Abstract
Residing in lower socioeconomic status (SES) neighborhoods is associated with increased risk of morbidity and mortality. Few studies have examined this association for cardiovascular disease (CVD) outcomes in a treated population in New York City (NYC). The purpose of this study was to determine the relationship between neighborhood level poverty and 1-year clinical outcomes (rehospitalization and/or death) among hospitalized patients with CVD. Data on rehospitalization and/or death at 1-year were collected from consecutive patients admitted at a university medical center in NYC from November 2009 to September 2010. NYC residents totaled 2,198. U.S. Census 2000 zip code data was used to quantify neighborhood SES into quintiles of poverty (Q1 = lowest poverty to Q5 = highest poverty). Univariate analyses were used to determine associations between neighborhood poverty and baseline characteristics and comorbidities. A logistic regression analysis was used to calculate odds ratios for the association between quintiles of poverty and rehospitalization/death at 1 year. Fifty-five percent of participants experienced adverse outcomes. Participants in Q5 (9 %) were more likely to be female [odds ratio (OR) = 0.49, 95 % confidence interval (CI) 0.33–0.73], younger (OR = 0.50, 95 % CI 0.34–0.74), of minority race/ethnicity (OR = 18.24, 95 % CI 11.12–29.23), and have no health insurance (OR = 4.79, 95 % CI 2.92–7.50). Living in Q5 was significantly associated with increased comorbidities, including diabetes mellitus and hypertension, but was not a significant predictor of rehospitalization/death at 1 year. Among patients hospitalized with CVD, higher poverty neighborhood residence was significantly associated with a greater prevalence of comorbidities, but not of rehospitalization and/or death. Affordable, accessible resources targeted at reducing the risk of developing CVD and these comorbidities should be available in these communities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although overall deaths due to cardiovascular disease (CVD) have continuously decreased throughout the years, it is still the number one killer in the United States [1]. The association between neighborhood socioeconomic status (SES) and health outcomes is increasingly being assessed in order to determine what in the surrounding environment affects health, including CVD-related health status, beyond that of individual factors and the characteristics of those who may be affected disproportionately.
Research indicates that residing in neighborhoods of lower SES increases the risk of morbidity and mortality [2–14]. Studies have examined links between area-level deprivation or wealth with the incidence and prevalence of poor health outcomes such as low birth weight [15], asthma [16], physical activity [17], depression and mental health [6], stroke [4, 5], heart disease [3, 18], and increased mortality [3, 13, 18]. Others have looked at the availability and access to food and medical facilities, finding that deprived areas often have less access to both [16, 19–21].
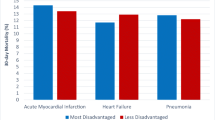
The relationship between residing in a disadvantaged neighborhood and having an increased risk of adverse outcomes has also been observed in cardiac outcomes. Examining the influence of socioeconomic factors in the community may provide a unique means of reducing the burden of CVD deaths. Many studies have found disparities in cardiac incidence, prevalence, and mortality when analyzed by area level SES in the United States and elsewhere [2–5, 7, 12]. For the most part, research indicates that the association still holds true after controlling for individual SES [3, 7, 8, 12]. Others have suggested that risk factors for heart disease such as smoking, obesity, and high cholesterol, may be mediators in the correlation [7]. Although results have been slightly inconsistent, most studies have found that the association between neighborhood disadvantage and poor cardiac outcomes is still visible even after controlling for these variables [2, 5, 6, 8, 12, 22].
A longitudinal study examining the incidence of stroke after having suffered a myocardial infarction based in Israel found an increased risk of stroke amongst those living in an area of lower SES [5]. Gerber et al. [1, 5] suggest that possible mechanisms for the increased risk among disadvantaged neighborhoods may be due to stress caused by the social norms of that community or poor quality of care, and not just the behavioral and disease risk factors commonly associated with strokes, e.g. smoking, diabetes, and hypertension. A nationwide study in France found similar results when examining the incidence of coronary heart disease (CHD) and area level deprivation. There was an inverse correlation between neighborhood SES and CHD incidence. In this case, after controlling for individual factors, the investigators did find that the classic risk factors mediated the link but only partly [7]. Silhol et al. [7] however stated the potential for a stronger relationship existed if analyzed at a smaller geographical level.
