Abstract
The U.S. migrant and seasonal farmworker (MSFW) workforce is aging. Aging causes functional changes that can affect work performance and increase injury/accident risk. It also has been linked with deferred health-seeking. The exploratory study was conducted to investigate occupational injuries and health-seeking in Hispanic MSFW on the U.S.–Mexico border. Data were collected using an abbreviated Spanish-version of the California Agricultural Worker Health Survey. Nearly 60% of the 141 participants were middle-aged or older. Musculoskeletal injuries and those consistent with agrochemical and environmental exposures were common. Farmworkers aged >40 years were 2.5–5 times more likely than younger MSFW to report persistent single and multiple injuries involving the knees, shoulder, feet, and hands. Except for neck and back injuries, few received any medical treatment. Although many self-treated with traditional home remedies, few used CAM practitioners. The study findings highlight the multiple workplace health and health-seeking challenges faced by aging immigrant MSFW.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The 1.01–3 million migrant and seasonal farm workers (MSFW) who are employed on U.S. farms [1, 2] play an essential role in supporting the nation’s multibillion dollar fruit, vegetable and nut crop industries and assuring population access to a safe and nutritious food supply [3]. Longitudinal data collected by the National Agricultural Worker’s Survey (NAWS) since 1989 confirms that the predominantly Mexican immigrant labor force is aging but the proportion of older workers varies by geographic region and labor stream [4]. It also indicates that the NAWS Southwest region (Texas, New Mexico, Arizona, Oklahoma), has the highest proportion of middle-aged and elderly MSFW in the U.S. [4]. Fifty-two percent were ≥40 years of age, 25% were ≥50 years, and 9% were ≥60 years [4]. Published data from several surveys conducted in the Desert Southwest border region of Texas, New Mexico, and Arizona also indicate that MSFW tend to be older than those in other areas [5–7]. Likewise, the Midwest labor stream has a high proportion of MSFW aged 40 years and older [4].
Cultivating and harvesting agricultural crops requires physically demanding manual labor performed outdoors under often harsh environmental conditions. Farmworkers are regularly exposed to a variety of mechanical, chemical, and environmental stressors that increase their risk for sprains, strains, fractures and other musculoskeletal injuries [8–13], pesticide poisoning [6, 10, 11, 14, 15], sunstroke, dehydration [16–18], and other work-related injuries [1, 7, 10, 11, 19–22]. Although little is known about the occupational health challenges of aging MSFW, studies of workers employed in other intensive manual occupations suggest that changes in physiological and cognitive functioning associated with aging can reduce physical work capacity and increase susceptibility to musculoskeletal and other injuries [23–27]. In addition, as individuals age, chronic conditions (i.e., arthritis, obesity, diabetes, hypertension), decreased vision, hearing, and balance become more common. This can make it more difficult for MSFW to safely and efficiently perform work tasks [24, 28, 29]. Furthermore, the type and intensity of agricultural work demands can aggravate chronic conditions further impeding safe work performance and increasing injury risk [23, 24].
Many Hispanic MSFW appear to receive little or no medical treatment for their work-related injuries, and if they do, it may be delayed or limited [9, 10, 13, 30]. The health-seeking patterns of aging MSFW have not yet been investigated but diagnosis and treatment delays are reported as more common among older persons suffering from low back pain [31] and other chronic illness [32–34] compared to those who are younger. It is important to explore these issues in aging MSFW since deferrals in health-seeking have the potential to prolong pain, delay recovery time and result in poorer clinical outcomes.
Many MSFW use complementary and alternative medicine (CAM) and over-the-counter remedies to treat illness. However, similar to other Hispanic groups [35–37], the specific methods, usage frequency, and conditions under which CAM methods are employed appears by MSFW group and illness [10, 13, 35, 38, 39]. It has been reported that older foreign-born immigrants appear to preferentially use CAM [35] but it is uncertain whether this is also the case for aging MSFW. The study of the usage patterns for CAM, home remedies, and other form of self-treatment for occupational injuries and other conditions can provide useful information for health agencies and providers involved in the MSFW care.
