Abstract
The present study investigated the link between the sizes of the Chinese community to the health of Chinese seniors in Canada. A secondary data analysis of survey data from a representative sample of 2,272 Chinese older adults aged 55 and over was conducted. Hierarchical regression analyses were performed to assess the effects of the size of Chinese communities in Chinese seniors’ health. Chinese seniors residing in the community with a small Chinese population reported better physical and mental health than the Chinese seniors residing in communities with a larger Chinese population. The findings were contrary to expectations that health of Chinese seniors should be higher in cities with large Chinese communities. These findings raise new questions for future investigations into the dynamics and impact of ethnic community size, and the importance of studying intragroup differences within ethno-cultural groups to better understand health disparities in ethnic groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The growth in migration, long-term settlement, and aging of immigrants and non-immigrants in Canada has implications for the availability and accessibility to health and social care services that meet the needs of diverse service users. In Canada, Chinese people aged 65 and over make up 11% of the Chinese Canadian community [1]. Many of these Chinese seniors are immersed in their respective communities in various Canadian cities [2–7]. These communities are built on a firm foundation by which Chinese Canadians maintain their cultural identity and practices, regardless of their length of residence and immigrant status [5]. In the context of aging, Chinese communities or “ethnic enclaves” are considered beneficial to Chinese seniors because of the ease of access to culturally and linguistically appropriate resources [2, 3, 8–14].
Researchers have documented that visible, ethnic minority groups, such as the Chinese seniors, experience cultural barriers to service access that may lead to foregone care and health disparities [10, 11, 15–17]. However, there are more than individual level factors at play in the occurrence of health disparities. From a social determinant of health perspective, the size of the ethno-cultural community, or ethnic group density, may be relevant to understanding its effects on health. Presently, a small number of studies suggest there might be a protective effect between ethnic group density and the health and wellbeing of the group members [18–20]. More research evidence is needed though to verify the strength and presence of this effect, and to expand the knowledge base for professional practice and policy making. The present study aims to contribute to the literature on the influence of ethnic group density on health by studying the effect of the size of the Chinese community on the health of Chinese seniors in Canada.
Conceptual Framework: Ethno-Cultural Communities, Health, and Well-Being
It is natural for ethno-cultural minorities to seek social support from other members in their groups [14, 21–25]. Participating and belonging in one’s community are associated with positive health outcomes [21, 26–29]. Social cohesion among community members, through social bonds, buffers the effects of stress and provides resources and assistance in times of need [25, 28, 30–32]. Social bonds become structures of social organization by which health-enhancing resources may be accessed [28, 33–36]. Research on Chinese seniors in Canada and elsewhere show the importance of culture and social supports to their health and well-being [2, 8–14, 37–41].
Segregation and racism has historically contributed to creating Chinese “ethnic enclaves” [42] in Canada. The “ethnic enclaves” offered immigrants, new and settled, a space of belonging, and access to cultural resources in various life domains [5, 6, 21, 43, 44]. Well-established ethnic enclaves have a stable ethnic economy arising from professional, commercial, and other goods and services that meet the needs of the community, as well as to outsiders (e.g., broader community) [45]. A major benefit is the social and physical space for respite from race-based hostility and discrimination by members outside the Chinese community [6, 21, 42, 43, 46]. During times of transition (i.e., immigration), engagement in one’s ethno-cultural community may provide stability, and facilitate individual and community growth by guiding behaviors according to culturally based values and beliefs [47]. The largest concentration of Chinese people in Canada resides in the cities of Toronto and Vancouver. In these cities, the Chinese community exists beyond the “ethnic enclaves” and borders of Chinatown(s) spreading into urban and suburban areas. This wide spread of Chinese residents has meant that businesses and services are also spread out and not localized to only one central geographic area, as is the case of cities with a smaller Chinese population size (e.g., Winnipeg, Edmonton, Victoria). The availability and accessibility to multiple sites of cultural spaces and practices are beneficial to Chinese seniors’ quality of life [13].
