Abstract
This study examined maternal and reproductive health (MRH) access of Somali refugees in the U.S. across four access dimensions (willingness to seek care, gaining entry to the health system, seeing a primary provider and seeing a specialist). We conducted a cross-sectional survey of 427 Somali refugee reproductive-age women in Franklin County, Ohio. Following descriptive statistics of demographics, we conducted multivariate analyses to test associations between demographics and the four access dimensions. Most Somali refugee women were married (68%), attained primary education (92%), employed (64%) and were circumcised (82%). Young (OR 2.61, 95% CI 1.25–5.60), single (OR 1.78, 95% CI 1.15–2.78), and minors upon arrival (OR 2.36, 95% CI 1.44–3.90) were more willing to seek care. Lack of insurance, limited language fluency and being circumcised limited access to care across all dimensions. Barriers to access need to be systematically addressed. Deconstructing beliefs regarding health systems may improve access, especially among older Somali women.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the 1980 Refugee Act was passed, the United States (U.S.) has welcomed over three million refugees [1]. In the past decade, there has been an increasing proportion of refugees coming from Africa, with those from Somalia constituting the highest percentage (40%) [1]. Since 2002, 103,800 Somali refugees have resettled in the U.S., with states like Minnesota (16,596), Ohio (7981), Texas (7501), New York (6679) and Arizona (6030) receiving the majority [1]. While recent U.S. policy amendments have reduced the number of Somali refugees settling in the country [2], the state of persistent unrest in Somalia points to the possibility that more Somalis will be seeking refugee status—a situation described as “a crisis that can no longer be ignored” [3].
Refugees represent a distinct immigrant subgroup [4]. They face unique challenges in accessing healthcare after settling in a new country [5]. These challenges in access have been reported amongst Somali refugee women, more so in their quest to access critical maternal and reproductive health (MRH) across the entire continuum of care (prenatal care, intrapartum care, postnatal care and family planning) [6,7,8,9]. Access to MRH can significantly improve quality of life and in some instances be life-saving [10] and lack of it provides some explanation for the poorer pregnancy outcomes seen amongst Somali women post-migration compared to native women [11]. Compared to their male counterparts, Somali women are an especially vulnerable population as they face additional obstacles in maintaining their health and well-being in the host country, mostly due to their lower English proficiency due to reduced opportunities to access basic education while they grew up in Somalia [8, 12]. In addition, Somali women are faced with nefarious cultural practices such as female genital cutting (FGC), with 98% of the total female population having some type of FGC [13]. FGC is known to have severe short and long-term negative impacts on the physical and psychosocial health of women [14].
Despite the importance of MRH access, there is limited quantitative evidence describing MRH access needs among Somali refugee women. Access to healthcare is well recognized as a complex concept with “having access” (referring to a “willingness to utilize a health service if required”) different from “gaining access” (“the initiation into the process of utilizing a service”) [15]. The Institute of Medicine recognizes three access dimensions: gaining entry, getting access to care sites, and finding providers who can meet patient needs while sharing mutual trust with patients [16]. Building on both frameworks and relating this to the specific health needs of Somali women, we theorized that there are four access dimensions for MRH: willingness to seek care, gaining entry into the health system, attending to see a primary provider and seeing specialist if required. The aim of this study was to assess factors that influence their MRH access across these four dimensions of access.
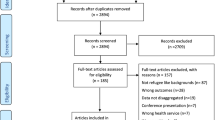
Methods
Participants
This study was part of a larger cross-sectional survey assessing access and health seeking behavior of Somali women across varying age groups resettling in Franklin, Ohio—a Midwestern state in the U.S. Somalis are the largest group of African-born refugees in the county. For this study, we highlighted women respondents of reproductive age (18–49 years), as MRH was most relevant to this group. Participants were recruited exclusively via word-of-mouth across social networks within the community using snowball sampling techniques. The sample size was estimated using STATA SE version 13.0 (StataCorp, College Station, Texas, USA), targeting a power of 80% and an α-error of 0.05 for the comparison of those who had a positive experience in terms of access versus those who did not. We used an 80% benchmark for positive access experience, aiming to achieve a sample size of 400.