The exploratory study investigated the occupational health challenges and health-seeking reported by aging immigrant MSFW on the U.S.–Mexico border. It specifically investigated the type and frequency of farmwork-related musculoskeletal and other injuries in MSFW ≥40 years with their younger counterparts. In addition, the study explored the health-seeking of farm workers specific to work-related injuries and other types of illnesses and conditions including conventional medical (i.e., allopathic, osteopathic), CAM practitioners, traditional home remedies, and over-the-counter methods.
Materials and Methods
Study Site and Participants
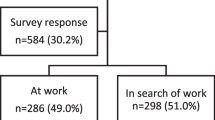
The present work was part of a larger study of the household food security, nutrition, and health of MSFW [40] carried out during a 10-month period in 2003 in two contiguous border counties (El Paso County, Texas, and Dona Ana County, New Mexico). An estimated 12,000 MSFW cultivate and harvest chile and other crops (i.e., onions, cotton, lettuce, pecans) in the region. A site-based convenience sampling strategy was used to recruit prospective households. This previously described strategy is recommended for use in hard to sample groups such as the farmworker households sampled in the present work [40]. Briefly, prospective households were recruited through several MSFW-serving organizations and agencies in the two local counties. Those who noted an interest in taking part in the study were subsequently visited by the study team in a location they specified (e.g., home, migrant farmworker center, community center, etc.).
Adults aged ≥18 years who had performed paid farm work during the previous 12-month period and did not have any sensory or developmental conditions that would impede their ability to understand and answer questions were eligible to participate. The protocol for the study was approved by the University of Texas at El Paso (UTEP) Institutional Review Board (protocol #1669). One hundred forty-one adults living in 100 MSFW households agreed to participate and went through the written informed consent process. Study households were compensated for their time with free $20 food baskets. Household members also were given free anthropometric, blood pressure, and blood hemoglobin, glucose and lipid profile examinations. The exam results were explained to them (oral and written) and in the case of an abnormal finding, they were referred to free/low cost medical clinics in their local communities.
Data Collection
The occupational health and health-seeking issues of study participants were explored using an abbreviated California Agricultural Worker Health Survey (CAWHS) main instrument and male and female health supplements [41]. The survey data were collected in face-to-face interviews from participants by trained bilingual, bicultural interviewers from the local area who were native Spanish speakers. Closed and open-ended questions were used to collect data on participant and household sociodemographic characteristics (e.g., age, gender, ethnicity, education, marital status, household size, and composition), living conditions, migration patterns, work history, medically diagnosed health conditions (e.g., arthritis, hearing and vision problems, skin conditions). They also were questioned about ethnospecific illnesses. Ethnospecific or folk illnesses are culturally defined conditions that form part of the belief systems of ethnic groups. Examples of common ethnospecific illnesses associated with Mexican culture include conditions such as “nervios,” “susto”, “latidos” [42].
Participants also were questioned about any farm work-related musculoskeletal strains and sprains that they may have experienced during the prior 12 months that persisted for one or more weeks, the specific type and location of any such injury(s), whether they still had current pain at that site, and how long the pain had lasted. The CAWHS instrument restricted the time frame to the previous 12 months to differentiate recent work-related injuries from those injuries that occurred in the past [41]. The participants also were questioned as to whether they had been treated for these musculoskeletal injures and if so, what type of treatment they had received. Other questions asked participants about traumatic injuries and other symptoms they may have experienced during the previous 12-month period while performing agricultural work (e.g., skin irritation, cloudy vision, eye irritation, headache, dizziness, dehydration). If they replied in the affirmative, they were asked to describe under which circumstances these had occurred. Other data were gathered on health-seeking for work-related and other conditions including their use of conventional medical care, complementary and alternative medicine (CAM), and self-treatment modalities on both sides of the U.S.–Mexico border.
