Abstract
Immigrant populations in the United States (US) have lower cancer screening rates compared to none immigrant populations. The purpose of this study was to assess the rates of cancer screening and examine factors associated with cancer screening behavior among African immigrant women in Minnesota. A cross sectional survey of a community based sample was conducted among African immigrants in the Twin Cities. Cancer screening outcome measures were mammography and Papanicolau smear test. The revised theoretical model of health care access and utilization and the behavioral model for vulnerable populations were utilized to assess factors associated with cancer screening. Only 61 and 52 % of the age eligible women in the sample had ever been screened for breast and cervical cancer respectively. Among these women, duration of residence in the US and ethnicity were significant determinants associated with non-screening. Programs to enhance screening rates among this population must begin to address barriers identified by the community.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disparities in cancer screening and optimum utilization of available screening tools remain major public health issues in the United States. Immigrant populations in general have lower screening rates compared to non immigrant populations in the United States (US) [1]. According to data from the National Health Interview Survey only 60 % of immigrant women reported having Pap smears in the past 3 years when compared to over 80 % of women born in the United States [2]. Goel and his colleagues compared cancer screening by race and ethnic groups. Results showed immigrants (Hispanics, Asian-American and Pacific Islander) had lower screening rates for cervical and breast cancer [3].
Over the last decade there has been a growing number of African immigrants (Somalis, Ethiopians, and Nigerians) migrating to Minnesota [4, 5]. There is significant diversity in culture, language, religion, and health perception among various African immigrant groups. An understanding of the barriers impacting cancer screening behavior among African female immigrant in Minnesota may help to develop targeted interventions. Although several studies have showed reduced cancer screening among Non-African immigrant populations [6–10], very few studies have examined factors associated with cancer screening among the African immigrants in the United States. This study sought to determine the rates of participation in breast and cervical cancer screening among age eligible female African immigrants in the Twin Cities and to examine barriers associated with these cancer screening procedures.
The Andersen [11] revised model for health care access and utilization in vulnerable populations was utilized in this study. In this model, vulnerable populations included minorities: undocumented immigrants, children and adolescents, mentally ill, disabled persons, refugees, the elderly; and homeless persons [12].
Applying models for health care access and utilization to vulnerable groups can be especially helpful in identifying the particular challenges individual groups face in obtaining services needed; and may provide insights into interventions that might improve and maintain health. We applied this revised model to age eligible African immigrant women in Minnesota. As immigrants they arguably experience problems emanating from language and cultural differences that may be barriers to seeking health care.
Conceptual Model
The revised Behavioral Model for Vulnerable Populations [11] is a major revision to the original behavioral model, a leading model widely used to explain the use of health services among vulnerable populations. The original behavioral model was developed by Andersen et al., [11, 13–15]. This model suggest that use of health care services is a function of (1) predisposing factors (those that predispose an individual to seek care); (2) enabling factors (those that would enhance or impede the use of care); (3) need characteristics (a person’s need for care); and (4) personal health behaviors.
Predisposing factors include characteristics such as demographic characteristics like age, gender, and marital status; social structural characteristics that include ethnicity, education, employment, family size, acculturation, immigration status, literacy; childhood characteristics, living conditions, psychological resources, and health beliefs [13].
Enabling factors are factors that would enhance or impede an individual’s ability to use healthcare services, should the need arise. These factors include personal/family resources (such as regular source of care), insurance status and affordability of getting medical care, income, competing needs, availability of information sources and ability to understand and utilize the available information[1, 13].
Need characteristics are the most immediate cause of the utilization of health services. They involve both perceived (self perception) and evaluated health status. The symptoms an individual experiences and their self-reported health status is used to assess their perceived illness while evaluated health measures are actual health problems that the individual is experiencing and those that have been clinically identified by health practitioners[1, 13].
The personal health practices domain is another component of the behavioral model and it includes diet, exercise, tobacco use, food sources and hygiene, unsafe sexual behavior, self-care, and adherence to care[1, 13].
Methods
Study Design
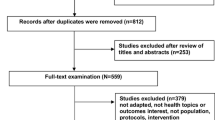
This study is based on a secondary data analysis from a cross sectional survey of a community based sample to determine a variety of health behaviors among African immigrants in Minnesota. The survey was conducted by New Americans Community Services (NACS) from 2006 to 2007. Prior to conducting the study, NACS facilitated focus groups to assist in the development of survey questions that would identify health conditions and health care seeking behavior of African immigrants in the Twin Cities. The survey included items that assessed background, social and economic factors, health care assess and utilization, lifestyle and risk behavior, and reproductive and sexual health. NACS employed and trained twenty-five interviewers in interview methodology prior to conducting the survey.
