose or by β1-6 linkage to N-acetyllactosamine. The core HMO structure can be further elongated by the addition of lacto-N-biose and N-acetyllactosamine units by β1-3 and β1-6 linkages; terminal positions can be fucose monomers connected by α1-2, α1-3 or α1-4 linkages and/or sialic acid residues attached by α2-3 or α2-6 linkages. The distribution in term breast milk was reported as 35–50 % fucosylated, 12–14 % sialylated and 42–55 % non-fucosylated neutral HMO structures i [72]. Unlike HMO, glycoconjugates are even more complicated due to the respective protein or lipid moieties.
Lewis blood type and secretor status determine the structure and concentration of fucosylated oligosaccharides providing a clear example of how maternal genotype can affect milk composition and, subsequently, the infant gut microbiota [72, 73]. Women who possess a functional FUT2 gene, i.e., who express detectable levels of α-1,2-fucosyltransferase, in body fluids such as tears, saliva, and milk are called secretors. Non-secretors are women who fail to produce measureable levels of this enzyme, resulting in milk glycans with distinct linkages compared to secretors [74]. FUT3 is referred to as the Lewis gene and encodes an α-1,3/4-fucosyltransferase, adding even more complexity to HMO profiles [74]. Infants that are breast fed by secretor mothers are protected from moderate-to-severe diarrhea caused by a variety of enteric pathogens, ostensibly the HMOs act as decoy binding sites for the pathogens thus reducing access to epithelial binding sites [72, 75]. This is possible because secretor mothers produce more free milk oligosaccharides in terms of both structural diversity and total amount produced compared to non-secretor mothers [72, 73]. However, there is a great deal of functional redundancy in lactation. For example, the absence α-1,2-linked fucosylated HMOs in breast milk in non-secretors is offset by increased concentrations of lacto-N-fucopentaose III, lacto-N-fucopentaose II, 3-fucosyllactose, and lacto-N-tetraose [73, 76]. These oligosaccharides are also capable of pathogen deflection in the infant intestine [77], and potent prebiotics for beneficial Bifidobacteria strains [78].
Maternal phenotype may also influence the composition of HMO. For example, mothers with a BMI of 14–18 have significantly lower total HMOs compared with mothers with a BMI of 24–28 [79]. Very few studies take into consideration differences related to maternal phenotype and even less are able to link these to their impact on infant microbiome and infant gut function. A more comprehensive and systematic examination of the mother-infant dyad is required to understand the importance of variation in breast milk composition on infant health outcomes.
Breast Milk Proteins and Protection from Pathogens
In order to cultivate a healthy intestinal ecosystem, facilitating the growth of beneficial bacteria is needed but not sufficient. The growth of potentially harmful microorganisms must also be limited. This dichotomy is difficult to tease apart, because reducing the number of detrimental microbes may liberate niches that can be exploited by beneficial microbes may not directly affect the growth of these commensals. Glycosylated breast milk proteins such as lactoferrin, lysozyme, and immunoglobulins have important non-nutritive functions that protect infants from infection and, as a result, affect the development of the intestinal microbiome [80–82]. These bioactive proteins are the first line of defense against potential pathogens within the infant gut, and exert their protective effects via multiple and often overlapping mechanisms. These may have either direct or indirect effects on the intestinal microbiome by promoting the growth of beneficial bacteria, acting as substrates for microbial metabolism, engaging in pathogen destruction/deflection, in addition to other antibacterial activities such as modulating the infant immune system and stimulating epithelial barrier function.
Lysozyme (also known as muramidase or N-acetylmuramide glycanhydrolase) is an enzyme found in several mammalian secretions, including breast milk, which hydrolyzes cell wall peptidoglycans, resulting in cell lysis. This is a particularly effective defense against gram-positive pathogens such as Streptococcus and Bacillus [83]. Lysozyme is more highly concentrated in human milk (400 mg/ml) than milk from other species (0.130 mg/ml in cow’s milk and 0.250 mg/ml in goat’s milk) [84]. McInnis et al. (2012) analyzed the fecal microbiota of piglets fed milk produced by transgenic goats expressing human lysozyme at the same level found in human milk using both 16S rRNA gene sequencing and a Phylochip microarray [85]. Consumption of lysozyme-rich milk decreased levels of Firmicutes and increased those of Bacteroidetes compared to control-fed animals over time. More specifically, the abundance of families associated with gut health (Bifidobacteriaceae and Lactobacillaceae) increased, while those associated with disease (Mycobacteriaceae, Streptococcaceae, Campylobacterales) decreased in animals given the lysozyme-rich milk compared to controls.