Data Analysis
Categorical data are described as % (n) or % (nl sample size) in cases where a subset of the study sample was used. Continuous data are described as means ± SD. The bivariate associations of participant characteristics with reported injuries were examined with logistic regression. These were used to calculate odds ratios and their 95% confidence intervals. Content analysis was employed to analyze the qualitative data from the open-ended questions.
Results
Table 1 displays the characteristics of the 141 MSFW study participants. As shown, the majority of the poorly educated, married, Mexican-born immigrant farmworkers were middle-aged or older (\( \bar{x} \) = 42.5 ± 14.3 years). The average size of their households was 4.4 ± 2.4 members.
The participants indicated that had performed paid farm work in the U.S. for an average of 18.8 ± 11.7 (range: 8.4 months to 58.0 years). At the time of their interview, they also reported that they had been employed for 3–10 months on local Paso del Norte region farms during the previous 12-month period. During this period, they noted working an average of 4.9 ± 1.5 days/week during the season planting, cultivating, and/or harvesting chiles, onions, and other crops such as lettuce, cabbage and pecans.
Farm Work-Related Injuries
Persistent Musculoskeletal Injuries
Table 2 displays the frequency and characteristics of persistent musculoskeletal injuries reported by the MSFW for the prior 12 month period. The most commonly reported injuries were those of the knee and back which affected 40–50% of participants. Those affected attributed their strain and sprain injuries to lifting heavily loaded baskets and sacks of agricultural crops onto truck beds or spending prolonged time bending over, kneeling, squatting, or in other awkward or uncomfortable positions while carrying out agricultural tasks. At the time of their interview, 20.3–37.8% indicated that they were continuing to experience pain at the affected injury site(s).
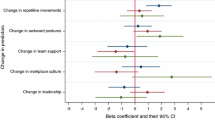
As Table 3 reveals, middle-aged and elderly MSFW (≥40 years) were more likely than younger ones to report persistent work-related injuries of the hand, knee and foot. They also were more likely to report multiple musculoskeletal injuries compared to their younger counterparts. Male farmworkers were more likely than female farmworkers to report suffering a persistent back or knee injury. None of the other participant characteristics measured in the study were associated with the risk for musculoskeletal injuries.
Other Work-Related Injuries
As Fig. 1 shows, participants also reported that they had experienced other types of injuries such as serious cuts/lacerations, contusions/abrasions, and bone fractures during the prior 12 months while working in the fields and/or traveling to and from their farm work sites. Other types of farmwork-related injuries during this time period included eye irritation, itching, or tearing, cloudy/blurry vision, paresthesias, headaches, allergic reactions, dizziness, skin irritation, diarrhea, dehydration, and nausea/vomiting. They attributed these to prolonged exposure to agricultural chemicals, harsh desert conditions (e.g., sun, wind, low humidity), and/or insect stings and bites. Different from what was reported for persistent musculoskeletal injuries, neither age, gender, nor other participant characteristics were associated with these types of work-related symptoms.
Health-Seeking
Occupational Health-Seeking for Recent Persistent Musculoskeletal Injuries
Two-thirds of the study participants who suffered a farm work-related persistent back injury during the past 12 months and all of those with a neck injury reported they had been treated for their problem by a conventional medical practitioner such as a physician, nurse, or physician’s assistant (Table 2). In contrast, only around one-quarter of those with a persistent knee, hand, shoulder, hand and/or foot injury received any medical treatment. Instead, they tended to self-treat their injuries using heating pads, ice packs, self-massage, over-the-counter anti-inflammatory remedies, and commercially available salves (e.g., Bengay, Icy-Hot). Participants who were treated for a persistent musculoskeletal injury by a conventional medical practitioner said their care was received at a medical clinic (64.2%; 34/53), the office of a private physician (24.5%; 13/53), or a hospital emergency room (11.3%; 6/53). None of the study participants reported receiving any physical or occupational therapy for their injuries. Age, gender, and other participant characteristics were not associated with reported patterns of treatment for persistent musculoskeletal occurring in the previous 12 month period.
