Abstract
This study examined whether distinct subgroups could be identified among a sample of non-treatment-seeking problem and pathological/disordered gamblers (PG) using Blaszczynski and Nower’s (Addiction 97:487–499, 2002) pathways model (N = 150, 50% female). We examined coping motives for gambling, childhood trauma, boredom proneness, risk-taking, impulsivity, attention-deficit/hyperactivity disorder (ADHD), and antisocial personality disorder as defining variables in a hierarchical cluster analysis to identify subgroups. Subgroup differences in gambling, psychiatric, and demographic variables were also assessed to establish concurrent validity. Consistent with the pathways model, our analyses identified three gambling subgroups: (1) behaviorally conditioned (BC), (2) emotionally vulnerable (EV), and (3) antisocial-impulsivist (AI) gamblers. BC gamblers (n = 47) reported the lowest levels of lifetime depression, anxiety, gambling severity, and interest in problem gambling treatment. EV gamblers (n = 53) reported the highest levels of childhood trauma, motivation to gamble to cope with negative emotions, gambling-related suicidal ideation, and family history of gambling problems. AI gamblers (n = 50) reported the highest levels of antisocial personality disorder and ADHD symptoms, as well as higher rates of impulsivity and risk-taking than EV gamblers. The findings provide evidence for the validity of the pathways model as a framework for conceptualizing PG subtypes in a non-treatment-seeking sample, and underscore the importance of tailoring treatment approaches to meet the respective clinical needs of these subtypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There has been increasing recognition of the clinical variability among problem and disordered gamblers, as well as the need to tailor treatment approaches to address the variations in severity, course, and prognosis across different profiles of gamblers (Blaszczynski and Nower 2002; Milosevic and Ledgerwood 2010; Sharpe 2002). Over the past few decades, theoretical and empirical research on problem and pathological/disordered gambler (PG) subtypes has advanced our understanding of the heterogeneity that exists among this population, and provided frameworks for understanding possible etiologies of the disorder (for a review, see Milosevic and Ledgerwood 2010). Although several theories of PG subtypes exist, Blaszczynski and Nower’s (2002) pathways model represents the most comprehensive and widely-accepted framework to date, integrating biological, psychological, and ecological variables to describe the development of PG. Nevertheless, a relatively small number of studies have examined the validity of this model.
Pathways Model Subtypes
The pathways model proposes three subtypes (or etiological pathways) of PGs: (1) behaviorally conditioned (BC), (2) emotionally vulnerable (EV), and (3) antisocial impulsivist (AI). According to the model, all subtypes begin with availability and access to gambling (common ecological factor), and are influenced by classical and operant conditioning which serve to reinforce habitual patterns of gambling and irrational gambling-related beliefs (Blaszczynski and Nower 2002). BC gamblers are theorized to initiate gambling activities for entertainment or socialization, and develop gambling problems primarily as a result of behavioral conditioning. Symptoms of psychopathology (e.g., depression and anxiety, substance use/abuse) are thought to be a consequence rather than the cause of PG among this subgroup (Blaszczynski and Nower 2002; Milosevic and Ledgerwood 2010). Compared to BC gamblers, EV gamblers are believed to have higher levels of premorbid anxiety, depression, and substance use/abuse, and a history of negative childhood experiences. In this subgroup, the primary motivation to gamble is to experience relief from negative affective states (Anderson and Brown 1984; Blaszczynski and Nower 2002; Jacobs 1986; Lister et al. 2015a; Milosevic and Ledgerwood 2010). Lastly, AI gamblers overlap in the antecedents of gambling proposed in EV gamblers. However, they exhibit additional impairments in neuropsychological functioning, including higher rates of attention deficit and impulsivity problems, substance use/abuse, as well as symptoms of antisocial personality disorder which may result in greater gambling severity (Steel and Blaszczynski 1996; Blaszczynski et al. 1997, Blaszczynski and Nower 2002; Lister et al. 2015b).