Lactoferrin is the most abundant glycoprotein in milk [86], and has an extremely high affinity for iron. It’s structure and function has been extensively reviewed elsewhere [87–89]. It plays a key role in iron homeostasis in the newborn; sequestering this important nutrient away from potentially harmful bacteria and reserving it for uptake by enterocytes [90]. Lactoferrin may be partially digested in the infant’s intestine, resulting in the release of the peptide lactoferricin. Lactoferricin possesses even greater antibacterial activity than its precursor [91]. Lactoferrin also exhibits several immune-modulating properties in addition to those better-known iron-dependent, anti-infective capabilities [92, 93]. Differences in these functions, may be strongly influenced by glycosylation patterns, which vary over the course of lactation [94, 95]. As changes in protein glycosylation can significantly affect structure and stability, this could lead to changes in predominant function attributed to lactoferrin at different times in lactation.
Although all classes of immunoglobulins can be detected in human milk, the most abundant is IgA, specifically a form known as secretory IgA (sIgA). The infant is reliant on sIgA in breast milk since the infant since it possess an immature immune system, and does not produce sufficient amounts of sIgA on its own. Mucosal IgA production and, thus, sIgA levels, does increase with age, but it does not reach adult levels until age 5 [96]. Milk sIgA molecules are derived from maternal IgA antibodies that were developed against pathogens that the mother encountered via her own mucosal membranes, especially her digestive tract. Camphylobacter, Vibrio cholerae, Escherichia coli, Giardia, Salmonella, and Shigella [97, 98]. arecommon bacterial causes of diarrheal disease, which is second leading cause of death among children (<5 years of age) worldwide [99]. For example, milk sIgA antibodies against the above mentioned enteric pathogens helps explain the protective effect that breast feeding has against diarrheal disease [97].
One mechanism that explains immunoglobulin function in the intestinal lumen is immune exclusion, which involves preventing an antigen from entering into the systemic circulation through mucosal membranes. sIgA accomplishes this through agglutination, which precipitates antigens by mucus entrapment followed by mucociliary clearance [100]. sIgA may also bind to bacterial adhesins, which are glycosylated cell surface proteins that facilitate adherence to other cells or surfaces. This blocks attachment of ingested bacteria to receptors on host epithelial cells, preventing infection [101]. Perrier et al. (2006) showed that the secretory component of IgA isolated from human colostrum could bind to enteropathogenic E. coli, thereby protecting epithelial cells from bacterial invasion [102]. Another study demonstrated that secretory component isolated from human colostrum inhibited adhesion of Helicobacter pylori to human gastric mucous cells [103]. Rogier et al. (2014) developed a polymeric immunoglobulin receptor knock-out mouse model to assess the benefits of maternally derived sIgA on gut microbiome communities [104]. PhyloChip microarray hybridization of fecal DNA was used to identify roughly equivalent bacterial species at the phylogenetic level. Weanling mice that received maternal sIgA in breast milk had a significantly different gut microbial compositions compared to mice that did not receive maternal sIgA, and these differences persisted into adulthood. Specifically, Gram-negative Comamonadaceae was present only in weanling offspring of homozygote knock-out dams and Gram-negative Pasteurellaceae and Gram-positive Lachnospiraceae were also up-regulated in the absence of sIgA. They also found that maternal sIgA was needed to prevent the translocation of aerobic bacteria including, but not limited to, Ochrobacterium anthropi, a common opportunistic pathogen in the gut of preterm infants and mesenteric lymph nodes of immunocompromised individuals.
Maternal phenotype has been shown to influence levels and glycan composition of immunoglobulins. For example, colostrum from women diagnosed with type 2 diabetes has 30 % lower concentrations of IgA, IgG, and complement C3 protein compared to colostrum obtained from normo-glycemic women [105, 106]. Glycomic profiling using nano-HPLC chip/TOF MS + multivariate modeling by Smilowitz et al. (2013) showed that total abundances for HMO and HMO composition did not vary in breast milk between women with and without gestational diabetes mellitus (GDM), but that the total protein and composition of oligosaccharides N-linked to sIgA and lactoferrin were significantly different [107]. Specifically, the percent of mannose, fucose, and sialic acid residues per total oligosaccharide residues linked to sIgA were lower by up to 43 % in milk from women with GDM. On the other hand, the percent of fucose and sialic acid per total oligosaccharide residues linked to lactoferrin were higher up by to 72 % in milk from women with GDM. The effects of altered glycosylation patterns of human milk glycoproteins by gestational diabetes mellitus on infant gut microbiota have not been investigated.
Conclusion
The development of the infant intestinal ecosystem is a highly coordinated process with profound implications for both short- and long-term health. The pre-weaning period, i.e., the first 3–4 months of life, is a critical period in the development of the intestinal microbiome as early microbial colonization events provide important stimuli that guide the maturation of the immune system and help establish proper gut barrier function. Diet and other environmental factors such as mode of delivery and exposure to antibiotics play a significant role in determining the number and diversity of bacteria that the infant is exposed to. Breast milk is the gold standard for infant nutrition, because it delivers prebiotic glycans, live bacteria, and several different types of immune factors that provide passive protection from pathogens while simultaneously seeding the gut with wholesome bacterial species.