Little research has looked at how neighborhood SES specifically affects post discharge outcomes in a recently hospitalized cardiac population in NYC. The purpose of this study was to examine the relationship between neighborhood SES and the 1-year clinical outcomes (rehospitalization and/or death) of patients treated for CVD at a major NYC university hospital.
Methods
Study Population
The present substudy uses data from the National Heart, Lung, and Blood Institute-funded Cardiac Caregiver Investigation To Evaluate Outcomes (FIT-O) study [23, 24]. Participants enrolled in FIT-O were consecutive patients admitted to the cardiac units of a major university medical center in NYC from November 2009 to September 2010. This prospective cohort study sought to examine the association between having a caregiver and the clinical outcomes of those who were hospitalized with cardiovascular disease. Although caregiver status was not a variable examined in the current analysis, the definition used for a caregiver in the parent study was a person, paid or non-paid, who assists the patient with medical and/or preventive care [23]. The methods from this parent study have previously been described elsewhere [23, 24].
Briefly, eligible participants were identified daily by the hospital’s admission log. Patients were excluded from participating if they were unable to read or understand English or Spanish, if their permanent residence was in a nursing facility, or if they declined participation. Surveys regarding caregiver status were systematically distributed to eligible participants of the cardiovascular service line by trained research staff. Electronic chart review for key baseline variables and comorbidities was also conducted. Rehospitalization and/or death at 1-year post-hospitalization were assessed through electronic medical records and were supplemented by a follow-up survey. The follow-up survey was completed through a telephone or mail interview administered approximately 1 year from the initial hospitalization. The FIT-O study was approved by the Institutional Review Board of Columbia University Medical Center (CUMC) and all participants gave informed consent [23].
For the current substudy, the sample was limited to those who lived in NYC (n = 2,198). Zip codes were selected as proxies for neighborhoods. The participants’ zip code of residence obtained at baseline was used to determine residency in NYC and to subsequently assign the SES of their neighborhood. Twenty participants could not be assigned a neighborhood because they did not report an address or their zip code reflected a post office box. Zip code tabulation area (ZCTA) data from the 2000 US Census was used to quantify the neighborhood SES into quintiles. Zip code tabulation areas are geographic approximations of United States Postal Service zip codes used by the decennial census in order to provide better estimations of land areas [25]. Census tracts, a smaller subdivision initially created to represent a more homogenous population [26], are often used to assess the influence of neighborhood SES on various health outcomes. Studies measuring this association in NYC have often used zip codes to represent neighborhoods [19, 27–29].
From the Census 2000 Summary File 3, the measure “Percentage of Individuals Living Below the Federal Poverty Level” was selected to define each neighborhood’s SES. Previous research has found that the use of single variable measures such as poverty levels yielded similar results to more complex composite scores [2, 30, 31]. Kreiger et al. [30] suggest poverty may be the ideal indicator to use because it produces similar results to other multivariable indices. Poverty status was categorized into the following quintiles in ascending order from least to most poverty in the neighborhood: <10 % (Q1), 10–19.9 % (Q2), 20–29.9 % (Q3), 30–39.9 % (Q4), >40 % (Q5). The cut points were chosen based upon the US Census Bureau definitions of poverty areas [32]. When 20 % or more of the population is living below the poverty line it is considered a poverty area. When rates are as high as 40 % or more, it is then deemed an extreme poverty area [32].
Study Measures
The main outcome variables measured were death and/or rehospitalization at 30 days and 1-year post-hospitalization. As previously described, hospitalizations and death were ascertained by electronic medical records and were supplemented by the 1 year follow-up survey. Demographic factors including sex, race/ethnicity (White, Hispanic, non-Hispanic Black, other), age, and insurance status (yes or no) were among the individual covariates assessed. Cardiovascular risk factors and comorbidities were also obtained at baseline. Participants’ smoking status was reported as yes or no to being a current/recent smoker within the previous year. Body mass index was classified as underweight (≤18.5 kg/m [2]) or overweight/obese (≥25 kg/m [2]), each analyzed separately. Current or prior history of hypertension or dyslipidemia was identified via medical chart.
The history and prevalence of other medical conditions were determined using the International Classification of Disease, 9th Revision (ICD-9), billing codes, via electronic medical chart review. These include prior or current diabetes mellitus, renal disease, heart failure, peripheral vascular disease, stroke, and chronic obstructive pulmonary disease. The Ghali co-morbidity index, a measure of disease burden, was also computed for each participant [33]. Scores range from 0–11, with higher scores indicating greater comorbidities, which have been correlated with greater risk for adverse outcomes. Scores were dichotomized as ≤1 versus >1 due to research indicating significant disease burden observed with scores >1 [24].
