Abstract
We examine changes in health insurance coverage and access to and utilization of health care before and after the national implementation of the Patient Protection and Affordable Care Act (ACA) among the U.S. adult immigrant population. Data from the 2011–2016 National Health Interview Survey are used to compare adult respondents in 2011–2013 (before the ACA implementation) and 2014–2016 (after the ACA implementation). Multivariable logistic regression analyses are used to compare changes over time. This study shows that the ACA has closed the coverage gap that previously existed between U.S. citizens and non-citizen immigrants. We find that naturalized citizens, non-citizens with more than 5 years of U.S. residency, and non-citizens with 5 years or less of U.S. residency reduced their probability of being uninsured by 5.81, 9.13, and 8.23%, respectively, in the first 3 years of the ACA. Improvements in other measures of access and utilization were also observed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Early evidence from the Patient Protection and Affordable Care Act (ACA) shows that uninsured rates have declined from 16.6 to 10.4% between 2013 and 2016 [1, 2]. Various studies have linked the different ACA provisions with short-term improvements in access to care, prescription drug utilization, health outcomes, and health care disparities by race and ethnicity [3,4,5,6]. Studies have also documented that changes in health insurance coverage are strongly associated with improved health care access and primary care utilization [7,8,9,10]. As a result of the 2016 election, both the executive and legislative branches have promised to repeal and replace the ACA, and the Senate has promoted legislation to repeal the individual health insurance mandate. To that end, it is important to understand what impact the ACA has had on vulnerable populations, as they are likely to be disproportionally affected by changes to the law.
Under the ACA, U.S.-born individuals, naturalized citizens, and legally authorized immigrants have similar entitlements. U.S.-born and naturalized citizens are entitled to receive Medicaid coverage up to 138% of the federal poverty level (FPL) in states that implemented the expansion. Those with incomes between 100 and 400% of the FPL are eligible to receive subsidies in the private health insurance exchanges (HIE).
Non-citizen lawfully present immigrants (e.g., “green card” holders and other visa categories) face a 5-year waiting period to enroll in Medicaid. Some states have chosen to eliminate the 5-year wait through state financed coverage to adults, pregnant women, and children or for those who need specific health services [11]. Individuals with incomes below 100% of the FPL who are ineligible for Medicaid based on immigration status are entitled to purchase coverage from the HIE and receive subsidies.
All other non-citizen lawfully present immigrants are entitled to purchase health insurance coverage in the HIE and receive subsidies in the same terms as U.S.-born and naturalized citizens [12]. Uninsured U.S.-born, naturalized citizens, and non-citizen lawfully present immigrants with incomes above 400% of the FPL are eligible to purchase health insurance coverage without subsidies in the HIE [11]. Undocumented immigrants are excluded from all of the ACA’s provisions [13, 14]. While undocumented immigrants are represented in our study, information about documentation status is unavailable in the National Health Interview Survey (NHIS).
To our knowledge, this is one of the first studies to analyze access to and utilization of health care specifically among U.S. immigrants before and after the national implementation of the ACA using a nationally representative survey. We also explore how the main predictors associated with access to and utilization of health care changed after the implementation of the ACA.
Conceptual Framework
The conceptual framework for this study is the behavioral model of health services utilization developed by Aday and Andersen and Andersen [15, 16]. This model postulates that health care access and utilization are determined by predisposing, enabling and need factors. Our analyses use this framework to guide model specification and variable selection. The predisposing factors in our models include characteristics such as age, gender, race and ethnicity, marital status, education, and language. Enabling factors include health insurance coverage, income, employment status and region of residence. Need factors are captured by self-reported health status and poverty status [17,18,19].
In this study, we hypothesize that health insurance coverage would increase among immigrants, due to the ACA health insurance mandate and related programs. The ACA made health insurance more affordable for lawfully stayed immigrants through the Medicaid expansion and the available subsidies at the state and federal health insurance exchanges [6]. At the same time, lacking health insurance became costly due to the penalties associated with the health insurance mandate.