General Health-Seeking Patterns
Conventional Medical Care
Participant use of conventional medicine and CAM modalities for various health conditions was next explored to better understand their health-seeking patterns. The study participants reported that the timing of their last visit to a conventional medical practitioner occurred an average of 28.4 ± 74.5 months prior to the interview. Seventy percent of the 141 study participants indicated that their last medical visit had taken place across the border in Mexico and 92 had an explanation for why they had sought out health care in Mexico. As Fig. 2 shows, most common reasons given were the lower cost of services and medicine in Mexico, the ability to obtain a faster appointment from Mexican health care providers, the greater convenience of health care on the Mexican side of the border and the fact that Mexican health care providers better understand their needs. Only a few mentioned they had sought out health care in Mexico because they lacked U.S. health insurance or familiarity with the U.S. health care system.
The study participants were next questioned about how they had paid for the cost of their last health care visit. The majority (77.2%) indicated that they had paid out-of-pocket as they were not covered by either U.S. or Mexican health insurance. The others reported that it had been covered through the Mexican Social Security Institute (12.8%), another Mexican public health program (2.8%), or U.S. Medicaid or Medicare (7.1%). The reported timing of the last health care visit, the site or cost coverage of the visit, or the reasons for seeking health care in Mexico were not associated with age nor other participant characteristics.
Complementary and Alternative Medicine Use
As Table 4 indicates, only a minority of study participants reported using the services of a chiropractor or other CAM practitioner such as a huesero/fregador (joint/bone setter/massage therapist), curandero (spiritual healer), or yerbero (herbalist) to treat or prevent illness. Those who used chiropractic services said they did so mainly to treat work-related injuries. Several also admitted to using hueseros/fregadors for the same purpose. The few who used curanderos and herbalists said they mostly did so for the treatment of fatigue/malaise, genitourinary problems, and ethnospecific illnesses.
Slightly more than half of participants admitted to using medicinal plants and other traditional remedies to self-treat or prevent respiratory and gastrointestinal complaints and to a lesser extent, other conditions such as arthritis/rheumatism and musculoskeletal problems, headaches, fever, and other ailments (Table 4). The reported average frequency of use varied from only a few times a year (44%) to monthly (19.2%), weekly (17.9%) or daily (19.2%). Figure 3 displays the reasons reported by the participants for self-treating with traditional home remedies. These two most frequent reasons noted were the lower cost and greater convenience or greater familiarity with traditional home remedies for treating illnesses. The other reasons noted by participants were the greater usefulness of these methods for treating minor illnesses or using in an adjunctive capacity, superior treatment effects as indicated by more rapid effectiveness and/or fewer secondary effects, and greater ability to prevent illnesses. Age, gender, and other participant characteristics were not associated with reported patterns of CAM use including type, frequency, and rationale for their use.
Discussion
The findings from this exploratory study highlight the occupational health challenges and health-seeking of aging Hispanic immigrant farmworkers. The study of this economically significant group and their occupational and other health issues is important because the proportion of middle-aged and elderly individuals in the national farm labor force has been steadily increasing over the past decade [4]. In some areas of the country, individuals aged ≥40 years constitute as much as 40–60% of the MSFW workforce [4–7].