Statistical Analysis
Descriptive statistics were performed to describe the participant population at baseline. Participant characteristics were also stratified by neighborhood SES quintiles. Univariate analysis was used to determine any associations between neighborhood poverty levels and baseline characteristics and comorbidities and to assess candidate variables for multivariate analyses. Logistic regression analysis was performed in order to calculate the odds ratios for the association between poverty level and rehospitalization and/or death at 30 days and 1 year. Statistical significance was set at p < 0.05. All statistical analyses were performed using SAS software, version 9.2 (SAS Institute, Cary, NC).
Results
Baseline characteristics for the participants are detailed in Table 1. A majority of the population (58 %) was male, 41 % were white, and the mean age was 65 (SD = 14) at the time of hospitalization. Most participants were overweight or obese (75 %), had a history of, or current hypertension (71 %), and had prior cardiovascular disease (81 %). Nearly a quarter of participants reported no health insurance.
The distribution of the study population across neighborhood poverty quintiles was as follows: 11 % lived in Q1 (wealthiest), 23 % in Q2, 30 % were in Q3, 27 % lived in Q4, and 9 % resided in Q5 (most poverty). For ease of representation and interpretation, tables and analyses display the two extreme quintiles (Q1 and Q5) and the middle one (Q3). Table 2 describes participant demographics, comorbidities, and selected factors by neighborhood poverty status. In general, a higher poverty status was significantly associated with being minority, not married, and not having insurance. Living in Q5 as compared to Q3 was significantly associated with prior or current hypertension and prior peripheral vascular disease but the association was not seen between Q3 and Q1. Table 2 also shows that female gender and being a Medicaid recipient was associated with residence in Q3 versus Q1, but there was no significant association between Q5 and Q3 for these variables. A similar trend was seen in the prevalence of diabetes mellitus, where the association was significant between quintiles three and one but it was not observed between quintiles five and three.
Univariate associations were assessed between participant characteristics and the most and least deprived neighborhoods, Q5 and Q1 (Table 3). Living in Q5 compared to Q1 was significantly associated with being younger (odds ratio [OR] 0.50, 95 % Confidence interval [CI] 0.34–0.74), being female (OR 0.49, 95 % CI 0.33–0.73), and being of a minority race or ethnicity (OR 18.24, 95 % CI 11.12–29.93). Among the comorbidities examined, hypertension, diabetes and previous or current renal disease were significantly associated with residing in neighborhoods with the highest poverty, (OR 1.94, 95 % CI 1.27–2.98), (OR 2.13, 95 % CI 1.42–3.20), and (OR 1.77, 95 % CI 1.09–2.90), respectively. The odds of prior CVD were significantly associated with living in the wealthiest zip codes, Q1 (OR 0.50, 95 % CI 0.30–0.84). Abnormal body weight and having a Ghali Comorbidity Index >1 were not significantly associated with living in either Q1 or Q5.
Fifty-five percent of all participants experienced adverse outcomes (rehospitalization and/or death) within 1 year post initial hospitalization. Table 4 shows the association between poverty status and rehospitalization/death at 30 days and 1 year for each poverty quintile in reference to Q1, the wealthiest. Although there was a trend for the odds of death or rehospitalization to increase with increasing poverty level, no significant associations were found.
Interpretation
This study documented that among patients hospitalized for CVD, higher poverty levels were significantly associated with several demographic and CVD risk factors, and increased comorbidities including diabetes mellitus, hypertension, peripheral vascular disease, and renal disease. Those living in neighborhoods with the highest poverty levels were more likely to be young, minority, female, not married, and have no insurance. The association between poverty status and rehospitalization and/or death at 30 days and 1-year was not significant.
We used deprivation cut points defined by the US Census to quantify neighborhood SES. Q3 was identified as a poverty area (≥20 % live below poverty level) and Q5 as an extreme poverty area (≥40 %). Several significant associations were found between those living in Q5 and residents of Q1, the most advantaged neighborhoods. Participants in the uppermost quintile of poverty (Q5) were almost twice as likely as those in Q1 to have a history of hypertension, peripheral vascular disease, and renal disease. Of note, some significant associations in participant characteristics were also observed in those living in Q3 versus Q1. Namely, those who lived in Q3 had a significantly higher prevalence of diabetes mellitus than those in Q1. This suggests that appreciable effects of area-level poverty on an individual’s health are already measurable in areas that are not in the uppermost disadvantaged neighborhoods (Q5).