Data Collection
All surveys were conducted in women’s homes between mid-May 2007 and January ending 2008. Surveys lasted 60–75 min and comprised of 69 questions covering six broad topics: (1) socio-demographics, (2) health status, (3) MRH access (4) MRH use, (5) experiences with providers, and (6) self-reported female genital Cutting (FGC) status and type using the RAINBO FGC full color quick reference chart [17]. However, the focus of this paper is on access to MRH (Topic 3). Questions examined our four theorized access dimensions: willingness to seek care; gaining entry into the health system; access to primary provider; and access to specialist care (urogynecologists or perinatologists) [15, 16], in the year preceding the survey. The instrument was translated into Somali. Accuracy and face validity of the translated versions were tested in discussions with volunteer respondents and certified Somali medical interpreters who reviewed the content to ensure cross-cultural equivalence [18]. We leveraged a community-based participatory research partnership to mobilize community support wherein bilingual and highly respected community members were trained as community mobilizers/surveyors [19]. Data collected was entered into a spreadsheet, error-checked and cleaned.
Data Analysis
Standard descriptive statistics were used to characterize the study population using various independent variables [age, marital status, education, poverty index, length of time lived in the U.S (≤ 4 years or > 4 years)], age category at resettlement (minor or adult), insurance status, FGC status, FGC type (Type I–III) and English language literacy. Specific independent variables were re-coded. Age was analyzed as a categorical variable (18–19 years, 20–34 years and 35–49 years), based on the well-established risk-profile of reproductive age-group, with women age 18–19 years and > 35 years known as being high-risk pregnancies. For poverty index, we used the U.S. government poverty thresholds [20]. To classify respondents into above or below the poverty threshold, household size and annual family income were used. Classification of respondents into those who have resided in the U.S. for ≤ 4 years or > 4 years was based on previously published evidence on the significance of the four-year mark in refugee acculturation [21].
We used cross-tabulations and bivariate analysis (Chi square test) to understand the nature of association between the dependent variable (access to care) and the different independent variables. The Chi square statistic and p-value allowed us to verify any significant associations between the dependent variables and the independent variables, based on a p < 0.05 statistical significance level. Subsequently, a multivariate analysis using a forward selection was conducted to demonstrate the strength of association between the dependent variable and the various independent variables for which the bivariate analysis showed to be significant. Results were presented with odds ratio, 95% confidence intervals (CI) and p-values. All statistical analyses were conducted with STATA SE 13.0 (StataCorp, College Station, Texas, USA). Significant associations are presented in a tabular format. In cases in which respondents did not respond to specific questions, such missing data were excluded from the analysis.
Results
Of the 515 women recruited, 427 women met our age inclusion criterion for the study (18–49 years). The mean age of the entire sample was 31 years and 1 month. 290 of 426 (68%) women had been married at some point in time with 233 (55%) stating that they were presently living with their partners. 390 (92%) women had attained at least primary education while 32 (8%) women had received no formal education at all. 262 of 408 respondents (64%) were employed. 167 (53%) of 315 women were classified as living in households below the poverty threshold. 111 (26%) had no insurance at all while 139 (33%) had lived four or less years in the U.S. 108 (25%) of those surveyed arrived in the U.S. as minors. 152 (36%) of 421 respondents classified themselves as being either not able to speak well or not able to speak at all in English language. 336 (82%) of 409 respondents self-reported being previously circumcised and based on their self-described FGC status, 187 (58%) of 322 women self-reported undergoing the most severe form of FGC Type III (Table 1).
Respondents cited not having insurance as the most frequent reason for having to postpone care [81% (n = 121)] (Fig. 1) and difficulties experienced in seeing a specialist [32% (n = 44)] (Fig. 2). For those with insurance needing to see a specialist, 34 (24%) did not have their specialist care approved (Fig. 2).
Reasons for postponement of care. The figure shows frequency of reasons that Somali refugees gave for having to postpone care. Of 149 respondents, 121 (81%) did not have insurance cover, 16 (11%) did not have the time, 5 (3%) felt the wait was too long, 3 (2%) felt too lazy to travel (2%), 2 (1%) no transportation and 2 (1%) do not enjoy seeing the doctor
Reasons for difficulty in accessing a specialist. The figure shows frequency of reasons that Somali refugees gave for the difficulty they experienced in seeing a specialist. Of 139 respondents, 44 (32%) did not have insurance cover, 34 (24%) had insurance that did not approve care, 27 (19%) felt the wait was too long, 25 (18%) could not get a referral and 9 (6%) could not find a specialist
Teenage Somali refugee women age 18–19 years were almost three (CI 1.25–5.61) times more willing to seek care than Somali refugee women age 35–49 years. Similarly, those who arrived in the U.S. as minors were about two and half (CI 1.44–3.90) times more willing to seek care than those who arrived as adults. In terms of marital status, those who were single and had never been married before were about two (CI 1.15–2.78) times more willing to seek care than those who were married (Table 2).
