Abstract
A number of recent studies have questioned the conventional view regarding the existence of income-related inequalities in depression and have suggested that other factors have a more marked impact, most notably those socio-environmental effects linked to professional status and educational attainment. This paper seeks to measure and decompose the degree of socio-economic inequality in the factors underlying reported depression by drawing on data from Spain (Spanish National Health Survey, 2003), a country in which mental care coverage is somewhat limited, but where a marked social transformation has been apparent in recent decades. Contrary to recent evidence, our findings point towards the existence of significant income-related inequalities in the prevalence of reported (diagnosed) depression. However, the results from our decomposition analysis are more mixed. While a modest proportion of overall inequalities (6–13%) is accounted for by income alone, labour status, demographics and education appear to be more relevant. However, when controlling for potential endogeneity between income and depression by using instrumental variables (IV), income is found to account for more than 50% of overall inequality in reported depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In most European countries insurance coverage for mental health care is relatively limited compared to that for other health services, despite the fact that European societies have undergone marked transformations in their mental health. Globalisation has ushered in a range of changes in the social environment (e.g. increasing competition at work), increased access to knowledge and brought about general rises in income and affluence. Yet, while these changes have obvious economic benefits, they also entail certain health risks, and this is particularly true of mental conditions.
Mental conditions are responsible for significant financial outlays and a discernible social burden on individuals and families. Similarly, mental disorders are linked to a decline in workplace productivity, and shifts in the use of treatment and support services, especially among lower income groups who cannot afford the costs of private mental health care. The overall cost of mental disorders is estimated as accounting for 3–4% of GDP (WHO 2003). In Western Europe, 1-year prevalence of depression stands at about 5% (Paykel et al. 2005). The results of the ESEMED—‘European Study of the Epidemiology of Mental Disorders’—project for Spain (Haro et al. 2006) indicate that 19.5% of Spaniards aged 18 and over (23% of women and 16% of men) will be affected by a mental health disorder at some point in their life and about 8.5% in the 12 months preceding the interview (11.4% women and 5.3% of men). Among mental disorders, unipolar depression alone is responsible for 12% of the total number of years lived with disability, and ranks as the third-leading cause of the global burden of diseases (WHO 2003). By 2020, depression is expected to be the number one disorder in the developed world (WHO 2001). The European Commission suggests that 6.1% of the EU population aged 18–75 suffers from depression (in a 12-month period), which is estimated to cost about 18.4 million euros (EC 2005). There is evidence indicting that 15% of depressive patients under psychiatric treatment commit suicide (O’Leary et al. 2001).
Depressive disorders are recurrent (Paykel 2001) and have been found to be key components of life satisfaction and quality of life (Beck et al. 1974; de Leval 1999; Holzinger et al. 2002). Interestingly, evidence from countries in southern Europe and most notably from Spain suggests that depression can be explained by environmental, ecological and socio-cultural pathways that are differentiated by gender (Rajmil et al. 1998; Montero et al. 2004). Thus, whether or not a socio-economic vector explains the prevalence of mental illness is a key issue for health policy analysis. Indeed, it might be claimed that the persistence of health inequalities in the western world can in part be explained by the growth in inequalities in mental conditions among the relatively worse-off groups.Footnote 1
Several studies have consistently reported evidence of a higher incidence and persistence of depression among persons with low incomes. For instance, Kahn et al. (2000) found a significant association between state-level income inequality and depression among mothers with young children. Fiscella and Franks (2000) found a positive association between income inequality and depression in a sample of adults aged 25–74 years. Murumatsu (2003) reported evidence of a statistically significant association between county-level income inequality and depression among older Americans (aged 70 and older) and particularly those presenting more illnesses.Footnote 2 Wildman (2003), dealing with inequalities in mental health care in Great Britain, found evidence of income-related inequalities, although he concluded that the evidence might be attributable to the correlation between income and other (omitted) variables underlying these inequalities. More recently, Zimmerman and Katon (2005), using the 1992 National Longitudinal Survey of Youth, found that the relationship between income and depression was more pronounced at lower levels of income. However, when controls for other economic variables were considered, income was only significantly correlated with depression in the case of men with below-median incomes. In the same vein, a review of studies of common mental disorders concluded that social position determined a higher prevalence of mental disorders in general (Fryers et al. 2003) and a pioneer meta-analytical study found compelling evidence indicating that low socio-economic status (SES) slightly increased the risk of episode onset and moderately increased the risk for persistence of depression (Lorant et al. 2003).
Income inequalities in mental health mean that relatively poorer individuals are more likely to experience mental conditions than those who are not defined as poor. However, the underlying causes of these conditions need to be understood in order to guide policy action. A key issue here lies with the extent to which inequalities in depression might be reduced with an income transfer from the rich to the poor. Methodological improvements in the measurement of inequalities have focused on developing techniques to breakdown health-related inequality coefficients (Wagstaff and Van Doorslaer 2000; Van Doorslaer and Koolman 2004; Van Doorslaer et al. 2004; Wildman 2003), which in turn allow us to examine the extent to which income or other factors are behind income inequalities in the prevalence of mental disorders, such as depression.
The mental health literature in Spain is particularly interesting given that compared to other countries access to mental health care is widely under funded (Salvador-Carulla et al. 2005) and mental conditions are more stigmatised than in northern and central European countries. Furthermore, the burden to families is comparatively large as in Mediterranean countries the family is still the main provider of (informal) social care. For instance, more than 80% of patients with chronic mental disorders in Spain live with their families, suggesting that the social costs of depression are possibly larger than in any other EU country, although significant variation exists within the country (Gómez-Beneyto et al. 1986). Furthermore, stigmatisation probably results in the underreporting of certain mental conditions, which may in turn be income-dependent, although it is difficult to predict how this would affect inequality indicators. Finally, we should not ignore studies from the World Health Organization that report that between 44 and 70% of patients with mental disorders in developed countries do not receive treatment (WHO 2003).