A limited number of PG studies have employed various statistical approaches to identify subtypes of gamblers on the basis of select variables included in the pathways model, including psychopathology, impulsivity, and alcohol abuse (e.g., Gonzalez-Ibanez et al. 2003; Lesieur 2001; Suomi et al. 2014); illegal behaviors (Granero et al. 2015); gambling motivations (Stewart and Zack 2008; Stewart et al. 2008); and personality traits (e.g., Lobo et al. 2014; Vachon and Bagby 2009). These studies have enhanced our understanding of how different subtypes of gamblers may (or may not) show variations in co-occurring disorders (e.g., Suomi et al. 2014; Vachon and Bagby 2009; Valleur et al. 2016), problem gambling severity (e.g., Lobo et al. 2014; Stewart et al. 2008), and treatment outcomes (e.g., Ledgerwood and Petry 2010).
Although these studies provide evidence to support some aspects of the pathways model, few empirical studies have assessed a comprehensive set of variables differentiating the pathways model subgroups among a non-treatment seeking sample. For example, negative childhood experiences or trauma, a key characteristic of EV and AI gamblers according to the pathways model, has thus far received little attention in subtyping research, despite being identified as an important feature among PGs (Milosevic and Ledgerwood 2010). In addition, although research has demonstrated associations between PG severity and impulsivity, no empirical test of the pathways model has employed laboratory or behavioral-based measures of impulsivity, which have greater generalizability to real-world gambling conditions and may be less prone to response bias than self-report. The present study will also add to the relatively small number of studies of gambling subtyping that have focused on non-treatment seeking or community-recruited samples (others being Bonnaire et al. 2009; Stewart and Zack 2008; Stewart et al. 2008; Turner et al. 2008; Vachon and Bagby 2009), which may be characterized by lower problem severity than the more typically studied treatment-recruited population (Knezevic and Ledgerwood 2012).
In the present study we sought to provide a comprehensive empirical test of the pathways model among non-treatment seeking PGs by examining key variables theorized to differentiate the three gambling subtypes. Specifically, the present study examined pathway model variables thought to differentiate BC gamblers from EV and AI gamblers: coping motives for gambling, boredom proneness, risk-taking propensity, and childhood trauma. The current study also examined variables theorized to differentiate EV gamblers from AI gamblers: impulsivity, ADHD symptoms, and antisocial personality disorder (ASPD) symptoms. We also sought to establish the concurrent validity of these subtypes by testing whether the gambling subgroups would show differences in three categories of variables, including demographic characteristics (e.g., sex), gambling behaviors (e.g., gambling severity), and psychiatric disorders (e.g., unipolar mood disorders), consistent with the pathways model.
Methods
Participants and Procedure
Participants were 150 males (n = 75) and females (n = 75) 18 years or older who met criteria for lifetime and/or past year problem or pathological gambling (using DSM-IV criteria, as the data were collected before the release of DSM-5). Forty-two individuals who reported fewer than three past-year and/or lifetime PG symptoms on the National Opinion Research Centre DSM-IV Screen for Gambling Problems (NODS; Gerstein et al. 1999) were excluded from the study. One additional individual who was unable to understand and/or read English was also excluded.
Participants were recruited from both the community (n = 91, 60.7%) and a university (n = 59, 39.3%) in Ontario, Canada. Community participants were recruited through advertisements placed in local newspapers and online classifieds, and compensated for participation with a gift certificate ($45 CAN). University student participants were recruited through an undergraduate psychology research participant pool system, and compensated with course bonus points. None of the participants were in treatment for PG at the time of data collection. Participants completed a semi-structured diagnostic interview (SCID, First et al. 1996), a battery of self-report questionnaires, and a computer-presented impulsivity task. The typical study session lasted 1–2 h.
All participants provided written informed consent prior to study participation. The study protocol was approved by the university’s research ethics board.
