Abstract
The burden of diabetes is more severe for minority populations than for the white population in the United States. Analysis of Medicare fee-for-service claims data revealed a significant disparity regarding screening for lipids between white and African-American Medicare beneficiaries with diabetes as measured by the biennial lipid profile indicator in New York State and the disparity was even greater in New York City. Thus IPRO, the Medicare New York State Quality Improvement Organization, launched a multifaceted quality improvement project to reduce the disparity, targeting African-American Medicare beneficiaries with diabetes in New York City and the providers who serve them. There was an absolute increase of 16.7% in the proportion of African-American beneficiaries with diabetes receiving a biennial lipid profile in the intervention areas and the disparity reduced by 9.8% between African-American and all eligible white beneficiaries in the intervention areas. Although it was not feasible to determine the direct impact of selected interventions on reducing the disparity, the interventions collectively appeared to be effective.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetes is a serious and growing public health problem. More than 18 million Americans currently have diabetes and 5.2 million of them are undiagnosed. Diabetes is the sixth leading cause of death in the United States, attributing to 71,252 deaths in 2001. It is the primary cause of blindness, non-traumatic amputations of lower limbs, and kidney failure among adults. Diabetes is a major cause of heart disease and stroke, which are responsible for about 65% of deaths among people with diabetes.[1] Diabetes also imposes a significant economic burden. Diabetes-related costs have increased sharply in the United States over the last five years, from $98 billion in 1997 to $132 billion in 2002.[2] Of this amount, $91.8 billion was due to direct medical costs and $39.8 billion to indirect costs such as lost workdays, restricted activity, and disability due to diabetes. On average medical expenditures for a person with diabetes was $13,243 or 2.4 times greater than the cost for a person without diabetes. The burden of diabetes is more severe for minority populations than for the white population in the United States. Diabetes is reportedly 1.4–2.2 times more prevalent in non-Hispanic African-Americans than white persons.[3] The prevalence of diabetes is greatest among African-Americans age 65 and over, with women accounting for a majority of cases. Moreover, African-Americans with diabetes are more likely to develop diabetic complications and experience greater disability from the complications than non-Hispanic white Americans with diabetes. A similar pattern is noted for African-Americans in New York State (NYS). In 2001, Diabetes was the seventh leading cause of death in NYS.[4] According to the 1995–1999 NYS Behavioral Risk Factor Surveillance System (BRFSS), African-Americans had the highest prevalence of diabetes (7.9%). The prevalence was higher than for whites across all age groups. Among African-Americans, the prevalence was greatest for those age 65 and older. The prevalence for African-Americans in this age range was 20.8%. African-Americans also had the highest rates of hospitalization discharges due to diabetes compared to whites and Hispanics for ages less than 65 years. Mortality rates due to diabetes among African-Americans were highest compared to Hispanics and whites for all age groups. More recent data from the 2001 NYS BRFSS found that the following characteristics were associated with a higher prevalence of diabetes: being African-American, female, age 55 and older, with a lower income (less than $25,000), and less than a high school level of education.[5]
The Centers for Medicare & Medicaid Services (CMS) recognizes that diabetes is a major chronic condition in the population it serves. The Health Care Quality Improvement Program (HCQIP) has included diabetes quality-of-care indicators since the sixth scope of work (6th SoW). The indicators are part of a more extensive evidence-based diabetes measure set first promulgated by the Diabetes Quality Improvement Project in 1998.[6]
One of the indicators, the biennial lipid profile, is a process-of-care assessment for the identification and treatment of atherosclerosis and prevention of cardiovascular disease. Diabetes is associated with a two- to four-fold excess risk of coronary heart disease. The consequences of atherosclerosis and dyslipidemia cause most of the morbidity and mortality in patients with diabetes.[7] Although African-Americans do not have a disproportionate rate of myocardial infarctions and strokes compared to the white population in the United States,[3, 8] they do have an increased prevalence of diabetes with its attendant cardiovascular disease burden. The dyslipidemia pattern most commonly seen in diabetics is elevated triglycerides and decreased high-density lipoprotein (HDL) cholesterol levels and the low-density lipoprotein (LDL) particles tend to be smaller and denser. Cook and colleagues have also found that the dyslipidemia pattern in African-Americans tends to include greater LDL abnormalities than in whites.[9]
The relative roles of lipids, glucose levels and blood pressure in cardiovascular disease is complex and incompletely understood.[8] Elevated levels of each are associated with poor outcomes. A meta-analysis by Huang et.al.[10] demonstrated that lipid lowering and blood pressure control are more important than intensive glucose control in the prevention of cardiovascular disease. A cost-effectiveness analysis by the CDC Diabetes Cost-effectiveness Group determined that the cost per quality-adjusted life year saved was more favorable for lipid control in older patients with diabetes than for glucose control, though glucose control clearly remains an important treatment goal.[11]
A survey performed by the American Diabetes Association and the American College of Cardiology found that although most people with diabetes see their physicians frequently, almost one half do not recall having any discussion with their physicians regarding cholesterol.[12] In addition, national surveys conducted in the late 1980s and early 1990s showed that African-Americans were less likely to receive lipid tests and self-monitor their blood glucose than non-Hispanic whites.[13, 14]
Baseline Data
An analysis of the diabetes data for NYS for the baseline period, April 1, 1999 to March 31, 2001, revealed a significant disparity regarding screening for lipids among white Medicare fee-for-service (FFS) beneficiaries with diabetes compared to African-Americans as measured by the biennial lipid profile indicator (Table 1). The disparity in New York City (NYC) was even greater than the statewide disparity. While 82.1% of white beneficiaries received lipid profile test during the measurement period of April 1999 through March 2001, only 66.1% of African-American beneficiaries in NYS received it. In all NYC counties, the percent of white beneficiaries that received the test was 83.0% and the percent of African-Americans was 63.9%. In addition, nearly 60% of all African-Americans with diabetes live in NYC.