The association found between low SES areas and a greater prevalence of comorbidities and risk factors are in accord with other studies [5, 7, 9, 11]. The specific factors that were significantly associated with neighborhood deprivation varied by study. This substudy found that, while the prevalence of smoking and being overweight or obese did increase with greater disadvantage, this result was not statistically significant. Diabetes mellitus and hypertension were the only two variables with significant associations. Several studies in France and Australia did not find notable differences between neighborhood SES and diabetes, but did find a relationship existed with overweight/obesity and smoking [7, 9]. In a study conducted in Israel, Shimony et al. [11] found higher rates of smoking and diabetes correlated to lower neighborhood SES, but not hypertension. Differences in the location of study communities may account for the variations in findings between studies.
Since a higher prevalence of comorbidities was observed among higher poverty areas, greater rehospitalization and death rates might have been expected amongst higher poverty areas [34]. Although there was an increment in risk of death or rehospitalization at 30 days and 1 year with increasing neighborhood poverty levels, a statistically significant higher risk was not found. Several explanations may be implicated in the lack of significant association found. One possibility is that there simply is no correlation between neighborhood SES and death or rehospitalization amongst treated cardiac patients in NYC. Similarly, an Australian study found that obesity, smoking, and physical activity were independently related to neighborhood deprivation; however they did not find an increased risk of cardiovascular disease with increasing disadvantage [9]. However, a considerable amount of research indicates the contrary [3, 5, 8, 11, 13]. A state-level prospective analysis of six US states, the NIH-AARP Diet and Health Study, looked at cause-specific deaths in relationship with neighborhood SES [3]. They found that living in a deprived area increased the possibility of dying, with the highest risk from CVD-related deaths, even after controlling for traditional risk factors [3].
Considering the odds of adverse outcomes (albeit non-significant) was greater at 1 year than at 30 days, another possible explanation is that the 1 year follow-up period was insufficient to measure significant outcomes between neighborhoods. Numerous studies exploring post hospitalization outcomes in cardiac events have had a median of approximately 10 years of follow up, ranging from 1 to 14 years [5, 8, 11, 13, 19, 22]. Tonne et al. [22] used a comparable 1-year follow up period post discharge and found a significantly higher risk of death among the poorest neighborhoods. Their study however was limited to patients with acute myocardial infarction, which may have a less favorable prognosis than a patient population which includes chronic CVD among other cardiac diagnosis. Studies with longer follow up periods have found that the risk of adverse outcomes increased with increasing length of time [8, 11]. Others have measured incidence and mortality rates for different cardiovascular diseases based on population data, still using considerably longer study periods [3, 4, 7]. The larger sample size and lengthy study period (average of 10 years) may have allowed the researchers to capture more substantial effects of neighborhood SES.
Another possible explanation may be the significant age difference observed between the quintiles of poverty. Participants of the more deprived neighborhoods were generally younger than those of the wealthier areas and therefore may have better chances of survival. Older age is a well-established risk factor for CVD, and individuals 65 and older (whom comprised most of the richer zip codes) have a greater probability of poor outcomes, according to national data [1]. This age factor may be partially masking the effects of neighborhood deprivation on the rehospitalization or death rates. This is supported by the fact that those from wealthier neighborhoods had an approximately 50 % greater probability of having prior cardiovascular disease than those from the highest poverty zip codes, potentially due to their older age.
This larger prevalence of cardiovascular disease among richer neighborhoods may also hint at other contextual factors. For example, the younger population from the low SES neighborhoods may have been less likely to be diagnosed with prior cardiovascular disease due not only to their younger age, but also less access to healthcare. It is also quite notable that although the risk of death or rehospitalization was not significantly different between areas of different poverty levels, the comorbidities were highest amongst the younger population from Q5. In theory, this would imply that those from poorer neighborhoods would have greater adverse outcomes post-discharge. Since this was not the case, it may indicate that this population was not seeking care when needed. Due to the high percentage of uninsured residents in the highest poverty area, Q5, accessibility and affordability may have been an issue resulting in fewer rehospitalizations than expected, or possibly fewer prior diagnoses of cardiovascular disease. In a NYC-based study, however, Billings et al. [34] found that individuals in low income neighborhoods used hospitals at higher rates than those from richer neighborhoods. However, in terms of “higher-cost, more technology-intensive, referral-sensitive surgeries” which include many cardiac procedures, they found the opposite to be true. Therefore, the effects of environmental factors on an individual’s health may be manifested through complex relationships. A combination of these factors is likely to explain the unexpected finding amongst the participants of this substudy.
