Abstract
Childhood obesity is recognized as a major health problem in the United States and is occurring at ever younger ages. While most prevention efforts are aimed at school-age children, this project focuses on the caregivers of children from 0 to 24 months of age. This study is an evaluation of an educational English/Spanish infant feeding video, distributed for home viewing at one New York City Special Supplemental Food Program for Women, Infants and Children (WIC) center (video group) but not at three others (comparison group). Baseline, 3 and 6 month infant feeding knowledge and behavior surveys were conducted. For this report, analyses are restricted to Latina immigrant mothers. The video and comparison group mothers were similar in age, education, and parity. The video group was more likely to speak Spanish at home, and had lower knowledge scores at baseline. At the 6 month follow-up, knowledge increased for both groups, but the video group showed a greater increase in knowledge between baseline and 6 months: in ordered logistic regression analyses the video group had a 1.7 times greater score increase at each outcome level. The video group also showed positive changes in behavior—later age at first solid feeding was observed in the video group. We found that an inexpensive, low-intensity video intervention can positively impact maternal knowledge and behavior related to infant feeding among immigrant Latinas. Attention should be given to intervening early with high-risk populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The high prevalence of childhood obesity in the United States is a serious public health issue. Recently there has been an increased focus on early childhood. More than one-quarter of children 2–5 are overweight or obese according to large national studies such as the 2003–2004 National Health and Nutrition Examination Survey (NHANES) and 2007 Pediatric Nutrition Surveillance System (PedNSS) data [1, 2]. Studies from New York City (NYC) show even higher levels of overweight and obesity: a 2003 study of public elementary school children, found that 48% of kindergarteners were overweight or obese [3], and studies in programs such as Head Start and the Special Supplemental Food Program for Women, Infants and Children (WIC), which serve low-income communities, found levels at 42 and 38%, respectively [4, 5].
Given that studies estimate that one-quarter to one-third of pre-school age children are already overweight or obese, intervening to have an effect on diet and exercise at 2 years of age or older may be too late. A study of low-income minority pre-school children found that rapid weight gain in the first year of life was associated with obesity at 2–3 years of age [6]. A study of 1–5 year olds found that between ages one and two, the risk of overweight increased more than three fold [7]. Moreover, the onset of obesity is happening at early ages; according to the NHANES studies, the percentage of obese 2–5 year old children (defined as BMI-for-age at 95th percentile or higher) more than doubled from 5% in the 1970s and early 1980s [8], to 14% in 2003–2004 [1].
There are differences in the prevalence of early childhood obesity by race and ethnicity. Nationally, NHANES found that 25% of non-Hispanic White children and 24% of non-Hispanic Black children aged 2–5 were overweight or obese, in contrast to one-third (33%) of Mexican–American children [1]. The PedNSS survey of low-income children also shows differences in prevalence by race—36% of Latino children 2–5 were overweight/obese compared with 28% of non-Hispanic White children and 26% of non-Hispanic Black children of the same age [2]. In a WIC Center study from NYC, 42% of Hispanic children were found to be overweight or obese, compared with 27% of non-Hispanic Black children [4]. A study using data from the 2005 Early Childhood Longitudinal Study, Birth Cohort (ECLS-B) found that among 4 year old children in the US, there were significant differences in obesity by race. In the ECLS-B, Latinos had the second highest level of obesity (22%) (after American Indians), significantly higher than non-Hispanic White (16%) and Asian (13%) children, though not significantly higher than Black children (21%) [9].
Other recent research has found that young children of less acculturated immigrant mothers, as measured by exclusive use of the native language, were at greater risk of overweight compared to their more acculturated counterparts [10]. However, few published interventions addressed overweight and obesity among children under 2 years of age in populations of immigrant families.
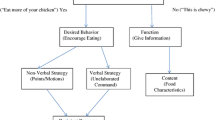
To provide a culturally appropriate behavioral intervention for parents of Latino infants and toddlers, we created a 25-minute educational video. The resulting English/Spanish video, “It’s Never Too Early: Feeding Your Baby Well/Empezando Temprano: La Buena Alimentación de Tu Bebé,” was developed using a professional production team and clients recruited from WIC Centers and other service locations. The video contains age-appropriate feeding messages divided into four chapters, 0–6 months; 6–12 months; 12–18 months and 18–24 months plus a fifth chapter about food and behavior. The data presented in this study are derived from an evaluation of the impact of the video among Latina WIC clients on changes in knowledge and behavior with regard to infant feeding.