The survey was conducted in-person at the participants’ home in either English or participant’s preferred languages such as Pidgin English, Somali, or Oromo. The survey focused on urban areas in Minneapolis and St. Paul with the largest concentration of African immigrant families. Of the 1600 households’ of African immigrant families residing in the Twin Cities approached, a total of 1,009 households consented to participate. Survey protocol and all procedures related to the survey were reviewed and approved by community advisory board and the University of Minnesota Institutional Review Board.
Measures
Screening Outcomes
The breast cancer screening outcome was defined as the proportion of women 40 years and older who had ever undergone mammography while cervical cancer screening outcomes were the proportion of women 18 years and older who had ever received Pap smear screening and the proportion that never had Pap smear screening.
Predisposing Factors
There were six predisposing factors assessed in the study including age, level of education, ethnicity, employment status, duration of years lived in the US and preferred language to discuss health matters. The number of years lived in the United States was coded dichotomously: “0” was assigned to individuals who lived in the United States less than 5 years, defined as “recent immigrants” for the purpose of this study and “1” was assigned to those who lived in the United States for 5 or more years, defined as “established immigrants”.
Need-for-Care Factors
To use health care services, individuals must perceive either illness or the need for preventive care. This was measured using self-reported perception of overall health. The question: “In general, would you say your health is? Excellent, very good, good, fair or poor” was used to assess the need-for-care factor. For analysis, the first three responses were grouped into the ‘good health’ category and the last two, the ‘poor health’ category.
Enabling Factors
The enabling factors assessed were: (1) Health care accessibility measured with the question: “How comfortable are you making an appointment with a doctor or other health care providers?” (2) Health care affordability, measured with the question: “During the past 12 months, how difficult has it been for you and your family to pay for health insurance premiums, co-pays and deductibles?” and (3) Trust in health care providers, measured by participants checking which of the following statements they most agreed with: (a) “My doctor always acts in my best interest”, (b) “My doctor usually acts in my best interest”, (c) “My doctor sometimes acts in my best interest” or (d) “My doctor rarely acts in my best interest”. Annual household income was omitted in this analysis, because more than 65 % of the participants in the study did not respond to the income question.
Statistical Methods
Descriptive statistics of demographics, perception of health, and utilization of the health care system were collected for age eligible African immigrant women who had screened and also for those never screened for breast or cervical cancer. We calculated mean and standard deviation (SD) for continuous variables and count and proportion for categorical variables. The relationships between demographics and perception of health and utilization of health care system to cancer screening status were examined using logistic regression analysis. Simple logistic regression was conducted first to look at the factors one at a time. Multiple logistic regressions models were then performed to assess the effect of each factor on the probability of ever having been screened after controlling for other factors. Final models were determined using stepwise selection. Using this effect-selection method, effects are entered and removed from the model in such a way that each forward selection step can be followed by one or more backward elimination steps, and the stepwise selection process terminates if no further effect can be added to the model or if the current model is identical to a previous visit model.
In our analysis, the significance level of the score Chi square either for entering an effect into the model in a forward selection step or for an effect to stay in the model in a backward elimination step was specified as 0.05. Odds ratio and its 95 % confidence interval from univariate analysis and final models were presented. A p value of less than 0.05 indicated statistical significance. In addition, for each cancer screening cohort, the fit of three sets of multivariate logistic regression models was measured by −2 log likelihood, Cox and Snell R square (i.e. coefficient of multiple determination) and Nagelkerke R square (i.e. adjusted coefficient of multiple determination), and improvement on model fit was evaluated using likelihood ratio test. The three sets of factors were [1] predisposing factors (demographics) only, [2] both predisposing and need for care factors, and [3] predisposing plus need for care plus enabling (utilization of the health care system) factors. SAS 9.2 (SAS Institute Inc., Cary, NC, USA) was used for the analysis.
Results
A total of 112 women age 40 and above were included in the analysis of breast cancer screening, and 421 women age 18 and above were included in the analysis of cervical cancer screening. Table 1 shows characteristics of participant in breast cancer screening analysis and how likely each characteristic was associated with ever having had mammogram. The mean age of the cohort was 52.7 years (SD = 10.1). Sixty-one percent (68/112) reported ever having had a mammogram. There were no differences in educational levels or employment status between those who have been screened and those who have never been screened. Results from simple logistic regression analysis (Table 1) show that ethnicity (Somali vs. other African immigrant groups) and duration of residence in the US (≤5 years vs. >5 years) were significantly related to ever having had a mammogram (p = 0.004 and <0.001, respectively). These two variables were the only significant factors in the final model of multivariate logistic regression analysis. The odds of ever having had a mammogram for Somali immigrants were 5 times greater than the odds for other African immigrant groups (odds ratio = 5.02, 95 % CI = 1.72–14.68, p = 0.003), while the odds of ever having had mammogram for recent immigrants were only 15 % of the odds for established immigrants (odds ratio = 0.15, 95 % CI = 0.05–0.46, p < 0.001).
