Abstract
Korean men and women have the highest current smoking rates across all Asian ethnic subgroups in the United States. This is a 2-arm randomized controlled study of a culturally adapted smoking cessation intervention. The experimental condition received eight weekly 40-min individualized counseling sessions that incorporated Korean-specific cultural elements, whereas the control condition received eight weekly 10-min individualized counseling sessions that were not culturally adapted. All participants also received nicotine patches for 8 weeks. One-hundred nine Korean immigrants (91 men and 18 women) participated in the study. The rate of biochemically verified 12-month prolonged abstinence was significantly higher for the experimental condition than the control condition (38.2 vs. 11.1 %, χ 2 = 10.7, p < 0.01). Perceived family norm significantly mediated the effect of cessation intervention on abstinence. Smoking cessation intervention for Korean Americans should be culturally adapted and involve family members to produce a long-term treatment effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Men in Korea typically become smokers during mandatory military service and continue to smoke throughout adulthood [1, 2]. Thus, the rates of smoking among men in Korea have been high hovering around 50 % [3] and male immigrants from this country smoke at higher rates (30–36 %) [4–6] than the general US male population (22 %) [7]. As a result, Korean men in California have a higher rate of smoking-related cancer deaths at 71 % [8, 9] as opposed to 30 % in the general US population [10]. Although Korean American women (12 %) are not likely to smoke more than the general US female population (17 %) [6, 7], the rate by Korean women is about four times higher compared to all Asian American women [5, 6]. Particularly, Korean American women who have high levels of acculturation to American culture smoke at higher rates than recent immigrants [6, 11]. Korean Americans also have the highest exposure to secondhand-smoke at work and at home within the Asian American population [12–15].
The 2008 Clinical Practice Guideline [16] stated that the first step in treating tobacco use is identifying the users and recommended that clinicians should seize the opportunity when tobacco users visit an office given that more than 70 % of them visit a physician each year. However, this opportunity may not exist for a large number of Korean Americans because they often do not have a primary care physician due to having the highest uninsured rate of all racial and ethnic groups [17, 18]. The high uninsured rate is largely due to the fact that Korean Americans are predominantly employed in small businesses that do not mandate health insurance coverage [19, 20]. The new health care reform policies may change this in the future. In addition, linguistic and other structural barriers further hinder them from accessing treatment for tobacco dependence. For example, based on the California Tobacco Use Surveys between 2003 and 2008, only 24 % of Korean American smokers had ever been advised to quit by their physicians as opposed to 46 % of general US smokers [21, 22].
Unfortunately there has been insufficient dissemination and evaluation of our existing evidence-based tobacco dependence treatment (e.g., cognitive behavioral therapy and pharmacotherapy) with racial and ethnic minority populations [16]. Thus, there is an urgent need to guide how to engage minority smokers and how to adapt existing interventions for them [16, 23]. Lau [24] invoked the term ‘social validity’ in discussing engagement. The social validity of a treatment refers to its perceived acceptability and utility, which might be influenced by cultural worldviews and the practical realities of life circumstances (e.g., immigration, acculturative stress, linguistic barrier, and insurance coverage) of the group being served. Thus, it has long been suggested that to be effective smoking cessation programs need to be anchored in the norms, values, and experiences of the cultural groups being studied [25, 26].
Despite recommendations for the need for culturally adapted interventions for minority smokers, findings regarding their effectiveness as compared with non-adapted interventions are mixed. For example, a review of 64 cessation studies revealed that culturally adapted interventions were generally effective, particularly, for those who had stronger racial/ethnic identity [27]. In contrast, a systematic review of 26 smoking cessation studies found that culturally adapted interventions did not yield better treatment outcomes than non-adapted interventions although the former were more acceptable to minority smokers than the latter [28]. Borrelli [29] suggested cultural adaptation is the next step to jump-start stalled smoking cessation rates for a special population and the adaptation should be at a deep structural level of the culture. As per Borrelli [29], a special population is a group of people that has disproportionate burden of tobacco-related diseases and has norms and customs that serve both as risk factors for smoking and as protective factors to facilitate quitting. Hence, Korean Americans can be classified as a special population that requires a deep-culturally adapted cessation intervention.
Three cessation intervention studies [15, 30, 31] had been conducted with Korean Americans. The first study of 848 Koreans in California [15] offered quitline cessation counseling plus nicotine replacement therapy (NRT) and found a significant treatment effect compared with self-help materials. However, this study is limited because abstinence was based on self-report and participants were followed for up to 6 months only. The second study of 30 participants in Pennsylvania [30] provided one face-to-face cessation counseling session in comparison with one general health education session. The third study of 1,409 participants recruited across the nation [31] compared an Internet-based cessation program with self-help materials. Neither of the second and third studies found any significant treatment effect of the interventions. Although all authors of the three studies stated that they provided a culturally adapted cessation intervention, the adaptation was limited to the use of the Korean language and Korean therapists with a focus on the common Asian cultural value such as collectivism. There is a need for more studies to adapt intervention strategies at a deep Korean cultural level in an effort to improve cessation rates [29].