The presence of large, well-established ethno-cultural communities are presumed to offer social, economic, and cultural resources that will expedite settlement and social integration of minorities in the host society [24, 44, 48, 49]. According to Pickett and Wilkinson’s recent review of studies on ethnic density and health, ethnic density has a positive effect on mental health and physical health [18]. Individuals living in high ethnic group density contexts have better psychological health and lower incidences of psychotic disorders than individuals who live in low ethnic group density contexts [20, 50]. Although studies of ethnic group density and physical health are few in number, these studies also suggest there is a protective effect [18, 51].
Methods
Participants
The data for this study were originally collected in a larger study examining health and well-being of aging Chinese Canadians [12] 55 years and older in seven major Canadian cities: Victoria, Vancouver, Calgary, Edmonton, Winnipeg, Montreal, and Toronto. Telephone numbers listed with a Chinese surname in all research sites comprised the sampling frame. The method of using surnames as identifiers to find Chinese and other Asian participants has been established as an effective sampling approach [52–54]. However, this method excluded households without a telephone, unlisted telephone numbers, individuals with non-Chinese surnames, and mixed ethnicity households in which the non-Chinese member’s name was used for registering the telephone number. A total of 40,654 telephone numbers were randomly selected from the 297,064 numbers listed with a Chinese surname. Trained interviewers conducted telephone screenings to identify eligible participants who were ethnic Chinese 55 years or older. The telephone screening resulted in identifying 12,621 Chinese households, of which 2,949 eligible individuals were identified and invited to participate in a face-to-face interview at the participant’s home or at one of the community organizations. In households with more than one eligible participant, the rolling dice method was used to select only one participant.
Data Collection
The Research Ethics Boards of the universities the researchers were affiliated with approved the study. Data collection occurred between summer 2001 and spring 2002, using a verbally administered structured questionnaire conducted in English or a Chinese dialect. The questions were constructed in Chinese, translated into English, and back translated to Chinese to ensure accuracy in meaning in both versions. For standardized instruments that had a Chinese version, the Chinese version was used. Interviews were conducted in the respondents’ language of choice, which included English, Cantonese, Shanghainese, Fukienese, Mandarin, Hakka, and Chiu Chow. A total of 2,272 participants completed the questionnaire, representing a response rate of 77%.
Measures
In this study, health status referred to both physical and mental health, and was measured by a Chinese version of the Medical Outcome Study 36-item Short Form (SF-36) [55, 56]. The SF-36 is a well-established standardized health assessment instrument that has been used with ethnically and culturally diverse samples [57–61], and has previously been adapted and translated into Chinese [55, 56]. The PCS (Physical Component Summary) and the MCS (Mental Component Summary) are two summary scores which were calculated using the norm-based scoring method suggested in the manual [59]. The scores range from 0 to 100, with higher scores indicating better health status. The Cronbach’s alphas for the PCS and MCS scales in this study were 0.90 and 0.84.
Size of the Chinese community was the key predictor variable for health status. The study’s participants were divided into three groups according to the size of the Chinese population in the seven Census Metropolitan Areas reported in the 2001 Canadian Census. The large community size group consisted of participants from Vancouver and Toronto with population of 342,665 and 409,535, respectively. The medium size group consisted of participants from Calgary, Edmonton, and Montreal with the Chinese population of 51,855, 41,290, and 52,110, respectively. Finally, the participants from Victoria and Winnipeg were grouped as the small size group with the Chinese population of 11,240 and 10,925, respectively. The size of the community variable was coded as 1, 2, and 3 to correspond with small, medium, and large community size, respectively.
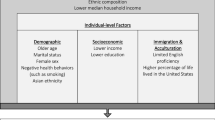
A few socio-demographic factors were included in the analysis to examine the effect of the size of Chinese community variable when controlling for the effects of these confounding factors. The categorical groupings of these variables are presented in Table 1. Self-rated financial adequacy referred to participants’ ratings of how well their income and investments satisfied their financial needs, represented by the answers of ‘very inadequate’, ‘not very well’, ‘adequately’, and ‘very well’, with corresponding scores ranging from 1 to 4, respectively. A higher score represented a higher level of financial adequacy.