Methods
Study participants were recruited from the Public Health Solutions Neighborhood WIC Program which serves over 45,000 women, infants and children in four of the five boroughs of NYC. Enrollment took place from June to October 2007. Using a quasi-experimental design, we enrolled a sample of women who received a free copy of the English/Spanish DVD to take home (video group) and another sample of women who did not receive the DVD (comparison group), in order to compare their knowledge and behavior at 3 and 6 month follow-up. The video group was recruited from the waiting room of a WIC Center in Queens, while the comparison group was recruited from three WIC centers, two in Queens and one in Brooklyn. Eligibility criteria for the mothers at the baseline interview were (1) self-identification as Latina; (2) speaking English and/or Spanish; (3) being 18 years of age or older; (4) having a singleton infant under 5 months old who was enrolled in WIC; and (5) agreeing to be contacted by telephone 3 and 6 months after the baseline interview. Mothers of non-singleton children, and infants who had been born prematurely or at low or very low birth weight were excluded. This study was approved by the Institutional Review Board of Public Health Solutions.
A total of 439 women were enrolled in the study: 368 (84%) completed 3 month and 339 (77%) completed 6 month follow-up interviews. The analyses presented are limited to the 272 women who completed the 6 month follow-up interview and who were born outside the United States or in Puerto Rico. The US-born mothers were excluded from the analysis because of the disproportionately small number of US-born women in the video group, 13 (8.3%) vs. 54 (29.5%) in the comparison group and their dramatically different characteristics. The US-born mothers were younger (mean age: 24 vs. 29), more likely to be obese (33 vs. 19%), to be primiparas (49 vs. 31%), and to be exclusively formula-feeding their infant (46 vs. 13%) (all P < .05).
Survey Development
Content that was covered in the video and included in the survey was derived from anticipatory guidance sources from the United States Department of Agriculture and the American Academy of Pediatrics [11–13]. The goal of the intervention was to encourage breastfeeding, the delay of feeding complementary foods until 6 months of age and to increase maternal knowledge of appropriate infant feeding practices. Our analysis is focused on those knowledge items most likely to result in excess weight gain and less healthy feeding habits in early childhood.
Survey Administration
At baseline, the participants were recruited and interviewed by trained bilingual (English/Spanish) interviewers in the waiting room of the participating WIC Centers. The interviewers consecutively recruited mothers and informed consent was obtained from all participants. Thirteen eligible women refused to participate. Using a structured questionnaire, participants were asked about demographic characteristics and infant feeding knowledge and practices. At the 3 and 6 month telephone interviews, the knowledge questions from the baseline were repeated. A feeding grid that asked about age of introduction of various foods was added to the 3 and 6 month surveys. From the feeding grid the timing of each item was determined, including whether it occurred before the baseline interview. The items on this grid included three kinds of juices, cereal, jarred baby foods, and fresh fruits and vegetables. In addition, the grid also contained non-recommended foods such as soda, sugar-sweetened juice drinks and flavored milk. At the end of the food grid, there was an open-ended question to ascertain when and whether any other food items had been introduced, including culturally specific foods.
The video and comparison groups answered identical baseline questionnaires adapted from the Bright Futures Nutrition series [12]. Immediately after the baseline interview the video group women were given a copy of the video in DVD format to take home with them. Formative survey research at a WIC site with similar demographics had shown that almost all of the women at the centers had access to DVD players or computers that could play DVDs. The 3 and 6 month surveys were the same for both groups with the exception of questions about viewing the video that were directed only to the video group. The children of respondents were not required to maintain enrollment in WIC during the 6 months of the study, though no mothers reported withdrawing from WIC at the 3 or 6 month interviews.