It has been reported that changes in functional capacity, especially those related to physical ability, start to decline around the age of 30 years. These age-related declines become readily apparent by a person’s forties and fifties especially if the physical demands of the workplace do not decrease [43]. Decreased physical work capacity increases the risk for musculoskeletal sprains and strains. Aging is associated with reductions in muscular strength, aerobic capacity, agility, balance, vision, hearing and other attributes [23]. Aging workers are especially susceptible to injuries caused by chronic muscle fatigue due to the longer recovery time they require [24]. Our study results suggest that MSFW aged ≥40 years have an elevated burden of musculoskeletal injuries since persons in this age group were 2.5–5 times more likely than younger individuals to report suffering from persistent injuries of the knees, hands, and feet as well as injuries involving multiple sites. The prevalence of persistent musculoskeletal injuries was elevated compared to figures reported in a study for a younger group of California Hispanic MSFW which used the same CAWHS instrument [41]. Although previous studies have not specifically focused on musculoskeletal injuries among aging MSFW, the increased prevalence of sprains and strains identified among the study participants is consistent with reports published on aging farmers [44, 45], construction workers [23], and other persons in heavy manual occupations [24, 26].
Studies of workers in diverse occupations suggest that age-related decreases in healing ability also mean that older individuals often require additional time to recuperate from musculoskeletal injuries [23, 46, 47]. However, for most MSFW, regardless of their age and physical condition, taking time off to seek treatment and recuperate is infeasible because of the intensive seasonal demands of crop cultivation and harvesting coupled with their precarious financial situations [19, 48–50]. When farm workers are unable or unwilling to take needed time off from their jobs to seek treatment and/or recuperate, their injuries may become chronic or incapacitating.
The study findings also indicated that other types of farm work-related injuries were common but different from persistent musculoskeletal strains and sprains, these equally affected older and younger workers alike. The specific respiratory, dermal, gastrointestinal, central nervous system and ocular injuries the study participants identified are consistent with those noted for other U.S. farmworker groups [10, 11, 20, 22, 48–50]. The reported symptoms were consistent with exposure to air-, soil-, and plant-borne pesticides, herbicides, fungicides, fertilizers, and other toxic agrochemicals. It is also possible that some of these symptoms could be the result of the harsh environmental conditions under which agricultural workers labor. These frequently expose them to excessive sun and heat, high aridity, aerosolized dust, and venomous insects. The adequate prevention and prompt treatment of agrochemical and environment-related injuries is important for all adult farm workers but particularly so for older individuals due to their increased vulnerability to chemical toxins, heat stroke, and dehydration, among others.
Our study results are consistent with prior reports indicating that medical treatment for the job-related injuries incurred by MSFW is frequently delayed, inadequate or absent [1, 10, 19, 30, 48–50]. Similar to reports for other farmworker groups, the majority practiced self-treatment of their work-related and other conditions themselves using a variety of over-the-counter analgesics, topical preparations, and massage or heat/cold therapy [10, 38, 50]. Although our a priori expectation was that farmworkers who were older, female, or had been in the U.S. for a shorter period of time would be more likely to use traditional home remedies to self-treat their injuries and other illnesses than others, this was not the case. One reason for this may be the multiple economic, legal, linguistic, and other barriers that limit the access of immigrant MSFW to medical treatment [1, 19, 48, 49], no matter their age or other characteristics. In addition, they and other Mexican-born immigrants frequently have conceptualizations about work safety, health, and illness [19, 39, 51–54] that differ from those of their US-born employers and health care providers. In turn, U.S. health care providers may not be familiar with their specialized occupational and other health care needs [22, 50, 51, 55]. This combination of factors has the potential to reduce access to medical care for the work-related and other health conditions that disproportionately affect all immigrant farmworkers [11, 19, 54]. Timely access to appropriate medical care is especially needed for aging farmworkers because of their high burden of musculoskeletal injuries and other chronic conditions.
The potential limitations and strengths of this study should be taken into account when interpreting its results. The sample size of 141 participants was relatively small. In addition, the non-random sampling procedure used to identify and recruit this hidden immigrant population may have reduced sample representativeness. However, participant ethnicity, age, education, immigration, and other major characteristics are consistent with those previously reported farmworkers in the Southwest region [4–7]. It is also possible that the burden of work-related injuries might have been under-estimated due to survivor bias since persons with severe injuries or other illnesses that did not allow them to work would have been underrepresented in the study. Although self-reports are potentially subject to recall and other forms of bias, the CAWHS survey instrument used a restricted time frame to help distinguish recent injuries from those that occurred in the past [41]. In addition, the CAWHS was specifically developed for and validated in MSFW of Mexican-origin. It was administered in the preferred language of the participants (Spanish) by trained bilingual, bicultural interviewers which increases confidence that measurement and interpretative bias were minimized.
