Abstract
This study examined disparities in cervical cancer mortality rates among US women in metropolitan and non-metropolitan areas from 1950 through 2007. Inequalities in incidence, stage of disease at diagnosis, and patient survival were analyzed during 2000–2008. Age-adjusted mortality, incidence, and 5-year relative survival rates were calculated for women in metropolitan and non-metropolitan areas, and differences in relative risks were tested for statistical significance. Log-linear regression was used to analyze annual rates of change in mortality over time. During the last five decades, women in non-metropolitan areas had significantly higher cervical cancer mortality than those in metropolitan areas. Disparities persisted against a backdrop of consistently declining mortality rates. Throughout 1969–2007, both white and black women in non-metropolitan areas maintained significantly higher cervical cancer mortality rates than their metropolitan counterparts. Among black women, cervical cancer mortality declined at a faster pace in metropolitan than in non-metropolitan areas. In both metropolitan and non-metropolitan areas, black women had twice the mortality rate of white women. During 2000–2008, white, black, and American Indian women in non-metropolitan areas had significantly higher cervical cancer incidence rates than their metropolitan counterparts. Survival rates were significantly lower in non-metropolitan areas, particularly among rural black women. The 5-year survival rate for black women diagnosed with cervical cancer was 50.8% in non-metropolitan areas, compared with 60.2% for black women and 71.0% for white women in metropolitan areas. Disparities in survival existed after controlling for disease stage. Rural–urban disparities in cervical cancer have persisted despite steep declines in incidence and mortality rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is the third most common cancer in women and one of the leading causes of cancer death among women in the world [1]. It is also one of the top cancer sites in the United States, particularly among such ethnic minority women as blacks, Asians/Pacific Islanders, American Indians, and Hispanics [2]. In 2008, 12,200 US women were diagnosed with invasive cervical cancer and 4,018 died from it, which accounted for approximately 2% of all new cancer cases and deaths among women [2, 3]. Cervical cancer mortality rates in the United States have declined dramatically in the past 6 decades, from 13.1 deaths per 100,000 women in 1950 to 2.4 in 2007 [2, 4]. Incidence rates have also declined substantially over the past 3 decades, from a rate of 17.2 cervical cancer cases per 100,000 women in 1973 to a rate of 6.6 in 2008 [2]. Against the backdrop of consistently declining incidence and mortality rates, however, racial and socioeconomic disparities in cervical cancer have remained substantial [5, 6].
Trends in cervical cancer mortality are often analyzed by age and race in the United States [2, 4]. A few studies have also examined long-term trends and disparities in US cervical cancer mortality according to socioeconomic status [5–7]. However, the extent to which disparities in cervical cancer mortality rates between metropolitan and non-metropolitan areas have changed over time has not been studied. Since cervical cancer incidence has been shown to vary between rural and urban areas [8], cervical cancer mortality may also vary by urbanization levels.
Examining temporal patterns is important because it allows us to track progress toward reducing social and geographic disparities in cervical cancer mortality, such as those between metropolitan and non-metropolitan areas [5, 6]. Temporal analysis may also reveal important insights into the differential impact of cancer prevention and cervical cancer screening programs among rural and urban populations [5, 6]. Moreover, assessing rural–urban disparities in cervical cancer is consistent with the goals of Healthy People 2010 and 2020 that emphasize reduction or elimination of health disparities across geographic areas [9, 10].
In this study, we use a county-based rural–urban variable linked to national mortality data to examine the extent to which differences in cervical cancer mortality among US women in metropolitan and non-metropolitan areas have changed during the past 6 decades. We also analyze the magnitude of contemporary rural–urban disparities in cervical cancer incidence, stage of disease at diagnosis, and patient survival among major racial/ethnic groups in order to explain disparities in mortality.
