Abstract
During normal mammary gland development, the tyrosine kinase Jak2 and its main substrate, the signal transducer and activator of transcription-5 (Stat5), are critical for the growth and differentiation of alveolar progenitors as well as the survival of secretory mammary epithelial cells. Genetic studies in mouse models support a role for the Stat5 transcription factor as a proto-oncogene in mammary tumor initiation. On the other hand, the analysis of nuclear Stat5 in human breast malignancies suggests a role of the Jak2/Stat5 pathway in the restriction of the metastatic potential of neoplastic mammary epithelial cells. Following an overview on the function of the Jak2/Stat5 pathway during normal mammary gland development, this review discusses recently published observations on human breast cancers as well as experimental evidence from genetically engineered mice that propose a dual role of Jak2/Stat5 signaling in breast cancer initiation and progression. Future studies to further test the concept of contrasting effects of Jak2/Stat5 pathway on breast cancer initiation and metastatic progression are proposed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Canonical Jak/Stat pathways mediate extra-cellular polypeptide signals, i.e. hormones and cytokines, from transmembrane receptors to target gene promoters in the nucleus. Specific cell types respond to these signals by altering their growth properties and their physiological activities [1]. Mammals possess four members of the Janus kinase (Jak) family, Jak1, Jak2, Tyk2, Jak3, and genetic studies in mice revealed that the biological functions of individual Janus kinases are pleiotropic. This is consistent with their suggested coupling to multiple cytokine receptors in a cell-type dependant manner [reviewed by [2]]. Specifically, Jak2 is suggested to mediate signals through single-chain receptors for ligands such as prolactin (PRL), growth hormone (GH), erythropoietin (EPO), and thrombopoietin (TPO) as well as the multi-chain IL-3 receptor family (e.g., IL-3R and GM-CSF-R), and members of the gp130 receptor family. Although more than one Jak family member was suggested to interact with certain cytokine receptors in vitro, knockout studies in mice revealed a remarkable physiological specificity of individual Janus kinases and their associated Stat proteins [2–4]. Seven signal transducers and activators of transcription (Stat) proteins have been identified in mammals that are being phosphorylated by their corresponding Janus kinases to become transcriptionally active: Stat1-4, Stat5a, Stat5b, and Stat6. As highlighted in this review, Stat5 is particularly important for normal mammary gland development since changes in the hormonal milieu, in particular elevated levels of PRL during pregnancy, trigger high levels of Stat5 phosphorylation and the numeric expansion and differentiation of milk-producing alveolar cells. The tyrosine kinase Jak2 is preassociated with the membrane-proximal region of the long form of the PRL receptor [5, 6]. Upon binding of PRL to its receptor, Jak2 autoactivates itself and phosphorylates Stat5a and Stat5b on positionally conserved tyrosine residues. In turn, active Stat5a and Stat5b translocate to the cell nucleus where they bind as homodimers or heterodimers to specific regulatory DNA elements. Using mammary epithelial cell lines conditionally deficient in Jak2 and their isogenic wild-type controls, Sakamoto and coworkers recently demonstrated that Jak2 is essential for the activation of Stat5 [7]. Jak2, however, was dispensable for the PRL-induced activation of c-Src, Fak, and the MAPK pathway, thus dissociating the Jak2/Stat5 pathway from other signaling cascades that emerge from the prolactin receptor (PRLR).
Stat5a was originally identified as a PRL-induced, nuclear DNA binding protein in udders of lactating sheep and therefore originally named the ‘mammary gland factor’ (MGF) [8]. Two years later, a second highly conserved Stat5b transcript was isolated from a cDNA library of the mouse mammary gland [9]. The two highly homologous Stat5a and Stat5b proteins encoded by different genes share an overall 96% amino acid similarity. Most of their structural differences are confined to the C-terminal transactivation domains. Truncated mutants that lack the C-terminus of either molecule function in a dominant negative manner for both Stat5a and Stat5b. Importantly, many studies performed over the last decade utilized molecular tools such as antibodies and nucleic acid-based reagents that do not discriminate between the two Stat5 isoforms, and, therefore, we will us the term ‘Stat5’ throughout this review when we discuss data where specific information regarding the Stat5 subtype is lacking or biologically insignificant.
In the nulliparous or nonpregnant parous mammary gland, Stat5 is constitutively activated at a basal level in rodent and human luminal epithelia cells [10, 11]. In experiments that utilized PRLR knockout mice, mammary transplants, or hypophysectomy in combination with hormone replacement, it was demonstrated that the basal activation of Stat5 was primarily maintained by circulating PRL [10]. During pregnancy and lactation, elevated levels of PRL hyper-activate both Stat5a and Stat5b in the mammary epithelium [9, 12] and, as discussed in the next section, drive the proliferative expansion and terminal differentiation of alveolar cells [13–15]. Despite the predominant role of PRL in the regulation of transcriptionally active Stat5, supra-physiological levels of growth hormone and EGF were also capable of activating Stat5 in mouse mammary epithelia, but to a much lower extent [10]. The administration of ovine PRL and growth hormone in virgin female rats showed that Stat5 was consistently activated by PRL in luminal cells of mammary ducts and alveolar units, while growth hormone preferentially activated Stat5 in a subpopulation of basal epithelial cells in addition to stromal cells [16] (Fig. 1). In addition, adipocytes and fibroblasts in the rat mammary stroma were preferentially responsive to growth hormone and not PRL [16]. Among members of the ErbB family of receptor tyrosine kinases, ErbB4 was suggested to activate Stat5 as part of an autocrine/paracrine loop supporting lactation [17]. In breast cancer cells, additional factors including the Src kinase [18] and Jak1 [19] may directly or indirectly regulate the activation of Stat5a and Stat5b. In conclusion, despite the suggested phosphorylation of Stat5 by a number of upstream signaling factors, the level of activation of this signal transducer is largely dependent on the cellular context as well as the developmental state of the mammary gland. PRL has been identified as the most potent growth factor for the basal activation of Stat5 in luminal epithelial cells throughout the epithelial ductal tree as well as proliferating and differentiating alveolar cells during pregnancy and lactation.
Schematic overview of prolactin and growth hormone responsive mammary epithelial cells. Prolactin and/or growth hormone-inducible Stat5 activation in epithelial cells within alveolar and ductal compartments of non-pregnant mammary glands is indicated. Luminal cells are columnar, basal/myoepithelial cells are spindle shaped, red color indicates prolactin responsiveness, green indicates GH-responsiveness, and yellow represents responsiveness to both prolactin and GH. Stromal fibroblasts and adipocytes that are responsive to growth hormone are not shown.
The murine mammary gland undergoes dramatic morphological changes before and after the onset of puberty and during the reproductive cycle (pregnancy, lactation, and weaning of the offspring). These defined stages of postnatal mammary gland growth and differentiation are controlled by the synergistic action of hormones and local growth factors as well as their downstream effectors. Although many hormone receptors are expressed and activated by their corresponding ligands in mammary epithelial cells during all phases of mammogenesis, biologically relevant functions of these receptors and their downstream targets seem to be limited to specified epithelial subtypes that emerge during distinct developmental stages. Specifically, PRL induces a basal activation of Stat5a and Stat5b in luminal epithelial cells within the ductal compartment of the mammary gland [10]. However, genetically engineered mouse models deficient in PRL or the PRLR [20, 21] provided experimental evidence that essential functions of PRL signaling are largely restricted to alveolar progenitors that reside at the terminal end of mature mammary ducts. The numeric expansion and differentiation of these alveolar progenitors occur predominantly during pregnancy and lactation. Females lacking two alleles of the PRLR specifically in mammary epithelial cells exhibited normal morphogenesis of ducts but lack milk-producing alveoli [22, 23].