One of the study’s strength is its diverse sample size which reflects the demographic distribution observed in NYC’s population. For instance, 41 % of our participants were white, 33 % Hispanic, and 18 % were black, compared to 44 %, 29 %, and 26 % in NYC, respectively [35]. This is compared to other studies which have stated that lack of diversity in the race and ethnicity of their study population was a limitation in their study [2, 3]. Furthermore, the collection of clinical conditions was systematic, ascertained through medical chart review and included a variety of baseline risk factors and comorbidities.
A limitation of this study may be the use of zip codes to define neighborhoods. When comparing outcomes using census blocks, census tracks, and zip codes, Kreiger et al. [30] found that zip codes did not capture the same associations seen with the smaller units of analysis. In the current study, zip codes were deemed as a suitable measure of neighborhood due to the small, discrete areas (a median of 3.58 km2) which zip codes represent in NYC [27]. Furthermore, the NYC Department of Health and Mental Hygiene aggregates zip codes to roughly represent neighborhoods in order to report on the health of its communities [36]. This single site population, NYC, may however reduce the generalizability of the findings.
Another limitation is the use of the single variable measure of neighborhood SES, poverty status. Due to the complexity of neighborhoods, defining their characteristics using one variable may miss important aspects of a community [22, 37, 38]. In a study examining stroke and myocardial infarction mortality in the East Tennessee Appalachia Region, Pedigo et al. [4] used both a composite measure of SES, and individual variables that were independently tested. The authors found no significant increased risk between the single variable of neighborhood median household income with mortality [4]. They did however find a significant association between neighborhood education levels and death, suggesting that including other measures of SES may produce more meaningful results. On the other hand, Foraker et al. [2] investigated the relationship between fatal coronary heart disease and individual variables, and found significant associations for each neighborhood variable measured independently, including poverty level. Poverty has frequently been used to quantify neighborhood disadvantage [2, 39]. Nonetheless, it is possible that more complex scales may yield a more comprehensive measure of community level SES and allow separate analysis of component measures.
In conclusion, due to the greater prevalence of comorbidities among poverty and extreme poverty areas, resources should target programs simultaneously aimed at reducing the risk of developing cardiovascular disease and comorbid conditions in these communities. Considering the high percentage of uninsured population found in high poverty neighborhoods, affordable and accessible care should be a priority. Tailoring of such programs toward the predominantly younger, female, minority population living in higher poverty areas should also be considered. Greater efforts should be made to understand how the contextual environment may affect the health decisions, and subsequent increased cardiovascular risk, of those living in higher poverty neighborhoods.
References
Roger, V. L., Go, A. S., Lloyd-Jones, D. M., Benjamin, E. J., Berry, J. D., Borden, W. B., et al. (2012). Heart disease and stroke statistics–2012 update: A report from the American Heart Association. Circulation, 125(1), e2–e220.
Foraker, R. E., Rose, K. M., Kucharska-Newton, A. M., Ni, H., Suchindran, C. M., & Whitsel, E. A. (2011). Variation in rates of fatal coronary heart disease by neighborhood socioeconomic status: The atherosclerosis risk in communities surveillance (1992–2002). Annals of Epidemiology, 21(8), 580–588.
Major, J. M., Doubeni, C. A., Freedman, N. D., Park, Y., Lian, M., Hollenbeck, A. R., et al. (2010). Neighborhood socioeconomic deprivation and mortality: NIH-AARP diet and health study. PLoS ONE, 5(11), e15538.
Pedigo, A., Aldrich, T., & Odoi, A. (2011). Neighborhood disparities in stroke and myocardial infarction mortality: A GIS and spatial scan statistics approach. BMC Public Health, 12(11), 644.
Gerber, Y., Koton, S., Goldbourt, U., Myers, V., Benyamini, Y., Tanne, D., et al. (2011). Poor neighborhood socioeconomic status and risk of ischemic stroke after myocardial infarction. Epidemiology, 22(2), 162–169.
