Abstract
Previous research with travelers points to higher risk behaviors during vacations. Relative to their day-to-day lives, leisure travelers have more free time to pursue sexual activities and are likely to engage in higher rates of substance use than when at home. Risk behaviors during vacation have not been thoroughly examined in men who have sex with men (MSM), a key group at risk for HIV. The present investigation examined substance use, sexual risk behaviors, and components of the Information-Motivation-Behavioral Skills (IMB) Model in MSM attending Mardi Gras celebrations in New Orleans. Almost half of the sexually active men reported having sex with a partner of unknown HIV status while in New Orleans and a similar number did not disclose their own HIV status to all of their sexual partners. Drug use and excessive alcohol use were associated with unprotected sex (ps < .05). Components of the IMB model also predicted sexual risk behavior: individuals with more accurate HIV transmission information reported fewer unprotected sex acts, and motivation to engage in sexual activity on vacation was associated with more unprotected sex (ps < .05). Findings suggest that some MSM on vacation are placing themselves at risk for HIV. Traditional HIV prevention interventions do not readily lend themselves for use with transient populations. New intervention approaches are needed to reduce sexual risk behaviors in persons traveling for leisure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The role of travel in the spread of HIV has been noted since early in the AIDS epidemic. “Patient Zero,” a Canadian flight attendant, traveled extensively and was sexually linked with many of the early known AIDS cases.1 Subsequent investigations have cast doubt on the centrality of Patient Zero’s role, but the fact remains that widespread access to high-speed travel has heightened the spread of infectious disease.2–4 Individuals who travel between areas of high and low HIV prevalence and who engage in unprotected sexual activity in both settings may inadvertently spread HIV to areas that previously were little affected by the disease.
Leisure Travel and Risk Behavior
Persons traveling on vacation may be particularly likely to engage in high-risk sexual behavior. Compared to their everyday lives, travelers have more free time to pursue sexual activities and are likely to engage in higher rates of substance use.5–6 Travelers far from home may also have fewer inhibitions and some expect to find a new sexual partner while on vacation.7–11 Previous research suggests that many people engage in high-risk sexual behavior while on vacation.7–9,12–13 The majority of these studies have examined risk behaviors in young, heterosexual adults. In one representative study, Apostolopoulos and colleagues found that 30% of the men and 31% of the women in their sample of American college students reported having sex with a new partner first met during a spring break holiday.7
Leisure Travel and Risk Among Men who Have Sex with Men (MSM)
A small number of studies have examined risk behaviors in travelers who are men who have sex with men (MSM).14–16 For example, Clift and Forrest found that 52 percent of British MSM reported sex with a new partner while on vacation and that 30 percent reported sex with three or more new partners.14 Factors associated with unprotected intercourse included an expectation of sexual behavior while on vacation and having an HIV-positive status. Whittier and colleagues collected data from men vacationing in a popular beach town on the American east coast.16 Participating MSM reported sexual behavior during their time at the resort and for the previous 60 days spent in their home communities. Men on vacation reported 11 times more non-main sexual partners with whom they had engaged in unprotected anal intercourse at the resort community, versus at their homes. In our previous work, we documented relatively high rates of risk behavior in MSM travelers to Key West, Florida.17 In that study, 22% of MSM travelers reported anal sex with multiple partners over a brief holiday. HIV-negative men were significantly less likely to report multiple anal sex partners (18%), compared to men who were HIV-positive or who did not know their HIV status (45%). Overall, 34% of the sample indicated that they had anal sex with a new partner first met during their trip. In a second study with MSM travelers to Key West and Rehoboth Beach, Delaware, we found that unprotected sex was associated with substance use and use of medications to facilitate sexual activity (e.g., Viagra).18
The risk-taking behavior of MSM on vacation may play an important role in the dissemination of HIV and other STDs. MSM continue to account for the majority of new AIDS cases in the United States.4 Participants in the present study were MSM attending Mardi Gras festivities in New Orleans, Louisiana. Mardi Gras celebrations in New Orleans attract more than 1 million visitors each year, including significant numbers of MSM.19 Although Mardi Gras celebrations have changed somewhat in the wake of Hurricane Katrina, this annual festival continues to attract substantial numbers of visitors. Traditional festival activities include parades, dancing, alcohol consumption, and public displays of nudity, which are rewarded with beads or other tokens. As is the case with some other tourist destinations popular among MSM, a permissive atmosphere prevails, with many celebrants encouraging and reinforcing disinhibited behavior in their fellow festival attendees.