It is for these reasons that the goal for the disparities project at IPRO, the Medicare Quality Improvement Organization (QIO) for NYS, was to improve biennial lipid profile evaluations in African-Americans residing in NYC. Richmond County was not included due to their small number of African-American Medicare FFS beneficiaries with diabetes (Table 7). The reference group was all white Medicare FFS beneficiaries with diabetes in the same counties (Table 7).
Underserved Population Group and Reference Group
The underserved population group comprised of African-American Medicare FFS beneficiaries with diabetes residing in the Bronx, Kings, New York, and Queens counties. The reference group was all white Medicare FFS beneficiaries with diabetes in the same counties (Table 6). Medicare FFS claims data for NYS, provided by the Outpatient Data Quality Improvement Organization Support Center (ODQIOSC) was used to examine the demographic characteristics of white and African-American Medicare FFS beneficiaries with diabetes in the intervention areas(Table 2).
There were marked differences between the African-American and white populations in the Bronx, Kings, New York, and Queens counties of NYC. The African-American population had a higher proportion of females, beneficiaries that were concurrently eligible for Medicaid, and beneficiaries aged 65 years and younger. The Medicaid status is a rough proxy for low income, and the younger age group may be a proxy for disability.
Multiple logistic regression analysis was performed to determine predictors of receipt of a biennial lipid profile for beneficiaries residing in NYC. The predictor variables included in the model were race, gender, age, and dual eligibility status, and the dependent variable was receipt of a biennial lipid profile. The results of the analysis reveal that race, age, and dual eligibility status predicted receipt of a biennial lipid profile and the corresponding p-values were statistically significant (Table 3). The following characteristics were each independently associated with a decreased likelihood of receiving a biennial lipid profile: African-American, age 65 and under, and concurrent enrollment in Medicaid. In addition, the interaction of race with age, dual eligibility status, and gender predicted receipt of lipid profile: older African-Americans and females age 66–75 were less likely to receive the test while the likelihood of receiving the test for African-American females overall and African-Americans dually eligible for Medicare and Medicaid, increased in contrast to the rest of the beneficiaries.
Analysis of claims data from subsequent interim periods, suggest that access-related factors may account for differences in lipid testing rates; African-American beneficiaries with diabetes in NYC don’t see the same providers as other beneficiaries (e.g., white, Hispanic, Asians, American Indians/Alaska natives) with diabetes. Providers that served at least 10 African-American beneficiaries in 2001–2002 were significantly more likely to have lower performance rates on diabetes indicators and their performance did not appear to vary by race. Furthermore, most of these providers (nearly 75%) saw less than 10 white beneficiaries with diabetes during the same time period.
The results of analysis of the distribution of eligible African-American beneficiaries by beneficiary ZIP code are presented in Table 4. More intense community interventions focused on these areas within NYC.
Data from the U.S. Census Bureau provided further insights into the demographic characteristics of African-Americans and whites in NYC. According to Census-2000 data, African-Americans comprised nearly 1/3 of the total population in NYC and almost a quarter of the population age 65 and older. In comparison, whites consisted of over 1/3 of the total population and nearly 60% of the population age 65 and older. More than 2/3 of African-Americans had at least a high school level education compared to over 3/4 of whites. The median household income for African-Americans was approximately $31,000 compared to more than $50,000 for whites. The percent of African-Americans age 65 and over below the poverty level was almost 25% compared to 12% of whites. The data also revealed a culturally and linguistically diverse African-American population. Nearly 1/3 of African-Americans in NYC were born outside of the U.S. and almost 90% of them were Latin-American (e.g., Caribbean, Central and South American). In addition, more than one in five African-Americans speak a language other than English and Spanish was the most common foreign language spoken at home. A similar trend was noted for African-Americans age 65 and older. These findings suggested the importance of incorporating culturally and linguistically appropriate interventions into our quality improvement activities.
The NYC Community Health Survey further illustrates the burden of diabetes among adults in NYC.[15] This cross-sectional survey of non-institutionalized adults age 18 and over with telephones in NYC was conducted over a 2-month period from May 2002 to July 2002. The results of the survey reveal a 2-fold increase in the prevalence of diabetes among adults in NYC during the past 8 years, from less than 4% in 1994 to nearly 8% in 2002. This rate was highest among Hispanics (12.2%) and African-Americans (10.8%) compared to whites and Asians (less than 7%). The burden of diabetes was highest in the Bronx and Brooklyn, followed by Queens, Manhattan, and Staten Island (Table 5).
Among adults age 40 and older, African-Americans were nearly 2 times more likely to have diabetes compared to whites. African-Americans with a high school level education or less were 1.6 times more likely to report a diagnosis of diabetes, compared to whites with the same level of education. Adults born outside the United States were found to have a higher prevalence of diabetes. Moreover, the survey revealed that the majority of adults reporting diabetes did not have the information to effectively manage their condition and reduce their risk of developing serious complications of diabetes: 89% of those reporting diabetes did not know their current hemoglobin HbA1c level; nearly two-thirds were unaware of their blood pressure; and over 75% did not know their cholesterol level. Among persons with diabetes who knew their HbA1c, African-Americans were more likely to report poorly controlled HbA1c (95%), compared to non-Hispanic whites (79%), Asians (75%) and Hispanics (70%). Overall, African-Americans were also more likely to be unaware of their level of HbA1c control (94%), compared to non-Hispanic whites (78%), Asians (57%) and Hispanics (90%). Less than 40% of persons with diabetes reported taking other basic preventive care steps such as taking aspirin to prevent heart disease, exercising regularly, and getting an annual flu shot.