Measures
Cluster Analysis Variables
Variables for cluster analysis were selected a priori on the basis of their theoretical fit with the three pathways model subtypes, and were administered within the context of a longer assessment battery. To differentiate BC from EV and AI gamblers, coping motives for gambling, childhood trauma, boredom proneness, and risk-taking propensity were assessed. Coping motives for gambling were measured using the Coping subscale of the Gambling Motives Questionnaire (GMQ; Stewart and Zack 2008), which assesses motivation to gamble to reduce or avoid negative emotions. Childhood trauma was measured using total scores on the Childhood Trauma Questionnaire (CTQ; Bernstein and Fink 1998), which assesses retrospective accounts of childhood maltreatment, including abuse (physical, emotional, and sexual) and neglect (emotional and physical). Boredom proneness was measured using scores on the (Lack of) Perseverance subscale of the UPPS Impulsive Behavior Scale (Whiteside and Lynam 2001), which measures an individual’s (in)ability to remain focused on boring, long, or difficult tasks (i.e., higher scores indicate greater boredom proneness). Risk-taking was assessed using scores on the Harm Avoidance subscale of the Multidimensional Personality Questionnaire (MPQ; Tellegan 2000), which measures an individual’s preference for safer activities over dangerous ones (i.e., lower scores indicate higher risk-taking propensity).
To differentiate EV from AI, impulsivity, ADHD symptoms, and ASPD symptoms were examined. Impulsivity was measured using the Delayed Discounting of Monetary Rewards Task (Petry and Casarella 1999), a computer-presented behavioral measure of an individual’s tendency to discount larger delayed monetary reinforcements in favor of smaller, more immediate ones. Area under the curve (AUC) was derived and analyzed as an overall measure of impulsivity (i.e., lower scores indicate greater impulsivity) consistent with past studies (Ledgerwood et al. 2009). ADHD symptoms were assessed using total DSM-IV ADHD symptom scores on the Conners’ Adult ADHD Rating Scale (CAARS; Connors et al. 1999). ASPD symptoms were assessed by using total symptom counts on the Structured Clinical Interview (SCID-P) for DSM-IV Antisocial Personality Disorder (First et al. 1996).
Demographic Characteristics
Continuous demographic variables included age, years of education, and annual income. Categorical demographic variables included sex (male/female), marital status (not married/married), employment/student status (unemployed/employed or student), and recruitment source (community/university).
Gambling Behaviors
We assessed seven gambling characteristics including lifetime and past-year gambling severity using the National Opinion Research Center DSM-IV Screen for Gambling Problems (NODS; Gerstein et al. 1999), number of past-year gambling activities, age of first gambling, age of first regular (three or more times a week) gambling, family history of gambling problems (yes/no), current interest in seeking treatment for problem gambling (yes/no), family history of alcohol and/or drug problems (yes/no), and gambling-related suicidal ideation/attempt (yes/no) using the Canadian Problem Gambling Index (CPGI; Ferris and Wynne 2001).
Psychiatric Disorder Variables
We assessed the presence of psychiatric disorders using lifetime and past-year diagnoses of unipolar mood disorders (major depression and/or dysthymia), anxiety disorders, alcohol dependence, and substance dependence (other than alcohol) using the SCID-P for DSM-IV Axis I disorders (First et al. 1996).
Data Analysis
All data were analyzed using IBM SPSS Version 22 (IBM SPSS Inc., Armonk, NY). Prior to conducting cluster analyses, bivariate correlations among variables were assessed for collinearity. All seven cluster analysis variables had correlation coefficients below .45 (Mooi and Sarstedt 2011).