Theory and Risk During Leisure Travel
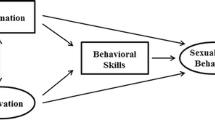
Although previous studies have documented high-risk sexual behavior in persons on vacation, few studies have examined the factors associated with risk among MSM traveling in the United States, particularly within the context of a coherent theoretical framework. The present study examined substance use, sexual risk behavior, and components of Fisher and Fisher’s Information-Motivation-Behavioral Skills (IMB) Model.20 The IMB model asserts that safer sexual decisions stem from having the correct information concerning HIV transmission, being sufficiently motivated to avoid HIV, and having the behavioral skills to enact safer sex behaviors.20 The Information component of the IMB model includes knowledge concerning HIV transmission, as well as information useful for avoiding exposure; the Motivation component includes expectations or motivations to engage in protective behaviors (or to avoid them), as well as perceived peer norms, and perceived personal vulnerability to the virus; the Behavioral skills component includes specific knowledge about protective measures (e.g., safer sex negotiation) as well as self-efficacy for skills enactment. Previous research has supported the utility of the IMB model in predicting risk and in planning intervention activities.20–21 In the present study, we anticipated that components of the IMB model would be significantly associated with risk reduction behaviors.
Methods
Procedures and Participants
A brief survey was administered to MSM recruited in the gay-oriented section of the French Quarter in New Orleans, LA. The study site was chosen because it is a popular tourist destination among MSM, and because New Orleans has a relatively high AIDS prevalence. Louisiana ranks sixth among U.S. states in current AIDS prevalence, with a significant portion of HIV infections occurring in metropolitan New Orleans.22–23 More than half of New Orleans’s AIDS cases have occurred among MSM.23 The survey was administered between the Friday before and the Tuesday of Mardi Gras, 2005. All study procedures and materials were approved by the Institutional Review Board of the University of Colorado at Denver & Health Sciences Center.
Participants were recruited as they walked through the gay section of Bourbon Street (90%) and from bars serving primarily gay clientele in the French Quarter (10%). Recruiters were outreach workers with substantial experience working with MSM. Participants were told that the survey was about the behavior of men on vacation, contained personal questions about their sexual history and substance use, was anonymous, and required approximately 10 minutes to complete. No formal incentive payment was offered, but participants were given Mardi Gras beads upon survey completion.
A total of 154 men completed the self-administered questionnaires. In order to insure that we were including in the analyses only individuals who were visitors to New Orleans, we asked participants to provide their home zip code. Men that provided a home zip code indicating that they traveled at least 50 miles to visit New Orleans were classified as visitors. Some participants were ineligible because they self-identified as heterosexual and reported no male sex partners (n = 10), reported a home zip code that indicated they traveled less than 50 miles to visit New Orleans (n = 3), or reported no zip code and therefore could not be classified as a visitor to New Orleans (n = 2). In addition, 7 participants (4%) were eliminated for problematic or random responding (e.g., circling multiple response choices). Of the 154 men who completed a survey, 132 (86%) were eligible for inclusion.
Measures
Participants completed a 2 ½ page self-administered anonymous survey that included questions assessing demographic information, time spent in New Orleans, sexual behavior, substance use in conjunction with sexual behavior, and measures related to the IMB model.
Demographics
Participants were asked their age, years of education, ethnicity, home zip code, sexual orientation, and HIV status.
Days in New Orleans
We asked participants how many days they had spent in New Orleans on their current trip.
Sexual Behavior and Sexual Partners
Participants reported the total number of times they had engaged in protected and unprotected receptive anal sex and protected and unprotected insertive anal sex during their present trip. They also reported the number of partners with whom they had engaged in each of these acts. In addition, participants responded to yes or no questions asking whether or not they had asked all of their sexual partners about their HIV status, and if they had disclosed their own HIV status to each of their sexual partners. Measures of sexual behaviors similar to those used in the present study have acceptable reliability and have shown utility in previous research.24–26
Substance Use in Conjunction with Sexual Activity
Participants were asked the number of times they had anal sex after having “too much to drink,” and the number of times they had anal sex after using drugs during their stay in New Orleans.