The main purpose of the present study was to test the feasibility and initial efficacy of a culturally adapted cognitive behavioral therapy that was delivered as individual therapy with NRT compared to treatment as usual (a brief behavioral therapy plus NRT). The experimental condition incorporated several Korean-culture specific intervention strategies into the treatment, which are described in Procedures of the Methods section.
Theoretical Framework of the Study
We have reported our findings from a prior focus group study that attitudes and perceived social norms are two important psychosocial factors driving Korean Americans’ smoking behavior [2]. Particularly, perceived social norms toward quitting seem to have a specific cultural implication in motivating Koreans to quit smoking given that they have been inculcated with the values of collectivism and conformity [2]. Based on these findings, we used the Theory of Planned Behavior as a guiding theoretical framework for developing our culturally adapted cessation intervention. The theory posits attitudes, perceived social norms, and self-efficacy are the main antecedents to behavior change [32, 33]. Thus, our intervention, particularly cultural adaptation of the cessation intervention, was directed towards: (a) facilitating positive attitudes toward quitting through culture-specific education and counseling, and alleviating negative attitudes with culture-specific counseling and NRT; (b) coaching family members to reinforce anti-smoking messages to smokers and to support treatment adherence; and (c) enhancing self-efficacy through culture-specific counseling and behavioral skills training.
Methods
The study is a two-arm randomized controlled trial with four follow-ups (1, 3, 6, and 12 months from the quit day). It was approved by the Institutional Review Board of the University of Massachusetts Medical School. The study was conducted in northeast regions of the United States. Participants were recruited by advertising the study in local Korean newspapers, on local Korean television and radio stations, and on online Korean websites. All advertisements were done in Korean because the study was aimed for Korean-speaking immigrants who might experience linguistic and cultural barriers to seeking cessation treatments. The recruitment took place for 19 months. The majority of the participants were from a Korean-immigrant dense area such as Queens in New York City and Palisades Park, New Jersey. We obtained contact information including home address and at least two connected telephone lines and verified the contact information via post office mails and calls. All participants signed an informed consent form upon enrollment in the study. Irrespective of smoking status, participants were paid a $20 gift certificate at baseline and 1-month follow-up and a $40 gift certificate at each of the three follow-ups (post-quit 3, 6, and 12 months).
Participants
Inclusion criteria were as follows: adult smokers who (1) self-identified as Korean ethnicity, (2) were 18 years or older, (3) were able to speak and read Korean or English, (4) had been smoking at least 10 cigarettes a day for the past 6 months, (5) were willing to use nicotine patches as directed, and (6) were expected to live in the current geographical area for at least 1 year. Individuals were excluded if they concurrently received treatment for smoking cessation outside of the study. Those who had contraindications (e.g., skin disease and pregnancy) to nicotine patches were excluded. Smokers with a serious mental illness (e.g., schizophrenia) were also excluded because we believed that they might require more intensive treatments than the intervention provided in this study. In addition, those who earned a score of 21 or higher on the Alcohol Use Disorders Identification Test [34] were excluded. This decision was based on the finding that they were more likely to withdraw from the study even before the target quit day [35]. The present study was powered to detect a difference of 25 % in abstinence rates between two conditions [36].
Procedure
Korean Americans were asked to call the contact number provided in the advertisement and were screened via telephone, which took about 5–10 min. If the caller met the selection criteria described above, he/she was directed to the office where the study was being conducted. At the first office visit, participants completed baseline research questionnaires in a paper-and-pencil format. The questionnaires were written in Korean or in English and a bilingual research staff was present to assist them if they needed help. The time spent to complete the questionnaires ranged from 30 to 60 min.
Individuals who had completed the questionnaires were provided with a sealed envelope enclosed with a paper on which a computer-generated random number was written. Individuals who had a yellow highlighted number were assigned to the experimental condition (the culturally adapted intervention) and those who had a non-highlighted number were assigned to the control condition (a brief standard intervention). The randomization was done at a ratio of 1:1 and was stratified by gender to have an equal number of women in each condition.