PRLR signaling can synchronously activate multiple signaling cascades such as the Jak2 tyrosine kinase and the Stat5 transcription factor [24], the Ras-MAPK pathway [25, 26], Akt, and the phospholipase C-PKC pathway [27, 28]. Despite the ability of the PRLR to activate diverse signal transducers, females lacking Stat5a alone or in combination with Stat5b [13–15, 23] resemble the overall phenotypic abnormalities that were observed in the mammary glands of PRL and PRLR knockout mice. Of the two closely related Stat5 proteins, Stat5a is more abundant in mammary epithelia than Stat5b [9, 12]. Stat5a-null mice possess organized lobuloalveolar units that fail to functionally differentiate during pregnancy [14]. Although deficiency in Stat5b alone does not result in impaired mammary gland development [15], this protein appears to have nonredundant functions in the mammary gland. Liu and colleagues observed that Stat5b levels increase in Stat5a deficient females after multiple gestation cycles, and this upregulation of Stat5b coincides with restored functional differentiation and normal lactation in the absence of Stat5a [29, 30]. Stat5b knockout females are incapable of maintaining a pregnancy until term [15, 30]. Therefore, synergistic functions of the two Stat5 proteins during gestational changes in the mammary gland can only be examined using a transplantation model on the basis of conventional Stat5a/b double knockout females [22, 23] or by utilizing a Cre-mediated, mammary-specific deletion model that lacks the entire Stat5 locus [13]. Using the transplantation approach, Miyoshi et al. [23] performed a comparative study on mammary glands in recipient animals that carried either Stat5a/b-null or PRLR deficient mammary epithelia. Both types of transplants failed to undergo functional specification of alveolar progenitors. Unlike in Stat5a deficient mice, the absence of both Stat5 proteins resulted in a dramatic decrease in milk protein gene expression, in particular the whey acidic protein (Wap) and β-casein. Using electron microscopy, Miyoshi and coworkers also identified subtle differences between the PRLR-null and Stat5a/b deficient epithelia. The latter exhibited a slightly more severe phenotype. The authors suggested that this might be due to the ability of other growth factors, in particular growth hormone (GH) and the epidermal growth factor (EGF), to activate Stat5 in the absence of PRL signaling. Although Stat5 could be phosphorylated to some extent after administration of extra-physiological levels of GH and EGF, the signaling pathways that these growth factors stimulate were incapable of rescuing Stat5 activation or impaired PRLR signaling. Moreover, it has been shown previously [31] that the main targets of these growth factors are stromal cells and not the mammary epithelium. Therefore, the subtle differences between the PRLR-null and Stat5a/b deficient transplants observed by Miyoshi and coworkers could also be the consequence of a dissimilar ability of Stat5-null and PRLR mutant alveolar progenitors to respond to pregnancy-associated paracrine signaling events that originate in the wild-type stroma of the corresponding transplants.
Mice that lack both forms of Stat5 have multiple abnormalities in a variety of organ systems. In addition to female infertility and impaired mammary gland development, the first double knockout model generated by Teglund et al. [15] exhibits severe growth inhibition due to lack of GH signaling. In addition, these animals display impaired proliferation and survival of hematopoietic stem cells, T cells, and other hematopoietic lineages [15, 32–34]. Despite all these defects, many animals survive until adulthood, and male knockout mice are able to reproduce. This is in sharp contrast to a recently generated Stat5 knockout model that lacks the entire Stat5 locus after Cre-mediated deletion of Stat5a and Stat5b including their shared 3 prime intergenic sequence [13]. These double knockout mice are perinatal lethal or die shortly after birth due to severe anemia. The mammary-specific deletion of the Stat5 locus throughout the epithelium using the Stat5 conditional mutants in combination with MMTV-Cre transgenic mice resulted in impaired mammary gland development in postpartum females. Specifically, these females lacked differentiated alveolar cells. Thus, the phenotype described in the newly generated conditional knockout of Stat5 is quite similar to the mammary transplant model that utilizes the conventional knockout. Nonetheless, the underlying mechanisms for the significant phenotypic differences between the two models in other organs, in particular the hematopoietic system, remain to be determined.
The biological relevance of Stat5 activation in response to PRL signaling has been studied extensively over the last decade. In contrast, the enzymatic coupling between the PRLR and Stat5 in vivo and biologically relevant functions of Jak2 in mammary epithelia were more difficult to elucidate due to the early embryonic lethality of Jak2 conventional knockouts [35, 36]. The first phenotypic examination of these knockout mice revealed that the biological functions of Jak2 are pleiotropic. This finding is consistent with the suggested role of Jak2 as a signal transducer for multiple cytokine receptors in specific target cells [reviewed by [2]]. Jak2 is suggested to mediate signals through a variety of single- and multi-chain receptors that are crucial for mammary gland development including the PRLR, the GH receptor, and the gp130 receptor family [21, 31, 37]. To define a biological role for Jak2 during mammary development, Shillingford et al. [38] reported the first successful attempt to transplant mammary gland anlagen from Jak2 deficient embryos into wild-type recipient females. This initial study revealed that Jak2 deficient mammary epithelial cells showed a reduced proliferation index in animals treated with estrogen and progesterone. Reminiscent of the Stat5-null phenotype, the lack of Jak2 impaired the formation of secretory alveoli during pregnancy.
The development of a Jak2 conditional knockout mouse now allows the examination of a variety of biological functions of this kinase in virtually all cell types at defined developmental stages during embryogenesis and in adult animals [39]. The mammary-gland specific deletion of the Jak2 gene revealed that essential functions of this kinase are not restricted to the differentiation of alveolar progenitors during pregnancy [11]. The MMTV-Cre-mediated excision of Jak2 from all major epithelial subtypes of the nulliparous mammary gland resulted in a complete absence of lobular units that usually reside at the terminal ducts of tertiary side branches. This observation suggests that Jak2 is already critical for the specification of alveolar progenitors in virgin females. Moreover, this animal model demonstrates that Jak2 deficiency uncouples signaling from the PRLR to its downstream mediator Stat5 in the presence of normal and supraphysiological levels of PRL. Consequently, mutant females that lack Jak2 throughout the mammary ductal compartment were unable to lactate as a result of impaired alveolar proliferation and differentiation. This observation suggests that other components of the PRLR signaling cascade or additional growth factors and their signal transducers, which include other Janus kinase family members, were unable to compensate for the loss of Jak2 in vivo. Interestingly, the inactivation of Jak2 specifically in differentiating alveolar cells during the last phase of pregnancy and lactation revealed that this kinase is still required in mammary epithelial cells that have initiated an advanced differentiation program. As mentioned earlier, the expression of the whey acidic protein gene (Wap) depends greatly on the activation of Stat5 [23]. Consequently, the expression of Cre recombinase under the Wap gene promoter targets specifically PRL responsive alveolar cells during later stages or pregnancy. Following a burst of alveolar proliferation during early pregnancy, the Wap-Cre-mediated deletion of the upstream kinase Jak2 led to a negative selection of Jak2 deficient cells in late pregnant and postpartum mammary glands [11]. This continuing importance of PRL signaling through Jak2 in alveolar cells that undergo terminal differentiation is mediated through Stat5. Using the Wap-Cre transgenic mice to conditionally delete Stat5a and Stat5b, Cui et al. [13] confirmed that, like Jak2, these downstream signal transducers are required for the survival of differentiating epithelial cells. Additional evidence for the role of Stat5 during lactogenesis was provided by Iavnilovitch and coworkers [40]. The expression of constitutively active Stat5 resulted in a delay of postlactational involution and remodeling of the mammary gland, suggesting that transcriptionally active Stat5 is a survival factor that acts as a potent suppressor of apoptosis of terminally differentiated alveolar cells.