Self-rated English competency was assessed by two questions; one question assessed the respondent’s ability to understand English while the second question assessed the respondent’s ability to speak English. The sum of the two questions formed the self-rated English competency score, ranging from 2 to 6, with higher scores representing a higher level of English competency. Country of origin referred to the country from where the participants immigrated. Social support was measured using the sum of two items of self-reported social support, “Someone to trust” and “Someone to provide care,” with corresponding scores of 0–2. A higher score represented higher self-reports of social support.
Service barriers were measured by asking participants to indicate either “yes” or “no” to a 22-item list of potential service barriers identified in previous research [62] and through consultation with services providers in the Chinese community. Examples of barriers included long waitlists, transportation difficulties, and professionals who do not speak the users’ language. The total score indicated the total number of barriers, with higher scores representing more service barriers.
Data Analysis
Descriptive statistics including frequency distributions and means were used to examine the socio-demographic backgrounds and study variables. Hierarchical multiple regression analysis was used to assess the contributions of the size of the Chinese community to the variance in health status as the dependent variable. The socio-demographic variables were entered into the regression model as a block in the first step. Then, the community size variable was entered in the second step.
Results
The participants in this study were on average 70 years old, mostly married, not living alone, educated, able to speak English, and had high social supports. Many migrated from different countries, including Asia, Europe, the United States, and Central and South America. Forty-seven percent of the responses in this study were from seniors living in Toronto or Vancouver, 37% were from Calgary, Edmonton, and Montreal, and 16% were from Victoria and Winnipeg. Table 1 presents the sample characteristics in detail. Tests of differences in means for the SF-36 physical health (PCS) and mental health (MCS) scores by the size of the community were conducted (see Table 2). Participants residing in communities with a small Chinese population reported higher scores for physical and mental health than the participants in communities with a larger Chinese population.
To assess the effect of the size of the community on mental and physical health, two separate multiple regression analysis were conducted. When mental health was the dependent variable, living alone, being an immigrant from Taiwan, Southeast Asian, or other countries, and having more self-reported service barriers predicted lower mental health scores. In contrast, individuals reported a higher level of self-rated financial adequacy or having higher scores for social support have higher MCS scores (i.e., better mental health). The size of the Chinese population was a significant predictor of mental health status when the confounding effects of all other predictors were controlled. Participants residing in cities with larger Chinese population reported lower scores for mental health, meaning poorer mental health, even when adjusted for the effects of the socio-demographic predictors.
When physical health was the dependent variable, being older, being from Southeast Asian or other countries, and higher reports of service barriers predicted lower scores for physical health status. Males and individuals with higher reports of financial adequacy were associated with higher scores for physical health status. Adding the community size variable at the second step did not change the effects of the socio-demographic factors that were significant in the first step. Similar to the regression analysis results for mental health status, physical health status was better for individuals residing in cities with a smaller Chinese population than for those residing in cities with a larger Chinese population (see Table 3).
The characteristics of the participants in the three different community sizes were also compared for differences. Statistically significant differences were found for education level, self-rated financial adequacy, country of origin, and number of service barriers. However, statistical significance was not found for age, gender, marital status, and living arrangement (see Table 4). Participants in communities with the smallest Chinese population reported a significantly lower education level when compared with the participants in communities with a bigger Chinese population. As well, a much higher proportion of the participants residing in communities with the smallest Chinese population size reported a positive level of financial adequacy when compared with the participants in the other two groups. The highest proportion of immigrants from Mainland China was found among the participants in communities with the smallest Chinese population size. While the highest proportion of immigrants from Hong Kong was found among the participants in communities with the largest Chinese population. Finally, participants in communities with the smallest Chinese population reported the least service barriers, while the greatest number of service barriers was reported by participants in the largest Chinese communities.