In conclusion, the analysis of the baseline data provided by the ODQIOSC, the results of Census-2000 and the NYC Community Health Survey suggest that the disparity observed between eligible African-American and white beneficiaries in the receipt of a biennial lipid profile may be related to age, dual eligibility status, access, level of knowledge regarding effective diabetes management and cultural and linguistic barriers.
Project Setting and Targeted Population
IPRO interventions targeted both African-American Medicare beneficiaries as well as the providers who serve them in the NYC metropolitan area. Provider settings included physician offices, hospital-outpatient clinics (OPD), and community health centers.
Our community-based interventions targeted beneficiaries in senior centers, religious organizations, and senior housing complexes.
-
Provider Settings
-
Physician offices
-
Hospital-outpatient clinics
-
Community health centers
-
-
Community Settings
-
Senior centers
-
Religious organizations
-
Senior housing complexes
-
Providers targeted for most intense interventions included:
-
Targeted Facilities/Providers
-
African-American serving Physicians in NYC
-
Identified Participants of IPRO’s Physician Office Quality Improvement Project located in the Bronx, Kings, New York, and Queens counties
-
African-American serving OPDs and Community Health Centers
-
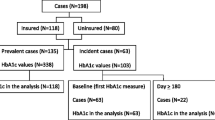
The Outpatient Data Reports: Diabetes and Breast Cancer Screening Performance and Provider Profiles, April 1, 1999–March 31, 2001 prepared by the ODQIOSC for NYS was used to identify targeted providers.[16] A total of 8,804 physicians have served the African-American Medicare FFS beneficiaries in NYS who met the CMS diabetes denominator criteria (hereafter referred to as “eligible” beneficiaries). The eligible beneficiaries were age 18–75 with a diagnosis of diabetes during the two-year measurement period, and had Medicare Part B coverage for at least 23 months of the measurement period. The diagnosis was identified from claims primary care providers submitted to Medicare. Seventy-four providers who saw at least 20 unique African-American Medicare beneficiaries with diabetes were identified as “African-American serving physicians”. Of these 74 providers, 47 (63%) were located within the four intervention counties of NYC. Fifteen of these 47 physicians were either hospital-based, retired, information on current practice was not retrievable, or declined to work with us and thus were not targeted. The remaining thirty-two African-American serving physicians in NYC were subjected to more intensive interventions to address the disparity in biennial lipid testing among eligible African-American beneficiaries, representing 6.7% of the target beneficiaries (Table 6).
In addition, 1,016 providers were identified as participants of IPRO’s Physician Office Quality Improvement Project (POQIP). Of these 1,016 providers, 339 who are located in NYC received disparities related interventions in addition to their general POQIP related interventions. Fifteen of the 339 providers have already been identified as African-American serving physicians, thus the remaining 324 providers linked to 8.6% of the targeted beneficiaries (Table 6).
IPRO also targeted OPDs and community health centers in NYC to increase our reach to the targeted beneficiaries. Many of these facilities provide primary care services both through their main OPD and through satellite clinics, all of which are not visible to Part B claims analysis. We estimate that 14.9% of the eligible African-American beneficiaries are served by these facilities (Table 6). This estimation is based on the 1,866 eligible African-American beneficiaries that were not linked to a physician UPIN on the outpatient data reports. In order to derive a list of OPDs and community health centers that submitted claims for treatment of Medicare beneficiaries, IPRO analyzed Part A claims. Claims submitted during the baseline period from April 1, 1999 to March 31, 2001 were captured for all eligible beneficiaries included in the baseline diabetes denominator file. The definition of an outpatient hospital clinic was based on the claims revenue codes describing services provided. Claims with at least one of the following charges: outpatient services (revenue code 50X), clinic services (revenue code 51X) or freestanding clinic (revenue code 52X), were used to identify OPDs and community health centers. For each facility, the number of unique African-American and non-Hispanic white eligible beneficiaries served was determined. Next, the performance measures for the biennial lipid screening indicator for African-American, white and all beneficiaries were determined for each facility using the beneficiary claim number (HIC) to link the part A claims data file to the baseline diabetes denominator file. The results of the analysis found a total of 17 facilities that have served the target population. Of these, 14 facilities had at least 10% of eligible beneficiaries identified as African-American. These facilities as well as those located in areas with a large proportion of eligible African-American beneficiaries were selected for provider interventions. IPRO defined areas with a large proportion of eligible African-American beneficiaries as those having ZIP codes where at least 50 percent of eligible beneficiaries are African-American (Table 4).
Beneficiaries Affected
During the baseline measurement period, there were 12,694 eligible African-American Medicare FFS beneficiaries in NYC, representing almost 60% of the statewide eligible African-Americans (n = 21,425). This represents 26% of the total eligible beneficiary population with diabetes in NYC. Based on analysis of baseline data for NYC provided by the ODQIOSC, only 63.9% of African-American beneficiaries with diabetes received a biennial lipid panel between April 1, 1999 and March 31, 2001, while 83.0% of white beneficiaries received a biennial lipid profile during the same time period, representing a 19.1% disparity (Table 1). Although our goal is to address the New York citywide disparity in the biennial lipid profile, the most intense interventions were directed at beneficiaries residing in the 4 boroughs of NYC. Richmond county was not targeted for intense interventions due to the small number of African-American Medicare beneficiaries with diabetes; approximately 1% of eligible African-American beneficiaries reside in Richmond county (Table 7).
Study Design
The study was a quasi-experimental design with one comparison group and a before-after analysis.