As cluster analysis is an exploratory approach, analyses were conducted using different clustering procedures and algorithms to find the best fit between the data and theoretical model of interest (Mooi and Sarstedt 2011). An agglomerative hierarchical cluster analysis (HCA) using Squared Euclidian and Ward’s method as distance and linkage measures, respectively, produced the most interpretable and meaningful findings.Footnote 1 Scores of the clustering variables were standardized using z-scores to adjust for differences in scale values (Milligan and Cooper 1988; Mooi and Sarstedt 2011).Footnote 2
Examination of information provided by the agglomeration schedule, scree plot, and dendrogram indicated possible three- and four-cluster solutions (Mooi and Sarstedt 2011; Yim and Ramdeen 2015). Differences in cluster centroids (means of clustering variables) were examined and compared using one-way ANOVAs to clarify the optimal cluster solution. Discriminant function analysis (DFA) was conducted to assess the stability and validity of the cluster solution (Hair and Black 2000; Suomi et al. 2014). The seven clustering variables were included in the DFA as predictors of membership for the cluster groups identified through HCA.
To evaluate concurrent validity, analyses of variance (ANOVA) and Chi square tests were conducted to examine overall differences between clusters on several gambling-related and psychiatric variables theoretically expected to distinguish between gambling subgroups, but that were not included in the cluster analysis. Demographic differences between gambling subgroups were also assessed using ANOVA and Chi square tests. Bonferroni post hoc analyses were applied to identify specific differences between pairs of subgroups for significant ANOVA results. Square root transformations were applied to variables that were moderately skewed (i.e., number of types of gambling engaged in past year, impulsivity, boredom proneness). To determine relative cell contributions to significant omnibus Chi square results, adjusted standardized residuals (ASRs) were examined. Kruskal–Wallis omnibus and pairwise comparison tests were conducted for nonparametric continuous variables (i.e., annual income).
Results
Number and Description of Gambling Subgroups
The three-cluster solution best differentiated between subgroups of gamblers. The discriminant function analysis generated two functions that significantly differentiated between the three clusters on the clustering variables, Wilks’ λ = .174, χ2 = 272.46, p < .001. The two functions accounted for 100% of the variance, with 93.3% of the original grouped cases correctly classified.
Cluster groups were identified and labeled based on mean scores on the cluster analysis variables, as presented in Table 1. The first cluster, labeled the “Behaviorally Conditioned” (BC) gambling subgroup, represented 31.3% (n = 47) of the total sample. The second cluster, labeled “Antisocial Impulsivist” (AI) gambling subgroup, represented 33.3% (n = 50) of the total sample. The third cluster, labeled “Emotionally Vulnerable” (EV) gambling subgroup, represented 35.3% (n = 53) of the total sample.
One-way ANOVA results showed a significant main effect of gambling subgroup on GMQ-Coping subscale scores (i.e., coping to reduce negative emotional states). Bonferroni post hoc tests revealed that the EV subgroup endorsed higher GMQ-Coping scores than both BC and AI gamblers. Further, AI gamblers had significantly higher GMQ-Coping scores than BC gamblers.
The BC gambling subgroup reported significantly lower scores on the CTQ (i.e., childhood trauma) and lack of perseverance subscale of the UPPS (i.e., boredom proneness) than both the AI and EV subgroups. The EV subgroup endorsed higher scores on the MPQ-Harm Avoidance (i.e., lower risk-taking propensity) subscale than both the AI and BC subgroups.
The EV gambling subgroup had significantly higher delayed discounting AUC scores than the BC and AI subgroups (i.e., lower behavioral-based impulsivity). The AI subgroup scored significantly higher than BC and EV gamblers on total ADHD scores. AI gamblers endorsed significantly more antisocial personality disorder symptoms than both the EV and BC subgroups.
Concurrent Validity Analyses
Demographics Characteristics
Means and frequencies on demographic variables as a function of gambling subgroups are presented in Table 2. EV gamblers were significantly older than both BC and AI gamblers. A greater proportion of EV gamblers were women and a greater proportion of BC gamblers were men. EV gamblers were more represented among participants recruited from the community whereas BC gamblers were more represented among university-recruited participants. EV gamblers were also less likely to be employed, but AI gamblers reported the lowest median incomes.