Discussion
Poorer health status was found in the older Chinese living in major, large Canadian cities. These findings counter the results of other studies where larger size of an ethnic community was positively related to better mental health [19, 20]. These results challenge the assumption that the presence of large, Chinese communities offers protective effects to its members. There are several possible reasons for these findings. First, segregation of the aging Chinese Canadian population and the effects of segregation may be one possible reason. A recent study of social distance and ethnic residential segregation found that as the Chinese population increases, so does its segregation from White European groups, particularly in the three main immigrant “gateway” cities of Canada, Toronto, Vancouver, and Montreal [63]. The growth of the ethno-cultural communities or ethnic enclaves indicates that segregation and negative effects of exclusion of Chinese people from the social, economic, and political spaces of Canada still exists [2, 5, 64, 65].
As well, it is plausible that although the Chinese Canadian population is relatively large, there is a low integration of this population in Canadian mainstream society despite the long history and presence of Chinese people in Canada [65]. Research has found that members of dominant groups tend to misperceive and overestimate the size of the visible minority groups leading to erroneous judgements and expectations of social and economic threat [66]. This may result in deepening the social distance and can negatively affect Chinese seniors because of fewer opportunities for interaction with people outside of their ethno-cultural community. The implication for Chinese seniors may be the psychosocial effects of segregation on health, such as depression and other mental health declines found in other studies [18, 20, 50].
A second possible reason for the health differences found in this study may be due to the Chinese seniors’ access to social support and their use of different strategies of social relating with dominant group members in their respective communities and cities [43]. Immigrants and ethnic visible minorities in societies dominated by a majority group may use different adaptation strategies [67]. Segmented assimilation is one strategy whereby the minority members take on the values, habits, beliefs, and social and cultural practices of the dominant group, as necessary, in order to belong [67, 68]. This survival strategy may be used by members of small ethno-cultural communities to reduce the perceived differences between members of the minority and majority group, while increasing their sense of similarity, inclusion, and belonging.
Members in smaller ethnic communities may have better well-being because of stronger social relationships because they support each other in ways unobtainable from outside of the group. This may lead to strong social bonds and a close-knit community that acts as a protective buffer against race-based hostility. Also, smaller size ethno-cultural communities may be tolerated and perceived more positively by the dominant group because they pose less of a threat to the dominant group’s claim to power and resources [66]. This is a useful strategy when the number of members that make up the minority community is small relative to the dominant group, and that the economic survival of minority members depends on the dominant group’s willingness to facilitate participation in gainful employment and business opportunities. Higher social support may be obtained in smaller communities for these reasons. This strategy is in contrast to members of larger “minority communities” where larger groups can retain the norms of the respective indigenous cultural group [69]. These factors would facilitate the group’s separation from the dominant group through deep integration in the ethno-cultural community to maintain positive, collective self-esteem.
The better physical and mental health found among seniors in smaller Chinese communities may be explained by their ability to access both “worlds.” Whereas for seniors in larger cities with large Chinese communities, usage of an assimilation strategy may not be necessary, partly due to segregation discussed early, and partly by their dependence on the Chinese community for cultural resources and supports [3]. This is somewhat reflected in the study where participants in the smaller communities reported having the least service barriers, while participants in the largest communities reported the most service barriers in accessing mainstream services.
Social support was a significant predictor for reports of better mental health status, but not for reports of physical health status. The finding of high scores for social support as a significant predictor of better mental health suggests that individuals in cities with smaller Chinese communities are more likely to maintain social contacts and to receive support [70–74]. Surprisingly, social support was not a significant predictor of health in larger Chinese communities, which may suggest social cohesion in the large Chinese communities is weak. This has implications in that Chinese seniors in large Chinese communities may experience more individual experiences of social isolation. As the current study was not designed to examine social support in depth, further research is needed to examine the role of perceived and actual social isolation in the context of ethnic group density and health among visible ethnic minority seniors.