Stafford, M., Gimeno, D., & Marmot, M. G. (2008). Neighbourhood characteristics and trajectories of health functioning: A multilevel prospective analysis. European Journal of Public Health, 18(6), 604–610.
Silhol, R., Zins, M., Chauvin, P., & Chaix, B. (2011). Investigating the spatial variability in incidence of coronary heart disease in the Gazel cohort: The impact of area socioeconomic position and mediating role of risk factors. Journal of Epidemiology and Community Health, 65(2), 137–143.
Foraker, R. E., Rose, K. M., Suchindran, C. M., Chang, P. P., McNeill, A. M., & Rosamond, W. D. (2011). Socioeconomic status, medicaid coverage, clinical comorbidity, and rehospitalization or death after an incident heart failure hospitalization: Atherosclerosis risk in communities cohort (1987 to 2004). Circulation Heart failure, 4(3), 308–316.
Adams, R. J., Howard, N., Tucker, G., Appleton, S., Taylor, A. W., Chittleborough, C., et al. (2009). Effects of area deprivation on health risks and outcomes: A multilevel, cross-sectional, Australian population study. International Journal of Public Health, 54(3), 183–192.
Stafford, M., & Marmot, M. (2003). Neighbourhood deprivation and health: Does it affect us all equally? International Journal of Epidemiology, 32(3), 357–366.
Shimony, A., Zahger, D., Ilia, R., Shalev, A., & Cafri, C. (2010). Impact of the community’s socioeconomic status on characteristics and outcomes of patients undergoing percutaneous coronary intervention. International Journal of Cardiology, 144(3), 379–382.
Diez Roux, A. V., Merkin, S. S., Arnett, D., Chambless, L., Massing, M., Nieto, F. J., et al. (2001). Neighborhood of residence and incidence of coronary heart disease. New England Journal of Medicine, 345(2), 99–106.
Wen, M., & Christakis, N. A. (2005). Neighborhood effects on posthospitalization mortality: A population-based cohort study of the elderly in Chicago. Health Services Research, 40(4), 1108–1127.
Wen, M., Cagney, K. A., & Christakis, N. A. (2005). Effect of specific aspects of community social environment on the mortality of individuals diagnosed with serious illness. Social Science and Medicine, 61(6), 1119–1134.
Krieger, N., Waterman, P. D., Chen, J. T., Soobader, M. J., & Subramanian, S. V. (2003). Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: Geocoding and choice of area-based socioeconomic measures–the public health disparities geocoding project (US). Public Health Reports, 118(3), 240–260.
Peled, R., Reuveni, H., Pliskin, J. S., Benenson, I., Hatna, E., & Tal, A. (2006). Defining localities of inadequate treatment for childhood asthma: A GIS approach. International Journal of Health Geographics, 17(5), 3.
Wen, M., & Zhang, X. (2009). Contextual effects of built and social environments of urban neighborhoods on exercise: A multilevel study in Chicago. American Journal of Health Promotion, 23(4), 247–254.
Winkleby, M., Cubbin, C., & Ahn, D. (2006). Effect of cross-level interaction between individual and neighborhood socioeconomic status on adult mortality rates. American Journal of Public Health, 96(12), 2145–2153.
Fang, J., Negassa, A., Gern, R. W., & Alderman, M. H. (2006). Access to revascularization among patients with acute myocardial infarction in New York City—Impact of hospital resources. Journal of Urban Health, 83(6), 1085–1094.
Comber, A. J., Brunsdon, C., & Radburn, R. (2011). A spatial analysis of variations in health access: Linking geography, socio-economic status and access perceptions. International Journal of Health Geographics, 25(10), 44.
Dubowitz, T., Williams, M., Steiner, E. D., Weden, M. M., Miyashiro, L., Jacobson, D., et al. (2011). Using geographic information systems to match local health needs with public health services and programs. American Journal of Public Health, 101(9), 1664–1665.
Tonne, C., Schwartz, J., Mittleman, M., Melly, S., Suh, H., & Goldberg, R. (2005). Long-term survival after acute myocardial infarction is lower in more deprived neighborhoods. Circulation, 111(23), 3063–3070.
Mosca, L., Mochari-Greenberger, H., Aggarwal, B., Liao, M., Suero-Tejeda, N., Comellas, M., et al. (2011). Patterns of caregiving among patients hospitalized with cardiovascular disease. The Journal of Cardiovascular Nursing, 26(4), 305–311.