Recent data suggests that maternal genotype and phenotype may affect the quantity, composition, and functionality of milk components as well. The impact of maternal phenotypic variation on the infant intestinal microbiome and the implications for future infant health warrants further investigation. A better understanding of the role of milk in the metabolic and immunological programming of the neonate and the effects of maternal variation on the components responsible would provide insight into novel means of improving infant health. High resolution, comprehensive datasets on a large number mother-infant pairs that link milk composition, intestinal microbiome to health status of mother and infant will provide the insights necessary to understand the role of the intestinal microbiome on the developing metabolic and immune function.
Abbreviations
- FUT:
-
Fucosyltransferase gene
- GDM:
-
Gestational diabetes mellitus
- HMG:
-
Human milk glycans
- HMO:
-
Human milk oligosaccharides
- MOM:
-
Milk oriented microbiome
- NEC:
-
Necrotizing enterocolitis
- sIGA:
-
Soluble Immuglobulin A
References
Zivkovic AM, Lewis ZT, German JB, Mills DA. Establishment of a milk-oriented microbiota (MOM) in early life: how babies meet their MOMs. Funct Food Rev. 2013;5(1):3–12.
Palmer C, Bik EM, DiGiulio DB, Relman DA, Brown PO. Development of the human infant intestinal microbiota. PLoS Biol. 2007;5(7):e177. doi:10.1371/journal.pbio.0050177.
Adlerberth I, Wold AE. Establishment of the gut microbiota in Western infants. Acta Paediatr. 2009;98(2):229–38. doi:10.1111/j.1651-2227.2008.01060.x.
Penders J, Thijs C, Vink C, Stelma FF, Snijders B, Kummeling I, et al. Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics. 2006;118(2):511–21. doi:10.1542/peds.2005-2824.
Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin N Am. 2013;60(1):49–74. doi:10.1016/j.pcl.2012.10.002.
Bäckhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A. 2004;101(44):15718–23. doi:10.1073/pnas.0407076101.
Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Microbial ecology: human gut microbes associated with obesity. Nature. 2006;444(7122):1022–3. doi:10.1038/4441022a.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444(7122):1027–31. doi:10.1038/nature05414.
Krajmalnik-Brown R, Ilhan ZE, Kang DW, DiBaise JK. Effects of gut microbes on nutrient absorption and energy regulation. Nutr Clin Pract. 2012;27(2):201–14. doi:10.1177/0884533611436116.
Gordon JI, Dewey KG, Mills DA, Medzhitov RM. The human gut microbiota and undernutrition. Sci Transl Med. 2012;4(137):137ps12. doi:10.1126/scitranslmed.3004347.
LeBlanc JG, Milani C, de Giori GS, Sesma F, van Sinderen D, Ventura M. Bacteria as vitamin suppliers to their host: a gut microbiota perspective. Curr Opin Biotechnol. 2013;24(2):160–8. doi:10.1016/j.copbio.2012.08.005.
Jumpertz R, Le DS, Turnbaugh PJ, Trinidad C, Bogardus C, Gordon JI, et al. Energy-balance studies reveal associations between gut microbes, caloric load, and nutrient absorption in humans. Am J Clin Nutr. 2011;94(1):58–65. doi:10.3945/ajcn.110.010132.
Umesaki Y, Okada Y, Matsumoto S, Imaoka A, Setoyama H. Segmented filamentous bacteria are indigenous intestinal bacteria that activate intraepithelial lymphocytes and induce MHC class II molecules and fucosyl asialo GM1 glycolipids on the small intestinal epithelial cells in the ex-germ-free mouse. Microbiol Immunol. 1995;39(8):555–62.
Arboleya S, Bahrami B, Macfarlane S, Gueimonde M, Macfarlane GT, de Los Reyes-Gavilan CG. Production of immune response mediators by HT-29 intestinal cell-lines in the presence of Bifidobacterium-treated infant microbiota. Benefic Microbes. 2015;1–10. doi: 10.3920/bm2014.0111.
Maranduba CM, De Castro SB, de Souza GT, Rossato C. Intestinal microbiota as modulators of the immune system and neuroimmune system: impact on the host health and homeostasis. 2015;2015:931574.
Macpherson AJ, Harris NL. Interactions between commensal intestinal bacteria and the immune system. Nat Rev Immunol. 2004;4(6):478–85. doi:10.1038/nri1373.
O’Hara AM, Shanahan F. The gut flora as a forgotten organ. EMBO Rep. 2006;7(7):688–93. doi:10.1038/sj.embor.7400731.
McVey Neufeld KA, Mao YK, Bienenstock J, Foster JA, Kunze WA. The microbiome is essential for normal gut intrinsic primary afferent neuron excitability in the mouse. Neurogastroenterol Motil. 2013;25(2):183–e88. doi:10.1111/nmo.12049.