The third explanation for the findings is that smaller-size ethnic communities may be more resilient in dealing with negative experiences than their counterparts living in larger-size ethnic communities. Such resilience may translate into better health and functioning. In larger ethnic communities, greater intra-group diversification [43] is likely based on the country of origin, language differences, and cultural practices that may distinguish one sub-group of Chinese people from another. The presence of intra-group diversification within the ethno-cultural community is good in that it acknowledges diversity within the community. However, it may not mean there is cohesion within the community. In the case of Chinese seniors who are members of sub-ethnic groups in the Chinese community (i.e., based on province of origin, language and sub-ethnic group customs and practices), social isolation may be higher for some than for others [43].
A related explanation is that older Chinese in poorer health tended to choose to move to larger urban cities where larger ethnic enclaves are more easily to be found. By so doing, they may think that they are in a better position or location to receive culturally and linguistically concordant services. However, without longitudinally tracking the health status of the participants before and after they move to the larger urban centers, it is difficult to draw any conclusion to this hypothetical explanation. Future research using a longitudinal design may provide answers to this observation.
The unique contribution of this study is the focus on ethnic group density effects on Chinese seniors, a group that is present and growing steadily in Canada and the United States. This study’s findings suggest that the presence of a larger ethnic community size does not necessarily enhance individual health and well-being. Similar to other studies [51], these findings have relevance in cautioning moving quickly to expect that Chinese and other seniors can rely solely on their immediate and community social networks for support to meet their health and well-being needs. This is particularly important with the current health service directions that try to relinquish state involvement in their care and costs of care to seniors by expecting that the seniors can depend on their immediate family and community networks.
A limitation of the findings is that the differences reported between small, medium, and large Chinese communities, though statistically significant, are modest in magnitude. However, such differences should not be neglected in a practical sense. Very often, communities with a small or medium size Chinese community are left with only one community-based service organization in its jurisdiction to provide all the immigrant support services and to meet all ranges of needs. The range of choices is very limited. On the other hand, urban centers with large Chinese communities are often equipped with relatively more service providers. Therefore, the availability of ethno-specific immigrant services may not be a key factor for the health differences. As practitioners and policy decision makers work with the immigrants, practical considerations have to be given to address the effects of other confounding factors. These potential residual confounding effects may be due to the macro socioeconomic and political environment related to race relations, racism, and various forms of discrimination that exist in the larger urban centers with a higher concentration of ethno-cultural minorities and immigrants. Further research is needed to examine the residual confounding effects of these macro factors and the practical approaches to reducing the health differences reported in this study.
Although the study adds new knowledge specific about ethnic group density effects and Chinese seniors in Canada, much more future research is needed to explore the effects of ethnic group density and intergenerational differences between older and younger seniors. As well, more studies are needed with various ethnic groups and demographic characteristics (i.e., gender) to piece together a better picture of how ethnic group density influence health.
Despite the fact that the participants in this study were obtained through screening through a list of randomly selected telephone numbers listed under Chinese surnames, the sample included is not a fully representative sample. There may be many aging Chinese adults meeting the inclusion criteria, but were not included since their telephone numbers were not listed using a Chinese surname. At the same time, aging Chinese adults who reside in locations or cities outside of these seven major urban centres were not included. Therefore, the findings have to be interpreted with caution due to the potential limitation in generalization power.
New Contributions to the Literature
From a social determinant of health perspective, this study highlights the relevance of the size of the ethno-cultural community as an important factor in understanding its influence on health outcomes. The findings also raise important questions about the role that intra-group diversity may have on settlement adjustment and health, and the question of integration/segregation of Chinese communities in contemporary, mainstream Canada.
References
Statistics Canada. Visible minority population, by age group (2006 census). In: 2006 Census of Population. Statistics Canada; 2009.
Chui T, Tran K, Flanders J. Chinese Canadians: enriching the cultural mosaic. Canadian Social Trends 2005, Catalogue No. 11-008:24-32.
Fong E, Ooka E. Patterns of participation in informal social activities among Chinese immigrants in Toronto. Int Migr Rev. 2006;40(2):348–74.