All participants but one had the interventions delivered in the Korean language. Two Korean bilingual natives (one female and one male) delivered the intervention and both took the tobacco treatment specialist training. The therapists provided counseling to both conditions and assured fidelity to the two interventions such as limiting the intervention time to 40 min for the experimental condition versus 10 min for the control condition and following each procedure described in the intervention manual of each treatment condition. To control possible therapist effects (e.g., experience in counseling) on treatment outcomes, we did not assign the therapists to a specific treatment condition. We requested that participants in both conditions should restrain from sharing the information learned in therapy with other Koreans in the community; however, it was possible that some might have shared the information. All therapy sessions were audiotaped and reviewed for fidelity. A research assistant who did not provide any interventions transcribed the audiotapes to scripts. Follow-up assessments were done by the same person so that she was not blinded to treatment condition.
Participants in both conditions received eight weekly individualized counseling sessions in a face-to-face format; however, the length of sessions differed between the two (40 vs. 10 min). Irrespective of treatment condition, all participants received the same education about the deleterious effects of smoking on the human body and behavioral skills training to deal with nicotine withdrawal symptoms. Expired-air CO test was done at the beginning of each session and participants were explained about the results of the test. They also had the same education on neurobiological changes in the brain associated with nicotine dependence and the treatment mechanism of NRT. They received a 1-week supply of nicotine patches at each visit from the quit day for 8 weeks and returned used patches to be monitored for medication adherence. Participants selected the quit day in consultation with the therapist and it was usually based on one’s level of readiness for quitting. However, the day was set between the second and fourth therapy sessions of each individual.
In addition to intervention components described above, the experimental condition received the following Korean-culture specific interventions: (1) explanation of the harmful effects of CO in an analogy of gas poisoning from coal briquettes that had been most widely used as a heating system in Korea till 1980s, (2) information on recent smoking-related cancer deaths of celebrities in Korea and high smoking-related cancer death rates among Korean men in California, (3) coaching family members for assistance and support by inviting them into therapy sessions or calling them, (4) information on the high prevalence of secondhand-smoke exposure in the Korean community and explanation of harms related to the exposure, (5) utilization of Korean news media in education (6) behavioral skills training in preparation for Korean-specific relapse-prone situations (e.g., a visitor who smokes from Korea and a trip to Korea). Family coaching (the third intervention) and utilization of Korean news media (the fifth intervention) are further described in the next two paragraphs. Details on the other interventions can be found elsewhere [35].
Family members of participants in the experimental condition were invited to therapy sessions. Those who could not attend were contacted via telephone calls at least two times, one before and the other one on the quit day. Family coaching before the quit day was focused on harms associated with exposure to secondhand smoke and relating antismoking messages to the participants. The coaching on the quit day was focused on supporting the participants during the first post-cessation week and monitoring adherence to nicotine patches. We also reached out to other smokers (e.g., mostly men such as husband and son[s]) within the family who did not want to quit at the time. We asked them not to smoke in front of the study participant and to the extent possible, to keep their cigarettes hidden from the participant. In contrast, none of the family members in the control condition was invited or contacted.
We used news articles in Korean newspapers to inform participants in the experimental condition of the dramatic change in social norms toward smoking and quitting in Korea. We also used the articles to educate harms associated with smoking. These articles are valuable resources to motivate Korean smokers for quitting. For example, after the Norwegian terrorist Anders Behring Breivik killed 68 people on July 22, 2011, Korean newspapers published numerous articles describing how the killer prepared a dum–dum bullet that he filled with nicotine liquid, including the commentary on the toxicity of nicotine liquid [e.g., [37, 38] ].
Measures
The primary outcome of the study was the 12-month prolonged abstinence assessed by self-report and biological confirmation. The secondary outcome was the 7-day point prevalence abstinence. The 12-month prolonged abstinence was defined as being continuously abstinent from the quit day except for the first 2-week grace period. The 7-day point prevalence abstinence was defined as having not smoked a single cigarette at least for the past 7 days. Self-reported abstinence was biochemically verified with expired-air CO (<6 parts ppm) and saliva cotinine (≤30 ng/ml) tests. We used a Micro + Smokerlyzer CO Monitor (Bedfont Scientific, NJ) and NicAlert® test strips. The NicAlert® test is a semi-quantitative measure of cotinine based on a colorimetric immunoassay reaction. Researchers often used a cutoff level of 20 ng/ml in saliva continine test as an indicator of abstinence [e.g., 39, 40]; hence, we used level 2 (30–100 ng/ml) as a cutoff level instead of level 1 (10–30 ng/ml). However, those who yielded a CO level of 6 ppm or higher were classified as smokers even if their cotinine test results were level 1.