Methods
To analyze rural–urban disparities in cervical cancer mortality over time, we used the national vital statistics mortality database [4, 11, 12]. Since the national mortality database does not allow the direct computation of mortality rates for people in rural and urban areas, a county-based rural–urban continuum variable was linked to the annual age-sex-county-specific mortality statistics from 1950 through 2007 [13–15]. The 1993 rural–urban continuum codes were used to analyze mortality data from 1950 to 1998, whereas the 2003 rural–urban definition was used to compute mortality rates from 1999 to 2007 [13, 14]. Trends in cervical cancer mortality for black and white women in metropolitan and nonmetropolitan areas were analyzed from 1969 through 2007. Each of the 3141 counties in the mortality database was assigned one of the two metropolitan-nonmetropolitan categories.
The rural–urban continuum variable was first developed in 1993 and revised in 2003 by the US Department of Agriculture [13–15]. This variable classifies all US counties into 9 distinct urban–rural groups, based on the population size of the counties and their proximity to metropolitan areas [13–15]. For this study, we used two broad groups of metropolitan and non-metropolitan counties. The metropolitan category includes large metro counties of a million people or more as well as smaller metropolitan counties of population <250,000. The non-metropolitan category includes small urban towns of population <20,000 as well as rural towns with a population of <2,500, which may or may not be adjacent to a metropolitan area [14]. In 2007, there were 2051 non-metropolitan and 1090 metropolitan counties. The metropolitan and non-metropolitan areas accounted for 83 and 17% of the total US population in 2007, respectively [14].
Age-sex-county-specific population estimates from 1950 to 2007, developed by the US Census Bureau, served as denominators for computing annual mortality rates [2, 4, 12, 16]. Age-race-county-specific population estimates were also available from 1969 to 2007 to permit computation of mortality rates for white and black women in metropolitan and non-metropolitan areas [2, 4, 12]. Between 1950 and 2007, an estimated 344,325 cervical cancer deaths occurred in the US. Mortality rates for the metropolitan and non-metropolitan categories were age-adjusted by the direct method using the age composition of the 2000 US population as the standard and age-specific mortality rates for 19 age groups: <1, 1–4, 5–9, … ,80–84, 85+ years [2, 4, 5].
Annual age-adjusted cervical cancer mortality rates were calculated for women in both metropolitan and non-metropolitan areas. Race-specific analyses were conducted to examine if rural–urban patterns in mortality and incidence differed by race/ethnicity. While trends in mortality rates for white women are presented on an annual basis, trends in mortality for black women in both metropolitan and non-metropolitan areas were analyzed as three-year moving average rates. The moving average smoothing technique allows the identification of a trend more clearly by reducing some of the variability associated with rates based on small number of annual deaths among black women [5].
The 2000–2008 data on cervical cancer incidence, stage of disease at diagnosis, and patient survival were obtained from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) database [2]. We used data from 17 population-based SEER cancer registries, which include the states of Connecticut, Hawaii, Iowa, New Mexico, Utah, California (San Francisco-Oakland, Los Angeles, San Jose-Monterey, and Greater California), Kentucky, New Jersey, Louisiana, Metropolitan areas of Detroit and Atlanta, Seattle-Puget Sound, Rural Georgia, and Alaska Native registry [2]. The 17 SEER registries cover approximately 26% of the total US population [2]. Average annual age-adjusted incidence rates were calculated for women in major racial/ethnic groups by urbanization level. Five-year relative survival rates by stage of disease were computed for women diagnosed with invasive cervical cancer during 2000-2007 and who were followed for vital status through December 31, 2008 [2]. Incidence, stage, and survival statistics by race/ethnicity and urbanization level were analyzed by using SEER*Stat software [2].
Log-linear regression models were used to estimate annual rates of decrease in mortality trends in metropolitan and non-metropolitan areas [17, 18]. Specifically, during the 1950–2007 or 1969–2007 period, the logarithm of the mortality rates were modeled as a linear function of time (calendar year), which yielded annual exponential rates of change in mortality rates [17, 18]. Metropolitan-nonmetropolitan disparities in mortality, incidence, stage, and patient survival were described by rate ratios or relative risks, which were tested for statistical significance at the 0.05 level [5, 6].