Across all four access dimensions, those with public or private insurance were at least two times more willing to seek care [public (CI 2.56–7.65) and private (CI 2.03–4.38)], three times more likely to gain entry into the health system [public (CI 1.85–5.26) and private (CI 2.09–9.36)], and three times less likely to have difficulty in seeing a primary provider [public (CI 0.05–0.30) and private (CI 0.20–0.05)] or experience difficulty in seeing a specialist [public (CI 1.76–7.67) and private (CI 1.30–7.93)] compared to those without insurance (Table 2).
The odds of Somali refugee women who were not able to speak the English language well, being willing to seek care was almost 80% (CI 0.12–0.43) less than those who were able to speak very well. Those who were not able to speak well or not able to speak at all had odds of about 60% (CI 0.17–0.78) and were 80% (CI 0.06–0.90) less likely to gain entry into the health system respectively compared to those who were to speak very well. Those who were not able to speak well or not able to speak at all were three (CI 1.05–11.19) and five (CI 1.23–24.90) times less likely respectively to have access to a primary care provider compared to those who were able to speak very well. Those who were not able to speak well or not able to speak at all had odds of about 60% (CI 0.18–0.86) and 70% (CI 0.07–0.99) less likely to see a specialist if required, respectively, compared to those who were able to speak very well (Table 2).
The odds of Somali refugee women with FGC being willing to seek care was about 50% (CI 0.30–0.94) less than those who had never been circumcised. Somali refugee women with the more severe FGC types felt even less willing [Type II (CI 0.17–0.83) and Type III (CI 0.32–0.98)], had more difficulty in gaining entry [Type II (CI 0.13–0.72) and Type III (CI 0.18–0.70)] and in accessing a primary provider [Type II (CI 1.03–14.42) and Type III (CI 1.90–17.07)] compared to those who had Type 1 FGC type (Table 2).
Discussion
In this cross-sectional survey, we assessed factors that influenced MRH access of U.S. based Somali refugee women across four theorized access dimensions (willingness to seek care, entering the health system, seeing a primary provider and seeing specialist if needed). Similar to the general population, English language literacy as well as having public or private insurance influenced access to care. However, we also found significant factors unique to the Somali refugee population such as having FGC and being minors influencing access to care.
We found a strong association between having public or private insurance and access to care across all four access dimensions. Our findings are consistent with what has been reported in the literature on effect of insurance on access [22, 23]. While many developed countries have explored ways to guarantee equity in access across various sub-populations, the U.S. still lags behind resulting in profound health disparities, particularly among vulnerable groups such as refugee populations [22]. As in our study, refugees in another conducted in San Diego County, U.S. viewed costs associated with insurance as their principal barrier to accessing healthcare [23].
Consistent with existing evidence [8, 24,25,26,27], we found language fluency to be a critical factor for access of Somali women to MRH services. In our study, about two-fifth of the sample could speak little or no English. Another study reported closer to half the population [28]. Those with little to no language competency struggled to gain entry into the system. In Australia and the United Kingdom, where phone calls were used to book appointments by refugees, lack of confidence in speaking English for bookings was deemed a barrier to accessing healthcare [24, 25]. While considerable focus has been placed on providing interpreters to bridge the discourse between refugee patients and providers, our findings suggests the “bridge” needs to be established before the women engages with the health system. This suggests a role for ‘Cultural Health Navigators’, as in Arizona, U.S [8]. or ‘refugee mentors’, as used in Melbourne, Australia [25], who are certified medical interpreters and members of the refugee community, and can help women at initial point of entry into the health system.