Gambling Behaviors
ANOVA and Chi square tests on gambling-related variables as a function of gambling subgroups are presented in Table 2. BC gambling subgroup reported significantly lower lifetime NODS gambling severity compared to both the AI and EV subgroups. BC gamblers also had significantly lower past-year NODS gambling severity scores than EV gamblers. EV gamblers were significantly older than both BC and AI gamblers at the time of first participation and first regular (three times a week) participation in gambling. Fewer BC gamblers reported an interest in seeking problem gambling treatment compared to the total sample. Lastly, a greater proportion of EV gamblers and a lower proportion of BC gamblers reported a family history of gambling problems. A larger proportion of EV gamblers and a lower proportion of BC gamblers reported lifetime gambling-related suicidal ideation/attempt. Although there was a significant main effect for the number of types of gambling engaged in the past year, post hoc tests revealed no significant differences between pairs of subgroups.
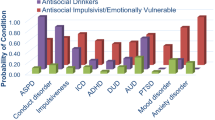
Psychiatric Disorder Variables
Results of Chi square tests on psychiatric variables as a function of gambling subgroup are presented in Table 2. A lower proportion of BC gamblers reported having experienced major depression and/or dysthymia in their lifetime compared to the EV and AI subgroups. Similarly, a lower proportion of BC gamblers reported having experienced a lifetime anxiety disorder compared to the EV and AI subgroups. Fewer BC gamblers experienced lifetime substance dependence compared to the EV and AI gamblers. A lower proportion of EV gamblers experienced lifetime alcohol dependence compared to BC and AI gamblers.
Discussion
The current study provides evidence for the validity of the pathways model as a framework to subtype problem and pathological/disordered gamblers (PGs). The current study employed a comprehensive array of pathways model variables, including measures of childhood trauma and behavioral-based impulsivity, to identify gambling subtypes among a non-treatment-seeking sample.
Implications
The findings of the present study have implications for treatment planning and intervention for PGs. Overall, the nature and length of treatment required for EV and AI gamblers are likely to be significantly more intensive compared to that required for BC gamblers, which is consistent with the findings of Ledgerwood and Petry (2010). More broadly, EV and AI gamblers require an integrated treatment approach whereby both PG and co-occurring conditions are targeted. An integrated treatment approach for these subgroups is critical given research demonstrating that factors such as depression and substance abuse frequently result in difficulties maintaining gambling abstinence among PGs (Hodgins and el-Guebaly 2010). In light of EV gamblers’ unique emotional vulnerability, the development of adaptive coping and emotion regulation skills would be an important component of treatment when working with gamblers who exhibit characteristics of this subgroup. The development of healthy coping skills may be part of a broader treatment plan that addresses the cognitive, affective, and behavioral difficulties characteristic of anxiety and depression, and may include cognitive-behavioral, humanistic, psychodynamic, or integrative psychotherapy approaches, among others.
Interestingly, a lower proportion of EV gamblers endorsed alcohol dependence compared to BC and AI gamblers. Lower proportions of alcohol dependence among EV gamblers compared to BC gamblers in our sample contrasts with the notion of EV gamblers as “escape” gamblers, as well as the results of subtyping research by Stewart et al. (2008) which found that “coping gamblers” (i.e., subgroup that gambles to cope for both positive and negative reinforcement) showed higher levels of drinking frequency, drinking problems, and coping drinking motives compared to “low emotion regulation gamblers” (i.e., subgroup that gambles for reasons other than modulating affect). Perhaps EV gamblers seek an optimal level of emotional arousal though activities that is neither overstimulating (i.e., risky activities that may give rise to new trauma) nor understimulating (i.e., boring activities that fail to provide emotional escape). This idea is consistent with the lower levels of risk-taking and impulsivity found among EV gamblers compared to BC gamblers, as well as research demonstrating that gamblers with a mood disorder showed lower levels of sensation seeking (i.e., openness to trying new experiences that may or may not be dangerous) but lower levels of perseverance (i.e., ability to remain focused on boring or difficult tasks), compared to gamblers without a mood disorder (Lister et al. 2015a). Future work on PG subtyping may include additional measures to better elucidate internal processes motivating gambling and types of coping among the EV subgroup.