Hou F. Changes in the initial destinations and redistribution of Canada’s major immigrant groups: reexamining the role of group affinity. Int Migr Rev. 2007;41(3):680–705.
Lai CD. Chinatowns: towns within cities in Canada. Vancouver: University of British Columbia Press; 1988.
Marger MN. The use of social and human capital among Canadian business immigrants. J Ethn Migr Stud. 2001;27(3):439–53.
Wong LL, Ng M. Chinese immigrant entrepreneurs in Vancouver: a case study of ethnic business development. Can Ethn Stud. 1998;30(1):22.
Lai DWL. Impact of culture on depressive symptoms of elderly Chinese immigrants. Can J Psychiatry. 2004;49(12):820–7.
Lai DWL. Predictors of use of senior centers by elderly Chinese immigrants in Canada. J Ethn Cult Divers Soc Work. 2006;15(1/2):97–121.
Lai DWL, Chau SBY. Effects of service barriers on health status of elderly Chinese immigrants in Canada. Soc Work. 2007;52(3):261–9.
Lai DWL, Chau SBY. Predictors of health service barriers for older Chinese immigrants in Canada. Health Soc Work. 2007;32(1):57–65.
Lai DWL, Tsang KT, Chappell NL, Lai DCY, Chau SBY. Relationships between culture and health status: a multi-site study on older Chinese in Canada. Can J Aging. 2007;26(3):171–84.
Chappell NL. Perceived change in quality of life among Chinese Canadian seniors: the role of involvement in Chinese culture. J Happiness Stud. 2005;6:69–91.
Wong ST, Yoo GJ, Stewart AL. Examining the types of social support and the actual sources of support in older Chinese and Korean immigrants. Int J Aging Hum Dev. 2005;61(2):105–21.
Casagrande SS, Gary T, LaVeist TA, Gaskin D, Cooper LA. Perceived discrimination and adherence to medical care in a racially integrated community. J Gen Intern Med. 2007;22(3):389–95.
Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67(3):478–86.
Kreps GL. Communication and racial inequities in health care. Am Behav Sci. 2006;49(6):760–74.
Pickett KE, Wilkinson RG. People like us: ethnic group density effects on health. Ethn Health. 2008;13(4):321–34.
Halpern D, Nazroo J. The ethnic density effect: results from a national community survey of England and Wales. Int J Soc Psychiatry. 2000;46:34.
Veling W, Susser E, van Os J, Mackenbach JP, Selten J-P, Hoek HW. Ethnic density of neighbourhoods and incidence of psychotic disorders among immigrants. Am J Psychiatry. 2008;165:66–73.
Noh S, Avison WR. Asian immigrants and the stress process: a study of Joreans in Canada. J Health Soc Behav. 1996;37(2):194–206.
Anthias F, Cederberg M. Using ethnic bonds in self-employment and the issue of social capital. J Ethn Migr Stud. 2009;35(6):901–17.
Mand K. Gender, ethnicity and social relations in the narratives of elderly Sikh men and women. Ethn Racial Stud. 2006;29(6):1057–71.
Shemirani FS, O’Connor DL. Aging in a foreign country: voices of Iranian women aging in Canada. J Women Aging. 2006;18(2):73–90.
Yan MC, Lauer S. Social capital and ethno-cultural diverse immigrants: a Canadian study on settlement house and social integration. J Ethn Cult Divers Soc Work. 2008;17(3):229–50.
Dutta-Bergman MJ. An alternative approach to social capital: exploring the linkage between health consciousness and community participation. Health Commun. 2004;16(4):393–409.
Edmondson R. Social capital: a strategy for enhancing health? Soc Sci Med. 2003;57:1723–33.
Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491–8.
Kritsotakis G, Gamarnikow E. What is social capital and how does it relate to health? Int J Nurs Stud. 2004;41:43–50.