Table 2 describes the characteristics of participants in cervical cancer screening analysis and the association between each characteristic and Pap smears in this cohort. The mean age of the cohort was 34.4 (SD = 13.2) years. Fifty-two percent (220/441) of the participants reported ever having had a Pap smear. There was no association (Table 2) between receiving Pap smear and age, level of education, perceived health status, or the identified enabling factors. Participants who were Somalis (p = 0.083), had lived in the United States for no more than 5 years (p < 0.001), were unemployed (p = 0.010), or had difficulty in paying health insurance premiums (p = 0.090) were less likely to have a pap smear done. Only duration of residence in the United States remained significant in relation to cervical cancer screening in the final model of multivariate logistic regression analysis. The odds of ever having had Pap smear screening for recent immigrants (≤5 years) were only 40 % of the odds for established immigrants (>5 years) (odds ratio = 0.40, 95 % CI = 0.24–0.65, p < 0.001).
Table 3 summarizes the fit of multivariate logistic regression models when different sets of factors were considered. The proportions of total variation explained by factors in set 1, 2 and 3 were 34, 36 and 38 %, respectively, for ever having had mammogram; and 9, 11 and 13 %, respectively, for ever having had Pap smear (Table 3, Nagelkerke R-squares). Results from likelihood ratio tests showed no significant improvement in the fit of the models for ever having had mammogram between every two sets (p = 0.235–0.647), while adding need for care factor (p = 0.026) or both need for care and enabling factors (p = 0.041) significantly improved model fit for ever having had Pap smear (Table 3).
Discussion
This study provides an analysis on breast and cervical cancer screening behavior among recent and more established age eligible African immigrants in the United States (US) using the revised behavioral model for vulnerable populations. The results of our study indicate that African immigrant women in Minneapolis and St. Paul have low breast and cervical cancer screening rates. This is consistent with prior studies showing that immigrant populations have lower rates for cancer screening [2, 8, 16]. A study conducted among Filipino and Korean immigrant women showed low rates of screening, with only 78 % of Korean women reporting mammogram screening for breast cancer [17, 18].
Furthermore, our study showed that African immigrant women who resided in the United States for less than 5 years were less likely to have had a mammogram or pap test done. Duration of residence in the US is a significant predictor of cancer screening [17]. Women with a longer duration of residence in the US were more likely to screen for breast and cervical cancer. This may be due to existing differences between women who have spent more time in US when compared to women who have been in the US for a shorter duration of time. Women who have spent more time in the US are more likely to be proficient in English, and more acquainted with and have better skills at navigating the seemingly complex US health system. They are also likely to be different in respect to cultural factors, concerns related to modesty and cancer screening knowledge [7, 19, 20].
Majority of women included in this analysis had health insurance with most of them under public health insurance. The State of Minnesota has subsidized health insurance known as MinnesotaCare which is available to both immigrant residents and low or moderate income families who have no health insurance [21].
Additionally, few women within this study identified difficulties with health care access. There is access to breast and cervical cancer screening through programs such as the Minnesota’s cancer screening program (SAGE), The Planned Parenthood or community/neighborhood clinics that provide reduced or no-cost services to low-income and uninsured patients. Services such as the SAGE program are targeted to increase access to cervical and breast cancer screening among uninsured women. Despite reports of high level of insurance and health care access, significant disparities in cervical and breast cancer screening still persist. While other studies among immigrants’ women showed consistent effects of age, education, and insurance status on cancer screening, this was not the case in our study [16, 22].
Our study showed Somali immigrant women had higher rates of mammogram use but lower rate of Pap testing when compared to other African immigrant women in the study. Pap smears are a more personal and invasive procedure that may pose particular cultural barriers and thus can hinder these women from obtaining services [23–25]. Previous studies have shown that gender of the health care provider impacts utilization of screening tools and opposite gender providers may increase anxiety. Immigrant women are culturally more likely to prefer female providers for their gynecologic care [23–25].
The strength of the study lies in the use of a conceptual model framework to explore factors impacting breast and cervical cancer screening behavior among African immigrant women. However several caveats apply in our study including, the limited sample size and the restriction of the data to urban areas in Minneapolis and St. Paul with the largest concentration of African Immigrant families. Those factors limit the generalizibility of the results. Secondly, the study was a secondary data analysis. Finally, use of mammograms or Pap tests was self-reported and may be subject to inaccurate recall.