This paper empirically examines the existence of income-related inequalities in the prevalence of reported depression in Spain and breaks down the contribution of each explanatory factor into the degree of inequality.Footnote 3 We employ microdata retrieved from the 2003 Spanish National Health Survey, which contains information on individuals reporting diagnosed depression (MHCA 2005) as well as household income data. The importance of this study lies in the fact that although a number of studies using individual data have confirmed the general existence of inequality in self-reported health in Spain (García-Gómez and López 2004), very little research has been conducted on the existence of a socio-economic vector for mental health.Footnote 4 However, to the best of our knowledge there is still no evidence concerning a decomposition of income-related inequalities in depression.
Our findings indicate the existence of income-related inequalities in the probability of an individual suffering depression in Spain and that these are attributable not only to income but also, and more importantly, to employment status, demographics and, to a lesser extent, to differences in educational attainment. Our evidence, therefore, supports the hypothesis that a portion of income inequalities in the prevalence of depression are largely environmentally driven and derive, in particular, from low professional status and limited educational attainment that might limit some forms of social participation. Therefore, inequalities in depression may be an inadvertent consequence of hierarchy and, perhaps more specifically, of lower employment status and levels of education, rather than absolute income itself. This claim constitutes a policy sensitive finding as we discuss in the concluding section. Given that when we control for some potential reverse causality between income and depression using an instrumental variables approach, we find that income is a fundamental contributor explaining more than 50% of overall depression inequalities. This being so, however, professional status still accounts for up to 44% of such inequalities.
The paper is organised as follows. Section 2 offers an overview of the relationship between the symptoms of depression and their socio-economic correlates. Section 3 describes the dataset and presents the empirical model used in performing the calculations from which the inequality indices are derived. Section 4 reports the results and, finally, Section 5 presents our conclusions.
2 Theoretical Background
Although depression is a chronic disease with a strong genetic component, the presence of depressive symptoms has also been shown to be dependent on a series of environmental factors. Following Zimmerman and Katon (2005) the relationship between depression and its empirical determinants could be simply modelled as follows,
where D is depression, A age, S sex, I income, E education, M marital status, L labour or occupation status and G genetics. Age and gender are two of the most frequently studied determinants of the condition in the literature. For instance, it is argued that women are often more vulnerable to the internalisation of mental disorders, such as depression, and hence exhibit higher prevalence rates. Biological explanations for gender differences include pre-menstrual hormone fluctuation and the significance of post-maternity depression, along with the higher prevalence shown by women in seeking health care assistance (Hirsch 1998).
In the case of income, the literature indicates that the channels through which income or socio-economic position correlate with the prevalence of mental conditions is somewhat contentious. Some claim the existence of a ‘pure income effect’ that may well underlie the capacity of individuals to undertake protective action to prevent and treat the symptoms of depression (Moser 2001; Hauck and Rice 2004), while others claim that low incomes or unemployment can also imply increased levels of financial stress and depression, understanding chronic financial strain as a situation in which basic needs struggle to be met (Hamilton et al. 1990). Others even cite the role played by the stress that is caused by the perception of income inequality, resulting in depression and poorer health status (Wilkinson 1996). Educational attainment is another well-known determinant of depression. It is argued that people with higher educational levels have greater access to information about treatment choices and the changes experienced in the relief of symptoms than those with lower levels of education. In common with education, labour status is a parallel socio-environmental mechanism that might also explain depression and the existence of inequalities in depression. In other words, higher quality jobs may afford greater social prestige and better psychosocial and physical working conditions, which in turn may serve to protect individuals from depression (Zimmerman and Katon 2005).Footnote 5
The effect of marital status on mental health has also been extensively analysed by numerous researchers. Interestingly, marriage has been found to have a preventive effect on occurrences of depression among men while augmenting the effect among women (Weissman et al. 1993; Murray and López 1994). Nonetheless, as Liu and Chen (2006) have shown we cannot ignore the interplay of household income in the relationship between marital instability (e.g., marital conflict and marital disruption) and depression, mainly among women, after controlling for the initial level of depression and other antecedents. Finally, genetics clearly has an underlying influence as some people are at a very low risk of suffering this chronic condition. For instance, it has been shown how personal characteristics (e.g., self-esteem, mastery, copying style, self-control, etc.) modulate the impact of stress on depression and that individuals with a higher SES are better endowed with such resources.Footnote 6
Notice, however, that depression also has an important impact on income and on several of the socio-economic covariates discussed above. In particular, symptoms of (chronic) depression in adults have been shown to reduce workplace productivity, increase absenteeism, reduce job-seeking activities or ambitions in job choice, etc., (Berndt et al. 1998) while an early-onset major depressive disorder causes lower educational attainment, particularly among women (Berndt et al. 2000). All of which can be expected to have a negative impact on income. It is also worth noting when examining the empirical relationship between depression and SES the existence of a number of third variables that go unobserved by the analyst (i.e., personality traits such as persistence and sociability or early childhood environment) which plausibly reduce episodes of depression and enhance economic success.Footnote 7 These unobservable traits might result in biased parameter estimates of the econometric model (Seligman 1991; Ettner 1996; Zimmerman and Katon 2005).