Chan YK, Lee RPL. Network size, social support and happiness in later life: a comparative study of Beijing and Hong Kong. J Happiness Stud. 2006;7:87–112.
Cohen S. Stress, social support, and disorder. In: Veiel HOF, Baumann U, editors. The meaning and measurement of social support. New York: Hemisphere Press; 1992. p. 109–24.
Stanton-Salazar RD. A social capital framework for understanding the socialization of racial minority children and youths. Harvard Educ Rev. 1997;67(1):1–40.
McMichael C, Manderson L. Somali women and well-being: social networks and social capital among immigrant women in Australia. Human Organ. 2004;63(1):88–99.
Cheong PH, Edwards R, Goulbourne H, Solomos J. Immigration, social cohesion and social capital: a critical review. Crit Soc Policy. 2007;27(1):23–49.
Hao L, Johnson RW. Economic, cultural, and social origins of emotional well-being: comparisons of immigrants and natives at midlife. Res Aging. 2000;22(6):599–629.
Helliwell JF, Putnam RD. The social context of well-being. Philos Trans Biol Sci. 2004;359(1449):1435–46.
Hampton NZ. Social support and quality of life among elderly Chinese Americans/immigrants with disabilities: an exploratory study. J Appl Rehabil Couns. 2004;35(2):17–24.
Jang M, Lee E, Woo K. Income, language, and citizenship status: factors affecting the health care access and utlilization of Chinese Americans. Health Soc Work. 1998;23(2):136–45.
Mui AC, Kang S-Y, Kang D, Domanski MD. English language proficiency and health-related quality of life among Chinese and Korean immigrant elders. Health Soc Work. 2007;32(3):119–27.
Torsch VL, Ma GX. Cross-cultural comparison of health perceptions, concerns, and coping strategies among Asian and Pacific Islander American elders. Qual Health Res. 2000;10(4):471–89.
Tsang EYL, Liamputtong P, Pierson J. The views of older Chinese people in Melbourne about their quality of life. Ageing Soc. 2004;24(1):51–74.
Li W. Beyond Chinatown, beyond enclave: reconceptualizing contemporary Chinese settlements in the United States. GeoJournal. 2005;64(1):31–40.
Chan AF. The global enclave model: economic segregation, intraethnic conflict, and the impact of globalization on Chinese immigrant communities. Asian Am Policy Rev. 2004;13(21–60):40.
Zai L. Social contact, social capital, and the naturalization process: evidence from six immigrant groups. Soc Sci Res. 1994;23:407–37.
Qadeer M, Kumar S. Ethnic enclaves and social cohesion. Can J Urban Res. 2006;15(2 Supplement):1–17.
Noh S, Beiser M, Kaspar V, Hou F, Rummens J. Perceived racial discrimination, depression, and coping: a study of Southeast Asian refugees in Canada. J Health Soc Behav. 1999;40(6):193–207.
Kim U, Yang K-S, Hwang K-K. Contributions to indigenous and cultural psychology: understanding people in context. In: Kim U, Yang K-S, Hwang K-K, editors. Indigenous and cultural psychology: understanding people in context. New York: Springer; 2006. p. 3–25.
Murphy HBM, editor. Socio-cultural factors in schizophrenia. New York: Grune & Stratton; 1968.
Potocky-Tripodi M. The role of social capital in immigrant and refugee economic adaptation. J Soc Serv Res. 2004;31(1):59–91.
Bécares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health & Place. 2009;15:700–8.
Osypuk TL, Diez Roux AV, Hadley C, Kandula NR. Are immigrant enclaves healthy places to live? The multi-ethnic study of atherosclerosis. Soc Sci Med. 2009;69:110–20.
Lauderdale DS, Kestenbaum B. Asian American race identification by surname. Popul Res Policy Rev. 2000;19:283–300.
Tjam EY. How to find Chinese research participants: use of a phonologically based surname search method. Can J Public Health. 2001;92(2):138–42.
Rosenwaike I. Surname analysis as means of estimating minority elderly. Res Aging. 1994;16:212–7.