Mosca, L., Aggarwal, B., Mochari-Greenberger, H., Liao, M., Blair, J., Cheng, B., et al. (2012). Association between having a caregiver and clinical outcomes 1 year after hospitalization for cardiovascular disease. American Journal of Cardiology, 109(1), 135–139.
U.S. Census Bureau. Census 2000 zip code tabulation areas (ZCTAs). Available at: http://www.census.gov/geo/ZCTA/zcta2000.html. Accessed 25 February 2012.
U.S. Census Bureau. Census tracts and block numbering areas. Available at: http://www.census.gov/geo/www/cen_tract.html. Accessed 25 February 2012.
Rundle, A., Neckerman, K. M., Freeman, L., Lovasi, G. S., Purciel, M., Quinn, J., et al. (2009). Neighborhood food environment and walkability predict obesity in New York City. Environmental Health Perspectives, 117(3), 442–447.
McCarthy, A. M., Dumanovsky, T., Visvanathan, K., Kahn, A. R., & Schymura, M. J. (2010). Racial/ethnic and socioeconomic disparities in mortality among women diagnosed with cervical cancer in New York City, 1995–2006. Cancer Causes and Control, 21(10), 1645–1655.
Inagami, S., Borrell, L. N., Wong, M. D., Fang, J., Shapiro, M. F., & Asch, S. M. (2006). Residential segregation and Latino, black and white mortality in New York City. Journal of Urban Health, 83(3), 406–420.
Krieger, N., Chen, J. T., Waterman, P. D., Soobader, M. J., Subramanian, S. V., & Carson, R. (2002). Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. American Journal of Epidemiology, 156(5), 471–482.
Rose, K. M., Suchindran, C. M., Foraker, R. E., Whitsel, E. A., Rosamond, W. D., Heiss, G., et al. (2009). Neighborhood disparities in incident hospitalized myocardial infarction in four U.S. communities: The ARIC surveillance study. Annals of Epidemiology, 19(12), 867–874.
Bureau of the Census. Poverty Areas. (1995). Available at: http://www.census.gov/apsd/www/statbrief/sb95_13.pdf. Accessed 15 January 2012.
Ghali, W. A., Hall, R. E., Rosen, A. K., Ash, A. S., & Moskowitz, M. A. (1996). Searching for an improved clinical comorbidity index for use with ICD-9-CM administrative data. Journal of Clinical Epidemiology, 49(3), 273–278.
Billings, J., Zeitel, L., Lukomnik, J., Carey, T. S., Blank, A. E., & Newman, L. (1993). Impact of socioeconomic status on hospital use in New York City. Health Affairs, 12(1), 162–173.
U.S. Census Bureau. State and County Quick Facts. (2012). Available at: http://quickfacts.census.gov/qfd/states/36/3651000.html. Accessed 15 January 2012.
New York City Department of Health and Mental Hygiene. Community Health Profiles. (2012). Available at: http://www.nyc.gov/html/doh/html/data/data.shtml#2. Accessed 1 April 2012.
Messer, L. C., Laraia, B. A., Kaufman, J. S., Eyster, J., Holzman, C., Culhane, J., et al. (2006). The development of a standardized neighborhood deprivation index. Journal of Urban Health, 83(6), 1041–1062.
Braveman, P. A., Cubbin, C., Egerter, S., Chideya, S., Marchi, K. S., Metzler, M., et al. (2005). Socioeconomic status in health research: One size does not fit all. Journal of American Medical Association, 294(22), 2879–2888.
Gary-Webb, T. L., Baptiste-Roberts, K., Pham, L., Wesche-Thobaben, J., Patricio, J., Pi-Sunyer, F. X., et al. (2011). Neighborhood socioeconomic status, depression, and health status in the Look AHEAD (Action for Health in Diabetes) study. BMC Public Health, 19(11), 349.
Acknowledgments
This study was funded by a research grant from the National Heart, Lung, and Blood Institute (2RO1HL075101) to Principal Investigator, Dr. Lori Mosca. The authors would like to thank Beatrice Krauss, PhD and Ming Liao, MS for their assistance with this study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Villanueva, C., Aggarwal, B. The Association Between Neighborhood Socioeconomic Status and Clinical Outcomes Among Patients 1 Year After Hospitalization for Cardiovascular Disease. J Community Health 38, 690–697 (2013). https://doi.org/10.1007/s10900-013-9666-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-013-9666-0