Components of the IMB Model
Information about HIV Transmission and HIV Prevalence in New Orleans
Participants were asked to respond to the True/False item, “The HIV rate in New Orleans is relatively low (below average) for a large U.S. City.” Participants were also asked four True/False questions assessing HIV transmission knowledge (e.g., “You can tell by looking at someone if they are infected with HIV”). Similar items have shown utility in previous research.27
Motivation to Avoid HIV
Consistent with Fisher and Fisher’s conceptualization of motivations to avoid HIV within the IMB model, we assessed participants’ perceptions of peer norms for vacation sex (e.g., “My friends always use condoms when they have sex on vacation.”). Items were modified from measures validated in previous research.28 Response choices ranged from 1 (strongly disagree) to 4 (strongly agree). Internal consistency for this measure was good (α = 0.82). Three items measured personal motivations or expectations for sex on vacation on the same 4-point scale. (e.g., “A big part of having a fun vacation is finding new guys to have sex with.”). Internal consistency for this measure was good (α = 0.84).
Behavioral Skills to Avoid HIV
Consistent with Fisher and Fisher’s conceptualization of behavioral skills to avoid HIV, we asked two questions assessing self-efficacy for reducing personal risk of contracting HIV in the context of a high-risk situation (e.g., “If you meet a really hot guy here in New Orleans, how confident are you that you could convince him that the two of you should use a condom, even if he really prefers the feel of bare skin?”). Items were modified from the self-efficacy scale used for the NIMH Multisite HIV Prevention Trial.29 Response choices ranged on a 4-point scale from “not at all confident” to “completely confident.” Internal consistency for this measure was acceptable (α = 0.73).
Data Quality Assurance and Statistical Analyses
All surveys were examined for inconsistencies and invalid responses. Missing data were omitted from analyses, resulting in slightly different ns for various statistical tests. Because distributions of sexual behavior were highly skewed, nonparametric analyses were used as recommended by Hays.30 Two-tailed significance levels were used for all statistical tests.
Results
Participants
Among the 132 eligible participants, the mean age was 33.7 years (SD = 9.9; range = 18 to 62). The sample was well-educated, with 89% reporting at least some college education. The majority of the sample was White (73.5%), with the remainder being African American (9.8%), Latino (8.3%), Native American (4.5%) Asian American (1.5%), or other/mixed ethnic heritage (2.4%). The sample represented diverse regions of the United States: participants reported 92 distinct home zip codes, representing 23 U.S. states and the District of Columbia. U.S. participants traveled an average of 868 miles from their home to New Orleans (SD = 672). International participants (n = 8) indicated traveling to New Orleans from Canada and Europe. Eighty-five percent of eligible participants self-identified as gay and 15% self-identified as bisexual. Participants were most likely to report that they were HIV-negative (83.6%) with 7.8% reporting that they were HIV-positive, and 8.6% indicating that their HIV status was unknown. At the time of survey completion, participants had spent an average of 3.7 days in New Orleans (SD = 8.90).
Sexual Behavior
During their present trip to New Orleans, 62% of participants reported having no anal sex (protected or unprotected), 22% reported only condom-protected anal sex, and 16% reported unprotected anal sex. Among the 38% of the sample that reported they were sexually active during the present trip, 25% reported having one partner with whom they engaged in unprotected insertive anal sex and 9% reported having two or more unprotected insertive anal sex partners. The mean number of unprotected insertive acts for the sexually active men was 0.81 (SD = 1.85). Fifteen percent of sexually active participants reported having unprotected receptive anal sex with one partner, and an additional 9% reported having unprotected receptive anal sex with two or more partners. The mean number of unprotected receptive acts for the sexually active men was 0.55 (SD = 1.36). Almost half (48%) of the sexually active men reported having anal sex with a partner of unknown HIV status. A similar number (49%) did not disclose their own HIV status to all of their sexual partners in New Orleans.