Bager P, Simonsen J, Nielsen NM, Frisch M. Cesarean section and offspring’s risk of inflammatory bowel disease: a national cohort study. Inflamm Bowel Dis. 2012;18(5):857–62. doi:10.1002/ibd.21805.
Bager P, Wohlfahrt J, Westergaard T. Caesarean delivery and risk of atopy and allergic disease: meta-analyses. Clin Exp Allergy. 2008;38(4):634–42. doi:10.1111/j.1365-2222.2008.02939.x.
Pei Z, Heinrich J, Fuertes E, Flexeder C, Hoffmann B, Lehmann I, et al. Cesarean delivery and risk of childhood obesity. J Pediatr. 2014;164(5):1068–73.e2. doi:10.1016/j.jpeds.2013.12.044.
Roger LC, Costabile A, Holland DT, Hoyles L, McCartney AL. Examination of faecal Bifidobacterium populations in breast- and formula-fed infants during the first 18 months of life. Microbiology. 2010;156:3329–41. doi:10.1099/Mic.0.043224-0.
Sela DA, Mills DA. Nursing our microbiota: molecular linkages between bifidobacteria and milk oligosaccharides. Trends Microbiol. 2010;18(7):298–307. doi:10.1016/j.tim.2010.03.008.
Ward RE, Ninonuevo M, Mills DA, Lebrilla CB, German JB. In vitro fermentation of breast milk oligosaccharides by Bifidobacterium infantis and Lactobacillus gasseri. Appl Environ Microbiol. 2006;72(6):4497–9. doi:10.1128/AEM.02515-05.
Ward RE, Ninonuevo M, Mills DA, Lebrilla CB, German JB. In vitro fermentability of human milk oligosaccharides by several strains of bifidobacteria. Mol Nutr Food Res. 2007;51(11):1398–405. doi:10.1002/mnfr.200700150.
LoCascio RG, Niñonuevo MR, Kronewitter SR, Freeman SL, German JB, Lebrilla CB, et al. A versatile and scalable strategy for glycoprofiling bifidobacterial consumption of human milk oligosaccharides. Microb Biotechnol. 2009;2(3):333–42. doi:10.1111/j.1751-7915.2008.00072.x.
Sela DA, Chapman J, Adeuya A, Kim JH, Chen F, Whitehead TR, et al. The genome sequence of Bifidobacterium longum subsp infantis reveals adaptations for milk utilization within the infant microbiome. Proc Natl Acad Sci U S A. 2008;105(48):18964–9. doi:10.1073/pnas.0809584105.
LoCascio RG, Desai P, Sela DA, Weimer B, Mills DA. Broad conservation of milk utilization genes in Bifidobacterium longum subsp. infantis as revealed by comparative genomic hybridization. Appl Environ Microbiol. 2010;76(22):7373–81. doi:10.1128/aem.00675-10.
Sela DA, Mills DA. The marriage of nutrigenomics with the microbiome: the case of infant-associated bifidobacteria and milk. Am J Clin Nutr. 2014;99(3):697s–703. doi:10.3945/ajcn.113.071795.
Huda MN, Lewis Z, Kalanetra KM, Rashid M, Ahmad SM, Raqib R, et al. Stool microbiota and vaccine responses of infants. Pediatrics. 2014;134(2):e362–72. doi:10.1542/peds.2013-3937.
Underwood MA, Arriola J, Gerber CW, Kaveti A, Kalanetra KM, Kananurak A, et al. Bifidobacterium longum subsp. infantis in experimental necrotizing enterocolitis: alterations in inflammation, innate immune response, and the microbiota. Pediatr Res. 2014. doi:10.1038/pr.2014.102.
Underwood MA, Salzman NH, Bennett SH, Barman M, Mills DA, Marcobal A, et al. A randomized placebo-controlled comparison of 2 prebiotic/probiotic combinations in preterm infants: impact on weight gain, intestinal microbiota, and fecal short-chain fatty acids. J Pediatr Gastroenterol Nutr. 2009;48(2):216–25. doi:10.1097/MPG.0b013e31818de195.
Jacobs SE, Tobin JM, Opie GF, Donath S, Tabrizi SN, Pirotta M, et al. Probiotic effects on late-onset sepsis in very preterm infants: a randomized controlled trial. Pediatrics. 2013;132(6):1055–62. doi:10.1542/peds.2013-1339.
Samanta M, Sarkar M, Ghosh P, Ghosh J, Sinha M, Chatterjee S. Prophylactic probiotics for prevention of necrotizing enterocolitis in very low birth weight newborns. J Trop Pediatr. 2009;55(2):128–31. doi:10.1093/tropej/fmn091.