In our study, we found that women who had been cut previously had almost 50% less odds of being willing to seek MRH. FGC status had no association with the remainder of the access spectrum (gaining entry/seeing primary provider/seeing specialist). However, in addition to its effect on willingness to seek care, FGC type had a significant association with gaining entry and seeing a primary provider. It appears having any form of FGC affected women’s willingness to engage with the health system. Once committed to engaging, those who had more severe FGC types experienced greater challenges with gaining entry and difficulty in accessing a primary provider. Somali refugee women with FGC who have resettled in many Western countries, where the practice is not native have lamented about how they were perceived and managed by health care providers (HCPs) in pregnancy and labor [29, 30]. While we did not assess provider perceptions in our study, such provider attitudes may have affected care access of Somali refugee women [30].
We found that younger and single Somali refugee women were more willing to seek care compared to the older and married women. Similarly, those who resettled in the U.S. as minors were more willing to seek MRH. It is possible that the general negative perceptions regarding health systems in developed countries held by Somali refugee women is much more ingrained in the older and married women. These perceptions have resulted in divergent expectations between HCPs and patients regarding treatment and healthcare interactions [31] and contributed to a diminished willingness to seek care [23]. Some of the older and married women are also more likely to have “experienced the health system” already and have been disconcerted because of stereotyping, implicit bias and racism from HCPs, and a lack of understanding from HCPs on their own cultural differences [26]. Distrust and fears such as those associated with cesarean sections are also crystallized amongst the older age-group [32,33,34,35]. In other Western country settings, Somali refugee women have described a feeling of their presence within the system being ‘pathologized’, as they are often seen as intrusive [24]. Evidence suggests such pathologized presence leads to ‘minoritization’ (setting apart) and ultimately leads to hindering access to healthcare [36, 37]. It is also important to consider the role of her husband and how his opinion may impact her own agency to make such care seeking decisions [38].
New Contribution to the Literature
To the best of our knowledge, this is the first quantitative assessment of MRH access across all dimensions among Somali refugee women that involved a relatively large sample size. Being a community-based survey, it ensured that Somali refugees who would rather not engage with the health system were not systematically excluded. Our findings show that language fluency, insurance, and FGC influence access to care across all dimensions. Younger, single, Somali refugee women and those who resettled in the U.S. as minors are more willing to seek MRH compared to the older and married women.
Study Limitations
There are limitations to consider when reviewing our findings. Data was based on self-reporting. However, we sought clarifications from the women to ascertain their responses. Specifically, for FGC status and type, the woman may not be able to accurately describe the type of her cutting. To minimize this, we used visual aids [19], helping women to get a better sense of the FGC type in describing it. In this study also, we have based their experience of care on the year preceding the survey, while this in itself may be viewed as a strength, especially as it limits recall bias, responses may have been different if we looked at broader time-periods.
Implications for Future Research and Policy
There is a case to further research the association we found between age, singleness and willingness to seek care, using even larger sample size of Somali refugees in other places of resettlement. As regards policy, innovative approaches to aid refugee women in financing critical MRH would significantly help with breaking barriers to accessing care. More emphasis needs to be placed on deconstructing perceptions of Somali refugees regarding health systems, especially amongst the older women as this may be limiting their willingness to seek care. When refugee women do engage with the system, our findings support the general assertion that they should have bilingual/bicultural staff who can bridge the language and cultural divide. However, such engagements need to be implemented at the community level, before the women even make their journey to engage health systems, in order to increase their willingness to seek care. While community reorientation efforts should be done across the board, our findings suggest a case for placing even more emphasis on older and married Somali refugee women who have had more time to imbibe their cultural beliefs and perceptions of the health system.
Conclusion
Amongst vulnerable Somali refugee women, those who are uninsured, not fluent in the English language and have the most severe FGC types are even more vulnerable. If the aim remains to uphold the 1951 Refugee Convention which states that “refugees should enjoy access to health services equivalent to that of the host population” [39], then cultural, structural and functional barriers that limit access to care amongst Somali refugee women need to be excluded, whether they are perceived or real.
References
Refugee Processing Center. Admissions & Arrivals [Internet]. Reports. 2018. http://www.wrapsnet.org/admissions-and-arrivals/. Accessed 14 April 2018.
The White House. Executive Order Protecting the Nation from Foreign Terrorist Entry into the United States [Internet]. United States of America; 2017. https://www.whitehouse.gov/presidential-actions/executive-order-protecting-nation-foreign-terrorist-entry-united-states/.
Davidson PM, Mbaka-Mouyeme F. The refugee crisis: we cannot ignore this for much longer. Health Care Women Int. 2016;37(9):945–5.