Substance Use and Sexual Behavior
During their present stay in New Orleans, 48% of sexually-active participants reported having anal sex after having “too much” to drink and 19% reported having anal sex after using drugs. Having sex after having too much to drink was significantly correlated with having sex after using drugs (rho = 0.55, p < .001). Substance use in conjunction with sexual activity was associated with higher risk behaviors. Excessive alcohol use in conjunction with sex was a risk factor for engaging in unprotected anal sex (Odds Ratio [OR] = 1.40, 95% Confidence Interval [CI] = 1.02, 1.91, p < .05) as was drug use (OR = 2.34, 95% CI = 1.02, 5.40). Having anal sex after using drugs was also negatively correlated with disclosure of HIV status to sex partners (rho = −0.29, p < .05).
Information, Motivation, and Behavioral Skills
HIV-related information
Participants demonstrated high knowledge concerning how HIV is transmitted. Participants were likely to correctly indicate that New Orleans does not have a low HIV prevalence for a large U.S. city (86% correct). Overall, the mean score on the 5-item knowledge test was 4.75 (SD = 0.54), or 95% correct.
Motivation
Perceived peer norms
Participants generally perceived their peers’ behaviors to be safe. As shown in Table 1, the majority of participants believed that their friends would use condoms while having sex on vacation. Similarly, only a minority of participants believed that their friends would have unsafe sex on vacation when using drugs or alcohol.
Expectations concerning sex on vacation
Many participants appeared to have a heightened motivation for sex when on vacation. As shown in Table 1, most participants indicated that finding a new sex partner is part of what makes a vacation fun. A significant minority of participants also believed that their interest in sex and their sexual activity increases when on vacation.
Behavioral Skills
As shown in Table 2, participants had relatively high confidence that they could maintain safer sex practices even in a high-risk situation. Almost three-quarters (72.8%) were “very confident” or had “complete confidence” in their ability to set safer-sex guidelines with an attractive partner who wanted to have higher-risk sex. Similarly, a considerable majority (79%) indicated a high degree of confidence that they could refuse to have sex with an attractive partner who declined to use a condom.
Relationships between IMB Constructs and Sexual Risk Behavior
Information
Lower knowledge was associated with higher sexual risk behaviors. Individuals scoring higher on the knowledge scale reported fewer unprotected insertive anal sex acts (rho = −0.20, p < .05), fewer unprotected insertive anal partners (rho = −0.21, p < .05), fewer unprotected receptive anal sex acts (rho = −0.29, p < .01), and fewer unprotected receptive anal partners (rho = −0.29, p < .01).
Motivation
Expectations of having sex on vacation were correlated with total anal sex acts (protected or unprotected), rho = 0.25, p < .01. Expectations were also correlated with unprotected insertive anal intercourse acts (rho = 0.18, p < .05) and unprotected insertive anal intercourse partners (rho = 0.19, p < .05). Expectations were unrelated to unprotected receptive acts or partners. Perceived peer norms were not associated with sexual risk behavior in this study.
Behavioral Skills
Personal self-efficacy for avoiding high-risk behaviors was not related to sexual risk activity in the present sample.
Multivariate test of association between IMB constructs and sexual risk
We performed a multivariate logistic regression analysis to examine the independent effects of different IMB constructs on sexual risk behavior. Factors of the IMB Model (AIDS knowledge, perceived peer norms, expectations of sex on vacation, and self-efficacy) were entered as a block to predict if a participant had reported unprotected anal sex during his stay in New Orleans. The overall model was significant, χ2 (4, N = 112) = 11.20, p < .05. After accounting for the influence of other factors, higher AIDS knowledge was a significant protective factor, reducing the likelihood of unprotected anal sex (OR = 0.40, 95% CI = 0.17, 0.94), p < .05. Other factors included in the model did not significantly predict high-risk behavior, although expectations for having sex on vacation approached significance, p < .10.
Discussion
The majority of participants in the present study did not report high-risk sexual behavior during their visit to New Orleans. A substantial minority, however, did report sexual behavior that could place them or their partners at risk for HIV or STD infection. Considering the short duration of their stay in New Orleans ( < 4 days) this level of unprotected sexual activity is a concern.