Lin HC, Su BH, Chen AC, Lin TW, Tsai CH, Yeh TF, et al. Oral probiotics reduce the incidence and severity of necrotizing enterocolitis in very low birth weight infants. Pediatrics. 2005;115(1):1–4. doi:10.1542/peds.2004-1463.
Fernandez-Carrocera LA, Solis-Herrera A, Cabanillas-Ayon M, Gallardo-Sarmiento RB, Garcia-Perez CS, Montano-Rodriguez R, et al. Double-blind, randomised clinical assay to evaluate the efficacy of probiotics in preterm newborns weighing less than 1500 g in the prevention of necrotising enterocolitis. Arch Dis Child Fetal Neonatal Ed. 2013;98(1):F5–9. doi:10.1136/archdischild-2011-300435.
Bin-Nun A, Bromiker R, Wilschanski M, Kaplan M, Rudensky B, Caplan M, et al. Oral probiotics prevent necrotizing enterocolitis in very low birth weight neonates. J Pediatr. 2005;147(2):192–6. doi:10.1016/j.jpeds.2005.03.054.
Szajewska H, Guandalini S, Morelli L, Van Goudoever JB, Walker A. Effect of Bifidobacterium animalis subsp lactis supplementation in preterm infants: a systematic review of randomized controlled trials. J Pediatr Gastroenterol Nutr. 2010;51(2):203–9. doi:10.1097/MPG.0b013e3181dc0d93.
Unger S, Stintzi A, Shah P, Mack D, O’Connor DL. Gut microbiota of the very-low-birth-weight infant. Pediatr Res. 2015;77(1–2):205–13. doi:10.1038/pr.2014.162.
Taft DH, Ambalavanan N, Schibler KR, Yu Z, Newburg DS, Ward DV, et al. Intestinal microbiota of preterm infants differ over time and between hospitals. Microbiome. 2014;2:36. doi:10.1186/2049-2618-2-36.
Westerbeek EA, van den Berg A, Lafeber HN, Knol J, Fetter WP, van Elburg RM. The intestinal bacterial colonisation in preterm infants: a review of the literature. Clin Nutr. 2006;25(3):361–8. doi:10.1016/j.clnu.2006.03.002.
Groer MW, Luciano AA, Dishaw LJ, Ashmeade TL, Miller E, Gilbert JA. Development of the preterm infant gut microbiome: a research priority. Microbiome. 2014;2:38. doi:10.1186/2049-2618-2-38.
Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, Fierer N, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A. 2010;107(26):11971–5. doi:10.1073/pnas.1002601107.
Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486(7402):222–7. doi:10.1038/nature11053.
Fanaro S, Chierici R, Guerrini P, Vigi V. Intestinal microflora in early infancy: composition and development. Acta Paediatr Suppl. 2003;91(441):48–55.
Biasucci G, Benenati B, Morelli L, Bessi E, Boehm G. Cesarean delivery may affect the early biodiversity of intestinal bacteria. J Nutr. 2008;138(9):1796S–800.
Mshvildadze M, Neu J, Shuster J, Theriaque D, Li N, Mai V. Intestinal microbial ecology in premature infants assessed using non-culture based techniques. J Pediatr. 2010;156(1):20–5. doi:10.1016/j.jpeds.2009.06.063.
Wang Y, Hoenig JD, Malin KJ, Qamar S, Petrof EO, Sun J, et al. 16S rRNA gene-based analysis of fecal microbiota from preterm infants with and without necrotizing enterocolitis. ISME J. 2009;3(8):944–54. doi:10.1038/ismej.2009.37.
La Rosa PS, Warner BB, Zhou Y, Weinstock GM, Sodergren E, Hall-Moore CM, et al. Patterned progression of bacterial populations in the premature infant gut. Proc Natl Acad Sci U S A. 2014;111(34):12522–7. doi:10.1073/pnas.1409497111.
Perez PF, Dore J, Leclerc M, Levenez F, Benyacoub J, Serrant P, et al. Bacterial imprinting of the neonatal immune system: lessons from maternal cells? Pediatrics. 2007;119(3):e724–32. doi:10.1542/peds.2006-1649.
Martin R, Jimenez E, Heilig H, Fernandez L, Marin ML, Zoetendal EG, et al. Isolation of bifidobacteria from breast milk and assessment of the bifidobacterial population by PCR-denaturing gradient gel electrophoresis and quantitative real-time PCR. Appl Environ Microbiol. 2009;75(4):965.
Grönlund MM, Gueimonde M, Laitinen K, Kociubinski G, Grönroos T, Salminen S, et al. Maternal breast‐milk and intestinal bifidobacteria guide the compositional development of the Bifidobacterium microbiota in infants at risk of allergic disease. Clin Exp Allergy. 2007;37(12):1764–72.