The underserved population group is the eligible African-American beneficiaries residing in NYC (excluding Richmond County). Both communities and the providers that serve them received the most intense interventions. The absolute improvement in the indicator over the study period, April 1,1999 to March 31, 2004, was compared against the reference group. The reference group received the statewide interventions that IPRO implemented for our POQIP. The description of the underserved population and the reference groups are summarized in Table 8.
Data Sources/Collection, Case Selection, and Sampling
The data for this project was based on the Medicare FFS claims data that was regularly updated by CMS and analyzed by the ODQIOSC. The ODQIOSC provided diabetes indicator information that was stratified by age, county, gender and race, as well as information necessary for provider-specific profiles.
Data Analysis
The claims data used in this project were summarized by the ODQIOSC. Additional analysis was conducted using the Statistical Analysis System (SAS)® statistical software version 8.2. All tests of significance were evaluated at the p<0.05 level. Descriptive statistics were obtained for all study variables. Multiple logistic regression analysis was performed to determine predictors of LDL testing for beneficiaries in NYC. A model containing the independent variables for race, gender, age, and dual eligibility status and dependent variable for lipid profile was conducted to estimate the odds ratios, 95% confidence intervals (CI), and p-values. Interactions between beneficiary characteristics and receipt of lipid profile were also examined by including interaction terms for these variables.
Interventions
Provider Interventions
IPRO reviewed the literature on effective interventions to improve the use of preventive health services and specific approaches to improve services for African-Americans. The review of effective interventions with underserved populations provided by CMS and the UQIOSC was especially helpful in identifying barriers and potential strategies.[17, 18] Barriers at the provider level identified in the review included lack of physician recommendation, inadequate tracking procedures (e.g., patient- and provider-oriented reminder systems), and cross-cultural barriers in the delivery of care. Other health systems barriers included poor organization of service delivery and lack of facilities or physicians (especially in low income and rural communities). Health system and community interface factors, specifically cost of services coupled with low incomes and inappropriate preventive health care interventions, were also recognized as barriers to preventive services. Effective provider interventions included interventions that focused on system changes surrounding the physician visit. Buy-in from the targeted physicians was an important factor for success.
Recently, the John Hopkins University Evidence-based Practice Center performed a systematic review of the evidence concerning the effectiveness of interventions designed to improve the quality of healthcare in racial and ethnic minorities.[19] There was excellent evidence that provider tracking and reminder systems improve the quality of healthcare among minorities. In addition, cultural competency training was found to be effective in improving patient satisfaction and cross-cultural attitudes, knowledge, and skills among healthcare providers. However there was fair evidence to support the use of multifaceted interventions, provider education, and the strategy of bypassing the physician to offer standardized services directly from a nurse or nurse practitioner to patients.
The selection of interventions was based both on the review of the literature and IPRO’s prior experience with quality improvement activities in the physician office setting. IPRO targeted African-American serving physicians for on-site visits to assess practice organization. The goal was to identify methods that work for individual practices in maximizing their lipid profile screening rates. The internally developed provider contact information system, a windows-based application, was used to track office contacts by telephone, in person, or by mail. IPRO’s provider contact information system also allowed for assessments by IPRO staff on the “organizational state” of the practice either by a free-text comment field or through a variation of the Stages of Change Model.[20] During the three-year project period, August 1, 2002 to July 31, 2005, our outreach staff completed 5 rounds of on-site visits. The initial on-site visits entailed an introduction of IPRO’s Diabetes Disparities project to the targeted providers, review of the American Diabetes Association’s (ADA) guidelines for screening for lipid disorders, and distribution of the provider toolkits developed by IPRO. The diabetes management toolkit for providers consists of various decision support tools including clinical practice guidelines for diabetes prevention and management (plus dyslipidemia in adults with diabetes), provider reminder materials (e.g., medical record flow sheets, chart stickers), and culturally- and linguistically-appropriate patient reminders and educational materials (e.g., pamphlets, posters, bookmarks). To standardize the data collected on initial assessment of the practice, the medical practice assessment (MPA) tool was subsequently developed. This comprehensive tool examines the practice’s cfapacity to participate and monitor various quality improvement activities as well as its’ motivational readiness for change. Specifically, we are able to determine the extent to which the practice is organized to address some elements of the Chronic Care Model such as decision support, clinical information systems, self-management support, and delivery system design. Moreover, the tool includes questions to ascertain the degree to which the practice has implemented the national standards for culturally and linguistically appropriate services (CLAS) in healthcare. Subsequent visits were conducted to provide technical assistance, promote the continuing medical education (CME) program launched by CMS, and implement the manual patient registry, Outpatient Rapid Assessment Tool (OPRA). As of this writing, over one-third of targeted providers have enrolled in the OPRA program.
Provider feedback was also part of our provider-oriented interventions. In December 2003, IPRO conducted a mailing of provider performance feedback reports to approximately 300 primary care physicians in NYC who have cared for a sizable number (≥ 10) of African-American Medicare beneficiaries with diabetes. The reports included provider-specific rates, the median rates for providers who care for a sizable number of African-Americans in NYC (by race), and a benchmark rate for four diabetes indicators: HbA1c testing, retinal examinations, lipid profile testing and a composite diabetes indicator based upon the average of the previous three measures. In February 2004, we sent our updated toolkits, on diabetes management, to these primary care providers as a follow-up to the provider profile mailing, and to provide additional resources for quality improvement efforts. This was followed by another mailing of provider performance reports in November 2004. A physician survey was also included in this mailing to get feedback on how we can further improve the content and quality of services IPRO offers physician offices.