In summary, important biological functions of the Jak2/Stat5 signaling pathways are not restricted to the proliferation and differentiation of committed secretory alveolar cells during pregnancy. A basal level of Stat5 activation occurs in mammary epithelia of nulliparous females (mouse and humans alike), and Jak2 signaling mediates the specification of alveolar progenitors prior to the first pregnancy. The most dramatic physiological consequence of Jak2 deficiency and lack of Stat5 activation is the absence of secretory alveolar cells and impaired lactogenesis in postpartum females. Nonetheless, a sustained activation of Jak2 and Stat5 is important for the survival of committed alveolar cells that undergo an advanced differentiation program during late pregnancy and lactation. The rapid inactivation of Stat5 in response to milk stasis upon weaning of the offspring appears to be an early event that results in the termination of milk synthesis and the initiation of subsequent molecular events that trigger the postlactational remodeling of the mammary gland. Interestingly, this interference of active Jak2/Stat5 signaling during the first phase of involution appears to be mediated predominantly by intrinsic factors produced in the mammary gland that act synergistically with reduced circulating levels of lactogenic hormones [41].
FormalPara Jak2/Stat5 Signaling in Mouse Mammary TumorigenesisThe developmental studies that utilized genetically engineered mice lacking Jak2 and Stat5 during mammogenesis as well as Stat5 overexpression models clearly demonstrated that the Jak2/Stat5 signaling pathway plays a role in the specification and proliferation of alveolar progenitors and the survival of their more differentiated descendants along the alveolar lineage including terminally differentiated secretory epithelial cells. Hence, the most pertinent functions of Jak2/Stat5 signaling are defined to epithelial cells at the terminal ends of the ductal tree, a region known as terminal duct lobular units (TDLU) in humans or lobular units (LU) in mice [42]. It has been previously suggested that the TDLUs are the site in the human breast where neoplastic lesions arise [43]. Hence, this specific region in the mammary gland appears to contain hormone-responsive epithelial cells that exhibit an elevated susceptibly to neoplastic transformation depending on the reproductive status and the genetic predisposition.
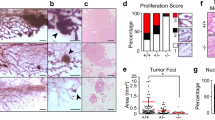
When deregulated, Jak2 and Stat5 may facilitate two important hallmarks of cancer, i.e. evasion from apoptosis and self-sufficiency in growth signals [44]. Although genomic alterations in Jak2 and Stat5 have not been reported in neoplastic lesions of the mammary gland, active Stat5 was detected in a subset of human breast cancer cases [45]. The notion that a hyperactive Jak2/Stat5 pathway plays a role in neoplastic transformation is supported by studies in caveolin-1 knockout mice [46–52]. Loss of Cav-1 removes a tonic inhibition of Jak2 signaling in mammary glands, resulting in hyperactivation of Stat5a and hyperplastic, well-differentiated mammary tumors. Interestingly, this hyperactivation of Stat5a is associated with increased ERα and Cyclin D1 expression [46, 47, 49, 50]. Recently, Iavnilovitch et al. [53] provided the first experimental evidence that the overexpression of wild-type and constitutively active Stat5 can promote the occurrence of sporadic mammary cancers in mice. Both animal models developed highly differentiated micropapillary and papillary adenocarcinomas after a latency of 8 to 12 months. Since only a fraction of these transgenic mice (10%) exhibited mammary cancer within two years, Stat5 cannot be considered a very potent proto-oncogene for the transformation of mammary epithelial cells in vivo. Classical oncogenes, for example c-Myc, activated Her2/Neu, or Wnt1, cause mammary cancer with a significantly higher incidence after a shorter latency period. Interestingly, also the overexpression of a Stat5 variant that lacks the C-terminal transactivation domain (i.e. a dominant-negative mutant) was able to transform mammary epithelial cells in vivo [53]. In contrast to the wild-type overexpression model, these females developed poorly differentiated adenocarcinomas after a nearly identical latency period. The inhibition of endogenous, wild-type Stat5 may be responsible for this histopathological phenomenon. It is also reasonable to suggest that Stat5 lacking a transactivation domain still possesses biological functions that mediate neoplastic transformation. For example, this short form of Stat5 may act as a transcriptional repressor [54] or it could simply serve as an adaptor for other interacting partners within a transcriptional complex. On the other hand, it is also possible that excess levels of the three forms of Stat5 investigated may elevate the occurrence spontaneous lesions in the FvB strain. Although no incidence in mammary cancer was observed by Iavnilovitch and colleagues in their control cohort, it has previously been reported that approximately 15% of FvB mice develop pituitary abnormalities by the age of two years [55–57]. These pituitary lesions lead to an increase in the secretion of lactogenic hormones including PRL that can cause alveolar hyperplasia and mammary cancer in aging mice. As a downstream mediator of PRL signaling, deregulated Stat5 expression could greatly modify the onset of these spontaneously arising lesions in the mammary gland.
The involvement of pregnancy hormones and PRL in Stat5-mediated mammary carcinogenesis was recently addressed in a follow-up report by Eilon et al. [58]. The β-lactoglobulin gene promoter, whose activation itself is induced by PRL, was used to regulate the expression of dominant active Stat5. It is therefore not entirely surprising that mammary tumorigenesis occurred more frequently in multiparous females. However, parity seemed to also have a lasting effect on the structure of the chromatin, in particular the histone acetylation of the Bcl-x and Cyclin D1 promoters that contain Stat5 binding sites. Consequently, cells that co-express Cyclin D1 and nuclear Stat5 were only observed in multiparous females. This finding is in line with the idea that epigenetic alterations, such as chromatin remodeling, DNA methylation, and histone modification, might be involved in the parity-induced changes in the fate of particular epithelial subtypes [59]. While the precise cellular basis for neoplastic transformation needs to be determined in the Stat5 overexpressing females, the presence of active Stat5 and Cyclin D1 within alveolar units of multiparous females as well as the dependency of tumorigenesis on a full-term gestation cycle indicate that parity-induced mammary epithelial cells (PI-MECs) might be the cancer-initiating epithelial subtype in this model [60]. PI-MECs are located within lobular units of parous females. They are defined as a pregnancy-hormone-responsive cell type that originates during late gestation and that exhibits, at least transiently, an advanced differentiation profile. Unlike terminally differentiated alveolar cells, PI-MECs do not undergo apoptosis during the postlactational involution period, and they serve as alveolar progenitors during subsequent pregnancies. Despite their limited role as alveolar progenitors, these cells retain characteristics of multipotent stem cells such as self-renewal and contribution to ductal and alveolar morphogenesis upon transplantation into a cleared fat pad [61–63]. It has been previously demonstrated that PI-MECs facilitate mammary tumorigenesis in multiparous females overexpressing Her2/neu, and the targeted inhibition of PI-MECs resulted in a significantly reduced tumor onset [64]. Given the fact that the genesis of PI-MECs during pregnancy depends on PRL signaling, targeting Jak2 or Stat5, therefore, might be a feasible strategy to prevent the onset of PRL-mediated mammary cancer. Indirect evidence for this assumption was first provided by Humphreys and Hennighausen [65]. The authors could demonstrate that females deficient in Stat5a exhibited delayed TGFα-induced tumorigenesis. The incidence of mammary cancer was also reduced in heterozygous Stat5a knockout mice that express the simian virus 40 (SV40) large T-antigen [66].