3 Data and Methods
We employ data from the 2003 edition of the Spanish National Health Survey (‘Encuesta Nacional de Salud’) conducted by the National Statistical Institute (INE).Footnote 8 This is a nationwide representative cross-section health survey based on face-to-face interviews (complemented by telephone interviews where required) that gathers information on aspects which include self-assessed health status, primary and specialized health care utilization, consumption of medicines, lifestyles, conducts related to risk factors, anthropometrical characteristics, preventive practices and socio-economic status. The data can be seen as a “lay-interview external assessment” which is high quality data for obtaining information on reported depression, though ideally a double phase design using screening instruments and semi-structured psychiatric interview should be used to identify cases of “diagnosed depression”, and so this study refers mainly to reported depression.Footnote 9
The original sample contained 21,650 adults (49% men and 51% women) aged 16–99 years, but after deleting several observations owing to missing earnings data, the estimated sample eventually comprised 16,167 individuals. Income (our ranking variable) was used as a proxy for a continuous measure of SES as is standard practice (Wagstaff and Van Doorslaer 2000; Van Doorslaer and Koolman 2004; Van Doorslaer et al. 2004).Footnote 10 In particular, earnings refer to total net household income per month. Since it was measured as a categorical variable with eight response categories, an interval regression model was used to obtain a continuous household income measurement (see the Appendix).Footnote 11 Once net monthly household income was predicted we divided it by an equivalence factor (equal to the number of household members powered to 0.5), to adjust for differences in household size and composition.
3.1 Measurement of Depression
Our measure of depression derives from the respondents’ answers regarding their chronic conditions as diagnosed by a physician, reported as a categorical variable to the question: ‘During the last 12 months, has your doctor diagnosed you to be suffering chronically from the following diseases or health problems?’. Up to 16 chronic diseases—ranging from arterial hypertension and high cholesterol to depression—were read out to the interviewee. Hence, we used this binary variable as a measure of reported depression. Unfortunately, the survey does not include additional information on clinical syndromes of depression (i.e., major and rapid alterations of mood such as sadness, irritability, loss of motivation/pleasure or psychological symptoms involving appetite, sleep, libido, energy level and psychomotor activity) which could be used to improve our measure of depression.Footnote 12
We then transformed the dichotomous depression measure (y i ) into a continuous variable by adjusting and using the OLS predictions of a Linear Probability Model (LPM) as shown below,
where y i = 1 (if individual i declares he/she suffers depression), ε i is the random error term, x k is a set of exogenous determinants of depression and β k is the vector of associated parameter estimates. From the specification of Eq. 2, the probability of suffering (reported) depression is as follows,
The option for adjusting an LPM, which gives consistent estimations of the parameters β k , is justified on the grounds that linearity in parameters is a useful property (without incurring any loss of estimation efficiency) for decomposition, during a second stage, of the inequality index of the prevalence of depression (Van Doorslaer and Koolman 2004; Van Doorslaer et al. 2004; García-Gómez and López 2004; Costa-Font and Gil 2008).Footnote 13 Unlike previous studies, we consider here the effect of some reverse causality between income and mental health using instrumental variables (IV).
Following the evidence reported in the existing literature (e.g., La Gory and Fitzpatrick 1992; Kahn et al. 2000; Lorant et al. 2003; Muramatsu 2003; Zimmerman and Katon 2005; Paykel et al. 2005) our empirical strategy to estimate the prevalence of depression considers the following set of exogenous covariates (x k ): (i) the logarithm of equivalent net household income, (ii) six age-gender categories corresponding to groups 16–34, 35–44, 45–54, 55–64, 65–74 and 75+ for men and women. These covariates are aimed at displaying non-linear effects of age and the fact that women are twice as likely to experience depressive disorders (Fryers et al. 2004; Blehar and Oren 1995), (iii) four categories for marital status, (iv) four categories for educational level to measure the impact of knowledge on health risks; (v) five categories for labour status, and (vi) 17 Autonomous Communities or geographical variables to control for regional heterogeneity in lifestyles, values and other environmental conditions (e.g., weather conditions). The profile of the omitted reference category was a young male, single, employed with secondary education and from the region of Andalusia.
The linear model outlined above should be not seen as a structural model of depression; neither should the results be interpreted as a causal relationship. However, it is useful to note that this regression equation can be interpreted as a reduced form model whose estimates provide an indication of how exogenous changes in depression covariates may affect the degree of income-related inequality in depression. Table 1 presents variable definitions and descriptive statistics.
3.2 Measurement of Inequality
As is customary in the literature on health inequalities, the concentration index (CI) of suffering depression on income is used to measure income-related inequality of depression (Van Doorslaer and Koolman 2004; Van Doorslaer et al. 2004). The CI of the probability of depression on income can be adequately calculated from individual level data. Following the covariance method (Jenkins 1998):
where \( \overline{y} \) is the mean of the prevalence of depression, R i is the fractional income rank of the ith individual (i.e., the cumulative proportion of the population ranked by income up to the ith individual) and cov(·) denotes the covariance statistic. This CI coefficient ranges from a minimum value of −1 to a maximum of +1 and occurs when the depression in an entire population is concentrated in the poorest or richest person, respectively. A zero value indicates equality in the prevalence of depression (i.e., depression is equally distributed across all income groups).