In the case of access to and utilization of health care, we hypothesize that they improved or remained unchanged after the ACA was implemented. Previous research shows that immigrants are self-selected, which partly explains the existence of a “healthy immigrant” effect on health care access and utilization [20,21,22]. We hypothesize that the healthy immigrant effect can partly explain reduced health care utilization among immigrants, particularly in the early years of U.S. residence. As immigrants acculturate, age and become more familiar with the U.S. health system, differences between the U.S.-born population and immigrants should decrease. Immigrants who have been in the U.S. for a long period will have similar health care access and utilization patterns of the U.S.-born population, as previous research has concluded [23, 24].
Methods
Data
This study uses a repeated cross sectional design that pools data from the 2011–2016 National Health Interview Survey (NHIS), a nationally representative survey of the civilian, non-institutionalized U.S. population [25]. This survey reports information on a broad range of health care topics and socioeconomic and demographic characteristics of survey respondents. Our total sample size is 113,439 adults 18–64 years of age. The weighted sample size corresponds to 48,839,629 adults nationwide.
Insurance Coverage and Access to and Utilization of Care
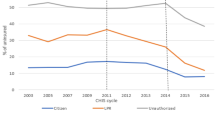
Survey questions used as outcome variables are the share of immigrants who reported health insurance coverage, if they experienced any delay when trying to access health care, if they forgone treatment due to cost, if they have used emergency department services, and if they reported a physician visit (Fig. 1; Table 1).

Source 2011–2016 National Health Interview Survey. Notes: “Before” corresponds to mean values for years 2011–2013, period before the implementation of the ACA individual health insurance mandate. “After” corresponds to mean values for years 2014–2016, period after the implementation of the ACA individual health insurance mandate. Vertical axis corresponds to percentage point changes. Horizontal axis describes the study variables
Health insurance coverage and access to and utilization of care by U.S. Immigration status before and after the ACA Implementation.
Before and After Comparison
We created variables of survey years as main explanatory variables to compare insurance coverage and access to and utilization of health care measures before and after the implementation of the ACA in 2014. In accordance with our pooled cross-sectional design, variable years for 2011, 2012, and 2013 correspond to the period before the national implementation of the ACA. The variable years for 2014, 2015 and 2016 correspond to the years after the implementation of the ACA. This empirical framework has been used previously in studies that have investigated differences in insurance coverage and access to and utilization of health care before and after the implementation of the ACA [3, 26].
Citizenship and Time of U.S. Residence
We constructed three mutually exclusive dichotomous measures of citizenship and time of U.S. residence based on immigrant eligibility rules under the Affordable Care Act: U.S.-born citizen, naturalized U.S. citizen, non-citizen immigrant with 5 years or less of U.S. residence (≤ 5 years), and non-citizen immigrant with more than 5 years residence (> 5 years), which coincide with the 5 year waiting period that non-citizen lawfully present immigrants (e.g. “green card” holders and other visa categories) need to observe before they become eligible for Medicaid in states that have expanded this program. Besides the 5-year waiting period for Medicaid coverage, non-citizen lawfully present immigrants are eligible to access Medicaid and the HIE in equal terms as U.S.-born or naturalized citizens.
The ACA does not make any distinctions between U.S.-born and naturalized citizens in terms of eligibility or responsibilities. Thus, these populations are analyzed as single categories. Consequently, U.S.-born citizens (N = 90,513), naturalized U.S. citizens (N = 10,691), non-citizen immigrants with 5 years or less of U.S. residence (N = 2,391), and non-citizen immigrants with more than 5 years residence (N = 9844) are the groups of focus in our study. Undocumented immigrants are represented in our study under the non-citizen immigrant categories. Our study, however, does not distinguish between lawful non-citizen immigrants and undocumented immigrants since NHIS lacks an identifier for documentation status.
Other Covariates
Our study included additional co-variables that have been identified in prior studies to affect insurance coverage and health care access and utilization, including socioeconomic and demographic variables [19, 23]. The selection of co-variables in our models is consistent with our conceptual framework, and they include sex, marital status, race and ethnicity, age, education, income, self-reported health status, Spanish interview, and region of residence.