Although the findings from various genetically engineered mouse models suggest that PRL signaling through Stat5 can contribute to mammary cancer initiation, in vivo model systems are still missing that specifically address whether inhibiting the activation of the PRLR or its downstream mediators is also a therapeutically relevant strategy to treat the established disease, in particular metastatic breast cancer. A recent study by Oakes et al. [67] suggests that PRLR deficiency prevents the early progression of neoplasia to invasive carcinoma. It has yet to be determined whether this inhibition is due to the lack of Jak2/Stat5 signaling or the result of a reduced activation of other signal transducers (e.g. Src, Akt, Erk1/2). In contrast, immunohistochemical studies on human breast cancers suggest that transcriptionally active Stat5 is not required for cancer progression and metastasis [68]. Nuclear Stat5 was reported to be a favorable prognostic marker, in particular for lymph node-negative breast cancers, suggesting that active Stat5 contributes to a more differentiated phenotype of breast cancer cells within the primary lesion. As reviewed earlier, this finding is in line with the histopathological features of differentiated neoplasia observed in Stat5-overexpressing females. Unfortunately, conventional knockout models (e.g. Stat5a or Cyclin D1 deficient mice) in combination with oncogene-expressing transgenics are unsuitable to address whether the targeted inhibition of signal transducers are therapeutically relevant. Many of these animals never develop mammary cancer and consequently serve only as models for cancer prevention. Two experimental requirements are essential to model therapeutic intervention: (a) animal models need to develop progressing tumors, and (b) the therapeutic target protein has to be expressed in neoplastic cells [69]. None of these conditions exist in the current models to study Jak2/Stat5 signaling in cancer. Conditional knockout mice, such as Stat5a/b and Jak2 floxed mice, might be more suitable to adequately test therapeutic strategies in preclinical trials. These models allow determining whether the targeted inhibition of Jak2 or Stat5 is relevant for chemoprevention (Jak2/Stat5 deletion before tumor onset) and therapy (Jak2/Stat5 deletion in preneoplastic, neoplastic, or metastatic cells). With these new models now on hand, it will be interesting to further define the role of Jak2 and Stat5 during early and late-stage cancer progression.
FormalPara The Jak2/Stat5 Pathway in Human Breast CancerGenetic and endocrine studies in mice and rats have focused primarily on the mechanistic role of the PRL-Jak2-Stat5 pathway in mammary tumor initiation. In contrast, the majority of studies on clinical specimens from established human breast cancers are by nature correlative and address the involvement of these pathways in growth and invasive progression. Additional mechanistic studies of human breast cancer are being performed on cell lines in vitro or as xenotransplants in immunocompromized animals, two experimental models that both have significant experimental limitations. Cell lines provide important insight into biochemical reactions and pathways activation under relatively well-defined but unphysiological conditions. Therefore, knowledge gained from these in vitro studies are often not informative of the behavior of primary cancers in patients. Studies of human breast cancer cell lines xenotransplated into mice require an immunodeficient host environment and are affected by incompatibilities between the human cells and the microenvironmental and endocrine factors in the mouse [11, 70].
Biochemical evidence of Stat5 activation in selected human breast cancer specimens was initially reported in the form of Stat-DNA-binding activities, predominantly Stat1 and Stat3, in electrophoretic mobility shift assays performed on tumor extracts [71]. The cellular source of Stat5 DNA binding activity was not identified, since breast tumors consist of multiple cell types in addition to carcinoma cells including Stat5-containing stromal fibroblasts, vascular endothelium, and leukocytes. Later, in situ studies localized Stat5 within carcinoma cells of malignant human breast tumors [45]. Indeed, Stat5a was found to be activated in a high proportion of breast cancers. In the initial report by Cotarla et al. [45], approximately 76% of human breast tumors displayed nuclear localized, tyrosine phosphorylated Stat5a. In addition, the authors observed a positive correlation between tumor differentiation and active Stat5a. However, no relationship was found between nuclear localized Stat5a and menopausal status, tumor size, ploidy, percentage of cells in S-phase, lymph node metastases, ER, ErbB2, nuclear localized p21 or nuclear localized Stat5b/Stat3.
In a larger study investigating three separate clinical materials totaling more than 1,100 breast cancer specimens, active Stat5 in tumors was associated with favorable prognosis [68]. Consistent basal activation of Stat5 was detected in luminal cells of healthy breast epithelia but was frequently lost during metastatic progression of human breast cancer, with less than 20% of metastases exhibiting nuclear localized, tyrosine phoshorylated Stat5. Importantly, determination of levels of active Stat5, first in 683 patients in a training material to establish a threshold for positive Stat5 activation status, showed that tumors with active Stat5 were associated with more favorable overall patient survival. Applying this threshold to a second, independent test material of 428 patients with breast cancer-specific survival data confirmed the favorable prognostic effect of active Stat5. Furthermore, the favorable association was particularly pronounced in patients with breast cancer without detectable lymph node metastases. In fact, loss of active Stat5 in the primary tumor of patients with lymph node-negative breast cancer was associated with an eight-fold increased risk of latent, residual disease and subsequent death from breast cancer [68]. Importantly, in node-negative breast cancer Stat5 was an independent prognostic factor when other markers, including age, ER, PR, Her2, tumor size, and grade were included in multivariate analyses.
Two other studies have investigated associations of Stat5 in breast cancer with clinicopathological features using immunohistochemical analyses of clinical specimens. Yamashita and colleagues provided further support for the correlation between histological differentiation of breast cancer and levels of Stat5 in a material of 517 cases [72]. In ER-positive breast cancer, Stat5 protein levels correlated with favorable prognosis and were predictive of therapeutic response of breast cancer to antiestrogen therapy [72]. Furthermore, levels of Stat5a were generally reduced in breast carcinomas compared to that observed in healthy luminal breast epithelial cells [73], but were retained in more differentiated, secretory breast cancer [74].
A biological mechanism to explain the favorable prognostic effect associated with active Stat5 in human breast cancer was provided by the observation that Stat5a, but not a dominant-negative Stat5a or wild-type Stat3, promoted homotypic cell clustering and suppressed invasive characteristics of both ER-positive and ER-negative breast cancer cells in vitro [75]. In established human breast cancer, our current working hypothesis therefore is that Stat5 promotes differentiation and inhibits invasive characteristics. This notion has been supported by independent reports that demonstrate a positive correlation between breast tumor histological differentiation and activation of Stat5 [45, 72, 74]. Furthermore, inhibition of PRL-induced AP-1 signaling in breast cancer cells by Stat5 [76] also provides a potential growth-suppressive, prodifferentiation mechanism for Stat5. The concept that Stat5 may serve as a suppressor of human breast cancer progression has been recently highlighted in an independent review [77] and may underlie a reported prodifferentiation effect of PRL in breast cancer cells [78]. However, roles of PRL as a chemoattractant and a mitogenic factor in human breast cancer cells have also been reported [79, 80], possibly mediated by alternative PRLR pathways. Further studies, including in vivo studies of invasion and metastasis in mice, are needed to determine whether the observed Stat5 activation in breast cancer is causally involved in suppression of breast cancer metastatic progression, or whether inactivation of Stat5 is instead simply a correlative marker, for instance of epithelial-mesenchymal transition. Reports from one group have described a cell death-inducing effect of a dominant-negative Stat5 mutant upon adenoviral gene delivery into T47D cells [54, 81, 82]. Unfortunately these studies were not controlled for cytopathic effects of adenovirus, and work in our laboratory did not observe this effect when viral controls were included [75]. Nonetheless, further studies are needed to determine to what extent Stat5 also acts as a survival factor in established breast cancer [83–86]. More detailed analyses of the relative involvement of Stat5a and Stat5b in human breast cancer biology and prognosis will be important.