In line with Wagstaff et al. (2003), we then proceeded to break down the aforementioned degree of income-related inequality into the determinants of the depression condition. To do so, an LPM of depression must first be adjusted against a set of x k exogenous covariates as described by Eq. 3.Footnote 14 Hence, the CI for the probability of being depressed can be expressed as,
where \( \overline{{x_{k} }} \) is the mean of x k and C k denotes the concentration index for x k against income (i.e., how income is distributed over each explanatory variable of depression). The term in brackets in Eq. 5 expresses the elasticity of the probability of y (depression) with respect to x k (evaluated at the population mean). Thus, if we define this estimated elasticity with respect to a specific k as follows,
then we can interpret the CI of the probability of depression on income as a weighted sum of the inequality in each of its determinants, with the weights being equal to the depression elasticities,
This decomposition, as pointed out by Van Doorslaer and Koolman (2004), has the advantage of clarifying how each correlate of the prevalence of depression contributes to total income-related inequality in two parts: (i) its impact on depression, as measured by the depression elasticity (η k ) along with (ii) the extent of unequal income distribution, measured by the concentration index (C k ). Moreover, following Kakwani et al. (1997) and Wagstaff et al. (2003) total depression inequality can be usefully broken down into the so-called “potentially avoidable” and “unavoidable” (or intrinsic) inequality. The latter can be attributed, for instance, to differences in the age and gender composition of the population by income. Thus, by subtracting the influence of the age-gender expected inequality (CI*) from the total CI, a measure of avoidable inequality or inequity is obtained \( {\left( {{\text{I}}^{*} = {\text{CI}} - {\text{CI}}^{*}} \right)}. \)
4 Results
4.1 Preliminary Evidence
The prevalence of reported (diagnosed) depression in our sample of Spanish adults (16 years of age and over) was 5.91% in 2003 (see Table 1), although the condition, as it has been extensively demonstrated, was significantly more pronounced in women (8.39%) than in men (3.28%) (Table 2).Footnote 15 Our data also confirm that depression increases with age until a peak is reached (6.9% around 55–64 years for men; 15.8% around 65–74 years for women) and then declines. Hence, the results corroborate the claim that depression affects mostly women and the elderly.
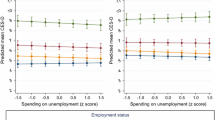
Figure 1 plots the distribution of depression among different income deciles and by gender. Here the (log) of household income measured in equivalent terms was used to define income deciles. Interestingly, we found that whilst for men there was a moderate declining pattern of depression across income deciles, the prevalence of depression among women was approximately similar for the first three deciles (12–14%) and then fell markedly to 3.4% in the top income decile. Therefore, we tentatively conclude that there is some evidence of an income gradient underlying the prevalence of depression.
Distribution of depression by income deciles and gender. Note: (Log) equivalent income was employed as the measure to compute income deciles. Source: Spanish National Health Survey, 2003 (MHCA 2005)
4.2 Estimation of the Prevalence of Depression
The OLS parameter estimates of an LPM on depression are reported in column 2 in Table 3. As expected the (log) equivalent income coefficient exerted a negative and statistically significant effect on the prevalence of (reported) depression. Interestingly, when controlling for other influences, the prevalence of depression increased with age in women and this pattern seemed to take the shape of a curve in the latter stages of life. This is consistent with quadratic or curvilinear effects whereby depression peaks in middle age and then falls off (Jorm 1987; Paykel et al. 2005). Marital status also affected the probability of suffering depression, since divorced or legally separated adults had far greater chances (around 8%) of suffering poor mental health. Furthermore, individuals with little or no education were 2.8% more likely to suffer depression, compared to the reference category (i.e., secondary education), while this did not hold for those with more education. Finally, our data revealed a differentiated impact of depression by employment status: compared to individuals who are still working, a higher propensity to depression was found among disabled pensioners (11%), the unemployed (3.8%) and other pensioners (3.4%). This picture is, of course, very similar to the evidence reported by the results of the ESEMED-Spain project or the results found by García-Gómez and López (2005) in the case of Catalonia.
The next two econometric regressions (models 2 and 3) in Table 3 were run for robustness purposes. Model 2 (column 3) estimated the prevalence of depression by OLS when excluding the influence of the labour status covariates on the calculations of the inequality indices. Note that a roughly similar qualitative pattern was found although, as expected, once these variables were dropped we observed a greater impact on depression caused by income, age and gender dummies (mainly in women) and primary education. In model 3 (column 4) we estimated a non-linear probit model—model 4—for the prevalence of the mental illness but the linear marginal effects are presented in Table 3. Although the income effect was roughly similar, the most remarkable impact of the probit estimation, compared to model 1, was the stronger influence of the demographic variables on depression.
Given the suspicion that income acts as an endogenous regressor in the equation of depression, we performed an Instrumental Variables (two-stage least square) estimation of the probability of suffering depression (model 4).Footnote 16 The instruments used to proxy the (log) of equivalent income were a set of dummies including employer (business person or professional) with wage earners, employer without wage earners, fixed wage earner permanently employed, working for the public administration, working in public companies and domestic service. These are all supposedly uncorrelated with the error term of the depression equation. These instruments were demonstrated to be valid candidates as they were statistically significant at 5% and also jointly significant according to an F-test. Interestingly, as a consequence of the instrumenting of an individual’s income, the size of the income effect on depression increased by a factor of four (as did its robust standard errors) and having a university degree increased the probability of suffering depression (2.45%) compared to the omitted category. The remaining parameter covariates were approximately similar to those of reference model 1.Footnote 17
Finally, we estimated a bivariate model of self-selection (Heckman 1979) on the prevalence of depression with the GP visit acting as the participation equation and private health insurance as an exclusion restriction, in order to tackle a potential sample selection problem of reporting depression when there has been a previous visit to the GP. We found a low value for the Wald test (1.33) and could not reject the null hypothesis of absence of correlation between the errors of the bivariate sample selection model.
4.3 Income-related Inequalities in Depression: A Decomposition Analysis
The last column of Table 3 presents the estimation of the concentration index for each explanatory determinant of being depressed.Footnote 18 The CI of the log income (0.0461) showed an unequal income distribution that favours the wealthiest population segments. The bootstrapped standard errors indicated that this index was statistically significant. In the case of demographic determinants such as age and gender, we found that the elderly population concentrated in low-income groups, although income inequality appeared more stringent and at earlier ages in women. As expected, Spanish adults with higher levels of education are strongly concentrated in the upper tail of income distribution, while the opposite is true for people with relatively little education (e.g., primary studies or unschooled).Footnote 19 In the same vein, pensioners, the unemployed, and those inactive are more likely to display lower income levels, whereas the working population is concentrated among high incomes. Furthermore, the data show evidence of pro-poor income distribution in widowhood, as most of the income of widows is made up of non-contributory benefits (García-Gómez and López 2004). Finally, the concentration indices for the regional variables confirm the existence of pronounced disparities in regional income in Spain (Van Doorslaer and Koolman 2004; García-Gómez and López 2004).