The CDC/NIOSH has identified the musculoskeletal and other work-related health challenges of aging workers as a high priority area for research [56]. Aging is associated with changes in physiological, cognitive, and psychosocial functioning that can affect occupational performance and increase the risk for injuries and accidents. However, prior studies have not addressed the occupational health challenges of the growing proportion of middle-aged and elderly individuals working in migrant and seasonal farm labor in the U.S. This information is needed to help support evidence-based occupational health practice and policy for this economically important labor force.
The data from this exploratory study were used to inform a new binational study now being conducted on both sides of the U.S.–Mexico border. The study is focused on the impact of aging on the physical functioning (i.e., mobility, flexibility, muscle strength, balance, posture, pain), occupational exposures and injury, and psychosocial function in MSFW aged 40 years and older. In addition, it is also exploring health-seeking and health care access changes that may have occurred subsequent to the onset of drug-related violence along the border.
References
Kandel W. A profile of hired farm workers: a 2008 update. United States Department of Agriculture, Economic Research Service. Econ Res Rep. 2008;60:1–59.
National Center for Farmworker Health. Facts about MSFW. 2009. http://www.ncfh.org/docs/fs-Facts%20about%20MSFW.pdf. Accessed 1 May 2010.
United States Department of Agriculture. Economic Research Service. Fruit and nut trees. Background. http://www.ers.usda.gov/Briefing/FruitandTreeNuts/Background.htm. Accessed 1 May 2010.
United States Department of Labor. The national agricultural worker survey, 1989–2006. Public database. http://www.doleta.gov/agworker/naws.cfm. Accessed 3 May 2010.
Nolte KD, Fonseca JM. Vegetable field workers provide insight for improving farm labor retention at the US-Mexican border. J Agric Ext Rural Develop. 2010;2(5):64–72.
Poss J, Pierce R. Characteristics of selected migrant farm workers in West Texas and Southern New Mexico. Calif J Health Promot. 2003;1(2):138–47.
Robson M, Schneider D, Marentes C, Villanueva E. Field conditions for agricultural workers in the El Paso, Texas region. New Solut J Environ Occup Health Policy. 2001;11:141–8.
Shipp EM, Cooper SP, del Junco DJ, Delclos GL, Burau KD, Tortolero S, Whitworth RE. Chronic back pain and associated work and non-work variables among MSFW from Starr County, Texas. J Agromed. 2009;14(1):22–32.
Brower MA, Earle-Richardson GB, May JJ, Jenkins PL. Occupational injury and treatment patterns of MSFW. J Agromed. 2009;14(2):172–8.
Anthony MJ, Martin EG, Avery AM, Williams JM. Self care and health-seeking behavior of migrant MSFW. J Immigr Minor Health. 2010;12:634–9.
Villarejo D, McCurdy SA. The California agricultural workers health survey. J Agric Saf Health. 2008;14(2):135–46.
McCurdy SA, Samuels SJ, Carroll DJ, Beaumont JJ, Morrin LA. Agricultural injury in California migrant Hispanic farm workers. Am J Ind Med. 2003;44(3):225–35.
Cooper SP, Burau KE, Frankowski R, Shipp EM, Del Junco DJ, Whitworth RE, Sweeney ME, Macnaughton N, Weller NF, Hanis CL. A cohort study of injuries in migrant farm worker families in South Texas. Ann Epidemol. 2006;16(4):313–20.
McCauley LA, Anger WK, Keifer M, Langley R, Robson MG, Rohlman D. Studying health outcomes in farmworker populations exposed to pesticides. Environ Health Perspect. 2006;114(6):953–60.