FormalPara Stat5 Target GenesThe identification of target genes of PRLR signaling through Jak2 and Stat5 in normal and malignant mammary glands are subject of ongoing investigations and may shed important mechanistic light on the function of Jak2-Stat5 pathways at different stages of tumor initiation and progression [87, 88]. While global transcript profiling is useful to identify candidate target genes following pathway activation, identification of direct Stat5a/b target genes require chromatin-immunoprecipitation assays and mutational verification of DNA binding sites. These studies show that some target genes are broadly activated by Stat5 such as the SOCS family member Cish [89]. Recently, Sakamoto et al. have shown in Jak2 deficient mammary epithelial cells that Cish mRNA and protein expression depends on active Jak2/Stat5 signaling [7]. However, in a particular cellular context, other target genes are activated conditionally by Stat5. For example, the Stat5-mediated expression of the beta2-macroglobulin gene requires pretreatment of T47D breast cancer cells with glucocorticoids to make its promoter accessible for Stat5 binding [89]. The expression of milk protein genes such as Wap and β-casein during pregnancy and lactation clearly depends on the PRL-induced activation of Stat5a and Stat5b in differentiated alveolar cells in vivo [14, 23]. On the other hand, Jak2/Stat5 target genes that specifically mediate the proliferative expansion of undifferentiated alveolar precursors in response to PRL signaling during pregnancy have not been intensively studied. Among regulators of the cell cycle, Cyclin D1 is a strong candidate target of PRL signaling since females deficient in Cyclin D1 exhibit impaired mammary gland development similar to Stat5 knockout mice [90, 91]. The proposed underlying mechanisms that link biologically relevant functions of Stat5 and Cyclin D1 in the developing mammary gland are quite diverse. It has been previously suggested that Cyclin D1 expression is directly regulated by PRL signaling through the Stat5-mediated transcriptional activation of the Cyclin D1 promoter [92, 93]. In addition, PRLR signaling might modulate indirectly Cyclin D1 expression through upregulation of IGF-2 [94]. Microarray expression studies, however, did not provide experimental evidence that Cyclin D1 is a direct or indirect transcriptional target of PRL signaling and Stat5 [87, 88]. Nonetheless, recent evidence from Jak2 knockout mammary epithelial cell lines suggests that signaling through Jak2 controls not only the expression of the Cyclin D1 mRNA but, more importantly, Jak2 regulates the accumulation of Cyclin D1 protein in the nucleus by inhibiting signal transducers that mediate the phosphorylation and nuclear export of Cyclin D1. The proliferation of Jak2 deficient MECs can be rescued by expressing a mutant form of Cyclin D1 that constitutively resides in the nucleus [7]. Finally, if Stat5 is directly involved in the maintenance of epithelial differentiation and suppression of epithelial-to-mesenchymal transitioning in breast cancer, a key set of candidates for further investigation are Stat5 target genes that are involved in maintaining an epithelial phenotype such as regulators of E-cadherin and homotypic cell adhesion.
FormalPara Jak2 and Stat5a/b Gene Alterations and Regulation in Breast Cancers and Other Human MalignanciesThe human Jak2 gene is localized to chromosome 9p24, and is frequently amplified in several hematopoietic malignancies, particularly lymphomas, where Jak2/Stat5 signaling promotes tumorigenesis [95, 96]. In addition, a V617F activating mutation was found in a number of myeloproliferative disorders [97, 98]. Furthermore, in lymphomas, Jak2 is also involved in chromosomal translocations with the TEL gene to generate a constitutively active TEL-Jak2 fusion gene product. In contrast, Jak2 gene amplification or activating mutations have not been found in human breast cancers [99]. Intriguingly, one study reported loss of heterozygosity or homozygous deletion at microsatellite loci spanning 9p22 to 9p24 in 40% (32 of 80 cases) of human breast cancer, suggesting that Jak2 could be lost in some breast cancers. The human Stat5a and Stat5b loci are located on chromosome 17q21.1-21.2 [100] where they reside in a head-to-head orientation separated by only 10 kb. Thus far, germline mutations have only been reported for the Stat5b locus, and these alterations lead to severe growth hormone insensitivity as well as bleeding diathesis due to defective thrombocyte aggregation [101, 102]. The Stat5a/b genes are in close proximity to Brca1 (17q21) and the Her2/neu locus (17q21.1). Somatic loss of heterozygosity (LOH) on chromosome 17 occurs frequently in human breast cancers but their detailed analysis is complicated since as many as six regions of 17q are affected. While interstitial deletions include the chromosomal region 17q21, the Stat5a/b gene loci have not been subject of a direct study in human breast cancers. In light of the proposed invasion-suppressive role of Stat5, a detailed investigation of these loci therefore is now highly warranted. Gene deletions may account for a subset of advanced breast cancer cases that lack Stat5 expression. Epigenetic silencing might be another mechanism that leads to an absence of Stat5 in advanced lesions. Nonetheless, the Stat5 protein was detected in the majority of breast cancer cases that lack phosphorylated Stat5, suggesting that other negative regulators of Jak2/Stat5 signaling, such as tyrosine phosphatases as well as SOCS and PIAS proteins, might play a role in the suppression of the activity of Stat5.
FormalPara Concluding RemarksThe peptide hormone PRL plays an important role in normal mammary gland development and breast cancer etiology. Studies in mouse models for breast cancer provided experimental evidence that the Jak2/Stat5 pathway, which is the central signaling axis used by this hormone during normal mammogenesis, also contributes to the tumor-promoting effects of PRL during breast cancer initiation. Nonetheless, a differentiation-promoting and invasion-suppressive role of Stat5 in advanced human breast cancers has been proposed. Consistent with this notion, the levels of active Stat5 are significantly reduced in primary breast cancers with unfavorable prognosis and in metastatic lesions. Despite reduced Stat5 activity, it is reasonable to hypothesize that PRL is still capable of promoting breast cancer progression and invasion through Jak2/Stat5-independent pathways. It is known that upon ligand binding, the PRLR can activate additional signal transducers including c-Src, Fak, Ras-MAPK, C-PKC, PI3K, and Akt. It was demonstrated recently that the activity of some of these signal transducers may not depend on the functionality of Jak2 as previously suggested. It is therefore possible that a reduction in phosphorylated Stat5 in poorly differentiated breast cancers is able to potentiate PRL signaling through these parallel signaling pathways that are known to mediate other biological processes such as cell proliferation and cell survival. Future studies that might shed light on the biological significance of such combinatorial effects of altered PRL signaling could help explain the divergent role of Jak2/Stat5 and PRL signaling in the etiology of breast cancer initiation and progression.
Abbreviations
- Akt:
-
thymoma viral proto-oncogene 1
- AP-1:
-
adaptor protein 1
- Bcl-x:
-
B-cell leukemia gene 2-like 1 gene
- Brca1:
-
breast and ovarian cancer gene 1, early onset
- Cish:
-
cytokine inducible SH2-containing protein
- Cre:
-
site-specific recombinase in bacteriophage P1 (catalyses recombination between loxP sites)
- EGF:
-
epidermal growth factor
- ER:
-
estrogen receptor
- ErbB2–4:
-
epidermal growth factor receptors 2–4
- Erk1/2:
-
mitogen activated protein kinases
- Fak:
-
focal adhesion kinase
- floxed:
-
flanked by loxP sites
- GH:
-
growth hormone
- GM-CSF-R:
-
colony stimulating factor 2 receptor, alpha, low-affinity (granulocyte-macrophage)
- gp130:
-
interleukin 6 signal transducer
- Her2/Neu:
-
ErbB2; member of the epidermal growth factor receptor family
- IGF-2:
-
insulin-like growth factor 2
- IL-3R:
-
interleukin 3 receptor
- Jak2:
-
Janus kinase 2
- loxP:
-
locus of crossing (X-ing) over
- MAPK:
-
mitogen activated protein kinase
- MECs:
-
mammary epithelial cells
- MMTV:
-
mouse mammary tumor virus
- Myc:
-
myelocytomatosis oncogene
- PI-MECs:
-
parity-induced mammary epithelial cells
- PI3K:
-
phosphatidylinositol 3-kinase
- PIAS:
-
protein inhibitor of activated signal transducers and activators of transcription
- PRL:
-
prolactin
- PRLR:
-
prolactin receptor
- PKC:
-
protein kinase C
- Ras:
-
Harvey rat sarcoma virus oncogene 1
- SOCS:
-
suppressor of cytokine signaling
- Src:
-
Rous sarcoma oncogene
- Stat5:
-
signal transducer and activatorof transcription 5
- SV40:
-
simian virus 40
- TEL:
-
ets variant gene 6
- TDLU:
-
terminal duct lobular unit
- TGFα:
-
transforming growth factor alpha
- Tyk2:
-
tyrosine kinase 2
- WAP:
-
whey acidic protein
- Wnt1:
-
wingless-related MMTV integration site 1
References
Aaronson DS, Horvath CM. A road map for those who don’t know JAK-STAT. Science. 2002;296(5573):1653–5.