Statistical Analyses
Initial analyses provided summary statistics for each outcome measure and showed how insurance coverage and access to and utilization of health care changed from 2011 to 2016 (Fig. 1). Multivariable logistic regression analyses were used to compare the change in insurance rates and access to and utilization of care before (reference category) and after the national implementation of the ACA. After we performed the goodness of fit test for our models (i.e. svylogitfof), we ran separate regression analyses for the outcome measures including all co-variables in each model (Table 1).
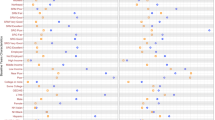
A comparison of means analyses compared the main study outcome measures before and after the implementation of the ACA for all population categories. We summarized the main outcomes of the data analyses using marginal effects to ease interpretation of the main findings (Table 2; Fig. 2). Marginal effects were first estimated using the values of year indicator for each individual. Then, the results for each individual were averaged to estimate the marginal effect, as recommended by Karaca-Mandic [27]. The statistical analyses included sampling weights to estimate nationally representative results. We used Stata 13 and perform -svy- commands for all statistical analyses.

Source 2011–2016 National Health Interview Survey. Notes: Marginal effect shows percentage changes in 2014–2016 compared to the 2011–2014 period. Vertical axis corresponds to percentage point changes. Horizontal axis describes the U.S. immigrant categories
Likelihood of Being Uninsured by U.S. Immigration Status After the ACA Implementation.
Results
Figure 1 shows mean differences in health insurance coverage and access to care before (2011–2013) and after (2014–2016) the implementation of the ACA. Uninsured rates across all categories declined after its implementation. The drop of the mean uninsured rates was 5% points for U.S.-born citizens, 6% points for naturalized U.S. citizens, 8% points for non-citizens with more than 5 years of U.S. residence, and 9% points for non-citizens with 5 years or less of U.S. residence.
Similar trends were observed for two of our outcome measures. Individuals reporting that they delayed care diminished by 3% points among U.S. born citizens, 4% points for naturalized U.S. citizens, 3% points for non-citizens with more than 5 years of U.S. residence, and 5% points for non-citizens with 5 years or less of U.S. residence. Approximately 2% of U.S.-born and naturalized citizens and immigrants with more than 5 years of U.S. residence forwent care after the ACA implementation, while the corresponding figure for non-citizens with 5 years or less of U.S. residence was 4%.
The before-after mean difference of adults reporting emergency department (ED) utilization was relatively constant for all categories, with the exception of non-citizen adults with 5 years or less of U.S. residence, who had a 2% increase after the implementation of the ACA. The share of adults reporting at least one physician visit in the previous year increased 2% for U.S.-born individuals, 3% for naturalized U.S. citizens, 4% for non-citizens with more than 5 years of U.S. residence, and 2% for non-citizens with 5 years or less of U.S. residence.
Table 1 shows the results of the multivariable logistic regressions that include socioeconomic and demographic characteristics. After controlling for all co-variables, the ACA implementation measure (after ACA) shows that adults had lower odds of being uninsured (OR = 0.62, p < 0.001), delaying (OR = 0.76, p < 0.001) and forgoing care (OR = 0.76, p < 0.001) and had higher odds of reporting a physician visit in the previous year (OR = 1.10, p < 0.001).
When compared to U.S.-born citizens, naturalized U.S. citizens had higher odds of being uninsured (OR = 2.25, p < 0.001) and lower odds of using the ED (OR = 0.63, p < 0.001) and having a physician visit in the previous year (OR = 0.60, p < 0.001). Non-citizens with more than 5 years of U.S. residency had higher odds of being uninsured (OR = 3.02, p < 0.001) and of forgoing care (OR = 1.14, p = 0.02) and lower odds of using the ED (OR = 0.59, p < 0.001) and of having a physician visit in the previous year (OR = 0.66, p < 0.001). Non-citizens with 5 years or less of U.S. residency had higher odds of being uninsured (OR = 1.16, p < 0.001) and lower odds of using the ED (OR = 0.82, p < 0.001).