Next, Table 4 shows the inequality index estimates for the prevalence of reported depression in Spain under different econometric specifications. Interestingly, as model 1 (column 2) indicates the CI of the probability of depression on income was negative (−0.1551) and statistically significant, indicating high income-related inequalities in depression consistent with previous studies (Wildman 2003). Hence, individuals ranked according to (log) income seem to exhibit inequalities in the prevalence of depression (ill-mental health), since depression is concentrated in low income groups. A similar picture was derived from the CI estimated by models 2 and 3 (columns 3 and 4). Indeed, the inequality index of depression was also negative but much lower and statistically significant (−0.1090) when the IV regression model was run to estimate the determinants of the probability of depression symptoms. In this case, we found that both education and regional heterogeneity were the main factors reducing the size of the income-related inequalities in depression. The second row in Table 4 depicts an estimate of the share of inequalities in reported depression episodes that are not explained by age and gender \( {\left( {{\text{I}}^{*} = {\text{CI}} - {\text{CI}}^{*}} \right)}, \) indicating what has been labelled both here and in other studies as the degree of potentially “avoidable inequality”. In addition to showing the same pattern as its raw counterpart, the resulting figure for model 1 (−0.1214) thus indicates that only a relatively low share of the degree of income-related depression inequality is due to differences in the age-gender structure of population alone. This is not the case in models 2 (where the influence of the labour status variables were first dropped) and 3 (where a probit model was used) in which avoidable inequalities of depression were much lower.
Some interesting and, to some extent, conflicting results emerged following the breakdown of the contributions of explanatory variables to the degree of income-related depression inequalities (Table 4). According to models 1–3, we found that income was not a fundamental contributor of SES inequalities in the prevalence of depression when other covariates were considered (6–13% of overall inequality). Thus, our data seem to suggest that other determinants, at varying degrees, account for an even higher proportion of these inequalities, which is consistent with recent studies reporting a reduced impact of income on depression when other controls are included (Zimmerman and Katon 2005).Footnote 20 Hence, income-related depression inequality would still be substantial even if income had been equally distributed across the income range or if it had had zero depression elasticity. The evidence presented by models 1–3 undoubtedly points towards other factors besides income (e.g., employment status, education and demographics) as key covariates in the prevalence of self-declared (diagnosed) depression amongst Spain’s adults. Certainly, our results confirm that labour or employment status dummies accounted for a significant portion (between 30 and 40%) of the overall depression inequality. Interestingly, we found that the effects of the ‘other pensioner’ category—chiefly retirement and widow pension benefits—and ‘disabled pensioner’ were crucial and played an even greater role than individuals’ income. Demographic variables accounted for a similar share in the overall income-related inequality (between 22 and 42%) and the key element here were women in the oldest age categories. In common with demographics, education levels also had a noticeable effect as a determinant of the overall CI of depression (between 16 and 35%), which would appear to link the prevalence of depression to knowledge (e.g., awareness of mental health symptoms), time preferences and the array of associated mechanisms. Note, however, as our data contain evidence of diagnosed or reported rather than perceived depression, we cannot rule out the possibility that education influences access to mental health care services or the prevention of mental disorders, given the limited health care coverage provided in Spain.
However, a different picture emerged when the instrumental variables model regression (model 4) was employed. Although some caution should be exercised as to the validity of the instruments, we found that after controlling for potential endogeneity, income became a crucial determinant of the observed level of income-related inequalities in depression, accounting for more than 50% of overall inequality, whilst university education served to reduce inequalities by about 21% and professional status still accounted for up to 44% of such inequalities in reported depression.
5 Conclusions
This paper has addressed the issue of income-related inequalities in a major mental disorder, namely reported depression, as well as the decomposition of the factors underlying the condition. The study has been conducted in Spain, a country in southern Europe with limited mental health care coverage and increasing patterns of mental disorders. We have sought to provide evidence regarding the extent of socio-economic inequalities in sufferers’ mental conditions so as to motivate health policy action in terms of services provision and financing. We found, firstly, that when individuals were ranked by income, the higher the individuals’ social status was, the lower the prevalence of depression. Moreover, this finding proved consistent with different econometric specifications.
Interpreting this evidence is by no means straightforward. On the one hand, the influence of pure income effects on income-related inequalities suggests that efforts should be made within the Spanish National Health System (NHS) to prevent the deterioration in the mental health of the relatively less affluent population. In other words these data call for a re-examination of the limited mental health care available in Spain today. However, a significant proportion of these income inequalities would not be eradicated by redistribution programs alone, although 50% of them would be when using an instrumental variables approach that accounts for the potential endogeneity of income. Besides income, the influence of labour (professional or occupation) status is of particular importance, so that individuals occupying a managerial position in a professional organisation would seem to serve as an inhibitor of depression. There are several contentious arguments that might well shed additional light on these results, including the effects of unobserved variables.
The implications for social policy design are considerable. If mental health care has a significant effect on physical health as some studies suggest (Istvan et al. 1992; Smith and DeFelice 2004), then the existence of inequalities in mental health might help explain the persistence of income-related health inequalities.Footnote 21 For instance, it could be argued that unless income inequalities in mental health are reduced, inequalities in health are likely to persist over time. Given that mental health care coverage may prevent “pure” income-related inequalities, significant inequalities would still prevail and could be tackled by programs that seek to reduce income inequalities. However, it would not suffice simply to increase income redistribution, as employment status and education are also crucial factors in the socio-economic vector. Although a high income implies the availability of resources for investing in the prevention and/or cure of mental illness at the individual level, environmental factors that influence a person’s perceived social status might, in the light of our results, indirectly explain the existence of income-related patterns of depression.