Kisseleva T, Bhattacharya S, Braunstein J, Schindler CW. Signaling through the JAK/STAT pathway, recent advances and future challenges. Gene. 2002;285(1–2):1–24.
Ihle JN. The Stat family in cytokine signaling. Curr Opin Cell Biol. 2001;13(2):211–7.
Levy DE, Darnell JE Jr. Stats: transcriptional control and biological impact. Nat Rev Mol Cell Biol. 2002;3(9):651–62.
Rui H, Kirken RA, Farrar WL. Activation of receptor-associated tyrosine kinase JAK2 by prolactin. J Biol Chem. 1994;269(7):5364–8.
DaSilva L, Howard OM, Rui H, Kirken RA, Farrar WL. Growth signaling and JAK2 association mediated by membrane-proximal cytoplasmic regions of prolactin receptors. J Biol Chem. 1994;269(28):18267–70.
Sakamoto K, Creamer BA, Triplett AA, Wagner KU. The Janus kinase 2 is required for expression and nuclear accumulation of Cyclin D1 in proliferating mammary epithelial cells. Mol Endocrinol. 2007;21(8):1877–92.
Wakao H, Gouilleux F, Groner B. Mammary gland factor (MGF) is a novel member of the cytokine regulated transcription factor gene family and confers the prolactin response [published erratum appears in EMBO J 1995 Feb 15;14(4):854–5]. EMBO J. 1994;13(9):2182–91.
Liu X, Robinson GW, Gouilleux F, Groner B, Hennighausen L. Cloning and expression of Stat5 and an additional homologue (Stat5b) involved in prolactin signal transduction in mouse mammary tissue. Proc Natl Acad Sci USA 1995;92(19):8831–5.
Nevalainen MT, Xie J, Bubendorf L, Wagner KU, Rui H. Basal activation of transcription factor signal transducer and activator of transcription (Stat5) in nonpregnant mouse and human breast epithelium. Mol Endocrinol. 2002;16(5):1108–24.
Wagner KU, Krempler A, Triplett AA, Qi Y, George NM, Zhu J, et al. Impaired alveologenesis and maintenance of secretory mammary epithelial cells in Jak2 conditional knockout mice. Mol Cell Biol. 2004;24(12):5510–20.
Liu X, Robinson GW, Hennighausen L. Activation of Stat5a and Stat5b by tyrosine phosphorylation is tightly linked to mammary gland differentiation. Mol Endocrinol. 1996;10(12):1496–506.
Cui Y, Riedlinger G, Miyoshi K, Tang W, Li C, Deng CX, et al. Inactivation of Stat5 in mouse mammary epithelium during pregnancy reveals distinct functions in cell proliferation, survival, and differentiation. Mol Cell Biol. 2004;24(18):8037–47.
Liu X, Robinson GW, Wagner KU, Garrett L, Wynshaw-Boris A, Hennighausen L. Stat5a is mandatory for adult mammary gland development and lactogenesis. Genes Dev. 1997;11(2):179–86.
Teglund S, McKay C, Schuetz E, van Deursen JM, Stravopodis D, Wang D, et al. Stat5a and Stat5b proteins have essential and nonessential, or redundant, roles in cytokine responses. Cell. 1998;93:841–50.
LeBaron MJ, Ahonen TJ, Nevalainen MT, Rui H. In vivo response-based identification of direct hormone target cell populations using high-density tissue arrays. Endocrinology. 2007;148(3):989–1008.
Jones FE, Welte T, Fu XY, Stern DF. ErbB4 signaling in the mammary gland is required for lobuloalveolar development and Stat5 activation during lactation. J Cell Biol. 1999;147(1):77–88.
Kazansky AV, Kabotyanski EB, Wyszomierski SL, Mancini MA, Rosen JM. Differential effects of prolactin and src/abl kinases on the nuclear translocation of STAT5B and STAT5A. J Biol Chem. 1999;274(32):22484–92.
Neilson LM, Zhu J, Xie J, Malabarba MG, Sakamoto K, Wagner KU, Kirken RA, Rui H. Coactivation of janus tyrosine kinase (Jak)1 positively modulates prolactin-Jak2 signaling in breast cancer: recruitment of ERK and signal transducer and activator of transcription (Stat)3 and enhancement of Akt and Stat5a/b pathways. Mol Endocrinol. 2007;21(9):2218–32.
Horseman ND, Zhao W, Montecino-Rodriguez E, Tanaka M, Nakashima K, Engle SJ, et al. Defective mammopoiesis, but normal hematopoiesis, in mice with a targeted disruption of the prolactin gene. EMBO J. 1997;16:6926–35.
Ormandy CJ, Camus A, Barra J, Damotte D, Lucas B, Buteau H, et al. Null mutation of the prolactin receptor gene produces multiple reproductive defects in the mouse. Genes Dev. 1997;11(2):167–78.
Brisken C, Kaur S, Chavarria TE, Binart N, Sutherland RL, Weinberg RA, et al. Prolactin controls mammary gland development via direct and indirect mechanisms. Dev Biol. 1999;210(1):96–106.
Miyoshi K, Shillingford JM, Smith GH, Grimm SL, Wagner KU, Oka T, et al. Signal transducer and activator of transcription (Stat) 5 controls the proliferation and differentiation of mammary alveolar epithelium. J Cell Biol. 2001;155(4):531–42.
Hennighausen L, Robinson GW, Wagner KU, Liu W. Prolactin signaling in mammary gland development. J Biol Chem. 1997;272(12):7567–9.
Das R, Vonderhaar BK. Prolactin as a mitogen in mammary cells. J Mammary Gland Biol Neoplasia. 1997;2(1):29–39.
Erwin RA, Kirken RA, Malabarba MG, Farrar WL, Rui H. Prolactin activates Ras via signaling proteins SHC, growth factor receptor bound 2, and son of sevenless. Endocrinology. 1995;136(8):3512–8.
Grimley PM, Dong F, Rui H. Stat5a and Stat5b: fraternal twins of signal transduction and transcriptional activation. Cytokine Growth Factor Rev. 1999;10(2):131–57.
Llovera M, Touraine P, Kelly PA, Goffin V. Involvement of prolactin in breast cancer: redefining the molecular targets. Exp Gerontol. 2000;35(1):41–51.
Liu X, Gallego MI, Smith GH, Robinson GW, Hennighausen L. Functional rescue of Stat5a-null mammary tissue through the activation of compensating signals including Stat5b. Cell Growth Differ. 1998;9(9):795–803.
Udy GB, Towers RP, Snell RG, Wilkins RJ, Park SH, Ram PA, et al. Requirement of STAT5b for sexual dimorphism of body growth rates and liver gene expression. Proc Natl Acad Sci USA 1997;94(14):7239–44.
Gallego MI, Binart N, Robinson GW, Okagaki R, Coschigano KT, Perry J, et al. Prolactin, growth hormone, and epidermal growth factor activate Stat5 in different compartments of mammary tissue and exert different and overlapping developmental effects. Dev Biol. 2001;229(1):163–75.
Bunting KD, Bradley HL, Hawley TS, Moriggl R, Sorrentino BP, Ihle JN. Reduced lymphomyeloid repopulating activity from adult bone marrow and fetal liver of mice lacking expression of STAT5. Blood. 2002;99(2):479–87.
Kieslinger M, Woldman I, Moriggl R, Hofmann J, Marine JC, Ihle JN, et al. Antiapoptotic activity of Stat5 required during terminal stages of myeloid differentiation. Genes Dev. 2000;14(2):232–44.