Participants appeared to be well informed as to the modes of HIV transmission. This is consistent with the large number of HIV prevention programs directed at MSM, most of which have a strong informational or educational component.31–32 We found that AIDS information was a significant predictor of reduced sexual risk-taking in this sample. It may be beneficial to sensitize travelers to the risks associated with travel. For example, although participants demonstrated accurate HIV transmission knowledge, they were less likely to know that New Orleans is a relatively high HIV prevalence area. Interventions directed at tourists in New Orleans and similar locations may benefit from heightening travelers’ awareness of the local HIV rates. Information strategies might also incorporate health information into travel brochures or the travel web sites geared towards MSM. Sections featuring cities that attract large numbers of MSM tourists might include information on attractions, hotels, restaurants and safer sex tips. Fisher and Fisher’s IMB model suggests that accurate information is necessary but not sufficient for HIV risk behavior change.20 Prevention efforts aimed at MSM vacationers will also need to emphasize the motivational and behavioral skills components of the model.
In everyday life, the normative influence of a person’s social network may act to curb excessive substance use or high-risk sexual behaviors.33 Some vacation venues may have the opposite effect.9 There are many anecdotal and popular press accounts of the permissive atmosphere in many resort destinations popular among MSM and among heterosexual men and women. In many of these locations, high alcohol and substance intake are common, and a party atmosphere prevails.6,7,18 Such activities are entrenched in the milieu of these settings and are likely among the reasons travelers select this particular destination.34 It is unlikely that much can be done to alter these behaviors; however, perhaps interventions can curb the risk associated with such behaviors.
The IMB model suggests that motivation is an important factor in modifying sexual risk behavior.20 This study examined motivation in terms of individual’s expectations regarding having sex on vacation and peer norms regarding protective behaviors while vacationing. We found a small, but significant, relationship between expectations regarding finding sexual partners on vacation and sexual risk behavior. Insofar as travelers are choosing destinations based on the availability of willing sexual partners, it may be unrealistic to attempt to modify these attitudes. A useful approach may be to attempt to influence expectations regarding the outcomes of such behavior. If MSM vacationers have some expectation of negative consequences from engaging in high-risk behaviors, they may be motivated to take fewer risks. Most men in the present study were confident in their ability to maintain safer-sex behaviors under difficult conditions. However, safer-sex self-efficacy was not a significant predictor of safer behavior. Instilling the behavioral skills necessary for HIV prevention in a transient population is inherently challenging. Most effective HIV prevention interventions rely on multiple contacts with intervention participants, which is not a practical approach for use with travelers. However, one of the necessary conditions for condom use is condom availability. Efforts should be made to make condoms ubiquitous in MSM tourist areas. Condom packs with a variety of different, interesting and funny inserts could be provided to guest houses, restaurants, bars and other venues frequented by MSM.
As with much previous work, risk was highest for individuals who used alcohol or drugs in conjunction with sexual activity.35 Experimental investigations have indicated that intoxicated individuals show increased intentions to engage in unprotected sexual intercourse and are more likely to agree with a justification to do so than sober controls.36 Steele and Joseph’s work on “alcohol myopic vision” provides some evidence that the impairing effect of alcohol on cognition, attention and information processing leads to a narrowing of attention that may increase the possibility of engagement in disinhibited behaviors.37 Although the causal link between alcohol consumption and high-risk sexual behavior is debated in the literature, alcohol use in conjunction with certain contexts may serve to alter schemas associated with protective behaviors under specific circumstances.38 Successful interventions may also need to incorporate substance use moderation strategies.