Socioeconomic and demographic characteristics show that Latinos, adults ages 25–64 years of age, those from households 100–200% of the FPL, those reporting poor, fair, good and very good health status, those responding to the questionnaire in Spanish, those living in rural areas, and those living in the Midwest, the South and the West had significantly higher odds of being uninsured compared to the reference categories. Females, married individuals, and those with a college degree or more had statistically significant lower odds of being uninsured after the implementation of the ACA compared to the reference categories.
Table 2 and Fig. 2 show the results of the multivariable logistic regressions using marginal effects comparing individuals by citizenship/nativity status before and after the implementation of the ACA. U.S.-born individuals were 4.47% less likely to be uninsured (p < 0.001), 2.44% less likely to delay care (p < 0.001) and 1.81% less likely to forego care (p < 0.001), after controlling for all co-variables (not shown in the exhibit but available upon request). They were 0.02% more likely to report a physician visit (p < 0.001) in the previous year. U.S. naturalized citizens were 5.81% less likely to be uninsured (p < 0.001), 3.92% less likely to delay care (p < 0.001) and 2.21% less likely to forego care (p < 0.001). They were 0.03% more likely to report a physician visit (p < 0.001) in the previous year.
Non-citizens with more than 5 years of U.S. residency reported that they were 9.13% less likely to be uninsured (p < 0.001). Non-citizens with 5 years or less of U.S. residency were 8.23% less likely to be uninsured (p < 0.001) and 0.04% more likely to report a physician visit (p < 0.004) in the previous year. Utilization differences of the ED before and after the implementation of the ACA were not statistically significant for all comparison categories.
Discussion and policy implications
After its approval in 2010, access to ACA-related health insurance programs were restricted for some U.S. immigrants based on their time of U.S. residency and legal authorization status [17, 18]. Our study shows that, in spite of these restrictions, uninsured rates for U.S. immigrants were reduced significantly. The coverage gap that previously divided non-citizen U.S. immigrants with naturalized U.S. citizens and U.S.-born individuals was shortened in the first 3 years of the national implementation of the ACA. These findings are consistent with our hypothesis that health insurance rates would increase among immigrants because of increased health insurance affordability through the Medicaid expansion and the subsidies available at the state and federal health insurance exchanges. At the same time, lawfully present immigrants were incentivized to seek health insurance coverage due to the penalties associated with the ACA health insurance mandate. The penalties associated with the mandate increased the cost of being uninsured.
Measures of access to health care also showed some improvement. U.S.-born individuals and naturalized U.S citizens were less likely to forgo or delay care than immigrants with less than 5 years of residency. These two populations were also slightly more likely to report a physician visit in the previous year. These findings are consistent with the hypothesis that access to and utilization of health care among immigrants would improve or remain unchanged after the ACA. Prior research that has investigated the healthy immigrant effect partly explains reduced health care access and utilization among immigrants due to immigrant self-selection [22, 24]. Recently arrived immigrants are more likely to be healthy compared to the average population. Over time, immigrants acculturate, learn how to navigate the U.S. health system and their health status starts to resemble that of the average population. Consequently, longer-stayed immigrants would be more likely to seek care because they are perhaps in greater need of using health care, and they have learned how to use the health system. Increased access to and utilization of health care among longer-stayed immigrants supports this hypothesis.
Improvements in access to care, however, could have potentially been better for non-citizens with more than a 5-year residency if it were possible to separate immigrants by documentation status. As mentioned above, even though undocumented immigrants were accounted in our analysis, the lack of a documentation status identifier in NHIS did not allow us to distinguish between lawfully present and undocumented immigrants. Since approximately 85% of undocumented immigrants in the U.S. would be accounted for in this cohort, separating the analyses by documentation status would have shown a larger improvement for eligible immigrants who have lived in the U.S. for more than 5 years.
Non-citizens with less than 5 years of U.S. residency reported fewer improvements in access to care, but their overall insurance rate increased substantially. This change could be due to the ACA eligibility among non-citizen lawfully present immigrants, who are eligible for ACA benefits. However, lower coverage levels compared to longer-stayed immigrants could be due to both the 5-year waiting period for Medicaid eligibility and the difference in socio-demographic characteristics. These findings are important considering that approximately 15% of undocumented immigrants in the U.S. have less than 5 years of residency [28].