Arcury TA, Grzywacz JG, Isom S, Whalley LE, Vallejos QM, Chen H, Galván L, Barr DB, Quandt SA. Seasonal variation in the measurement of urinary pesticide metabolites among Latino MSFW in eastern North Carolina. Int J Occup Environ Health. 2009;15(4):339–50.
Luginbuhl RC, Jackson LL, Castillo DN, Loringer KA. Heat-related deaths among crop workers-United States, 1992–2006. MMWR. 2008;57(24):649–53.
Salas R. Sun-protective behaviors in California MSFW. J Occup Environ Med. 2005;47:1244–9.
Mirabelli MC, Quandt SA, Crain R, Grzywacz JG, Robinson EN, Vallejos QM, Arcury TA. Symptoms of heat illness among Latino farm workers in North Carolina. Am J Prev Med. 2010;39(5):468–71.
Arcury TA, Quandt SA. Delivery of health services to MSFW. Annu Rev Public Health. 2007;28:345–63.
Lacey SE, Forst LS, Petrea RE, Conroy LM. Eye injury in migrant farm workers and suggested hazard controls. J Agric Saf Health. 2007;13(3):259–74.
Rabinowitz PM, Sircar KD, Tarabar S, Galusha D, Slade MD. Hearing loss in migrant agricultural workers. J Agromed. 2005;10(4):9–17.
National Center for Farmworker Health. Occupational health and safety, 2009. http://www.ncfh.org/docs/fs-Occ%20Health.pdf. Accessed 18 Nov 2010.
Crawford JO, Graveling RA, Cowie HA, Dixon K. The health safety and health promotion needs of older workers. Occup Med. 2010;60:184–92.
De Zwart BC, Frings-Dresen MHW, van Duivenbooden JC. Senior workers in the Dutch construction industry: a search for age-related work and health issues. Exp Aging Res. 1999;25(4):385–91.
van den Berg TI, Elders LA, de Zwart BC, Burdorf A. The effects of work-related and individual factors on the work ability index: a systematic review. Occup Environ Med. 2009;66(4):211–20.
Kenny GP, Yardley JE, Martineau L, Jay O. Physical work capacity in older adults: implications for the aging worker. Am J Ind Med. 2008;51(8):610–25.
Silverstein M. Meeting the challenges of an aging workforce. Am J Occup Med. 2008;51:269–80.
Li X, Gignac MA, Anis AH. The indirect costs of arthritis resulting from unemployment, reduced performance, and occupational changes while at work. Med Care. 2006;44(4):304–10.
Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the U.S. workforce. JAMA. 2003;290(18):2443–54.
Ciesielski S, Hall SP, Sweeney M. Occupational injuries among North Carolina migrant MSFW. Am J Pub Health. 2001;81(7):926–7.
Knauer SR, Freburger JK, Carey TS. Chronic low back pain among older adults: a population-based perspective. Aging Health. 2010;22(8):1213–34.
Nguyen HL, Saczynski JS, Gore JM, Goldberg RJ. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes. 2010;3(1):82–92.
Tannenbaum C, Frank B. Masculinity and health in late life men. Am J Men Health. 2010. doi:10.1177/1557988310384609.
Mackenzie CS, Gekoski WL, Knox VJ. Age, gender, and the underutilization of mental health services: the influence of help-seeking attitudes. Aging Ment Health. 2006;10(6):574–82.
Loera JA, Reyes-Ortiz C, Kuo YF. Predictors of complementary and alternative medicine use among older Mexican Americans. Complement Ther Clin Pract. 2007;13(4):224–31.
Dente JM, Herman CJ, Allen P, Hunt WC. Ethnic differences in the use of complementary and alternative therapies among adults with osteoarthritis. Prev Chronic Dis. 2006;3(3):1–15.
White B, Knox L, Zepeda M, Mull D, Nunez F. Impact of immigration on complementary and alternative medicine use in Hispanic patients. J Am Board Fam Med. 2009;22(3):337–8.