In addition to on-site visits and provider feedback, IPRO has offered cultural competency training to providers statewide. In March 2003, IPRO, in conjunction with the New York State Department of Health (NYSDOH), held an educational session on cultural sensitivity & competency—a core element in improving health literacy. There is a direct correlation of health literacy with diabetes outcomes.[21] Moreover, providing culturally competent care has the potential to improve health outcomes, increase the efficiency of clinical and support staff and improve client satisfaction.[22] Hence, as part of National Public Health Week’s focus on eliminating health disparities (April 5–11, 2004), IPRO hosted the first introductory web-based training module on cultural competency training to improve diabetes care in African-Americans with offering of CME credits to providers participating in the teleconferences. Two additional teleconferences were hosted the following week. To optimize provider participation, the teleconferences were offered at various times on two separate days, however provider participation remained sub-optimal. The evaluations of the few that participated were 80% favorable. A recording of one of the teleconferences was made available on our website and distributed on CD-ROM. In March 2005, we launched our Diabetes Disparities website to assist providers in improving the quality of health care for minorities. Visitors to this website can access information on quality improvement products and services, practice guidelines, patient educational materials, CME programs, cultural competency and news items related to health disparities and diabetes.
IPRO also targeted OPDs and community health centers to increase our reach to African-American beneficiaries. Health care organizations participating in the New York City Department of Health and Mental Hygiene’s (NYC DOHMH) New York City Chronic Disease Collaboratives were invited to participate in our cultural competency training teleconference. IPRO also joined the Community Health Care Association of New York State (CHCANYS) in its efforts to increase community health centers’ participation in the Bureau of Primary Health Care’s Health Disparities Collaborative. IPRO continues to work with state and city government agencies in identifying and targeting practices for interventions. IPRO also works with the NYSDOH Office of Medicaid Management & Office of Health Systems Management in an intensive diabetes feedback effort to approximately 20 clinics and community health centers in both downstate and upstate New York.
Community Interventions
The review by CMS and the Underserved Quality Improvement Organization Support Center (UQIOSC) was also helpful in identifying barriers and potentially effective interventions at the level of the community and underserved person. Information and/or psychological barriers identified included myths and misconceptions, lack of knowledge, fear, suspicion, lack of trust, unfamiliarity with the health care system, and lack of social support. Effective community interventions involved community member staff, community advisory boards and partnerships, and included grassroots outreach, focus groups, pilot surveys, and community-based education.
IPRO has engaged various stakeholders to enhance community-based interventions to reduce the disparity. In November 2003, IPRO participated in the NYC Diabetes Summit hosted by the NYC DOHMH, and was a co-facilitator of the breakout session, entitled “Improving Clinical Diabetes Management in African American and Latino Populations.” This session generated great discussion on improving the quality of care for minorities with diabetes in NYC. In February 2004, IPRO hosted a follow-up meeting to continue this dialogue and coordinate the efforts of the various stakeholders who were already engaged in activities to improve quality of care and reduce morbidity and mortality from cardiovascular disease among African-Americans with diabetes in NYC. The stakeholders emphasized the importance of working within the existing diabetes task forces throughout NYC rather than convening another one dedicated to racial/ethnic disparities. IPRO has since submitted a letter of support for the Brooklyn Diabetes Task Force’s initiative, “LEAP to Health, Brooklyn!”, in response to the NYSDOH “Community Coalitions for Diabetes Prevention and Control” request for applications. As a result of the discussion that occurred during this meeting, a NYC Diabetes Clearinghouse is being developed for physicians and patients with diabetes. The goal will be to have one or two resource documents that these 2 populations can use to access services that are free or low cost.
In Fall 2003, focus groups were conducted to understand the population characteristics, point of view, needs, strengths, customs, preferred education styles, knowledge level, and beliefs regarding diabetes. IPRO worked with the ADA and the NYC Department for the Aging (DFTA) to identify African-American religious organizations and senior centers with high potential to reach a substantial proportion of the target population as sites to conduct focus groups. A focus group tool was developed to serve as a discussion guide. The groups were consistent with the project objectives and consisted predominantly of African-Americans. A total of five focus group sessions were held in the Bronx, Kings, and New York Counties, representing eighty-two participating seniors. The group size ranged from 9 to 35 with an average of 16 participants. Females comprised of the majority for most groups. Each session was one and one half hours in length and audio taped to capture qualitative information. Some key findings from the focus groups emphasized the need for: (1) cultural competency training for healthcare professionals to enhance provider-patient communication, (2) access to culturally appropriate formal diabetes educational programs, and (3) information on Medicare coverage for diabetes-related supplies and services. For some participants, religion played an important role in how they perceived and managed their diabetes. Many participants identified doctors, nurses, and the church as trusted sources of information on diabetes. These findings support many of the interventions adapted by IPRO to address the disparity in lipid profile rates.
The recommendations of the Task Force on Community Preventive Services were also influential in the development of our interventions. Based on the systemic review of published studies addressing the efficacy and cost effectiveness of population-based diabetes-related interventions in health care systems and in community settings, the Task Force strongly recommends disease and case management to improve the health of people with diabetes.[23] The Task Force also recommends diabetes self-management education (DSME) in community gathering places (such as community centers, libraries, and places of worship) for adults with type 2 diabetes, however there was insufficient evidence to determine the effectiveness of DSME in the home for those with type 2 diabetes.