Results
Long-Term Trends in Cervical Cancer Mortality
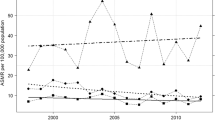
Rural–urban disparities in cervical cancer mortality persisted between 1950 and 2007 (Fig. 1). In 1950, the cervical cancer mortality rate for women living in non-metropolitan areas was 12.1 deaths per 100,000 population, 10% lower (RR = 0.90; 95% CI = 0.85–0.94) than the rate of 13.5 for those in metropolitan areas. Starting with the decade of the 1960s, women in non-metropolitan areas had higher cervical cancer mortality rates than women in metropolitan areas. In 2007, the age-adjusted cervical cancer mortality rate for women in non-metropolitan areas was 2.9 deaths per 100,000 population, 22% higher than the rate of 2.3 for those in metropolitan areas (RR = 1.22; 95% CI = 1.13–1.32).
Long-term trends in metropolitan and non-metropolitan disparities in cervical cancer mortality were generally similar for white and black women (Fig. 1). Despite consistently declining mortality rates, both white and black women in non-metropolitan areas experienced higher mortality risks than their metropolitan counterparts throughout 1969–2007. In both 1969 and 2007, white as well as black women in non-metropolitan areas had an approximately 24–29% higher cervical cancer mortality than their counterparts in metropolitan areas. Moreover, racial disparities in cervical cancer mortality remained marked, with black women experiencing at least two-fold higher risk of mortality than white women in both metropolitan and non-metropolitan areas throughout the period 1969–2007. Additionally, non-metropolitan black women had approximately three-fold higher cervical mortality than metropolitan white women throughout 1969–2007.
During 1950–2007, cervical cancer mortality decreased at 3.34% per year in metropolitan areas, significantly faster than the annual rate of decrease of 3.07% in non-metropolitan areas. Among the four race and urbanization groups, black women in metropolitan areas experienced the fastest decline in cervical cancer mortality during 1969–2007. The average annual rates of mortality decline were 3.68% for metropolitan black women, 3.15% for non-metropolitan black women, 2.63% for metropolitan white women, and 2.66% for non-metropolitan white women. Because of more rapid declines in mortality among black women, the black/white disparity in cervical cancer mortality narrowed over time in both metropolitan and non-metropolitan areas.
Recent Patterns in Cervical Cancer Mortality, Incidence, Stage at Diagnosis, and Survival
Contemporary mortality and incidence data indicate that cervical cancer rates increased in relation to increasing levels of rurality for all racial/ethnic groups except Hispanics (Fig. 2; Table 1). The broader non-metropolitan category is broken further into small-urban and completely rural areas. During 1999–2007, women in small-urban non-metropolitan areas and in completely rural areas had, respectively, 15 and 20% higher cervical cancer mortality risks than those in metropolitan areas. Differences in mortality were particularly marked among American Indian and black women. American Indian and black women in rural areas had 2.8 and 1.4 times higher mortality risks than their metropolitan counterparts, respectively (Table 1).
During 2000–2008, women in small-urban as well as in rural areas had, respectively, 6 and 15% higher cervical cancer incidence rates than women in metropolitan areas (Table 1). Non-Hispanic white and black women in rural areas had, respectively, 28 and 61% higher incidence rates than their metropolitan counterparts. However, Hispanic women in small-urban nonmetropolitan areas had 20% lower incidence rates than Hispanic women in metropolitan areas.
Even though women in non-metropolitan areas had a higher likelihood of being diagnosed at a more advanced (regional or distant) stage of cervical cancer than their metropolitan counterparts, the difference was not statistically significant (Table 2). Of all racial/ethnic and urbanization groups, rural black women had the lowest likelihood of being diagnosed with a localized-stage cervical cancer (Table 2). Less than 41% of black women in non-metropolitan areas were diagnosed with a localized-stage cervical cancer, compared with 51.0% of non-Hispanic white women in non-metropolitan areas and 52.9% of non-Hispanic white women in metropolitan areas.