Jost T, Lacroix C, Braegger C, Chassard C. Assessment of bacterial diversity in breast milk using culture-dependent and culture-independent approaches. Br J Nutr. 2013;110(7):1253–62. doi:10.1017/s0007114513000597.
Martin R, Langa S, Reviriego C, Jiminez E, Marin ML, Xaus J, et al. Human milk is a source of lactic acid bacteria for the infant gut. J Pediatr. 2003;143(6):754–8. doi:10.1016/j.jpeds.2003.09.028.
Delgado S, Arroyo R, Martin R, Rodriguez JM. PCR-DGGE assessment of the bacterial diversity of breast milk in women with lactational infectious mastitis. BMC Infect Dis. 2008;8:51. doi:10.1186/1471-2334-8-51.
Delgado S, Arroyo R, Jimenez E, Marin ML, del Campo R, Fernandez L, et al. Staphylococcus epidermidis strains isolated from breast milk of women suffering infectious mastitis: potential virulence traits and resistance to antibiotics. BMC Microbiol. 2009;9:82. doi:10.1186/1471-2180-9-82.
Hunt KM, Foster JA, Forney LJ, Schutte UM, Beck DL, Abdo Z, et al. Characterization of the diversity and temporal stability of bacterial communities in human milk. PLoS One. 2011;6(6):e21313. doi:10.1371/journal.pone.0021313.
Urbaniak C, Cummins J, Brackstone M, Macklaim JM, Gloor GB, Baban CK, et al. Microbiota of human breast tissue. Appl Environ Microbiol. 2014;80(10):3007–14.
Jost T, Lacroix C, Braegger CP, Rochat F, Chassard C. Vertical mother-neonate transfer of maternal gut bacteria via breastfeeding. Environ Microbiol. 2013. doi:10.1111/1462-2920.12238.
Grice EA, Kong HH, Conlan S, Deming CB, Davis J, Young AC, et al. Topographical and temporal diversity of the human skin microbiome. Science. 2009;324(5931):1190–2. doi:10.1126/science.1171700.
D’Amico CJ, DiNardo CA, Krystofiak S. Preventing contamination of breast pump kit attachments in the NICU. J Perinat Neonatal Nurs. 2003;17(2):150–7.
Cephas KD, Kim J, Mathai RA, Barry KA, Dowd SE, Meline BS, et al. Comparative analysis of salivary bacterial microbiome diversity in edentulous infants and their mothers or primary care givers using pyrosequencing. PLoS One. 2011;6(8):e23503. doi:10.1371/journal.pone.0023503.
Cabrera-Rubio R, Collado MC, Laitinen K, Salminen S, Isolauri E, Mira A. The human milk microbiome changes over lactation and is shaped by maternal weight and mode of delivery. Am J Clin Nutr. 2012;96(3):544–51. doi:10.3945/ajcn.112.037382.
Collado MC, Isolauri E, Laitinen K, Salminen S. Effect of mother’s weight on infant’s microbiota acquisition, composition, and activity during early infancy: a prospective follow-up study initiated in early pregnancy. Am J Clin Nutr. 2010;92(5):1023–30. doi:10.3945/ajcn.2010.29877.
Chichlowski M, De Lartigue G, German JB, Raybould HE, Mills DA. Bifidobacteria isolated from infants and cultured on human milk oligosaccharides affect intestinal epithelial function. J Pediatr Gastroenterol Nutr. 2012;55(3):321–7. doi:10.1097/MPG.0b013e31824fb899.
Kavanaugh DW, O’Callaghan J, Buttó LF, Slattery H, Lane J, Clyne M, et al. Exposure of bifidobacterium longum subsp. infantis to milk oligosaccharides increases adhesion to epithelial cells and induces a substantial transcriptional response. PLoS One. 2013;8(6):e67224.
Chichlowski M, De Lartigue G, German JB, Raybould HE, Mills DA. Bifidobacteria isolated from infants and cultured on human milk oligosaccharides affect intestinal epithelial function. J Pediatr Gastroenterol Nutri. 2012.
Underwood MA, Kalanetra KM, Bokulich NA, Lewis ZT, Mirmiran M, Tancredi DJ, et al. A comparison of two probiotic strains of bifidobacteria in premature infants. J Pediatr. 2013. doi:10.1016/j.jpeds.2013.07.017.
Coppa GV, Gabrielli O, Pierani P, Catassi C, Carlucci A, Giorgi PL. Changes in carbohydrate composition in human milk over 4 months of lactation. Pediatrics. 1993;91(3):637–41.
Gabrielli O, Zampini L, Galeazzi T, Padella L, Santoro L, Peila C, et al. Preterm milk oligosaccharides during the first month of lactation. Pediatrics. 2011;128(6):e1520–31.
Kunz C, Rudloff S, Baier W, Klein N, Strobel S. Oligosaccharides in human milk: structural, functional, and metabolic aspects. Annu Rev Nutr. 2000;20:699–722.