We found that a CO breath test was not sensitive enough to determine smoking status among Korean Americans. Approximately four out of ten participants (41.3 %) who were determined to be smoking either by self-reports or by saliva cotinine tests yielded CO readings lower than 10 ppm, which has been widely used as a cutoff level for abstinence. Thus, we used a cutoff level of 6 ppm to be more accurate. Among those who yielded CO readings less than 6 ppm, only one was classified as smoking by the saliva cotinine test even though the participant reported having been abstinent.
Sociodemographic information, including age, marital status, education, employment, acculturation, and years in the United States, was obtained. History of smoking was assessed regarding the following aspects: age when the participant began smoking regularly, the average number of cigarettes smoked per day, smoking at an indoor house, smoking at an indoor office, presence of other smokers among family members, any quit attempts made in the past year, and past use of cessation medications. Fagerström Test for Nicotine Dependence [41], Alcohol Use Disorder Identification Test [34], and Center for Epidemiologic Studies-Depression Scale (CESD-S) [42] were used to assess nicotine dependence, alcohol use problems, and depression, respectively because these variables have been identified as correlates of smoking in Korean Americans [e.g., 43, 44]. Instead the cutoff score of 16 recommended for the determination of depression by the CESD-S, we used a score of 21 recommended for Koreans [45].
The Theory of Planned Behavior variables (attitudes, perceived social norms, and self-efficacy) were assessed at baseline and each follow-up. Attitudes toward quitting were assessed using the Perceived Risks and Benefits of Quitting Questionnaire [46]. It consists of two subscales: Perceived Risks (negative attitudes) and Perceived Benefits (positive attitudes). Perceived social norms were assessed using the Perceived Social Norm Index [35]. The measure consists of two question-items (a normative belief and the level of motivation to comply with the belief) and assesses perceived norms of each referent group such as family and peers. Self-efficacy was assessed using a Korean version of the Situational Temptation Scale that was adapted in Koreans’ smoking cultural context [47].
Instruments that were originally developed in English were all translated and back-translated through a rigorous process of cross-cultural validation, including pilot-tests. More detailed descriptions of these measures and their psychometric functions have been reported elsewhere [35, 47–49].
Data Analysis Plan
Data analyses were performed with SPSS version 21.0. Demographics, smoking history and psychosocial variables were compared between the two treatment conditions (the experimental vs. the control), using Chi square tests for categorical variables and independent t-tests for continuous variables. Using the intent-to-treat analysis, we included all participants in treatment outcomes analyses and treated as smokers if they dropped out of the study or refused biochemical tests. Survival analyses were conducted to examine the relationship between treatment condition and abstinence using the Kaplan–Meier log-rank tests and the Cox proportional hazards model when including possible covariates such as nicotine dependence and self-efficacy. Finally, mediation analyses were performed to examine the effect of the intervention on abstinence via the TPB variables (attitudes, perceived social norms, and self-efficacy), using the Hayes’ PROCESS computation tool for a serial multiple mediator model with a binary outcome variable [50, 51]. In this model, the total effect is usually not equal to the sum of the direct and indirect effects because the indirect and total effects are scaled differently [50–52]. All tests were two-sided and all p values less than 0.05 were considered statistically significant.
Results
Of individuals (N = 232) who made the initial contact, 85 (36.6 %) did not meet inclusion criteria, and 33 (14.2 %) decided not to participate for a variety of reasons (e.g., conflict with work schedule) (Fig. 1). Those who did not meet the inclusion criteria were mostly non-smokers seeking information for smoking family members or light smokers who smoked less than 10 cigarettes per day. Other reasons for exclusion included having a hearing problem and refusal to follow study protocols.
Table 1 compares baseline characteristics of the final sample by treatment condition. Participants in the experimental condition were less likely to have a quit attempt (χ 2 = 5.23, p < 0.05) in the past year than those in the control condition. The former also trended more toward having other smokers in the family (χ 2 = 3.58, p = 0.08) than the latter. Except for these two, no difference was found between the two conditions. In contrast, baseline characteristics differed largely by gender. Compared with men, women smokers were less likely to be married (50.0 vs. 86.8 %, p < 0.01), started smoking at an older age (25.6 [mean] ± 6.5 [standard deviation] vs. 19.04 ± 2.65, p < 0.001), and smoked fewer cigarettes per day on average (13.11 ± 3.71 vs. 17.87 ± 5.82, p < 0.01). Women were more likely to smoke at home (55.6 vs. 27.5 %, p < 0.05) and to live with other smokers (50.0 vs. 22.0 %, p < 0.05). Women were less likely than men to have any serious quit attempts in the past year (27.8 vs. 61.5 %, p = 0.01). Exactly half (9/18) of the women screened positive for depressive symptoms as opposed to 15.4 % (14/91) of the men (p < 0.01). Women perceived a stronger peer norm favoring quitting than men did (4.28. ± 2.72 vs. 2.89 ± 2.73, p = 0.05).