Patient survival rates were significantly lower among non-metropolitan women, particularly among rural black women (Table 3). The 5-year survival rate for black women diagnosed with cervical cancer was 50.8% in non-metropolitan areas, significantly lower than the survival rate of 60.2% for black women in metropolitan areas and 71.0% for non-Hispanic white women in metropolitan areas. The 5-year survival rate for Hispanic women diagnosed with cervical cancer was 19% lower in non-metropolitan than in metropolitan areas (57.8 vs. 70.9%). Rural–urban disparities in survival existed even after controlling for stage of disease at diagnosis. Among women diagnosed with localized-stage cervical cancer during 2000–2007, the 5-year survival rate was 87.8% for non-metropolitan women, significantly lower than the survival rate of 91.3% for metropolitan women.
Discussion
In this study, we examined long-term trends in metropolitan-nonmetropolitan disparities in US cervical cancer mortality from 1950 through 2007. In order to better understand trends and patterns of disparities in mortality, we also analyzed contemporary rural–urban patterns in cervical cancer incidence, stage at diagnosis, and patient survival using data from 17 population-based SEER cancer registries. To our knowledge, this is first US study to systematically analyze temporal disparities in race-specific cervical cancer mortality rates by urbanization level.
Long-term data from 9 SEER cancer registries indicate a consistently downward trend in cervical cancer incidence rates between 1973 and 2008 and significant improvements in 5-year survival rates between 1973 and 2003 [2]. Thus, both reduced incidence rates and improved survival rates appear to have contributed to reductions in cervical cancer mortality over time in both metropolitan and non-metropolitan areas. However, time trends in the stage distribution of invasive cervical cancer cases did not show marked improvements in the percentage of cases diagnosed at localized stage. In 2008, 52% of invasive cervical cancers were diagnosed at localized stage, compared with 63% of cases in 1975 [2].
Racial/ethnic disparities in cervical cancer mortality remain quite marked in both metropolitan and non-metropolitan areas of the United States, with black women in particular having twice the mortality rate of white women. Based on the analysis presented here, such disparities in mortality seem to largely stem from racial/ethnic variations in both incidence and survival rates and to a smaller extent from inequalities in stage at diagnosis.
Metropolitan and non-metropolitan areas differ substantially in their socioeconomic characteristics [14]. The 2000 census data indicate higher poverty and unemployment rates and lower median family incomes in non-metropolitan areas compared to metropolitan areas [14]. Area deprivation and low socioeconomic status have been shown to be powerful determinants of cervical cancer mortality, incidence, and patient survival [5–7]. However, socioeconomic differences do not fully account for the rural–urban differences in cervical cancer mortality among both white and black women. For example, within counties with a poverty rate ≥20%, the age-adjusted cervical cancer mortality rate for white women in non-metropolitan areas during 1999–2007 was 3.3 per 100,000 population, 9% higher than the rate of 3.0 for white women in metropolitan areas. In high-poverty counties, non-metropolitan black women had 15% higher cervical cancer mortality than metropolitan black women. Additionally, within counties with a poverty rate <10%, the age-adjusted cervical cancer mortality rate for white women in non-metropolitan areas during 1999–2007 was 2.2 per 100,000 population, 16% higher than the rate of 1.9 for white women in metropolitan areas (analysis not shown).