Totten SM, Zivkovic AM, Wu S, Ngyuen U, Freeman SL, Ruhaak LR, et al. Comprehensive profiles of human milk oligosaccharides yield highly sensitive and specific markers for determining secretor status in lactating mothers. J Proteome Res. 2012;11(12):6124–33.
Smilowitz JT, O’Sullivan A, Barile D, German JB, Lonnerdal B, Slupsky CM. The human milk metabolome reveals diverse oligosaccharide profiles. J Nutr. 2013;143(11):1709–18. doi:10.3945/jn.113.178772.
Smilowitz JT, Lebrilla CB, Mills DA, German JB, Freeman SL. Breast milk oligosaccharides: structure-function relationships in the neonate. Annu Rev Nutr. 2014;34:143–69. doi:10.1146/annurev-nutr-071813-105721.
Morrow AL, Ruiz-Palacios GM, Jiang X, Newburg DS. Human-milk glycans that inhibit pathogen binding protect breast-feeding infants against infectious diarrhea. J Nutr. 2005;135(5):1304–7.
Reinhold V, Zhang H, Hanneman A, Ashline D. Toward a platform for comprehensive glycan sequencing. Mol Cell Proteomics. 2013;12(4):866–73. doi:10.1074/mcp.R112.026823.
Jantscher-Krenn E, Lauwaet T, Bliss LA, Reed SL, Gillin FD, Bode L. Human milk oligosaccharides reduce Entamoeba histolytica attachment and cytotoxicity in vitro. Br J Nutr. 2012;108(10):1839–46. doi:10.1017/s0007114511007392.
Ruiz-Moyano S, Totten SM, Garrido DA, Smilowitz JT, German JB, Lebrilla CB, et al. Variation in consumption of human milk oligosaccharides by infant gut-associated strains of Bifidobacterium breve. Appl Environ Microbiol. 2013;79(19):6040–9. doi:10.1128/aem.01843-13.
Bode L, Jantscher-Krenn E. Structure-function relationships of human milk oligosaccharides. Adv Nutr. 2012;3(3):383S–91. doi:10.3945/an.111.001404.
Maga EA, Desai PT, Weimer BC, Dao N, Kultz D, Murray JD. Consumption of lysozyme-rich milk can alter microbial fecal populations. Appl Environ Microbiol. 2012;78(17):6153–60. doi:10.1128/aem.00956-12.
Oda H, Wakabayashi H, Yamauchi K, Abe F. Lactoferrin and bifidobacteria. Biometals. 2014;27(5):915–22. doi:10.1007/s10534-014-9741-8.
Maga EA, Weimer BC, Murray JD. Dissecting the role of milk components on gut microbiota composition. Gut Microbes. 2013;4(2):136–9. doi:10.4161/gmic.23188.
Masschalck B, Michiels CW. Antimicrobial properties of lysozyme in relation to foodborne vegetative bacteria. Crit Rev Microbiol. 2003;29(3):191–214. doi:10.1080/713610448.
Maga EA, Cullor JS, Smith W, Anderson GB, Murray JD. Human lysozyme expressed in the mammary gland of transgenic dairy goats can inhibit the growth of bacteria that cause mastitis and the cold-spoilage of milk. Foodborne Pathog Dis. 2006;3(4):384–92. doi:10.1089/fpd.2006.3.384.
McInnis EA, Kalanetra KM, Mills DA, Maga EA. Analysis of raw goat milk microbiota: impact of stage of lactation and lysozyme on microbial diversity. Food Microbiol. 2015;46:121–31. doi:10.1016/j.fm.2014.07.021.
Barboza M, Pinzon J, Wickramasinghe S, Froehlich JW, Moeller I, Smilowitz JT, et al. Glycosylation of human milk lactoferrin exhibits dynamic changes during early lactation enhancing its role in pathogenic bacteria-host interactions. Mol Cell Proteomics. 2012;11(6):M111 015248.
Aly E, Ros G, Frontela C. Structure and functions of lactoferrin as ingredient in infant formulas. J Food Res. 2013;2(4):25–36. doi:10.5539/jfr.v2n4p25.
Liu B, Newburg DS. Human milk glycoproteins protect infants against human pathogens. Breastfeed Med. 2013;8(4):354–62. doi:10.1089/bfm.2013.0016.
Wada Y, Lonnerdal B. Bioactive peptides derived from human milk proteins--mechanisms of action. J Nutr Biochem. 2014;25(5):503–14. doi:10.1016/j.jnutbio.2013.10.012.
Scarino ML. A sideways glance: take it or leave it? The role of lactoferrin in iron sequestration and delivery within the body. Genes Nutr. 2007;2(2):161–2. doi:10.1007/s12263-007-0054-1.