Based on the Task Force recommendations, we partnered with nursing schools and NYC DFTA to provide culturally appropriate DSME as well as information on Medicare coverage for diabetes-related supplies and services to African-American beneficiaries in senior centers and religious organizations. This intervention addressed the need for diabetes education as demonstrated by the NYC Community Health Survey[15] and our focus groups. In Fall 2003, IPRO launched a pilot program in collaboration with Hunter-Bellevue College of Nursing to conduct DSME sessions in senior centers located in the Bronx, Manhattan, and Queens. IPRO also partnered with the SUNY Health Science Center at Brooklyn, College of Nursing to provide comprehensive diabetes education to African-American beneficiaries in Kings County, where over one-third of the target population resides and the baseline disparity in biennial lipid profiles was greatest (Table 7). In addition, IPRO initiated a similar partnership with DFTA to increase our reach to the target population in Kings County. The pilot program setting included senior centers and religious organizations. IPRO also worked with DFTA to identify senior centers in areas where the majority of beneficiaries with diabetes were African-American. The Centers for Disease Control and Prevention’s (CDC) Take Charge of Your Diabetes curriculum was selected because it is written at a reading level appropriate for our target population and is also available in Spanish.[24] This curriculum was delivered as six (6) modules (one hour each), each module addressing a particular aspect of diabetes care. An instructor’s manual for this curriculum was developed by IPRO to serve as a resource to those conducting the sessions. The nursing students and DFTA interns participating in this intervention received comprehensive culturally appropriate training on diabetes management, Medicare coverage for diabetes-related supplies and services, and effective methods for teaching the elderly. After the training, they continued to maintain regular contact with IPRO staff to provide updates on the progress of the sessions so that potential problems could be addressed in a timely manner. Participants (including seniors and others) were recruited through flyers, postings at our website, radio advertisements, and referrals by targeted providers. In addition to the CDC curriculum, participants also received CMS’ Medicare Coverage for Diabetes Supplies and Services booklet and other culturally- and linguistically-appropriate patient educational materials. From October 2003 to December 2004, we completed nearly 200 classes for seniors with class sizes ranging from 7 to 79 in the Bronx, Kings, Queens, and New York counties. To facilitate ongoing self-management support in the primary care setting, IPRO has also included the Diabetes Self-Management Goals worksheet in the toolkits for participating providers working on the project.
In Fall 2004, we expanded our effort to increase access to DSME by partnering with NYC DOHMH. Specifically, we worked with the NYC DOHMH to train health ministry directors and others in the Greater New York Seventh Day Adventist (SDA) Conference, and other religious groups to provide DSME in their community. These individuals received a condensed five-hour training session on DSME along with materials used for instruction in our DSME program in senior centers. In addition, the Joslin Diabetes Center’s curriculum, “Just a Start for Diabetes” was used to administer the actual program to the church congregation members that enable completion of the program in three hours. Finally, IPRO developed the patient education tool, “52 Ways to Prevent and Manage Diabetes,” which includes 52 tips on diabetes prevention and management that can be inserted in weekly bulletins of participating churches. Ministry leaders from 20 churches participated in the training for instructors and 90% of them implemented the program in their respective churches. This effort resulted in the participation of over 1,300 minority congregation members in the Bronx, Kings, New York, and Queens counties in DSME during the Spring of 2005.
Furthermore, in response to the overwhelming need expressed by beneficiaries, targeted providers, instructors of our DSME program and our analysis of Census-2000 data, IPRO has also developed a nutritional toolkit. This comprehensive culturally appropriate nutritional resource enables our ethnically diverse African-American population to make appropriate nutritional choices to accommodate their traditional ethnic diet. The components include a food guide pyramid specific to African-Americans, a healthy food substitution list, a guide to reading food labels and using food exchange lists, instructions for carbohydrate counting, and tips for healthy cooking as well as recipes of Southern African-American, Caribbean, continental African and other ethnic origins. At the end of the toolkit, we included references to additional resources to get more information about healthy foods, recipes, physical activity, and other materials for people with diabetes. This nutritional resource is available to beneficiaries participating in our DSME program as well as targeted physician offices.
Other educational interventions to increase awareness about diabetes care and racial/ethnic disparities in LDL testing have included mass media campaigns, pamphlets, brochures, health fairs, educational sessions, direct mailings to beneficiaries and postings on IPRO’s website. In September 2003, IPRO started a mass media campaign to increase awareness of health care disparities among African-American Medicare beneficiaries with diabetes in NYC with a press release highlighting the disparity in biennial receipt of lipid profiles between African-American and white beneficiaries. This resulted in coverage on some important NYC broadcasted outlets including WNYC-FM radio, WNBC-TV, and New York 1 News, which aired the story four times. The media campaign included IPRO’s participation in a panel discussion in the local (WABC-TV) African-American television program, “Like It Is” and a guest appearance in the local (WPHC) radio program, “My Home Town” to educate the audience on diabetes. The Summer/Fall 2003 issue of Healthy Seniors, a statewide IPRO publication (75,000 copies statewide), featured an article on how diabetes impacts the African-American community. In November 2003, as part of National Diabetes Month, a press release of a similar editorial article was distributed to various publications in the NYC area which resulted in a total of 16 stories appearing in top African-American press as well as a daily newspaper with a combined reach of over half a million readers. IPRO launched a radio advertising campaign on several NYC-based radio stations (e.g., WLIB, WBLS, and WRKS) with large African-American senior demographics urging diabetics to get some important tests (i.e., annual eye and foot exams and cholesterol tests as well as “A1C” tests twice a year) to manage their disease. These 60 seconds ads ran for three weeks from January to February 2004. An abbreviated (15 seconds) version was also broadcasted. A total of 84 ads ran with a reach of over 3 million people daily. In August 2004, a diabetes awareness advertising campaign was displayed on bus shelters throughout Kings County. IPRO also participated in the American Diabetes Association’s (ADA) Diabetes Expos in NYC and participated in the ADA’s quarterly meetings with clergy throughout NYC. Lastly, as part of National Diabetes Month (November 2004), IPRO issued a press release urging diabetics to manage their blood pressure, glucose, and lipids, and to reduce their risk for heart disease and stroke.