In line with the literature, we have found evidence of gender effects in the existence of income-related inequalities in depression. Yet, whether these gender related effects are a reflection of biological effects–which are perhaps unavoidable—or they are the result of sex discrimination—especially among less affluent women—cannot be determined from our data. Another interpretation of these results, however, might be that policies to tackle income-related inequalities require the coordination of various other social policies including employment and education. Of particular importance in the light of our results are policies to foster gender equality at work and in broader social settings as potential preventive tools for depressive disorders in less affluent women.
Among the study’s caveats are the potential effects derived from the use of reported depression (as noted earlier). An additional problem is the difficulty encountered in isolating the effects of inequality on psychological well-being and the possibility that socio-economic and socio-emotional factors interact in their incidence on depression. In addition, inequality studies depend on well-known econometric assumptions and so the violation of any of these might affect the reliability of our results. Likewise, the cross-sectional nature of our data means that the direction of association cannot be fully identified unless panel data evidence becomes available and adequate instruments are employed. Indeed, while our results suggest a pattern, this cannot be assumed as being causal. However, even in those instances where income alone does not necessarily lead to a higher prevalence of depression (see, for example, Zimmerman and Katon 2005), it may influence the willingness and ability to seek out depression counselling. This would, in turn, address the need of the traditionally under-funded health system to strengthen mental health care, an area that is often subject to stigmatisation. This finding rests on the effect of unobservable variables, such as anxiety and stress (Seligman 1991), and questions previous evidence (Ettner 1996) by suggesting that the relationship between income and depression might be the result of other unobserved or omitted variables. While some authors argue that high income encompasses social recognition, it might in turn lead to an expansion of an individual’s financially-related stress (Murphy et al. 1991). However, this is a matter for future research to clarify.
Notes
For instance, Smith and DeFelice (2004) argue that depression is a factor that shapes health production affecting the individual’s tastes and changes in mood, which might interact with other factors of health production such as the body mass production. Some studies find empirical evidence of a connection between obesity and depression (Istvan et al. 1992 or Costa-Font and Gil 2006). However, health production functions typically do not examine potential interactions between mental and physical health inputs.
We concentrate on income-related inequalities rather than other measures of SES (i.e., education, occupation or social class) in line with previous studies such as Wagstaff and Van Doorslaer (2000).
Notice that, in fact, income correlates with a number of the factors affecting depression described here, most notably education and labour status.
Indeed, ecological determinants seem to be an important underlying predictor of depression (La Gory and Fitzpatrick 1992). Some studies even claim that discrimination, and particularly that suffered by women (Belle and Doucet 2003) and racial minorities (Meltzer et al. 2004), is a common cause of inequalities in depression.
An example of the complex relationship between depression and income is provided by Frank and McGuire (2000), who point out that “personal characteristics which make a positive contribution to earnings (e.g., creativity, energy or attention to detail) are (relatively) more common among persons who have mania or obsessive-compulsive disorders”.
Cf. MHCA (2005).
The survey follows a stratified multi-stage sampling procedure in which the primary strata are the Autonomous Communities, and sub-strata are then defined according to population size in particular areas. Within the sub-strata, municipalities and sections (primary and secondary sampling units respectively) are selected using a proportional random sampling scheme. Finally, individuals are randomly selected from the sections.
Other covariates are also valid candidates for measuring the economic position of the household (e.g., education or occupation). However, the decomposition procedure employed in the analysis requires a continuous measure of SES.
In other to avoid identification problems in the computation of the inequality index, we adjusted the (household) income equation by using characteristics of the head of the household and also information regarding the spouse and children.
There is a potential problem of sample selection. It is plausible to conceive a respondent suffering from depression but not reporting it simply because there is not a GP/specialist visit.
As is shown in Sect. 4, the results do not change substantially when the linear marginal effects of a probit estimation model are alternatively employed to deduce the inequality index of depression.
Note that recent contributions suggest that linear models can be employed in the context of happiness measurement with little gain from imposing non-linearity (Ferrer-i-Carbonell and Frijters 2004).
Actually, our sample slightly overestimates the prevalence of diagnosed depression: 5.9% vs. 5.4% in the original sample for adults aged 16–99. The latter suggests estimates that are closer to those in recent studies employing standardised survey techniques (World Mental Health Survey Consortium 2004).
We applied the Hausman (1978) test to control for endogeneity by taking into account heteroskedastic-robust standard errors, and found only weak evidence supporting the inexistence of a reverse causality relationship between income and depression.
We need to interpret these results with caution, since it has been demonstrated that poor instruments can actually create more bias in an estimator than least squares in the presence of endogeneity.
Given that the components of Eq. 5 are non-linear functions of the data with complex sampling distributions, we opted to use bootstrapping methods to derive standard errors of the concentration indices. The number of replications was set to 100.
These features have also been observed in the EU (cf. Van Doorslaer and Koolman 2004).
This contrasts with findings by García-Gómez and López (2005). However, these authors restrict the analysis to the region of Catalonia and use a shortened GHQ instrument to measure mental health.
There is, however, a debate regarding the extent to which inequalities are largely avoidable or unavoidable. Some authors argue that it depends on normative standpoints and that it is not possible to establish a distinction with any degree of certainty (Vallgårda 2006).
References
Beck, A., Weissman, A., Lester, D., & Trexler, L. (1974). The measurement of pessimism: The hopelessness scale. Journal of Consulting and Clinical Psychology, 42, 861–865.