Moriggl R, Topham DJ, Teglund S, Sexl V, McKay C, Wang D, et al. Stat5 is required for IL-2-induced cell cycle progression of peripheral T cells. Immunity. 1999;10(2):249–59.
Parganas E, Wang D, Stravopodis D, Topham DJ, Marine JC, Teglund S, et al. Jak2 is essential for signaling through a variety of cytokine receptors. Cell. 1998;93:385–95.
Neubauer H, Cumano A, Muller M, Wu H, Huffstadt U, Pfeffer K. Jak2 deficiency defines an essential developmental checkpoint in definitive hematopoiesis. Cell. 1998;93:397–409.
Zhao L, Hart S, Cheng J, Melenhorst JJ, Bierie B, Ernst M, et al. Mammary gland remodeling depends on gp130 signaling through Stat3 and MAPK. J Biol Chem. 2004;279(42):44093–100.
Shillingford JM, Miyoshi K, Robinson GW, Grimm SL, Rosen JM, Neubauer H, et al. Jak2 is an essential tyrosine kinase involved in pregnancy-mediated development of mammary secretory epithelium. Mol Endocrinol. 2002;16(3):563–70.
Krempler A, Qi Y, Triplett AA, Zhu J, Rui H, Wagner KU. Generation of a conditional knockout allele for the Janus kinase 2 (Jak2) gene in mice. Genesis. 2004;40(1):52–7.
Iavnilovitch E, Groner B, Barash I. Overexpression and forced activation of stat5 in mammary gland of transgenic mice promotes cellular proliferation, enhances differentiation, and delays postlactational apoptosis. Mol Cancer Res 2002;1(1):32–47.
Li M, Liu X, Robinson G, Bar-Peled U, Wagner KU, Young WS, et al. Mammary-derived signals activate programmed cell death during the first stage of mammary gland involution. Proc Natl Acad Sci USA 1997;94(7):3425–30.
Cardiff RD. Are the TDLU of the human the same as the LA of mice? J Mammary Gland Biol Neoplasia 1998;3(1):3–5.
Wellings SR, Jensen HM, Marcum RG. An atlas of subgross pathology of the human breast with special reference to possible precancerous lesions. J Natl Cancer Inst. 1975;55(2):231–73.
Hanahan D, Weinberg RA. The hallmarks of cancer. Cell 2000;100(1):57–70.
Cotarla I, Ren S, Zhang Y, Gehan E, Singh B, Furth PA. Stat5a is tyrosine phosphorylated and nuclear localized in a high proportion of human breast cancers. Int J Cancer. 2004;108(5):665–71.
Li T, Sotgia F, Vuolo MA, Li M, Yang WC, Pestell RG, et al. Caveolin-1 mutations in human breast cancer: functional association with estrogen receptor alpha-positive status. Am J Pathol 2006;168(6):1998–2013.
Park DS, Lee H, Frank PG, Razani B, Nguyen AV, Parlow AF, et al. Caveolin-1-deficient mice show accelerated mammary gland development during pregnancy, premature lactation, and hyperactivation of the Jak-2/STAT5a signaling cascade. Mol Biol Cell. 2002;13(10):3416–30.
Sloan EK, Stanley KL, Anderson RL. Caveolin-1 inhibits breast cancer growth and metastasis. Oncogene 2004;23:7893–7.
Li J, Hassan GS, Williams TM, Minetti C, Pestell RG, Tanowitz HB, et al. Loss of caveolin-1 causes the hyper-proliferation of intestinal crypt stem cells, with increased sensitivity to whole body gamma-radiation. Cell Cycle. 2005;4(12):1817–25.
Sotgia F, Schubert W, Pestell RG, Lisanti MP. Genetic ablation of caveolin-1 in mammary epithelial cells increases milk production and hyper-activates STAT5a signaling. Cancer Biol Ther. 2006;5(3):292–7.
Sotgia F, Williams TM, Schubert W, Medina F, Minetti C, Pestell RG, et al. Caveolin-1 deficiency (−/−) conveys premalignant alterations in mammary epithelia, with abnormal lumen formation, growth factor independence, and cell invasiveness. Am J Pathol. 2006;168(1):292–309.
Williams TM, Cheung MW, Park DS, Razani B, Cohen AW, Muller WJ, et al. Loss of caveolin-1 gene expression accelerates the development of dysplastic mammary lesions in tumor-prone transgenic mice. Mol Biol Cell. 2003;14(3):1027–42.
Iavnilovitch E, Cardiff RD, Groner B, Barash I. Deregulation of Stat5 expression and activation causes mammary tumors in transgenic mice. Int J Cancer. 2004;112(4):607–19.
Yamashita H, Iwase H, Toyama T, Fujii Y. Naturally occurring dominant-negative Stat5 suppresses transcriptional activity of estrogen receptors and induces apoptosis in T47D breast cancer cells. Oncogene. 2003;22(11):1638–52.
Mahler JF, Stokes W, Mann PC, Takaoka M, Maronpot RR. Spontaneous lesions in aging FVB/N mice. Toxicol Pathol. 1996;24(6):710–6.
Nieto AI, Shyamala G, Galvez JJ, Thordarson G, Wakefield LM, Cardiff RD. Persistent mammary hyperplasia in FVB/N mice. Comp Med. 2003;53(4):433–8.
Wakefield LM, Thordarson G, Nieto AI, Shyamala G, Galvez JJ, Anver MR, et al. Spontaneous pituitary abnormalities and mammary hyperplasia in FVB/NCr mice: implications for mouse modeling. Comp Med. 2003;53(4):424–32.
Eilon T, Groner B, Barash I. Tumors caused by overexpression and forced activation of Stat5 in mammary epithelial cells of transgenic mice are parity-dependent and developed in aged, postestropausal females. Int J Cancer. 2007;121(9):1892–902.
Ginger MR, Gonzalez-Rimbau MF, Gay JP, Rosen JM. Persistent changes in gene expression induced by estrogen and progesterone in the rat mammary gland. Mol Endocrinol. 2001;15(11):1993–2009.
Wagner KU, Smith GH. Pregnancy and stem cell behavior. J Mammary Gland Biol Neoplasia. 2005;10(1):25–36.
Boulanger CA, Wagner KU, Smith GH. Parity-induced mouse mammary epithelial cells are pluripotent, self-renewing and sensitive to TGF-beta1 expression. Oncogene. 2005;24(4):552–60.
Matulka LA, Triplett AA, Wagner KU. Parity-induced mammary epithelial cells are multipotent and express cell surface markers associated with stem cells. Dev Biol. 2007;303(1):29–44.
Wagner KU, Boulanger CA, Henry MD, Sgagias M, Hennighausen L, Smith GH. An adjunct mammary epithelial cell population in parous females: its role in functional adaptation and tissue renewal. Development. 2002;129(6):1377–86.
Henry MD, Triplett AA, Oh KB, Smith GH, Wagner KU. Parity-induced mammary epithelial cells facilitate tumorigenesis in MMTV-neu transgenic mice. Oncogene. 2004;23(41):6980–5.
Humphreys RC, Hennighausen L. Signal transducer and activator of transcription 5a influences mammary epithelial cell survival and tumorigenesis. Cell Growth Differ. 1999;10(10):685–94.
Ren S, Cai HR, Li M, Furth PA. Loss of Stat5a delays mammary cancer progression in a mouse model. Oncogene. 2002;21(27):4335–9.
Oakes SR, Robertson FG, Kench JG, Gardiner-Garden M, Wand MP, Green JE, et al. Loss of mammary epithelial prolactin receptor delays tumor formation by reducing cell proliferation in low-grade preinvasive lesions. Oncogene. 2007;26(4):543–53.
Nevalainen MT, Xie J, Torhorst J, Bubendorf L, Haas P, Kononen J, et al. Signal transducer and activator of transcription-5 activation and breast cancer prognosis. J Clin Oncol. 2004;22(11):2053–60.