Intervention Implementation
IPRO used several methods to plan, track and monitor the implementation and effectiveness of activities. Work planning was performed through regular team meetings, and monthly health care quality improvement program (HCQIP) project management meetings. The Diabetes Disparities project work plan and major intervention activities were documented electronically on the “HCQIP Project Manager Switchboard.” These, as well as internal quality control (IQC) performance measures (e.g., lipid profile, HbA1C, retinal eye exam) were reviewed and discussed at least monthly. A separate electronic switchboard for the Diabetes Disparities project was launched to enhance the process in which work is performed, and to track attendance at various conferences and teleconferences. In addition, individual interactions with physician offices were tracked in IPRO’s provider contact information system. IPRO also routinely monitors the effectiveness of our activities through evaluation forms—for onsite visits, conferences, intervention toolkits, and the performance profile letters. The results of the evaluation of the conferences and onsite visits are tracked on the HCQIP Conference Evaluation module, and are reviewed monthly by the Project Director and the HCQIP Vice President. Interventions with an overall satisfaction score below 80% were determined to be in need of further evaluation to identify potential causes. All intervention activities have had positive feedback. The aggregate scores for the on-site physician office visits, the provider performance feedback mailings, and the cultural competency training pilot and teleconference were 100%, 84%, 92% and 80% favorable, respectively. In addition, evaluations from the Spring 2004 and 2005 DSME train-the-trainer session were 100% favorable. Finally, surveys completed by the church congregation members were 80% favorable.
Discussion
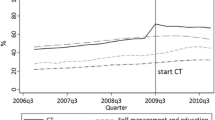
IPRO has met the project objectives. There was an absolute increase of 16.7% in the proportion of African-American beneficiaries with diabetes receiving a biennial lipid profile in the intervention areas (Table 8). The disparity between white and African-American beneficiaries also decreased. The disparity was reduced by 9.8% between African-American and all eligible white beneficiaries in the intervention areas. A greater reduction in the disparity (11.9%) was observed between African-American and non-dually enrolled white beneficiaries in the intervention areas.
Although it was not feasible to determine the direct impact of selected interventions on reducing the disparity, the interventions collectively appeared to be effective. Based on our analysis of evaluations of interventions, the intermediate objectives of most interventions were met. The aggregate scores relating to program objectives: for on-site visits, provider feedback reports, cultural competency training pilot, and DSME training for instructors were 100%, 87%, 91%, and 100% favorable, respectively.
IPRO’s prior experience in educational outreach visits and in developing materials/tools for practice improvement was instrumental in enhancing quality improvement efforts. Our provider contact information database enabled us to keep track of practice interactions via mail, telephone and in the physicians’ offices, but the need arose to standardize the data collected on the initial assessment of the practice, thus the MPA tool was developed. This comprehensive tool examines the practice’s capacity to participate and monitor various quality improvement activities as well as its’ motivational readiness for change. This tool has been piloted in practices targeted for our Diabetes Disparities project and facilitated sharing of best practices. Given the comprehensive nature of this tool, making arrangements beforehand to ensure adequate time to administer the tool is recommended rather than attempting to do so during an unscheduled visit. The provider feedback reports also appeared to be useful; more than 80% of providers who completed an evaluation indicated the report would be helpful in their quality improvement efforts.
Our DSME program in senior centers and religious organizations appeared to be effective in improving knowledge regarding effective diabetes management. Our analysis of pre- and post-tests completed by the participants of the Spring 2004 sessions found a statistically significant (p<0.05) increase (12.4%) in scores. In a survey of church congregation members participating in the Spring 2005 sessions, 91% of them reported that the program helped them to better understand how to take care of their diabetes and 69% of them stated that they are more motivated to make changes to care for their diabetes. Evaluations completed by participants of the Spring 2004 and
Spring 2005 training sessions further suggest that this intervention was effective. Feedback on the overall DSME program from our partners was also positive. It was a valuable public health teaching experience for the students and interns as well as an opportunity for them to take part in the effort to address the diabetes epidemic that is disproportionately affecting the African-American population in NYC. Support from the directors of the senior centers as well as nursing school faculty was essential for the success of this program. Furthermore, it is important to initiate early discussions with senior center staff to allow sufficient time for scheduling the sessions, as senior center calendars tend to fill quickly.
Interventions aimed at promoting cultural competency training were not as successful. Although feedback from the workshop and pilot of our cultural competency introductory training module was positive, participation by target providers in subsequent teleconferences remained suboptimal. Multiple offerings of the teleconference at various times with CME credits did not appear to increase provider participation rates. The challenges of promoting cultural competency may be due to limited resources and staff available to African-American serving providers. We found that more than 3/4 of providers targeted for more intensive interventions are in small practices with one or two providers and serve a substantial number of patients who are dual eligible for Medicare and Medicaid. Most recently a study found that physicians treating black patients may have less access to important clinical resources than physicians treating white patients.[25] These factors may have contributed to the suboptimal level of participation by providers in our recent cultural competency training intervention. IPRO has since posted a recording of one of the teleconferences on our website and distributed the CD-ROM. Alternative approaches may be more effective in emphasizing the importance of training.
References
Geiss LS, Herman WH, Smith PJ, National Diabetes Data Group. Diabetes in America. Bethesda, Md: National Institutes of Health, National Institutes of Diabetes and Digestive Kidney Diseases; 1995:233–257.