Department Homeland Security. United States Department of Homeland Security. Washington, DC; 2010.
Caulford P, Vali Y. Providing health care to medically uninsured immigrants and refugees. Can Med Assoc J. 2006;174(9):1253–4.
Keygnaert I, Vettenburg N, Temmerman M. Hidden violence is silent rape: sexual and gender-based violence in refugees, asylum seekers and undocumented migrants in Belgium and the Netherlands. Cult Health Sex. 2012;14(5):505–20.
Aptekman M, Rashid M, Wright V, Dunn S. Unmet contraceptive needs among refugees. Can Fam Physician. 2014;60(12):e613–9.
Banke-Thomas A, Gieszl S, Nizigiyimana J, Johnson-Agbakwu C. Experiences of refugee women in accessing and utilizing a refugee-focused prenatal clinic in the United States: a mixed methods study. Glob Women’s Health. 2017;1(1):14–20.
Khanlou N, Haque N, Skinner A, Mantini A, Kurtz Landy C. Scoping review on maternal health among immigrant and refugee women in Canada: prenatal, intrapartum, and postnatal care. J Pregnancy. 2017;2017:1–14.
WHO. Packages of interventions for family planning, safe abortion care, maternal, newborn and child health. Geneva: WHO; 2010.
Small R, Gagnon A, Gissler M, Zeitlin J, Bennis M, Glazier R, et al. Somali women and their pregnancy outcomes postmigration: data from six receiving countries. BJOG. 2008;115(13):1630–40.
Deacon Z, Sullivan C. Responding to the complex and gendered needs of refugee women. Affilia. 2009;24(3):272–84.
UNICEF. Female genital mutilation/cutting: a statistical overview and exploration of the dynamics of change [Internet]. New York; 2013. pp. 1–194. http://data.unicef.org/wp-content/uploads/2015/12/FGMC_Lo_res_Final_26.pdf.
WHO. Care of girls and women living with female genital mutilation: a clinical handbook [Internet]. Geneva, Switzerland: World Health Organization; 2018. p. 1–458. http://apps.who.int/iris/bitstream/handle/10665/272429/9789241513913-eng.pdf?ua=1.
Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson B, Beech R, et al. What does “access to health care” mean? J Health Serv Res Policy. 2002;7(3):186–8.
Institute of Medicine. Access to Health Care in America [Internet]. Millman M, editor. Access to Health Care in America. Washington DC: National Academies Press (US); 1993. pp. 1–240. http://www.ncbi.nlm.nih.gov/pubmed/25144064. Accessed 6 May 2018.
Toubia N. Female genital mutilation: a full color quick reference chart. New York: Research, action and information network for bodily integrity of women (RAINBO); 1999.
Lee C-C, Li D, Arai S, Puntillo K. Ensuring cross-cultural equivalence in translation of research consents and clinical documents: a systematic process for translating English to Chinese. J Transcult Nurs. 2009;20(1):77–82.
Johnson CE, Ali SA, Shipp MP-L. Building community-based participatory research partnerships with a somali refugee community. Am J Prev Med. 2009;37(6S1):230–6.
Department of Health and Human Services. U.S. federal poverty guidelines used to determine financial eligibility for certain federal programs [Internet]. Poverty guidelines. 2018. https://aspe.hhs.gov/poverty-guidelines. Accessed 20 Nov 2017
Gele AA, Johansen EB, Sundby J. When female circumcision comes to the West: attitudes toward the practice among Somali Immigrants in Oslo. BMC Public Health. 2012;12:697.
Kim W, Keefe RH. Barriers to healthcare among Asian Americans. Soc Work Public Health. 2010;25(3–4):286–95.
Morris MD, Popper ST, Rodwell TC, Brodine SK, Brouwer KC. Healthcare barriers of refugees post-resettlement. J Community Health. 2009;34(6):529–38.
Fang ML, Sixsmith J, Lawthom R, Mountian I, Shahrin A. Experiencing “pathologized presence and normalized absence”; understanding health related experiences and access to health care among Iraqi and Somali asylum seekers, refugees and persons without legal status. BMC Public Health. 2015;15:923.
Riggs E, Davis E, Gibbs L, Block K, Szwarc J, Casey S, et al. Accessing maternal and child health services in Melbourne, Australia: reflections from refugee families and service providers. BMC Health Serv Res. 2012;12:117.