Matulka LA, Wagner K-U. Models of breast cancer. Drug Discov Today 2005;2:1–6.
Utama FE, Lebaron MJ, Neilson LM, Sultan AS, Parlow AF, Wagner KU, et al. Human prolactin receptors are insensitive to mouse prolactin: implications for xenotransplant modeling of human breast cancer in mice. J Endocrinol. 2006;188(3):589–601.
Watson CJ, Miller WR. Elevated levels of members of the STAT family of transcription factors in breast carcinoma nuclear extracts. Br J Cancer. 1995;71(4):840–4.
Yamashita H, Nishio M, Ando Y, Zhang Z, Hamaguchi M, Mita K, et al. Stat5 expression predicts response to endocrine therapy and improves survival in estrogen receptor-positive breast cancer. Endocr Relat Cancer. 2006;13(3):885–93.
Bratthauer GL, Strauss BL, Tavassoli FA. STAT 5a expression in various lesions of the breast. Virchows Arch. 2006;448(2):165–71.
Strauss BL, Bratthauer GL, Tavassoli FA. STAT 5a expression in the breast is maintained in secretory carcinoma, in contrast to other histologic types. Hum Pathol. 2006;37(5):586–92.
Sultan AS, Xie J, LeBaron MJ, Ealley EL, Nevalainen MT, Rui H. Stat5 promotes homotypic adhesion and inhibits invasive characteristics of human breast cancer cells. Oncogene. 2005;24(5):746–60.
Gutzman JH, Rugowski DE, Nikolai SE, Schuler LA. Stat5 activation inhibits prolactin-induced AP-1 activity: distinct prolactin-initiated signals in tumorigenesis dependent on cell context. Oncogene. 2007;26(43):6341–8.
Barash I. Stat5 in the mammary gland: controlling normal development and cancer. J Cell Physiol. 2006;209(2):305–13.
Nouhi Z, Chughtai N, Hartley S, Cocolakis E, Lebrun JJ, Ali S. Defining the role of prolactin as an invasion suppressor hormone in breast cancer cells. Cancer Res. 2006;66(3):1824–32.
Maus MV, Reilly SC, Clevenger CV. Prolactin as a chemoattractant for human breast carcinoma. Endocrinology. 1999;140(11):5447–50.
Manni A, Wright C, Davis G, Glenn J, Joehl R, Feil P. Promotion by prolactin of the growth of human breast neoplasms cultured in vitro in the soft agar clonogenic assay. Cancer Res. 1986;46(4 Pt 1):1669–72.
Yamashita H, Iwase H. The role of Stat5 in estrogen receptor-positive breast cancer. Breast Cancer 2002;9(4):312–8.
Yamashita H, Nishio M, Fujii Y, Iwase H. Dominant-negative Stat5 inhibits growth and induces apoptosis in T47D-derived tumors in nude mice. Cancer Sci. 2004;95(8):662–5.
Boerner JL, Biscardi JS, Silva CM, Parsons SJ. Transactivating agonists of the EGF receptor require Tyr 845 phosphorylation for induction of DNA synthesis. Mol Carcinog. 2005;44(4):262–73.
Weaver AM, Silva CM. Modulation of signal transducer and activator of transcription 5b activity in breast cancer cells by mutation of tyrosines within the transactivation domain. Mol Endocrinol. 2006;20(10):2392–405.
Weaver AM, Silva CM. Signal transducer and activator of transcription 5b (STAT5b): a new target of breast tumor kinase/protein tyrosine kinase 6 (Brk/PTK6). Breast Cancer Res. 2007;9(6):R79.
Boerner JL, Gibson MA, Fox EM, Posner ED, Parsons SJ, Silva CM, et al. Estrogen negatively regulates EGF-mediated STAT5 signaling in HER family receptor overexpressing breast cancer cells. Mol Endocrinol. 2005;19:2660–70.
Gass S, Harris J, Ormandy C, Brisken C. Using gene expression arrays to elucidate transcriptional profiles underlying prolactin function. J Mammary Gland Biol Neoplasia. 2003;8(3):269–85.
Clarkson RW, Boland MP, Kritikou EA, Lee JM, Freeman TC, Tiffen PG, et al. The genes induced by signal transducer and activators of transcription (STAT)3 and STAT5 in mammary epithelial cells define the roles of these STATs in mammary development. Mol Endocrinol. 2006;20(3):675–85.
LeBaron MJ, Xie J, Rui H. Evaluation of genome-wide chromatin library of Stat5 binding sites in human breast cancer. Mol Cancer. 2005;4(1):6.
Fantl V, Stamp G, Andrews A, Rosewell I, Dickson C. Mice lacking Cyclin D1 are small and show defects in eye and mammary gland development. Genes Dev. 1995;9(19):2364–72.
Sicinski P, Donaher JL, Parker SB, Li T, Fazeli A, Gardner H, et al. Cyclin D1 provides a link between development and oncogenesis in the retina and breast. Cell. 1995;82(4):621–30.
Brockman JL, Schroeder MD, Schuler LA. PRL activates the Cyclin D1 promoter via the Jak2/Stat pathway. Mol Endocrinol. 2002;16(4):774–84.
Brockman JL, Schuler LA. Prolactin signals via Stat5 and Oct-1 to the proximal Cyclin D1 promoter. Mol Cell Endocrinol. 2005;239(1–2):45–53.
Brisken C, Ayyannan A, Nguyen C, Heineman A, Reinhardt F, Tan J, et al. IGF-2 is a mediator of prolactin-induced morphogenesis in the breast. Dev Cell. 2002;3(6):877–87.
Ruchatz H, Coluccia AM, Stano P, Marchesi E, Gambacorti-Passerini C. Constitutive activation of Jak2 contributes to proliferation and resistance to apoptosis in NPM/ALK-transformed cells. Exp Hematol. 2003;31(4):309–15.
Slupianek A, Hoser G, Majsterek I, Bronisz A, Malecki M, Blasiak J, et al. Fusion tyrosine kinases induce drug resistance by stimulation of homology-dependent recombination repair, prolongation of G(2)/M phase, and protection from apoptosis. Mol Cell Biol. 2002;22(12):4189–201.
Baxter EJ, Scott LM, Campbell PJ, East C, Fourouclas N, Swanton S, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365(9464):1054–61.
James C, Ugo V, Le Couedic JP, Staerk J, Delhommeau F, Lacout C, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005;434(7037):1144–8.
Lee JW, Kim YG, Soung YH, Han KJ, Kim SY, Rhim HS, et al. The JAK2 V617F mutation in de novo acute myelogenous leukemias. Oncogene. 2006;25(9):1434–6.
Arnould C, Philippe C, Bourdon V, Gr goire MJ, Berger R, Jonveaux P. The signal transducer and activator of transcription STAT5b gene is a new partner of retinoic acid receptor alpha in acute promyelocytic-like leukaemia. Hum Mol Genet. 1999;8(9):1741–9.
Kofoed EM, Hwa V, Little B, Woods KA, Buckway CK, Tsubaki J, et al. Growth hormone insensitivity associated with a STAT5b mutation. N Engl J Med. 2003;349(12):1139–47.
Hwa V, Little B, Adiyaman P, Kofoed EM, Pratt KL, Ocal G, et al. Severe growth hormone insensitivity resulting from total absence of signal transducer and activator of transcription 5b. J Clin Endocrinol Metab. 2005;90(7):4260–6.
Acknowledgments
This work was supported, in part, by the Public Health Service grant DK52013 (to H.R) as well as grants CA101841 (to H.R and K.U.W.), and CA117930 (to K.U.W.) from the National Cancer Institute.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Wagner, KU., Rui, H. Jak2/Stat5 Signaling in Mammogenesis, Breast Cancer Initiation and Progression. J Mammary Gland Biol Neoplasia 13, 93–103 (2008). https://doi.org/10.1007/s10911-008-9062-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10911-008-9062-z