Like much of the literature, the present preliminary study was limited by the use of convenience samples. Generalization to all MSM travelers or travelers to other types of tourist areas may not be warranted. An additional limitation was the necessity of utilizing very brief assessments of complex constructs. Guided only by the scant literature on MSM travelers, we designed reasonable, but necessarily limited, assessments of factors that may predict risk in this population. Additional research is needed to gain sufficient understanding of the context in which risk occurs, intentions for sexual activity on vacation, motivations for travel, information related to HIV risk while traveling, self-efficacy for engaging in HIV preventative behaviors while traveling, and other factors related to risk behaviors associated with leisure travel. A further limitation of the current study is that we did not assess if our participants were traveling with a companion or sexual partner. At least some of the sexual activity reported by participants in the present study may have been with a long-term partner with seroconcordant HIV status. However, the finding that 48% of our participants did not know the HIV status of all of their sexual partners suggests that sexual activity with a long-term partner did not account for all potentially high-risk behavior. Future work should conduct more detailed partner-by-partner assessments and should determine the type of each sexual partner (e.g., long-term, new partner, etc.).
Despite these limitations, this study is one of the few investigations of factors associated with sexual risk behavior in MSM vacationing in the United States. The present findings suggest several potential avenues for intervention, but additional research is needed. Future studies should attempt to assess if men’s substance use or sexual behavior differs on vacation versus their behavior in their home communities. Additional studies should also examine differences in key psychosocial factors (e.g., motivation for sex, self-efficacy for risk reduction behaviors) between home and tourist destinations. Finally, future work should examine men’s receptivity to risk-reduction efforts conducted in tourist areas.
References
Shilts R. And the Band Played On: Politics, People, and the AIDS Epidemic. New York: Penguin Books, 1987
Grassly NC, Fraser C, Garnett GP. Host immunity and synchronized epidemics of syphilis across the United States. Nature 2005;433:417–421
Rodriguez-Garcia R. The health-development link: Travel as a public health issue. J Com Health 2001;26:93–112
UNAIDS. AIDS Epidemic Update: December 2002. Geneva: Author, 2003
Bellis MA., Hughes K, Thomson R, Bennett A. Sexual behavior of young people in international tourist resorts. Sex Trans Inf 2004;80:43–47
Rogstad KE. Sex, sun, sea, and STIs: Sexually transmitted infections acquired on holiday. Br Med J 2004;329:214–217
Apostolopoulos Y, Sönmez S, Yu CH. HIV-risk behaviors of American spring break vacationers: a case of situational disinhibition? Int J STD AIDS 2002;13:733–743
Bellis MA, Hughes K, Lowey H. Healthy nightclubs and recreational substance use from a harm minimization to a healthy settings approach. Addict Beh 2002;27:1025–1035
Eiser JR, Ford N. Sexual relationships on holiday: A case of situational disinhibition? J Soc Pers Rel 1995;12:323–339
Mewhinney DM, Herold ES, Maticka-Tyndale E. Sexual scripts and risk-taking of Canadian university students on spring break in Daytona Beach, Florida. Canadian J Hum Sex 1995;4:273–288
Wright ER. Travel, tourism, and HIV risk among older adults. JAIDS 2003;33:S233–S237
Egan CE. Sexual behaviours, condom use and factors influencing casual sex among backpackers and other young international travelers. Canadian J Hum Sex 2001;10:41–58
Maticka-Tyndale E, Herold ES, Oppermann M. Casual sex among Australian Schoolies. J Sex Res 2003;40:158–169
Clift SM, Forrest SP. Factors associated with gay men’s sexual behaviours and risk on holiday. AIDS Care 1999;11:281–95
Crosby R, DiClemente RJ, Mettey A. Correlates of recent unprotected anal sex among men having sex with men attending a large sex resort in the south. Sex Trans Dis 2003;30:909–913
Whittier DK, St. Lawrence JS, Seeley S. Sexual risk behavior of men who have sex with men: Comparison of behavior at home and at a gay resort. Arch Sex Beh 2005;34:95–102
Benotsch EG, Mikytuck J, Ragsdale K, Pinkerton SD. Sexual risk and HIV acquisition among MSM travelers to Key West, Florida: A mathematical modeling analysis. AIDS Pat Care STDs 2006;20:549–556
Benotsch EG, Seeley S, Mikytuck J, Pinkerton SD, Nettles CD, Ragsdale K. Substance use, medications for sexual facilitation, and sexual risk behavior among traveling men who have sex with men. Sex Trans Dis 2006;33:706–711.