At the end of the intervention, the mean number of sessions attended significantly differed between the two conditions (experimental = 6.02 ± 1.87 vs. control = 4.91 ± 2.28, p < 0.01). The mean number of patches used also marginally differed (experimental = 42.49 ± 20.54 vs. control = 35.13 ± 22.18, p = 0.08). More participants in the experimental condition tended to stay in the study till the endpoint (the 12-month follow-up) than those in the control condition (80.0 vs. 63.0 %, p = 0.06) and the 12-month retention rate for the total participants was 72.5 % (79/109).
The rate of the 12-month prolonged abstinence was significantly higher in the experimental condition (38.2 %) than the control condition (11.1 %; odds ratio = 4.67, 95 % confidence interval = 1.67, 12.99, p < 0.01). The difference was significant for both men (34.8 vs. 13.3 %, p < 0.05) and women (55.6 vs. 0 %, p < 0.05). Interestingly, once women had achieved at least 3 months of prolonged abstinence, none relapsed to smoking at subsequent follow-ups. In contrast, men continued to relapse even after a 6-month prolonged abstinence. The rate of the 7-day point prevalence abstinence at the 12-month follow-up was 41.8 % for the experimental condition and 18.5 % for the control condition (p = 0.01). These rates included those (N = 6) who recovered from relapses at earlier follow-ups. The survival rate of participants who maintained abstinence over time differed significantly between the two conditions, favoring the experimental over the control condition (log rank χ 2 = 14.31, p < 0.001; Fig. 2). The Cox proportional hazards model did not show any baseline characteristics that predicted relapses when adjusted for treatment condition (experimental vs. control).
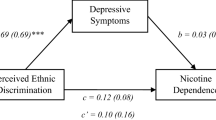
Among the three Theory of Planned Behavior variables, perceived family norm and self-efficacy were found to be significant correlates of 7-day point-prevalence abstinence at each follow-up. However, only perceived family norm had a significant relationship with treatment condition. Among the paths identified (see Fig. 3), the direct effect of treatment condition on perceived family norm at 1-month and 3-month follow-ups, and the direct effect of perceived family norm at 6-month follow-up on abstinence were significant, controlling for perceived family norm at baseline. The total effect of treatment condition on abstinence was significant (coefficient = 1.30, p = 0.02); yet, when the mediator, perceived family norm, was entered, the direct effect of treatment condition on abstinence was no longer significant. Bootstrapping approach with 5,000 replications estimated a total indirect effect of 1.92 with a 95 % bias-corrected and accelerated confidence interval of 0.34–6.32. Particularly, perceived family norm at 3-month and 6-month follow-ups were significant mediators.
A meditational model of abstinence (N = 68). Intervention condition was related to abstinence through the mediation of perceived family norm in the path (cessation intervention → 3-M F/U perceived family norm → 6-M F/U perceived family norm → 12-M prolonged abstinence). All coefficients in the diagram are unstandardized. Note. M = month, F/U = follow-up, †p < 0.10, *p < 0.05, **p < 0.01, and ***p < 0.001
Discussion
To the best of our knowledge, this is the first study reporting a significant treatment effect of a culturally adapted smoking cessation intervention for Korean Americans compared with the treatment as usual. Here, unlike previous studies on this population (15, 30, 31), abstinence rates were biochemically verified using expired-air CO and saliva cotinine tests. The odds for achieving the 12-month prolonged abstinence were almost five times higher in the experimental condition that received the culturally adapted intervention than the control condition wherein a non-culturally adapted intervention was provided. In addition, the difference between the two treatment conditions was significant for both men and women.
Gender was not a significant predictor of the 12-month prolonged abstinence although some notable differences were found between men and women. First, none of the women in the control condition had achieved short-term abstinence (e.g., 3-month prolonged) let alone long-term abstinence. On the other hand, a significant proportion of the men in the control condition achieved short-term abstinence although many of them relapsed at 6- and 12-month follow-ups. Second, none of the women who achieved at least 3 months of prolonged abstinence relapsed at subsequent follow-ups. In contrast, regardless of treatment condition, a significant proportion of the men who achieved a 3-month prolonged abstinence relapsed. Although findings are mixed in tobacco literature, there is substantial evidence that female smokers were less likely to succeed in quitting than male smokers [e.g., 53–55]. The present study supports this gender difference when cessation outcomes were compared among those in the control condition. However, no gender difference was found among those in the experimental condition and women were more likely to achieve long-term abstinence once they had short-term abstinence.