The lack of significant differences in delayed and forgone care and in reporting a physician visit after the ACA implementation among non-citizen immigrants could be related to the hypothesis of reduce demand for health care from recently arrived immigrants due to the healthy immigrant effect, as discussed above. Alternatively, it can be related to the type of care that immigrants use and the supply of physicians in the areas where immigrants settle. Non-citizens are likely to cluster in geographic areas with more physician shortages. These immigrants could rely more on non-physicians (e.g. advanced practice clinicians) health services to address their health needs.
A large share of non-citizen lawfully present immigrants with 5 years or less of U.S. residency reside in states that do not provide Medicaid coverage until immigrants have fulfilled the 5-year waiting period. This population, however, could have access to Medicaid if they lived in one of the 15 states (including Washington, DC) that use state funds to provide this benefit for recent immigrants. Non-citizen lawfully present immigrants with less than 5 years of U.S. residency who lived in other states were eligible to purchase coverage from the health insurance exchanges before the 5-year Medicaid threshold. Importantly, ED utilization remained constant for all comparison categories before and after the implementation of the ACA.
With the exception of Louisiana and Arkansas, Southern states did not expand Medicaid as part of the ACA. In our analyses, participants in Southern states had higher odds of reporting lack of health insurance coverage and forgone care after the ACA. A stratified analysis (not shown, but available upon request) among immigrants from the South versus immigrants from other U.S. regions did not reveal broad differences among immigrants. In Southern states, however, non-citizen (5<) immigrants did not report any statistically significant coverage changes after the ACA implementation, which contrast with the national results reported in our findings. Since most differences in ACA-related policies occurred at the state level, future research with access to state-level data should investigate how heterogeneity in the ACA implementation across states could impact coverage rates, access to and utilization of health care among immigrants.
The limitations of the analyses should be acknowledged. First, our study used a repeated cross-sectional design, which limits the observations of differences over time. Second, self-reported data are dependent on participants’ reports, which in some cases could differ from objective assessments of access to and utilization of care. Third, while the sample size for the analyses is relatively large and the statistical analyses are adequately powered, the analyses distinguish among only four U.S. regions (Northeast, Midwest, South and West). Future research could benefit from state level information to account for the regional factors that influence insurance coverage and access to care.
Conclusions
This study shows that the ACA has closed the coverage gap between U.S.-born and naturalized citizens and non-citizen immigrants. The ACA, however, excluded undocumented immigrants and preserved a 5-year residency requirement for non-citizens who were legally present in the U.S. in most states. Future health care and immigration reform efforts could reduce this gap further by including undocumented immigrants and by preserving affordable coverage options by all individuals who currently benefit from ACA-related coverage. Current proposals to undercut the benefits of the ACA, including the recent Senate tax bill that eliminates the ACA individual mandate, have led to much uncertainty about the future of health care financing and access. Research that documents the main outcomes of the ACA is necessary to compare how future policy changes would impact access to and utilization of health care among vulnerable populations. Future research should address the specific impact of programs such as the availability of Medicaid coverage in states where immigrants live and by studying coverage gains among individuals who were eligible for subsidies in the health insurance exchanges.
References
The Uninsured: An Interactive Tool. 2014. http://kff.org/interactive/the-uninsured-an-interactive-tool/. Accessed 14 Aug 2014.
Prevention CfDCa. Health insuance coverage: early release of estimtates from the National Health Interview Survey. Washington: U.S. Department of Health and Human Services; 2014.
Chen J, Vargas-Bustamante A, Mortensen K, Ortega AN. Racial and Ethnic disparities in health care access and utilization under the Affordable Care Act. Med Care. 2016;54(2):140–6.
Chen J, Bustamante AV, Tom SE. Health care spending and utilization by race/ethnicity under the Affordable Care Act’s dependent coverage expansion. Am J Public Health. 2015;105(Suppl 3):S499-507.
Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA. 2015;314(4):366–74.
Cutler DM. From the Affordable Care Act to affordable care. JAMA. 2015;314(4):337–8.
Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care. 2002;40(1):52–9.
Alegria M, Canino G, Rios R, Vera M, Calderon J, Rusch D, et al. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatr Serv. 2002;53(12):1547–55.
Waidmann TA, Rajan S. Race and ethnic disparities in health care access and utilization: an examination of state variation. Med Care Res Rev. 2000;57(Suppl 1):55–84.
Weinick RM, Zuvekas SH, Cohen JW. Racial and ethnic differences in access to and use of health care services, 1977 to 1996. Med Care Res Rev. 2000;57(Suppl 1):36–54.
Uninsured KCoMat. Key facts on health coverage for low-income immigrants today and under the Affordable Care Act, Washington; 2013.
Kaiser Commision on Medicaid and the Uninsured. Summary of New Health Reform Law. Kaiser Family Foundation; 2010.
CBO. The impact of unauthorized immigrants on the budgets of state and local governments. Washington: Congressional Budget Office; 2007.
Zuckerman S, Waidmann TA, Lawton E. Undocumented immigrants, left out of health reform, likely to continue to grow as share of the uninsured. Health Aff. 2011;30(10):1997–2004.
Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208–20.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10.
Ortega AN, Rodriguez HP, Vargas Bustamante A. Policy dilemmas in latino health care and implementation of the Affordable Care Act. Annu Rev Public Health. 2015;36:525–44.
Vargas Bustamante A, Chen J, Fang H, Rizzo JA, Ortega AN. Identifying health insurance predictors and the main reported reasons for being uninsured among US immigrants by legal authorization status. Int J Health Plan Manag. 2014;29(1):e83–96.
Vargas Bustamante A, Fang H, Garza J, Carter-Pokras O, Wallace SP, Rizzo JA, et al. Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status. J Immigr Minor Health. 2012;14(1):146–55.
Gee EM, Kobayashi KM, Prus SG. Examining the healthy immigrant effect in mid- to later life: findings from the Canadian Community Health Survey. Can J Aging. 2004;23(Suppl 1):S61–9.
Gushulak B. Healthier on arrival? Further insight into the “healthy immigrant effect”. CMAJ. 2007;176(10):1439–40.
Nolan A. The ‘healthy immigrant’ effect: initial evidence for Ireland. Health Econ Policy Law.1–20.
Bustamante AV, Chen J. Health expenditure dynamics and years of U.S. residence: analyzing spending disparities among Latinos by citizenship/nativity status. Health Serv Res. 2012;47(2):794–818.
McDonald JT, Kennedy S. Insights into the ‘healthy immigrant effect’: health status and health service use of immigrants to Canada. Soc Sci Med. 2004;59(8):1613–27.
National Health Interview Survey [Internet]. National Center for Health Statistics, Centers for Disease Control and Prevention. 2016 [cited 8/09].
Chen J, Vargas-Bustamante A, Novak P. Reducing young adults’ health care spending through the ACA expansion of dependent coverage. Health Serv Res. 2016;52(5):1835–57
Karaca-Mandic P, Norton EC, Dowd B. Interaction terms in nonlinear models. Health Serv Res. 2012;47(1 Pt 1):255–274.
Krogstad JM, Passel JS, Cohn DV. Five facts about illegal immigration in the U.S. Washington: Pew Research Center; 2016
Funding
P30-AG021684 & UL1-TR000124 and 1R01MD011523-01.
Author information
Authors and Affiliations
Contributions
AVB—study design, development and implementation of methods, data analysis, manuscript preparation. JC—study design, development and implementation of methdos, data analysis, and manuscript editing. RMM—Study design, manuscript editing. ANO—Manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Bustamante, A.V., Chen, J., McKenna, R.M. et al. Health Care Access and Utilization Among U.S. Immigrants Before and After the Affordable Care Act. J Immigrant Minority Health 21, 211–218 (2019). https://doi.org/10.1007/s10903-018-0741-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-018-0741-6