Data Analysis
Bivariate analyses were performed using SPSS statistical software version 14.0 (SPSS Inc., Chicago, IL). For baseline data, t-tests, Wilcoxon, or chi-square tests were performed as appropriate to assess the statistical differences between the video and comparison groups on maternal/infant characteristics, knowledge of four infant feeding items, and differences in timing of introduction of juice and solid foods.
Multivariate analyses were performed using Stata version 10 (Stata Inc., College Station, TX). An ordered logistic regression of change in knowledge over four points from reduced score to improved score by the 6 month follow-up was conducted [14]. Baseline characteristics that may affect these results were included in the model. Ordinary least squares were used to examine the effect of the video intervention on age at introduction of solids and juices taking into account baseline characteristics that differed between intervention and comparison groups.
Results
The 272 women who completed all three interviews, 143 video group participants and 129 comparison group participants, were Latina, between 18 and 45 years of age (median age: 29) and half had at least a high school education. The women were born predominantly in Ecuador (31%) and Mexico (31%) and 30% had been in this country 10 years or more (median time in the US: 7 years). At baseline the majority were not working or in school (84%) and were either married or living with their partner (73%). Of the mothers who received the video, at the 3 month interview 85% reported watching it (Table 1).
The video and control group mothers were similar at baseline, with some exceptions. The video group mothers were more likely to have been born in Ecuador (39.9 vs. 21.7%, P < .01) and to have been in the US less than 4 years (28.7 vs. 18.6%, P = .05), while the comparison group mothers were more likely to have been in the US over 10 years (37.2 vs. 23.1%). The video group was also more likely to speak only Spanish at home (74.8 vs. 60.2%, P = .05) (Table 1).
Knowledge of Age-Appropriate Infant Feeding Practices
We asked nine questions related to infant feeding knowledge, some related to obesity and some related to other feeding issues. Overall, the comparison group had higher knowledge at baseline of the questions related to the timing of feeding solids to infants and the question about the size of the baby’s stomach. The groups were about equally likely to be correct on the questions about breastfeeding. For example at baseline the comparison group showed somewhat higher knowledge of age-appropriate foods (nuts could make the baby choke) and the size of a baby’s stomach. These differences disappeared by the 3 month follow-up.
There were four knowledge items that were related to the development of obesity: (1) A sign that the baby was ready to eat solids (when she/he can sit with support); (2) The fact that solids do not replace formula/breastmilk at 6 months of age; (3) That solids become a baby’s main foods at 12 months of age and (4) That a baby’s stomach is the size of his/her fist. We excluded the breastfeeding items from the multivariate analyses because of little variation between the groups—approximately 95% of the participants knew the answers to the questions. By the time of the 3 month follow-up, a higher percentage of the video group knew at what age solids become a baby’s main food (74.4 vs. 56.6%, P < .01). While the comparison group had a significantly higher score on the four knowledge items (P < .05) relating to obesity at baseline, by the 3 month interview there was no significant difference in knowledge between the groups and improvement for the video group continued to the 6 month interview. The overall gain in scores for the intervention group was greatest from baseline to 6 months.
In an unadjusted ordinal logistic regression of the four knowledge items related to obesity indicated above, the video group showed a 1.7 times greater overall change in knowledge scores (OR = 1.74; 95% CI = 1.13–2.70, P = .01) compared to the comparison group. In a model of knowledge gain by intervention group adjusted for baseline characteristics known to differ between video and comparison group (years in the US, language spoken at home), the video group continued to have a significantly higher knowledge score and none of the other variables reached statistical significance. Other variables that may be related to change in knowledge, e.g. education, mother’s BMI, work status, birth order of child, were introduced into the model as well but were also not significant.
Feeding Behavior
There were no significant differences in age at introduction of complementary foods at the 3 month interview. However, at the 6 month interview, when those who had reported already feeding their infant solids at baseline were excluded, the video group had a later age at introduction of solids (5.2 vs. 4.9 months, P = .02) than the control group.
In ordinary least squares regression analysis the video group was more likely to begin feeding complementary foods at later, more appropriate ages (b = .309, 95% CI = .049–.569, P = .02) than the comparison group. When baseline characteristics were added to the model, this association remained and no other variables were statistically significant including years in the US, country of origin, and language spoken at home. No corresponding differences for introduction of juices were found between video and comparison groups and none of the other feeding behaviors differed between the video and comparison groups (see Table 2).