New Orleans Metropolitan Convention & Visitors Bureau. Visitor Statistics. Downloaded from < http://www.neworleanscvb.com/new_site/visitor/visstats.cfm>, July 3, 2005
Fisher JD, Fisher WA. Changing AIDS-risk behavior. PsychBull 1992;111:455–474
Benotsch EG, Kalichman SC. Preventing HIV and AIDS. In Glenwick D, Jason L (Eds.). Innovative Strategies for Promoting Health and Mental Health across the Lifespan. New York: Springer; 2002. pp. 205–226
Centers for Disease Control and Prevention. Cases of HIV infection and AIDS in the United States, 2003. HIV/AIDS Surveillance Report, Volume 15. Electronic document available online at http://www.CDC.gov, Accessed August 5, 2005
Louisiana Office of Public Health. Louisiana HIV/AIDS Annual Report, 2002. Downloaded from http://www.oph.dhh.louisiana.gov/HIVAIDS/index.html, July 3, 2005
Kalichman S, Benotsch EG, Rompa D et al. Unwanted sexual experiences and sexual risks in gay and bisexual men: Associations among revictimization, substance use, and psychiatric symptoms. J Sex Res 2001;38:1–9
Kauth MR, St. Lawrence JS, Kelly JA. Reliability of retrospective assessments of sexual HIV risk behavior: A comparison of biweekly, three month, and twelve month self-reports. AIDS Educ Prev 1991;3:207–214
Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: Prevalence, predictors, and implications for HIV prevention. Arch Sex Behav 2002;31:177–183
Benotsch EG, Pinkerton SD, Dyatlov RV et al. A comparison of HIV/AIDS knowledge and attitudes of STD clinic clients in St. Petersburg, Russia, and Milwaukee, WI, USA. J Com Health 2004;29:451–465
Kelly JA, Murphy DA, Sikkema KJ et al. Randomised, controlled, community-level HIV-prevention intervention for sexual-behaviour among homosexual men in U.S. cities. Lancet 1997;350:1500–1505
Murphy DA, Stein JA, Schlenger W, Maibach E, NIMH HIV Prevention Trial Group. Conceptualizing the multidimensional nature of self-efficacy: Assessment of situational context and level of behavioral challenge to maintain safer sex. Health Psychol 2001;20:281–290
Hays WL. Statistics. (4th Edition). Fort Worth: Holt, Rinehart, and Winston, 1988
Johnson WD, Hedges LV, Ramirez G et al. HIV prevention research for men who have sex with men: A systematic review and meta-analysis. JAIDS 2002;30(Suppl. 1):S118–S133
Stall RD, Hays RB, Waldo CR, Ekstrand M, McFarland W. The Gay ‘90s: A review of research in the 1990s on sexual behavior and HIV risk among men who have sex with men. AIDS 2000;14(suppl. 3):S101–S114
Kelly JA, St. Lawrence JS, Diaz YE, Stevenson LY. HIV risk behavior reduction following intervention with key opinion leaders of population: an experimental analysis. Am J Pub Health 1991;81:168–171
Gnoth J. Tourism motivation and expectation formation. Ann Tourism Res 1997;24:283–304
Leigh BC, Stall R. Substance use, risky sexual behavior for exposure to HIV: Issues in methodology, interpretation, and prevention. Am Psych 1993;48:1035–1045
Steele CM, Southwick L. Alcohol, social behavior I: The psychology of drunken excess. J Pers Soc Psychol 1985;48:18–34
Steele CM, Josephs RA. Alcohol myopia, its prized and dangerous effects. Am Psych 1990;45:921–933
Parsons JT, Vicioso KJ, Punzalan JC, Halkitis PN, Kutnick A, Velasquez MM. The impact of alcohol use on the sexual scripts of HIV-positive men who have sex with men. J Sex Res 2004;41:160–172
Acknowledgments
This study was supported, in part, by grants R21-MH078790, R34-MH 073409, R01-MH72474, T32-MH19985, K02-MH01919, and P30-MH52776 from the National Institute of Mental Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Benotsch, E.G., Nettles, C.D., Wong, F. et al. Sexual Risk Behavior In Men Attending Mardi Gras Celebrations In New Orleans, Louisiana. J Community Health 32, 343–356 (2007). https://doi.org/10.1007/s10900-007-9054-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-007-9054-8