Hogan P, Dall T, Nikolov P (2003). Economic costs of diabetes in the US in 2002. Diabetes Care 26:917–932
Agency for Healthcare Research and Quality. Diabetes Disparities Among Racial and Ethnic Minorities. November 2001. AHRQ Publication No. 02-P007. Agency for Healthcare Quality and Research, Rockville, MD. http://www.ahrq.gov/research/diabdisp.htm
CDC/NCHS, National Vital Statistics System, Deaths, “Percent of Total Deaths, and Death Rates for the 15 Leading Causes of Death: United States and Each State, 1999–2001”. Available at http://www.cdc.gov/nchs/data/dvs/LCWK9_2001.pdf [accessed June 3, 2005]
Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2001. Available at http://apps.nccd.cdc.gov/brfss/display.asp?cat=DB&yr=2001&qkey=1364&state=NY [accessed June 3, 2005]
Fleming B, Greenfield S, Engelhau M, for the DQIP Group et al (2001). The Diabetes Quality Improvement Project: moving science into health policy to gain an edge on the diabetes epidemic. Diabetes Care 24:1815–1820
Beckman J, Creager M, Libby P (2002). Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA 287:2570–2581
Karter AJ, Ferrara A, Liu JY, et al (2002). Ethnic disparities in diabetes complications in an insured population. JAMA 287:2519–2527
Cook CB, Erdman DM, Ryan GJ, et al (2000). The pattern of dyslipidemia among urban African-Americans with Type 2 diabetes. Diabetes Care 23:319–24
Huang ES, Meigs JB, Singer DE (2001) The effect of interventions to prevent cardiovascular disease in patients with type 2 diabetes. Am J Med 111:633–642
CDC Diabetes Cost-effectiveness Group (2002). Cost-effectiveness of intensive glycemic control, intensified hypertension control and serum cholesterol level reduction for type 2 diabetes. JAMA 287:2542–2551
Evans J. Initiative to address cardiac risk in diabetes. Int Med News. March 15, 2002:17
Cowie CC and Harris MI (1997) Ambulatory medical care for non-Hispanic whites, African-Americans, and Mexican-Americans with NIDDM in the U.S. Diabetes Care 20:142–147
Harris MI, Eastman RC, Cowie CC, Flegal KM and Eberhardt MS (1999). Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care 22:403–408
Thorpe LE, Mostashari F, Berger DK, Cobb LK, Helgerson SD, Frieden TR (2003). Diabetes is Epidemic. NYC Vital Signs 2(1):1–4
Centers for Medicare & Medicaid Services. Outpatient Data Reports – Diabetes and Breast Cancer Screening Performance and Provider Profiles, April 1, 1999 – March 31, 2001 (unpublished).
DASPRO. Reducing Disparities in Health Outcomes: Effective and Promising Outpatient Interventions with Underserved Populations. Center for Healthcare Quality, Memphis, TN. May, 2002.
DASPRO. Cultural Competency Guide: Supporting Projects with Diverse Communities. A project development tool. Center for Healthcare Quality, Memphis, TN. July, 2002.
Beach MC, Cooper LA, Robinson KA, Price EG, Gary TL, Jenckes MW, Gozu A, Smarth C, Palacio A, Feuerstein CJ, Bass EB, Powe NR. Strategies for Improving Minority Healthcare Quality. Evidence Report/Technology Assessment No. 90. (Prepared by the John Hopkins University Evidence-based Practice Center, Baltimore, MD.) AHRQ Publication No. 04-E008-02. Rockville, MD: Agency for Healthcare Research and Quality. January 2004.
Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: applications to addictive behaviors. Am Psychol. 1992:1102–1114.
Schillinger D, Grumbach K, Piette J, et al (2002). Association of health literacy with diabetes outcomes. JAMA 288:475–482
Brach C, Fraser I (2000). Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev 57(suppl 1):181–217
Centers for Disease Control and Prevention. Strategies for reducing morbidity and mortality from diabetes through health-care system interventions and diabetes self-management education in community settings: a report on recommendations of the Task Force on Community Preventive Services. MMWR 2001;50(No. RR-16):[1–16].
Centers for Disease Control and Prevention (2002) Take Charge of Your Diabetes. 3rd edition. Atlanta, U.S. Department of Health and Human Services
Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL (2004). Primary care physicians who treat blacks and whites. N Engl J Med 351(6):575–84
Acknowledgments
The authors wish to thank Shelia McCullugh, Martha Carney, Michele Jones, Deborah Johnson-Ingram, Raymond Han, and Thomas Huang, all of IPRO, who carried out the practice interventions and computer programming support for this study. In addition, the authors thank Dr. Pascal James Imperato for his insightful comments on earlier versions of this paper. The analyses on which this publication is based were performed under Contract 500-02-NY-01 entitled “Utilization and Quality Control Peer Review Organization for the State of New York,” sponsored by the Centers for Medicare and Medicaid Services (CMS), Department of Health and Human Services. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
The authors assume full responsibility for the accuracy and completeness of the ideas presented. This article is a direct result of the Health Care Quality Improvement Program initiated by the Centers for Medicare and Medicaid Services, which has encouraged identification of quality improvement projects derived from analysis of patterns of care, and therefore requires no special funding on the part of this contractor. Ideas and contributions to the authors concerning experience in engaging with issues presented are welcomed.
Author information
Authors and Affiliations
Corresponding author
Additional information
Terry Mahotière, MD, MPH is a medical officer at IPRO; Katja Ocepek-Welikson, MPhil, is a project manager/analyst at IPRO, Maryanne B. Daley, RN, BSN, is a project manager at IPRO; Johan P. Byssainthe, MPH is a performance improvement coordinator at IPRO.
Rights and permissions
About this article
Cite this article
Mahotière, T., Ocepek-Welikson, K., Daley, M.B. et al. A Program to reduce the disparity in the rate of biennial lipid profiles between african-american and white medicare beneficiaries with diabetes mellitus in new york city. J Community Health 31, 263–288 (2006). https://doi.org/10.1007/s10900-006-9015-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-006-9015-7