Among the three variables of the Theory of Planned Behavior, self-efficacy and perceived family norm were significant correlates of 7-day point prevalence abstinence at each follow-up. It was also found that perceived family norm had a significant mediating effect on the relationship between treatment condition and abstinence. Korean Americans have been known for its strong cultural values of collectivism and conformity [2]. Korean Americans who received the culturally adapted cessation intervention perceived a stronger family norm favoring quitting than those who received the brief cessation intervention, which in turn enhanced the former group’s likelihood of achieving the 12-month prolonged abstinence. In a previous study with Korean American men, perceived family norm was a significant predictor of a quit intention [56–58] and 24-h abstinence at 1-month follow-up [56].
Results of the present study should be interpreted with caution. First, treatment intensity differed between the two conditions (40 vs. 10 min), which might have contributed to the large treatment effect. Second, the small number of Korean American women in this study limited finding any gender interaction effects on treatment outcomes. Third, participants were treatment seeking individuals who may differ from the general population of Korean American smokers, which limits the generalizability of the findings. However, we found that participants in this study did not differ in terms of demographics and smoking behavior compared with a random sample of Korean American smokers who were not seeking treatment at the time [57].
There is a strong possibility of cross-condition contamination if therapists from the same ethnic group provide cessation treatment for both adapted and non-adapted conditions. To avoid this, therapists who were not familiar with the culture of an ethnic group are needed to provide a non-adapted intervention. For example, in a study with American Indians, native Indian therapists delivered a culturally adapted smoking cessation intervention for the experimental condition, whereas non-native therapists provided a non-adapted intervention for the control condition [59]. English was the language used in both conditions. However, it was difficult to find an Asian therapist who is fluent with the language of an Asian ethnic subgroup but not familiar with the culture of the group. For example, it was extremely difficult to find a therapist who is fluent with the Korean language but not familiar with the Korean culture. Due to this logistic difficulty researchers frequently compare a culturally adapted cessation intervention for ethnic minority smokers with usual care, a non-smoking cessation intervention (e.g., general health education), or self-help materials [27].
In conclusion, the high abstinence rate produced by the culturally adapted cessation intervention may be, in part, related to the depth and thoroughness in its cultural adaptation, which showed a distinctive departure from other culturally adapted cessation interventions developed for Korean Americans (15, 30, 31). Future studies should be conducted with a large sample of Korean women relative to Korean men and examine a possible gender interaction effect on treatment outcomes. In addition, more studies are warranted to examine the mediating effect of perceived family norm toward quitting that was found in this study.
References
Allem JP, Ayers JW, Irvin VL, Hofstetter R, Hovell M. South Korean military service promotes smoking: a quasi-experimental design. Yonsei Med J. 2012;53(2):433–8.
Kim SS, Son H, Nam KA. The sociocultural context of Korean American men’s smoking behavior. West J Nurs Res. 2005;27(5):604–23.
Jung-Choi KH, Khang YH, Cho HJ. Hidden female smokers in Asia: a comparison of self-reported with cotinine-verified smoking prevalence rates in representative national data from an Asian population. Tobacco Control. 2012;21(6):536–42.
Kim SS, Ziedonis D, Chen KW. Tobacco use and dependence in Asian Americans: a review of the literature. Nicotine Tob Res. 2007;9:169–84.
Caraballo RS, Yee SL, Gfroerer J, Mirza SA. Adult tobacco use among racial and ethnic groups living in the United States, 2002–2005. Public Health Res Pract Policy. 2008;5(3):1–9.
Li S, Kwon SC, Weerasinghe I, Rey MJ, Trinh-Shervin C. Smoking among Asian Americans: acculturation and gender in the context of tobacco control policies in New York City. Health Promot Pract. 2013;14(5):S18–28.
Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2011. MMWR. 2012;61(44):889–94.
Kwong SL, Chen MSJR, Snipes KP, Bal DG, Wright WE. Asian subgroups and cancer incidence and mortality rates in California. Cancer. 2004;104(12 Suppl):2975–81.
Raz DJ, Gomez SL, Chang ET, Kim JY, Keegan TH, Pham J, Kukreja J, Hiatt RA, Jablons DM. Epidemiology of non-small cell lung cancer in Asian Americans: incidence patterns among six subgroups by nativity. J Thorac Oncol. 2008;3(12):1391–7.
Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000—2004. MMWR. 2008;57(45):1226–8.
Song YJ, Hofstetter CR, Hovell MF, Paik HY, Park HR, Lee J, Irvin V. Acculturation and health risk behaviors among Californians of Korean descent. Prev Med. 2004;39(1):147–56.
Ma GX, Tan Y, Fang CY, Toubbeh JI, Shive SE. Knowledge, attitudes and behavior regarding secondhand smoke among Asian Americans. Prev Med. 2005;41(2):446–53.