Bulman KH, McCourt C. Somali refugee women’s experiences of maternity care in west London: a case study. Crit Public Health. 2002;12(4):365–80.
Kita S, Minatani M, Hikita N, Matsuzaki M, Shiraishi M, Haruna M. A systematic review of the physical, mental, social, and economic problems of immigrant women in the perinatal period in Japan. J Immigr Minor Health. 2015;17(6):1863–81.
Yoong W, Kolhe S, Karoshi M, Ullah M, Nauta M. The obstetric performance of United Kingdom asylum seekers from Somalia: a case-control study and literature review. Int J Fertil Womens Med. 2005;50(4):175–9.
Hamid A, Grace KT, Warren N. A Meta-synthesis of the birth experiences of African immigrant women affected by female genital cutting. J Midwifery Womens Health. 2018;63(2):185–95.
Lazar JN, Johnson-Agbakwu CE, Davis OI, Shipp MP-L. Providers’ perceptions of challenges in obstetrical care for somali women. Obstet Gynecol Int. 2013;2013:149640.
Pavlish CL, Noor S, Brandt J. Somali immigrant women and the American health care system: discordant beliefs, divergent expectations, and silent worries. Soc Sci Med. 2010;71(2):353–61.
Brown E, Carroll J, Fogarty C, Holt C. “They get a c-section… they gonna die”: Somali women’s fears of obstetrical interventions in the United States. J Transcult Nurs. 2010;21(3):220–7.
Carroll J, Epstein R, Fiscella K, Volpe E, Diaz K, Omar S. Knowledge and beliefs about health promotion and preventive health care among Somali women in the United States. Health Care Women Int. 2007;28(4):360–80.
Herrel N, Olevitch L, DuBois DK, Terry P, Thorp D, Kind E, et al. Somali refugee women speak out about their needs for care during pregnancy and delivery. J Midwifery Womens Health. 2004;49(4):345–9.
Small R, Roth C, Raval M, Shafiei T, Korfker D, Heaman M, et al. Immigrant and non-immigrant women’s experiences of maternity care: a systematic and comparative review of studies in five countries. BMC Pregnancy Childbirth. 2014;14:152.
Grove NJ, Zwi AB. Our health and theirs: Forced migration, othering, and public health. Soc Sci Med. 2006;62(8):1931–42.
Johnson JL, Bottorff JL, Browne AJ, Grewal S, Hilton BA, Clarke H. Othering and being othered in the context of health care services. Health Commun. 2004;16(2):255–71.
Johnson-Agbakwu CE, Helm T, Killawi A, Padela AI. Perceptions of obstetrical interventions and female genital cutting: insights of men in a Somali refugee community. Ethn Health. 2014;19(4):440–57.
UNHCR. Convention and protocol relating to the status of refugees. Geneva: UNHCR 2010.
Acknowledgements
This study was funded by the Robert Wood Johnson Foundation Clinical Scholars Program and the University of Michigan, Department of Obstetrics & Gynecology. Data analysis and manuscript development was supported by the Research Education and Training Core (RETC) of the Southwest Interdisciplinary Research Center (SIRC) at Arizona State University and the Early Career Faculty Fellowship from the National Institute on Minority Health and Health Disparities of the National Institutes of Health (NIMHD/NIH), award P20 MD002316 (F. Marsiglia, P.I.). We would like to thank Dr. Lubayna Fawcett for providing technical support, data entry error checking and data cleaning. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMHD or the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
Ethics approval for this study was obtained from the ethics committee of the University of Michigan Institutional Review Board (IRB) (HUM00009502).
Informed Consent
Participants’ written informed consent was obtained using an informed consent form, which had been reviewed and approved by the IRB. For those participants who could not read and write, the enumerators read out the research information sheet and the informed consent form, and their thumbprint was taken as proof of consent. All participation was voluntary, and participants were allowed to exit the survey if they desired.
Rights and permissions
About this article
Cite this article
Banke-Thomas, A., Agbemenu, K. & Johnson-Agbakwu, C. Factors Associated with Access to Maternal and Reproductive Health Care among Somali Refugee Women Resettled in Ohio, United States: A Cross-Sectional Survey. J Immigrant Minority Health 21, 946–953 (2019). https://doi.org/10.1007/s10903-018-0824-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-018-0824-4