The findings of this study are consistent with a previous study that showed higher cervical cancer incidence rates among rural women compared to women in metropolitan areas for the period 1998–2001 [8]. Although the rural–urban definition in the earlier study differed somewhat from our study, the age-adjusted cervical cancer incidence rates did increase by levels of rurality for all racial/ethnic groups except Hispanic women, a finding consistent with our study [8]. In our study, rural–urban disparities in incidence rates were partly due to differences in socioeconomic deprivation (data not shown). No significant differences were found between rural and urban areas in incidence rates for women living in affluent counties (poverty rate <10%). However, in middle-income (poverty rate = 10-19.99%) and high-poverty (poverty rate ≥20%) counties, non-Hispanic white women had significantly higher cervical cancer incidence rates in non-metropolitan areas than in metropolitan areas, whereas Hispanic women had significantly lower incidence rates in non-metropolitan areas than in metropolitan areas. This is compatible with the previous study that showed significant rural–urban disparities in cervical cancer incidence rates for black, Asian/Pacific Islander, and American Indian women even after adjustment for poverty level [8].
We did not find significant rural–urban disparities in stage of disease at diagnosis, and it is not clear the extent to which rural–urban disparities in cervical cancer screening may have contributed to declines in mortality rates over time. Detection of cancer at an early, localized stage may be considered a marker for access to health care and preventive health services, including cervical cancer screening. Screening can reduce rates of both cervical cancer incidence and mortality by detecting precancerous lesions (hence preventing cancer) and detecting invasive cervical cancers at an early stage, thereby increasing patient survival [19]. In 2008, 75.1% of US women reported having had a Pap test within the past 3 years [12]. Data from the National Health Interview Survey indicate that the proportion of women having had a Pap smear in the past 3 years has changed very little during the past two decades [12]. Although trend data on rural–urban disparities in use of Pap tests are lacking, an analysis of data from the 1998–1999 Behavioral Risk Factor Surveillance System showed that rural women were significantly less likely to receive a Pap test than women in metropolitan areas even after adjusting for socioeconomic and demographic differences [20].
Rural–urban and racial/ethnic disparities in cervical cancer incidence and mortality may also be due to differences in human papillomavirus (HPV) infection, the primary cause of cervical cancer [19, 21]. The 2005–2008 data from the National Health and Nutrition Examination Survey indicate a higher HPV prevalence among black and Mexican American women than among non-Hispanic white women [22]. However, data on HPV prevalence are not available by rural–urban residence.
The extent of metropolitan and non-metropolitan disparities in cervical cancer mortality, as documented here, contributes substantially to the overall cancer-related health disparities in the United States, since cervical cancer continues to be a leading cancer site among American women [2, 19]. Given the continuing disparities in incidence and survival, rural–urban disparities in cervical cancer mortality are not expected to diminish in the near future. Currently, rural or non-metropolitan women of all ethnicities as well as black and Hispanic women in metropolitan areas of the US have markedly higher cervical cancer mortality rates than the Healthy People 2010 goal of 2.0 deaths per 100,000 population [9]. Health policy interventions (e.g., cancer prevention and early detection programs through increased cervical cancer screening) aimed at reducing cervical cancer disparities should continue to target women in rural and medically underserved areas as well as high-risk populations in the metropolitan areas of the country.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, & Parkin DM. (2010). GLOBOCAN 2008, cancer incidence and mortality worldwide: IARC cancer base no. 10 [Internet]. Lyon, France: International Agency for Research on Cancer. Available at: http://globocan.iarc.fr. Accessed 22 June 2011.
Howlader N, Noone AM, & Krapcho M, et al (Eds). (2011). SEER cancer statistics review, 1975–2008. Bethesda, MD: National Cancer Institute. http://seer.cancer.gov/csr/1975_2008/.
Kochanek, K. D., Xu, J. Q., Murphy, S. L., et al. (2011). Deaths: Preliminary data for 2009. Natl Vital Stat Rep, 59(4), 1–68.
Xu, J. Q., Kochanek, K. D., Murphy, S. L., & Tejada-Vera, B. (2010). Deaths: final data for 2007. Natl Vital Stat Rep, 58(19), 1–136.