Conclusion
Our study highlights several important factors that potentially could improve cancer screening among African immigrant women in Minnesota. Community-based educational interventions should focus on the need for screening among all immigrant women in a culturally sensitive manner. Future research should explore the impact of acculturation on cancer screening among recent immigrant women. Being a recent immigrant is a barrier to receiving cervical and breast cancer screening. Additional research incorporating need-for-care factors, personal health practices factors, predisposing and enabling factors is needed to explore causal factors for differences in cancer screening rates between recent and established immigrant women.
References
Bazargan M, Bazargan SH, Farooq M, Baker RS. Correlates of cervical cancer screening among underserved Hispanic and African-American women. Prev Med. 2004;39:465–73.
Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–40.
Goel MS. Racial and ethnic disparities in cancer screening. J Gen Intern Med. 2003;18:1028.
Grieco EM. US data sources on the Foreign Born and Immigration. Int Migr Rev. 2011;45:1001.
Ronningen B. Estimates of selected immigrant populations in Minnesota, 2004.
McPhee SJ. Barriers to breast and cervical cancer screening among Vietnamese-American women. Am J Prev Med. 1997;13:205.
Maxwell AE. Demographic predictors of cancer screening among Filipino and Korean immigrants in the United States. Am J Prev Med. 2000;18:62.
Carrasquillo O, Pati S. The role of health insurance on Pap smear and mammography utilization by immigrants living in the United States. Prev Med. 2004;39:943–50.
KagawaSinger M. Kagawa-singer: Asian American and Pacific Islander breast and cervical carcinoma screening rates and healthy people 2000 objectives. Cancer. 2000;89:696.
Skaer TL. Cancer-screening determinants among Hispanic women using migrant health clinics. J Health Care Poor Underserved. 1996;7:338.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10.
Aday LA. Health status of vulnerable populations. Annu Rev Public Health. 1994;15:487.
Gelberg L. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273.
Bazargan M, Johnson K, Stein J. Emergency department utilization among Hispanic and African-American under-served patients with type 2 diabetes. Ethn Dis. 2003;13:369–75.
Andersen R. A behavioral model of families’ use of health services. Research Ser. 1968;xi–111.
Echeverria SE, Carrasquillo O. The roles of citizenship status, acculturation, and health insurance in breast and cervical cancer screening among immigrant women. Med Care. 2006;44:788–92.
Maxwell AE, Bastani R, Warda US. Demographic predictors of cancer screening among Filipino and Korean immigrants in the United States. Am J Prev Med. 2000;18:62–8.
Lee H, Kim J, Han HR. Do cultural factors predict mammography behaviour among Korean immigrants in the USA? J Adv Nurs. 2009;65:2574–84.
Rajaram S. Rajaram: minority women and breast cancer screening: the role of cultural explanatory models. Prev Med. 1998;27:757–64.
Maxwell AE, Bastani R, Warda US. Misconceptions and mammography use among Filipino-and Korean-American women. Ethn Dis. 1998;8:377–84.
Miles SH. Health care reform in Minnesota. N Engl J Med. 1992;327:1092.
Rimer BK, Conaway MR, Lyna PR, Rakowski W, Woods-Powell CT, Tessaro I, et al. Cancer screening practices among women in a community health center population. Am J Prev Med. 1996;12(5):351–357.
Abdullahi A. Cervical screening: perceptions and barriers to uptake among Somali women in Camden. Public Health. 2009;123:680.
Cronan TA, Villalta I, Gottfried E, Vaden Y, Ribas M, Conway TL. Predictors of mammography screening among ethnically diverse low-income women. J Womens Health (Larchmt). 2008;17:527–37.
Bloom JR, Grazier K, Hodge F, Hayes WA. Factors affecting the use of screening mammography among African American women. Cancer Epidemiol Biomarkers Prev. 1991;1:75–82.
Acknowledgments
This work was supported in part by NIH P30 CA77598 utilizing the Biostatistics and Bioinformatics Shared Resource of Masonic Cancer Center, University of Minnesota. A special thanks to the African immigrant families for volunteering to participate in this study. We would also like to thank the leaders, organizers and staff members of the New Americans Community Services who aided in recruitment and data collection of the study. Special thanks to Mary Ellen-Berman, who critically reviewed and edited article draft.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harcourt, N., Ghebre, R.G., Whembolua, GL. et al. Factors Associated with Breast and Cervical Cancer Screening Behavior Among African Immigrant Women in Minnesota. J Immigrant Minority Health 16, 450–456 (2014). https://doi.org/10.1007/s10903-012-9766-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-012-9766-4