Belle, D., & Doucet, J. (2003). Poverty, inequality and discrimination as sources of depression among U.S. women. Psychology of Women Quarterly, 27(2), 101–113.
Berndt, E. R., Finkelstein, S. N., Greenberg, P. E., Howland, R. H., Alison, K., Rush, A. J., Russell, J., & Keller, M. B. (1998). Workplace performance effects from chronic depression and its treatment. Journal of Health Economics, 17, 511–535.
Berndt, E. R., Koran, L. M., Finkelstein, S. N., Gelenberg, A. J., Korstein, S. G., Miller, I. M., Thase, M. E., Trapp, G. A., & Keller, M. B. (2000). Lost human capital from early-onset chronic depression. American Journal of Psychiatry, 157(6), 940–947.
Blehar, M. D., & Oren, D. A. (1995). Women’s increased vulnerability to mood disorders: Integrating psychobiology and epidemiology. Depression, 3, 3–12.
Costa-Font, J., & Gil, J. (2006). Revisiting the fat and jolly hypothesis: Obesity and depression in Spain. Socio-Economic Review, 4(3), 513–542.
Costa-Font, J., & Gil, J. (2008). Una exploración de las desigualdades socioeconómicas en morbilidad en España. Revista ICE, 68 (in press).
de Leval, N. (1999). Quality of life and depression: Symmetry concepts. Quality of Life Research, 8(4), 283–291.
Ettner, S. L. (1996). New evidence on the relationship between income and health. Journal of Health Economics, 15, 67–85.
European Commission-EC. (2005). Improving the mental health of the population. Towards a strategy on mental health for the European Union. Green Paper, COM(2005) 484 final.
Ferrer-i-Carbonell, A., & Frijters, P. (2004). How important is methodology for the estimates of the determinants of happiness? The Economic Journal, 114(497), 641–659.
Fiscella, K., & Franks, P. (2000). Individual income, income inequality, health and mortality: What are the relationship. Health Services Research, 35(1-part2), 307–318.
Frank, R. G., & McGuire, T. G. (2000). Economics and mental health. In A. J. Culyer, & J. P. Newhouse (Eds.), Handbook of health economics (Ch. 16, Vol. 1B). Elsevier: North Holland.
Fryers, T., Brugha, T., Morgan, Z., Smith, J., Hill, T., Carta, M., Lehtinen, V., & Kovess, V. (2004). Prevalence of psychiatric disorder in Europe: The potential and reality of meta-analysis. Social Psychiatry and Psychiatric Epidemiology, 39, 899–905.
Fryers, T., Melzer, D., & Jenkins, R. (2003). Social inequalities and the common mental disorders: A systematic review of the evidence. Social Psychiatry and Psychiatric Epidemiology, 38, 229–237.
García-Gómez, P., & López, A. (2004). The evolution of inequity in the access to health care in Spain: 1987–2001. UPF Economics Working Paper 756.
García-Gómez, P., & López, A. (2005). Socio-economic inequalities in health in Catalonia. Hacienda Pública Española/Revista de Economía Pública, 175–4, 103–121.
Gómez-Beneyto, M., Asensio, A., & Berenguer, M. J. (1986). Desinstitucionalización de enfermos mentales crónicos sin recursos comunitarios. In J. Espinosa (Ed.), Cronicicidad en Psiquiatria. Madrid: Mayoría Editorial.
Hamilton, V., Broman, C., Hoffman, C., & Renner, D. (1990). Hard times and vulnerable people: Initial effects of plant closing and autoworkers’ mental health. Journal of Health and Social Behaviour, 31, 123–140.
Haro, J. M., Palacín, C., Viladegut, G., Martínez, M., Bernal, M., Luque, I., Codony, M., Dolz, M., & Alonso, J. (2006). Prevalencia de los transtornos mentales y factores asociados: Resultados del estudio ESEMED-España. Medicina Clínica, 126(12), 445–451.
Hauck, K., & Rice, N. (2004). A longitudinal analysis of mental health mobility in Britian. Health Economics, 13, 981–1001.
Hausman, J. A. (1978). Specification tests in econometrics. Econometrica, 46, 1251–1271.
Heckman, J. J. (1979). Sample selection as a specification error. Econometrica, 47, 153–161.
Hirsch, S. (1998). Psychiatry beds and resources: Factors influencing bed use and service planning. London: Royal College of Psychiatrist.
Holzinger, A., Matschinger, H., & Stengler-Wenzke, K. (2002). Depression and quality of life: Results of a follow-up study. International Journal of Social Psychiatry, 48(3), 189–199.
Istvan, J., Zavela, K., & Weidner, G. (1992). Body weight and psychological distress in NHANES I. International Journal of Obesity 16, 999–1003.
Jenkins, S. (1998). Calculating income distribution indices from micro-data. National Tax Journal, 41(1), 139–142.
Jorm, A. F. (1987). Sex and age differences in depression: A quantitative synthesis of published research. Australian and New Zealand Journal of Medicine, 21, 46–53.
Kahn, R. S., Wise, P. H., Kennedy, B. P., & Kawachi, I. (2000). State income inequality, household income and mammal mental and physical health: Cross sectional national survey. British Medical Journal, 321(7272), 1311–1315.
Kakwani, N. C., Wagstaff, A., & Van Doorslaer, E. (1997). Socioeconomic inequalities in health: Measurement, computation and statistical inference. Journal of Econometrics, 77(1), 87–104.
La Gory, M., & Fitzpatrick, K. (1992). Effects of environmental context on elderly depression. Journal of Aging and Health, 4(4), 459–479.