Singh GK, Miller BA, Hankey BF, & Edwards BK. (2003). Area socioeconomic variations in US cancer incidence, mortality, stage, treatment, and survival, 1975–1999. NCI Cancer Surveillance Monograph Series, No. 4. Bethesda, MD: National Cancer Institute. NIH Publ No. 03-5417.
Singh GK, Miller BA, Hankey BF, & Edwards BK. (2004). Persistent area socioeconomic disparities in US incidence of cervical cancer, mortality, stage, and survival, 1975–2000. Cancer 101(5), 1051–1057.
Singh, G. K., & Siahpush, M. (2001). All-cause and cause-specific mortality of immigrants and native born in the United States. American Journal of Public Health, 91(3), 392–399.
Benard, V. B., Coughlin, S. S., Thompson, T., & Richardson, L. C. (2007). Cervical cancer incidence in the United States by area of residence, 1998–2001. Obste Gynecol, 110(3), 681–686.
US Department of Health and Human Services. (2006). Healthy people 2010: Midcourse review. Washington, DC: US Government Printing Office.
US Department of Health and Human Services. (2011). Healthy people 2020. Available at: http://www.healthypeople.gov/2020/default.aspx. Accessed 22 June 2011.
National Center for Health Statistics. (2011). National vital statistics system, mortality multiple cause-of-death public use data file documentation. Hyattsville, MD: US Department of Health and Human Services. Available at: http://www.cdc.gov/nchs/nvss/mortality_public_use_data.htm. Accessed 17 May 2011.
National Center for Health Statistics. (2011). Health, United States, 2010 with special feature on death and dying. Hyattsville, MD: US Department of Health and Human Services.
Butler MA, & Beale CL. (1994). Rural-urban continuum codes for metro and nonmetro counties, 1993. Washington, DC: Economic Research Service, US Department of Agriculture. Staff report 9425.
Bureau of Health Professions. (2010). Area resource file, 2009–2010, technical documentation. Rockville, MD: Health Resources and Services Administration.
Singh, G. K., & Siahpush, M. (2002). Increasing rural-urban gradients in US suicide mortality, 1970–1997. American Journal of Public Health, 92(7), 1161–1167.
US Census Bureau. (2003). 2000 Census of population and housing, summary file 3, technical documentation. Washington, DC: US Department of Commerce.
Singh, G. K. (2003). Area deprivation and widening inequalities in US mortality, 1969–1998. American Journal of Public Health, 93(7), 1137–1143.
Singh, G. K., & Kogan, M. D. (2007). Widening socioeconomic disparities in US childhood mortality, 1969–2000. American Journal of Public Health, 97(9), 1658–1665.
American Cancer Society. (2010). Cancer facts and figures 2010. Atlanta, GA: American Cancer Society.
Coughlin, S. S., Thompson, T. D., Hall, H. I., et al. (2002). Breast and cervical carcinoma screening practices among women in rural and nonrural areas of the United States, 1998–1999. Cancer, 94(11), 2801–2812.
de Sanjose, S., Bosch, F. X., Munoz, N., & Shah, K. (1997). Social differences in sexual behaviour and cervical cancer. IARC Sci Publ, 138, 309–317.
National Center for Health Statistics. (2009). The national health and nutrition examination survey (NHANES), 2005–2008 public use data files. Hyattsville, MD: US Department of Health and Human Services. Available at: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed 22 June 2011.
Conflicts of interest
None.
Human Subjects Review
No IRB approval was required for this study, which is based on the secondary analysis of public-use federal databases.
Author information
Authors and Affiliations
Corresponding author
Additional information
The views expressed are the author’s and not necessarily those of the Health Resources and Services Administration or the US Department of Health and Human Services.
Rights and permissions
About this article
Cite this article
Singh, G.K. Rural–Urban Trends and Patterns in Cervical Cancer Mortality, Incidence, Stage, and Survival in the United States, 1950–2008. J Community Health 37, 217–223 (2012). https://doi.org/10.1007/s10900-011-9439-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-011-9439-6