Gifford JL, Hunter HN, Vogel HJ. Lactoferricin: a lactoferrin-derived peptide with antimicrobial, antiviral, antitumor and immunological properties. Cell Mol Life Sci. 2005;62(22):2588–98. doi:10.1007/s00018-005-5373-z.
Actor JK, Hwang S-A, Kruzel ML. Lactoferrin as a natural immune modulator. Curr Pharm Des. 2009;15(17):1956–73.
Jenssen H, Hancock REW. Antimicrobial properties of lactoferrin. Biochimie. 2009;91(1):19–29. doi:10.1016/j.biochi.2008.05.015.
Wakabayashi H, Oda H, Yamauchi K, Abe F. Lactoferrin for prevention of common viral infections. J Infect Chemother. 2014;20(11):666–71. doi:10.1016/j.jiac.2014.08.003.
O’Riordan N, Gerlach JQ, Kilcoyne M, O’Callaghan J, Kane M, Hickey RM, et al. Profiling temporal changes in bovine milk lactoferrin glycosylation using lectin microarrays. Food Chem. 2014;165:388–96. doi:10.1016/j.foodchem.2014.05.086.
Fageras M, Tomicic S, Voor T, Bjorksten B, Jenmalm MC. Slow salivary secretory IgA maturation may relate to low microbial pressure and allergic symptoms in sensitized children. Pediatr Res. 2011;70(6):572–7.
Labbok MH, Clark D, Goldman AS. Breastfeeding: maintaining an irreplaceable immunological resource. Nat Rev Immunol. 2004;4(7):565–72. doi:10.1038/nri1393.
Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am J Clin Nutr. 2003;77(6):1537S–43.
Moszynski P. Diarrhoeal diseases still kill more than 1.5m children under 5 each year. BMJ. 2007;335(7632):1227. doi:10.1136/bmj.39426.352685.
Mathias A, Longet S, Corthesy B. Agglutinating secretory IgA preserves intestinal epithelial cell integrity during apical infection by Shigella flexneri. Infect Immun. 2013;81(8):3027–34. doi:10.1128/iai.00303-13.
Klemm P, Schembri MA. Bacterial adhesins: function and structure. Int J Med Microbiol. 2000;290(1):27–35. doi:10.1016/s1438-4221(00)80102-2.
Perrier C, Sprenger N, Corthesy B. Glycans on secretory component participate in innate protection against mucosal pathogens. J Biol Chem. 2006;281(20):14280–7. doi:10.1074/jbc.M512958200.
Boren T, Falk P, Roth KA, Larson G, Normark S. Attachment of Helicobacter pylori to human gastric epithelium mediated by blood group antigens. Science. 1993;262(5141):1892–5.
Rogier EW, Frantz AL, Bruno MEC, Wedlund L, Cohen DA, Stromberg AJ, et al. Secretory antibodies in breast milk promote long-term intestinal homeostasis by regulating the gut microbiota and host gene expression. Proc Natl Acad Sci. 2014;111(8):3074–9. doi:10.1073/pnas.1315792111.
Franca EL, Calderon Ide M, Vieira EL, Morceli G, Honorio-Franca AC. Transfer of maternal immunity to newborns of diabetic mothers. Clin Dev Immunol. 2012;2012:928187. doi:10.1155/2012/928187.
Morceli G, Franca EL, Magalhaes VB, Damasceno DC, Calderon IM, Honorio-Franca AC. Diabetes induced immunological and biochemical changes in human colostrum. Acta Paediatr. 2011;100(4):550–6. doi:10.1111/j.1651-2227.2010.02070.x.
Smilowitz JT, Totten SM, Huang J, Grapov D, Durham HA, Lammi-Keefe CJ, et al. Human milk secretory immunoglobulin a and lactoferrin N-glycans are altered in women with gestational diabetes mellitus. J Nutr. 2013;143(12):1906–12. doi:10.3945/jn.113.180695.
Acknowledgments
We acknowledge all of the researchers in the UC Davis Foods for Health Institute and the Milk Bioactives Program for their enthusiasm, imagination, and collective contribution to this subject matter. Work by the Milk Bioactives Program has been supported by the UC Davis Research Investments in the Sciences and Engineering Program; the UC Discovery Grant Program; the California Dairy Research Foundation; the Dairy Research Institute; the Bill & Melinda Gates Foundation; and the National Institutes of Health awards R01HD059127, R01HD065122, R01HD061923, R21AT006180, and R01AT007079, R01AT008759. We would also like to acknowledge seed funding from the UC Davis Office of Outreach and International Programs for UC Davis and UC Dublin Food and Health Strategic Partnership (UCD-UCD).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goldsmith, F., O’Sullivan, A., Smilowitz, J.T. et al. Lactation and Intestinal Microbiota: How Early Diet Shapes the Infant Gut. J Mammary Gland Biol Neoplasia 20, 149–158 (2015). https://doi.org/10.1007/s10911-015-9335-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10911-015-9335-2