Discussion
The findings from this study suggest that a relatively inexpensive low-intensity video intervention can positively impact maternal knowledge and behavior related to infant feeding. Six months after the baseline interview, mothers who received the video showed more age-appropriate introduction of complementary foods.
To our knowledge there have been no other studies focused on evaluating early infant feeding interventions in low-income Latina immigrant populations. Since children as young as two are known to have a high rate of overweight and obesity, appropriate interventions are needed to assist caregivers of children less than 24 months of age in learning about and implementing recommended feeding guidelines [15]. However, we found a paucity of interventions for children less than 24 months of age which aim to delay the introduction of solid foods and help to guide caregivers about healthy feeding practices and prevent childhood obesity as recommended by the American Academy of Pediatrics [13]. In the literature there is a video intervention designed for young African–American mothers of newborns [16], and a nutrition education program for Early Head Start children age 11–36 months in Michigan, which excluded non-English speaking families [17]. Interventions in Australia to prevent overweight and obesity in infancy have also been described [18, 19]. Most often, however, efforts to prevent early childhood obesity have focused on children two and over [20–23], when children may already be overweight or obese.
Our study has several limitations. We used a quasi-experimental design in which the video and comparison groups were recruited at different locations. We were not able to implement a randomized design due to the potential for informal sharing of the video among women within a WIC center. We did not restrict enrollment of US born women at the outset, but small numbers and lack of comparability led us to exclude them for this analysis. Second, because we recruited mothers who had already given birth and made decisions about breast or formula feeding, it was too late to have an influence on mothers’ initiation or duration of breastfeeding. Third, at the 6 month interview, all the infants were under 1 year of age. There was no follow-up past this time to ascertain the long-term effects of the video intervention on BMI and whether changes in knowledge and later feeding of complementary foods were associated with a reduction in overweight and obesity when the video group children were older. However, because the video includes chapters for children up to 24 months of age, we expect that families who received the video will continue to use it as a resource. In fact, informal follow-up with the clinics where recruitment took place suggest that many participants do continue to use the video.
Despite these limitations, the finding that an inexpensively produced video in DVD format was associated with increased knowledge and more appropriate feeding of solids in a high-risk, low-income population of Latina immigrants is encouraging. Given the scarcity of interventions at birth for families of very young children, and evidence of substantial overweight and obesity by pre-school, future attention should be given to educating mothers and other family caregivers of infants about healthy, culturally appropriate feeding behaviors.
References
Ogden, C. L., Carroll, M. D., Curtin, L. R., McDowell, M. A., Tabak, C. J., & Flegal, K. M. (2006). Prevalence of overweight and obesity in the United States, 1999–2004. JAMA, 295(13), 1549–1555.
Polhamus, B., Dalenius, K., Borland, E., Mackintosh, H., Smith, B., Grummer-Strawn, L. (2009). Pediatric nutrition surveillance report 2007. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention.
Thorpe, L. E., List, D. G., Marx, T., May, L., Helgerson, S. D., & Frieden, T. R. (2004). Childhood obesity in New York City elementary school students. American Journal of Public Health, 94(9), 1496–1500.
Nelson, J. A., Carpenter, K., & Chiasson, M. A. (2006). Diet, activity, and overweight among preschool-age children enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Prev Chronic Dis, 3(2), A49.
Young, C. R., Peretz, P., Jaslow, R., Chamany, S., Berger, D., Brunetti, J., et al. (2006). Obesity in early childhood: More than 40% of Head Start children in NYC are overweight. NYC Vital Signs, 5(2), 1–2.
Goodell, L. S., Wakefield, D. B., & Ferris, A. M. (2009). Rapid weight gain during the first year of life predicts obesity in 2–3 year olds from a low-income, minority population. Journal of Community Health, 34(5), 370–375.
Irigoyen, M., Glassman, M. E., Chen, S., & Findley, S. E. (2008). Early onset of overweight and obesity among low-income 1- to 5-year olds in New York City. J Urban Health, 85(4), 545–554.