Poss J, Pierce R, Prieto V. Herbal remedies used by selected migrant MSFW in El Paso, Texas. J Rural Health. 2005;21(2):187–91.
Pylypa J. Self-medication practices in two California Mexican communities. J Immigr Health. 2001;3(2):59–75.
Weigel MM, Armijos RX, Hall YP, Ramirez Y, Orozco R. The household food insecurity and health outcomes of US-Mexico border MSFW. J Immigr Minority Health. 2007;9(3):157–69.
California Institute for Rural Studies (CIRS). California Agricultural Worker Health Survey (CAWHS). Suffering in silence: a report on the health of California’s agricultural workers. 2002. http://www.calendow.org/reference/publications/pdf/agricultural/AgrWorkersSurveyver012301.pdf. Accessed 3 May 2010.
Foster GM, Anderson BG. Ethnomedicine. In: Medical anthropology. New York: Wiley; 1978. p. 51–80.
Ilmarinen J. Aging workers. Occup Environ Med. 2001;58:546. doi:10.1136/oem.58.8.546.
Voaklander DC, Umbarger-Mackey ML, Wilson ML. Health, medication use and agricultural injury: a review. Am J Ind Med. 2009;52:876–89.
Davis KG, Kotowski SE. Understanding the ergonomic risk for musculoskeletal disorders in the United States agricultural sector. Am J Ind Med. 2007;50:501–11.
Wegman DH. Older workers. Occup Med. 1999;14(3):537–57.
Wegman DH, McGee JP, editors. Health and safety of older workers. Washington, DC: National Research Council and Institute of Medicine of the National Academies. The National Academies Press; 2004.
Villarejo D. The health of U.S. hired farm workers. Ann Rev Public Health. 2003;24:175–93.
Hansen E, Donahue M. Health issues of MSFW. J Health Care for Poor Underserv. 2003;14(2):153–64.
Arcury TA, Vallejos QM, Feldman SR, Quandt SA. Treating skin disease: self-management behaviors of Latino farmworkers. J Agromed. 2006;11:27–35.
Holmes SM. An ethnographic study of the social context of migrant health in the United States. PLoS Med. 2006;36(10):1776–93.
Clingerman EM. Conceptualizations of health among Mexican and Mexican-American women employed in migrant farm work. Hispanic Health Care Int. 2006;4(1):45–55.
Feldman SR, Vallejos QM, Quandt SA, Fleischer AB Jr, Schulz MR, Verma A, Arcury TA. Health care utilization among migrant Latino MSFW: the case of skin disease. J Rural Health. 2009;25(1):98–103.
Lashuay N, Harrison R. Barriers to occupational health services for low-wage workers in California: a report to the commission on health and safety and workers compensation, California Department of Industrial Relations. http://www.dir.ca.gov/chswc/reports/barriers_to_ohs.pdf. Accessed 15 Nov 2010.
Villarejo D, McCurdy SA, Bade B, Samuels S, Lighthall D, Williams D. The health of California’s immigrant hired MSFW. Am J Ind Med. 2010;53:387–97.
Centers for Disease Control and Prevention. National Institutes of Occupational Safety and Health. Occupational health disparities. Occupational safety and health risks. http://www.cdc.gov/niosh/programs/ohd/risks.html. Accessed 14 May 2010.
Acknowledgments
Project funding provided by the Office of Rural Health Policy (ORSP) Special Projects, Health Resources and Services Administration, Department of Health and Human Services, ‘‘Migrant Border Health Initiative’’ (AHQR 02EM000075F2).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Weigel, M.M., Armijos, R.X. Exploratory Study of the Occupational Health and Health-Seeking of Migrant and Seasonal Farmworkers on the U.S.–Mexico Border. J Immigrant Minority Health 14, 648–656 (2012). https://doi.org/10.1007/s10903-011-9503-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-011-9503-4