Myung SK, McDonnell DD, Kazinets G, Seo HG, Moskowitz JM. Relationships between household smoking restrictions and intention to quit smoking among Korean American male smokers in California. J Korean Med Sci. 2010;25(2):245–50.
Tong EK, Nguyen TT, Vittinghoff E, Perez-Stable EJ. Smoking behaviors among immigrant Asian Americans: rules for smoke-free homes. Am J Prev Med. 2008;35(1):64–7.
Zhu SH, Cummins SE, Wong S, Gamst AC, Tedeschi GJ, Reyes-Nocon J. The effects of a multilingual telephone quitline for Asian smokers: a randomized controlled trial. J Natl Cancer Inst. 2012;104(4):299–310.
Fiore MC, Jaen CR, Baker TB, Bailey WC, Bennett G, Benowitz NL, Curry SJ, Wewers ME. Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville: USDHHS, U.S. Public Health Services; 2008.
Brown ER, Lavarreda SA, Ponce N, Yoon J, Cummings J, Rice T. The state of health insurance in California: findings from the 2005 California health interview survey. UCLA Center for Health Policy Research; 2007.
Shin H, Song H, Kim J, Probst JC. Insurance, acculturation, and health service utilization among Korean-Americans. J Immigr Minor Health. 2005;7(2):65–74.
Min PG. Ethnic solidarity for economic survival: Korean greengrocers in New York City. New York: Russell Sage Foundation; 2008.
Yoon IJ. Who is my neighbor? Koreans’ perceptions of Blacks and Latinos as employees, customers, and neighbors. Dev Soc. 1998;27(1):49–75.
Tong EK, Tang H, Chen MS Jr, McPhee SJ. Provider smoking cessation advice among California Asian-American smokers. Am J Health Promot. 2011;25(5):S70–4.
Al-Delaimy WK, White MM, Trinidad DR, Messer K, Gilmer T, Zhu S-H, Mills AL, Pierce JP. The California tobacco control program: can we maintain the progress? Results from the California Tobacco survey, 1990–2005. Sacramento: California Department of Public Health; 2008.
Piper ME, Fox BJ, Welsch SK, Fiore MC, Baker TB. Gender and racial/ethnic differences in tobacco-dependence treatment: a commentary and research recommendations. Nicotine Tob Res. 2001;3:291–7.
Lau AS. Making the case for selective and directed cultural adaptations of evidence-based treatments: examples from parent training. Clin Psychol Sci Pract. 2006;13(4):295–310.
Brugge D, Dejong W, Hyde J, Le Q, Shih CS, Wong A, Tran A. Development of targeted message concepts for recent Asian immigrants about secondhand smoke. J Health Commun. 2002;7(1):25–37.
Hall GC. Psychotherapy with ethnic minorities: empirical, ethical, and conceptual issues. J Consult Clin Psychol. 2001;69:502–10.
Cox LS, Okuyemi K, Choi WS, Ahluawlia JS. A review of tobacco use treatments in U.S. ethnic minority populations. Am J Health Promot. 2011;25(5 Suppl):S11–30.
Liu JJ, Wabnitz C, Davidson E, Bhopal RS, White M, Johnson MR, Netto G, Sheikh A. Smoking cessation interventions for ethnic minority groups—a systematic review of adapted interventions. Prev Med. 2013;57(6):765–75.
Borrelli B. Smoking cessation: next steps for special populations’ research and innovative treatments. J Consult Clin Psychol. 2010;78(1):1–12.
Fang CY, Ma GX, Miller SM, Tan Y, Su X, Shives S. A brief smoking cessation intervention for Chinese and Korean American smokers. Prev Med. 2006;43(4):321–4.
McDonnell DD, Kazinets G, Lee HJ, Moskowitz JM. An Internet-based smoking cessation program for Korean Americans: results from a randomized controlled trial. Nicotine Tob Res. 2011;13(5):336–43.
Ajzen I. Attitudes, personality, and behavior. Chicago: Dorsey; 1988.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: guidelines for use in primary care. 2nd ed. Geneva: World Health Organization; 2001.
Kim SS, Kim SH, Ziedonis D. Tobacco dependence treatment for Korean Americans: preliminary findings. J Immigr Minor Health. 2012;14:395–404.
G Power Data Analysis. Retrieved from http://www.psycho.uni-duesseldorf.de/abteilungen/aap/gpower3/.
Chung HM. [Devil bullet also called dum–dum bullet had fatal amount of nicotine], 2011. Retrieved from http://article.joinsmsn.com/news/article/article.asp?total_id=5853816&cloc.