Ogden, C. L., Flegal, K. M., Carroll, M. D., & Johnson, C. L. (2002). Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA, 288(14), 1728–1732.
Anderson, S. E., & Whitaker, R. C. (2009). Prevalence of obesity among US preschool children in different racial and ethnic groups. Archives of Pediatrics and Adolescent Medicine, 163(4), 344–348.
Sussner, K. M., Lindsay, A. C., & Peterson, K. E. (2009). The influence of maternal acculturation on child body mass index at age 24 months. Journal of the American Dietetic Association, 109(2), 218–225.
Gartner, L. M., Morton, J., Lawrence, R. A., Naylor, A. J., O’Hare, D., Schanler, R. J., et al. (2005). Breastfeeding and the use of human milk. Pediatrics, 115(2), 496–506.
Story, M., Holt, K., & Sofka, D. (2002). Bright futures in practice: Nutrition (2nd ed.). Arlington, VA: National Center for Education in Maternal and Child Health.
Krebs, N. F., & Jacobson, M. S. (2003). Prevention of pediatric overweight and obesity. Pediatrics, 112(2), 424–430.
StataCorp. (2007). Stata base reference manual. Vol 2, I-P, Release 10. College Station: Stata Press.
Briefel, R. R., Reidy, K., Karwe, V., & Devaney, B. (2004). Feeding infants and toddlers study: Improvements needed in meeting infant feeding recommendations. Journal of the American Dietetic Association, 104(Suppl 1), s31–s37.
Black, M. M., Siegel, E. H., Abel, Y., & Bentley, M. E. (2001). Home and videotape intervention delays early complementary feeding among adolescent mothers. Pediatrics, 107(5), E67.
Horodynski, M. A., & Stommel, M. (2005). Nutrition education aimed at toddlers: An intervention study. Pediatr Nurs., 364(5), 7–72.
Campbell, K., Hesketh, K., Crawford, D., Salmon, J., Ball, K., & McCallum, Z. (2008). The Infant Feeding Activity and Nutrition Trial (INFANT) an early intervention to prevent childhood obesity: Cluster-randomised controlled trial. BMC Public Health., 8, 103.
Wen, L. M., Baur, L. A., Rissel, C., Wardle, K., Alperstein, G., & Simpson, J. M. (2007). Early intervention of multiple home visits to prevent childhood obesity in a disadvantaged population: A home-based randomised controlled trial (Healthy Beginnings Trial). BMC Public Health., 7, 76.
Fitzgibbon, M. L., Stolley, M. R., Schiffer, L., Van Horn, L., KauferChristoffel, K., & Dyer, A. (2005). Two-year follow-up results for Hip-Hop to Health Jr.: A randomized controlled trial for overweight prevention in preschool minority children. Journal of Pediatrics, 146(5), 618–625.
Fitzgibbon, M. L., Stolley, M. R., Schiffer, L., Van Horn, L., KauferChristoffel, K., & Dyer, A. (2006). Hip-Hop to Health Jr. for Latino preschool children. Obesity (Silver Spring), 14(9), 1616–1625.
Haire-Joshu, D., Elliott, M. B., Caito, N. M., Hessler, K., Nanney, M. S., Hale, N., et al. (2008). High 5 for Kids: The impact of a home visiting program on fruit and vegetable intake of parents and their preschool children. Preventive Medicine, 47(1), 77–82.
Johnson, S. L. (2000). Improving Preschoolers’ self-regulation of energy intake. Pediatrics, 106(6), 1429–1435.
Acknowledgments
The authors wish to thank Edith Letamendi, Diane Quintero, and Vanessa Bransburg, who interviewed the participants in this project. Funding for this project was provided by the New York State Assembly and Assembly Speaker Sheldon Silver.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scheinmann, R., Chiasson, M.A., Hartel, D. et al. Evaluating a Bilingual Video to Improve Infant Feeding Knowledge and Behavior Among Immigrant Latina Mothers. J Community Health 35, 464–470 (2010). https://doi.org/10.1007/s10900-009-9202-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-009-9202-4