Liu, R. X., & Chen, Z.-Y. (2006). The effects of marital conflict and marital disruption on depressive affect: A comparison between women in and out of poverty. Social Science Quarterly, 87(2), 250–271.
Lorant, V., Deliège, D., Eaton, W., Robert, A., Philippot, P., & Ansseau, M. (2003). Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemiology, 157(2), 98–112.
Meltzer, D., Fryers, T., & Jenkins, R. (2004). Social inequalities and the distribution of the common mental disorders. Hove and New York: Psychology Press.
Ministry of Health and Consumer Affairs—MHCA (2005). Encuesta Nacional de Salud 2003. Tablas con Resultados Nacionales y Autonómicos (from http://www.msc.es).
Montero, I., Aparicio, D., Gómez-Beneyto, M., Moreno-Küstner, B., Reneses, B., Usall, J., & Vázquez-Barquero, J. L. (2004). Género y salud mental en un mundo cambiante. Gaceta Sanitaria, 18(supl 1), 175–181.
Moser, K. (2001). Inequalities in treated heart disease and mental illness in England and Wales, 1994–1998. British Journal of General Practice, 51, 438–444.
Muramatsu, N. (2003). County-level income inequality and depression among older Americans: Empirical analyses. Health Service Research, 38(6), Part II, 1863–1883.
Murphy, J., Olivier, D. C., Monson, R. R., Sobol, A. M., Federman, E. B., & Leighton, A. H. (1991). Depression and anxiety in relation to social status. A prospective epidemiological study. Archives of General Psychiatry, 48, 223–229.
Murray, C., & Lopez, J. J. (1994). Global comparative assessment in the health sector. Disease burden, expenditures and intervention packages. Geneva: World Health Organisation.
O’Leary, D., Paykel, E. S., Todd, C., & Vardulaki, K. (2001). Suicide in primary affective disorders revisited: A systematic review by treatment era. Journal of Clinical Psychiatry, 62, 804–811.
Paykel, E. (2001). Continuation and maintenance therapy in depression. British Medical Bulletin, 57, 145–159.
Paykel, E. S., Brugha, T., & Fryers, T. (2005). Size and burden of depressive disorders in Europe. European Neuropsychopharmacology, 15, 411–423.
Rajmil, L., Gispert, R., Roset, M., Muñoz, P. E., & Segura, A. (1998). Prevalence of mental disorders in the general population of Catalonia. Gaceta Sanitaria, 12, 153–159.
Salvador-Carulla, L., Tibaldi, G., Johnson, S., Scala, E., Romero, C., & Munizza, C. (2005). Patterns of mental health service utilisation in Italy and Spain. An investigation using the European Service Mapping Schedule. Social Psychiatry and Psychiatric Epidemiology, 40(2), 149–159.
Scheffler, R. M. (1999). Managed behavioral health care and supply-side economics. Journal of Mental Health Policy and Economics, 2(1), 21–28.
Scheffler, R., Zhang, A., & Snowden, L. (2001). The impact of realignment on utilization and cost of community-based mental health services in California. Administration and Policy in Mental Health, 29(2), 129–143.
Seligman, M. E. P. (1991). Helplessness: On depression, development and death (2nd ed.). New York: W.H. Freeman.
Smith, C. K., & DeFelice, K. L. (2004). Maternal depression and the production of infant health. Southern Economic Journal, 71(2), 260–286.
Vallgårda, S. (2006). When are health inequalities a political problem? European Journal of Public Health 16(6), 615–616.
Van Doorslaer, E., & Koolman, X. (2004). Explaining the differences in income-related health inequalities across European countries. Health Economics, 13, 609–628.
Van Doorslaer, E., Koolman, X., & Masseria, C. (2004). Equity in the delivery of inpatient care in the European Union: A pooled analysis. Equity Project III, Working Paper 13, 2004. Department of Health Policy and management, Erasmus University, Rotterdam.
Wagstaff, A., & Van Doorslaer, E. (2000). Income inequality and health: What does the literature tell us? Annual Review of Public Health, 21, 543–567.
Wagstaff, A., Van Doorslaer, E., & Watanabe, N. (2003). On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. Journal of Econometrics, 112, 207–223.
Weissman, M., Bland, R., Joyce, R. P., Newman, S., Wells, J. E., & Wittchen, H. U. (1993). Sex differences in rates of depression: Cross-national perspectives. Journal of Affective Disorders, 29, 77–84.
Wildman, J. (2003). Income related inequalities in mental health in Great Britain: Analyzing the causes of health inequality over time. Journal of Health Economics, 22, 295–331.
Wilkinson, R. G. (1996). Unhealthy societies: The afflictions of inequality. London: Routledge.
World Health Organization—WHO (2001). World Health Report 2001. Geneva: WHO. http://www.who.int/whr/2001.
World Health Organization—WHO (2003). Investing in mental health. Geneva: WHO.
World Mental Health Survey Consortium (2004). Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. The Journal of The American Medical Association, 291, 2581–2590.
Zimmerman, F. J., & Katon, W. (2005). Socioeconomic status, depression disparities, and financial strain: What lies behind the income–depression relationship? Health Economics, 14(12), 1197–1215.
Acknowledgements
We are grateful for the comments and suggestions received from three anonymous referees. These have enabled us to improve the clarity of the contribution. We also thank the Autonomous Government of Catalonia for research project 2005-SGR-460 and the Ministry of Science and Technology for projects SEJ2005-03196/ECON and SEJ2005-06270/ECON. Joan Costa-Font thanks the support from the Institut Ramon Llull, Generalitat de Catalunya.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Costa-Font, J., Gil, J. Would Socio-Economic Inequalities in Depression Fade Away with Income Transfers?. J Happiness Stud 9, 539–558 (2008). https://doi.org/10.1007/s10902-008-9088-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10902-008-9088-3