Jung SJ. [The Norwegian killer added a poisonous chemical inside the bullet], 2011. Retrieved from http://m.chosun.com/article.html?contid=2011072600938&sname=news.
Murray RP, Connett JE, Buist AS, Gerald LB, Eichenhorn MS. Experience of Black subjects in the Lung Health Study smoking cessation intervention program. Nicotine Tob Res. 2001;3(4):375–82.
Voorhees CC, Stillman FA, Swank RT, Heagerty PJ, Levine DM, Becker DM. Heart, body, and soul: impact of church-based smoking cessation interventions on readiness to quit. Prev Med. 1996;25(3):277–85.
Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1989;86:1119–27.
Radloff L. The Center for Epidemiologic Studies Depression (CES-D) Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Juon H, Kim M, Han H, Ryu JP, Han W. Acculturation and cigarette smoking among Korean American men. Yonsei Med J. 2003;44:875–82.
Kim KK, Yu ESH, Chen EH, Kim J, Brintnall RA, Vance S. Smoking behavior, knowledge, and beliefs among Korean Americans. Cancer Pract. 2000;8:223–30.
Cho MJ, Kim KH. Use of the Center for Epidemiologic Studies Depression (CES-D) Scale in Korea. J Nerv Ment Dis. 1998;186:304–10.
McKee SA, O’Malley SS, Salovey P, Krishnan-Sarin S, Mazure CM. Perceived risks and benefits of smoking cessation: gender-specific predictors of motivation and treatment outcome. Addict Behav. 2005;30:423–35.
Kim SS, Kim SH, Gulick EE. Cross-cultural validation of smoking abstinence self-efficacy scale with Korean-American men. Issues Ment Health Nurs. 2009;30(2):122–30.
Kim SS, Fang H, DiFranza J, Ziedonis D, Ma G. Gender differences in the Fagerström test for nicotine dependence in Korean Americans. J Smok Cessat. 2012;7:31–6.
Kim SS, Gulick EE, Nam KA, Kim SH. Psychometric properties of the Alcohol Use Disorders Identification Test: a Korean version. Arch Psychiatr Nurs. 2008;22(4):190–9.
Hayes AF. An introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: Guilford Press; 2013.
Hayes AF. PROCESS: a versatile computational tool for observed variable mediation, moderation, and condition process modeling [White paper]. Retrieved from http://www.afhayes.com/public/process2012.pdf.
MacKinnon DP, Lockwood CM, Brown CH, Wang W, Hoffman JM. The intermediate endpoint effect in logistic and probit regression. Clin Trials. 2007;4:499–513.
Cepeda-Benito A, Reynoso JT, Erath S. Meta-analysis of the efficacy of nicotine replacement therapy for smoking cessation: differences between men and women. J Couns Clin Psycho. 2004;72:712–22.
Piper ME, Cook JW, Schlam TR, Jorenby DE, Smith SS, Bolt DM, Loh WY. Gender, race, and education differences in abstinence rates among participants in two randomized smoking cessation trials. Nicotine Tob Res. 2010;12(6):647–57.
Wetter DW, Kenford SL, Smith SS, Fiore MC, Jorenby DE, Baker TB. Gender differences in smoking cessation. J Couns Clin Psychol. 1999;67(4):555–62.
Kim SS. Predictors of short-term smoking cessation among Korean American men. Public Health Nurs. 2008;25(6):516–25.
Kim SS, Kim SH, McKay C, Ziedonis D. Comparison of characteristics among Korean American men between survey and cessation studies. Open J Prev Med. 2013;3(3):293–300.
Kim SS, Kim SH, Seward G, Fortuna L, McKee S. Korean American women’s experiences with smoking and factors associated with their quit intentions. ISRN addict. 2013. Retrieved from http://www.hindawi.com/isrn/addiction/2013/796570/.
Choi WS, Faseru B, Beebe LA, Greiner AK, Yeh HW, Shireman TI, Talawyma M, Cully L, Kaur B, Daley CM. Culturally-tailored smoking cessation for American Indians: Study protocol for a randomized controlled trial. Trials. 2011:12: 126. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3117716/pdf/1745-6215-12-126.pdf.
Acknowledgments
This work was supported by the National Institute on Drug Abuse ([NIDA], 5K23DA021243-02 to Dr. Kim) and partially by the NIDA (R01DA033323-01A1 to Dr. Fang).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, S.S., Kim, SH., Fang, H. et al. A Culturally Adapted Smoking Cessation Intervention for Korean Americans: A Mediating Effect of Perceived Family Norm Toward Quitting. J Immigrant Minority Health 17, 1120–1129 (2015). https://doi.org/10.1007/s10903-014-0045-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-014-0045-4