Ren SX, Amick B, Zhou L, Gandek B. Translation and psychometric evaluation of a Chinese version of the SF-36 Health Survey in the United States. J Clin Epidemiol. 1998;51(11):1129–38.
Ren SX, Chang K. Evaluating health status of elderly Chinese in Boston. J Clin Epidemiol. 1998;51(5):429–35.
Ware JE, Gandek B. Overview of the SF-36 Health Survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol. 1998;51(11):903–12.
Ware JE, Kosinski M. Interpreting SF-36 summary health measures: a response. Qual Life Res. 2001;10(5):405–13.
Ware JE, Kosinski M, Keller SD. SF-36 physical & mental health summary scales: a user’s manual. Boston: The Health Institute, New England Medical Center; 1994.
Ware JE, Kosinski M, Gandek BG, Aaronson N, Alonso J, Apolone G, Bech P, Brazier J, Bullinger M, Kaasa S, et al. The factor structure of the SF-36 Health Survey in 10 countries: results from the International Quality of Life Assessment (IQOLA) project. J Clin Epidemiol. 1998;51(11):1159–65.
Ware JE, Sherbourne D. The MOS 36-item Short-Form Health Survey (SF-36). Conceptual framework and item selection. Med Care. 1992;30(6):473–83.
Tsai DT, Lopez RA. The use of social supports by elderly Chinese immigrants. J Gerontol Soc Work. 1997;29(1):77–94.
Hou F. Spatial assimilation of racial minorities in Canada’s immigrant gateway cities. Urban Stud. 2006;43(7):1191–213.
Lai DC. Vancouver Chinatown—racial discourse in Canada, 1875–1980—Anderson, KJ. J Hist Geogr. 1993;19(1):108–9.
Zucchi J, editors. A history of ethnic enclaves in Canada. Ottawa: The Canadian Historical Association; 2007. Vol 31, p. 1–32.
Alba R, Rumbaut RG, Marotz K. A distorted nation: perceptions of racial/ethnic group sizes and attitudes toward immigrants and other minorities. Soc Forces. 2005;84(2):901–19.
Lee C. Sociological theories of immigration: pathways to integration for U.S. immigrants. J Human Behav Soc Environ. 2009;19:730–44.
Neckerman K, Carter P, Lee J. Segmented assimilation and minority cultures of mobility. Ethn Rac Stud. 1999;22(6):945–65.
Kim BS, Abreu JM. Acculturation measurement: theory, current instruments, and future directions. In: Ponterro JG, Casas JM, Suzuki LA, Alexander CM, editors. Handbook of multicultural counseling. 2nd ed. Thousand Oaks, CA: Sage; 2001. p. 394–424.
Fiori KL, Antonucci TC, Cortina KS. Social network typologies and mental health among older adults. J Gerontol Psychol Sci. 2006;61B(1):25–32.
Lindström M. Social capital, the miniaturisation of community and self-reported global and psychological health. Soc Sci Med. 2004;59(3):595–607.
Poortinga W. Social relations or social capital? Individual and community health effects of bonding social capital. Soc Sci Med. 2006;63:255–70.
Veenstra G, Luginaah I, Wakefield S, Birch S, Eyles J, Elliott S. Who you know, where you live: social capital, neighbourhood and health. Soc Sci Med. 2005;60(12):2799–818.
Yamaoka K. Social capital and health and well-being in East Asia: a population-based study. Soc Sci Med. 2008;66(4):885–99.
Acknowledgments
This research was funded by the Social Sciences and Humanities Research Council under the Strategic Theme: Society, Culture and Health of Canadians (Grant No: 828-1999-1032). The authors thank the anonymous reviewers for their helpful comments on previous versions of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chau, S., Lai, D.W.L. The Size of an Ethno-Cultural Community as a Social Determinant of Health for Chinese Seniors. J Immigrant Minority Health 13, 1090–1098 (2011). https://doi.org/10.1007/s10903-010-9374-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-010-9374-0