Given that nearly one of three EV gamblers, and one of ten AI gamblers, endorsed suicidal ideation or attempt, regular suicide risk assessments and crisis and safety planning interventions (e.g., Jobes 2006; Joiner et al. 1999) should be critical components of treatment when working with both EV and AI gamblers. In addition, trauma-focused therapy (e.g., Seeking Safety Therapy; Najavits et al. 2013) should be incorporated within a treatment plan when working with EV and AI gamblers who confirm a history of trauma.
The high levels of ASPD and ADHD symptomology, behavioral-based impulsivity, and risk-taking propensity found among AI gamblers also warrant clinical investigation into possible neuropsychological bases for dysfunction and psychopathology. These findings are consistent with recent research demonstrating that ADHD is significantly related to problem gambling severity, motor impulsivity, and cluster B personality disorders (e.g., ASPD) among treatment-seeking problem gamblers (Waluk et al. 2016). A treatment plan for AI gamblers may begin with a comprehensive neuropsychological assessment that includes formal ADHD testing and management. In later stages of treatment, the development of self-control strategies could prove beneficial in addressing risk-taking and impulsive behaviors (Baumeister et al. 2007).
In contrast to the more severe gambler subgroups, BC gamblers may require only shorter-term interventions that focus on cognitive and behavioral strategies to directly reduce PG behaviors; that is, if treatment is sought by these gamblers at all. In our study, BC gamblers were least likely to report interest in seeking gambling treatment, which may reflect a perception that their gambling is not severe or consequential enough to warrant treatment. This finding is consistent with research demonstrating that individuals with less severe gambling behaviors stop gambling on their own (Hodgins and el-Guebaly 2000) and tend to be less likely to initiate treatment even after contacting gambling helplines (Ledgerwood et al. 2013). Further research may examine the efficacy of specific treatment approaches between and within subtypes of gamblers recruited from both treatment and non-treatment seeking samples.
Limitations and Directions for Future Research
There are limitations to the present study. Although the current study compared levels of psychopathology across the gambling subgroups identified through cluster analysis, it did not examine the onset of gambling disorder in relation to other psychopathology, which has been recommended in a review of subtyping research (Milosevic and Ledgerwood 2010). Although data on age of onset of psychiatric disorders were obtained from participants during clinical interviews, only self-reports of age of first regular gambling (versus onset of gambling disorder) was available in the current study. Given the mixed methodologies from which these data were obtained and the absence of a direct indicator of gambling disorder onset, we chose not to examine this relationship in the current study. Future research employing valid measures of premorbid levels of psychopathology would clarify the role of psychopathology as an antecedent or consequence of gambling disorder, and would provide greater evidence for the validity of the pathways model. The current study also did not assess biological vulnerabilities that may impact PG behaviors, as outlined by the pathways model. Inclusion of such variables would offer an enhanced biopsychosocial framework from which to subtype PGs (Ledgerwood and Petry 2006).
Conclusion
The current study has important theoretical and practical implications for the study and treatment of PG. It provides empirical support for the validity of the pathways model as a framework for conceptualizing PG etiology among PGs recruited from a non-treatment seeking sample, while also enhancing our understanding of the clinical profiles and unique treatment needs of behaviorally conditioned, antisocial impulsivist, and emotionally vulnerable gamblers.
Notes
Other runs using alternative clustering algorithms are available from the first author.
Raw scores are presented to facilitate comparison with other studies.
References
Anderson, G., & Brown, R. I. F. (1984). Real and laboratory gambling, sensation seeking and arousal: toward a Pavlovian component in general theories of gambling and gambling addictions. British Journal of Psychology, 75, 401–411.
Baumeister, R. F., Vohs, K. D., & Tice, D. M. (2007). The strength model of self-control. Current Directions in Psychological Science, 16, 396–403.
Bernstein, D. P., & Fink, L. (1998). Childhood trauma questionnaire: A retrospective self-report manual. San Antonio, TX: Psychological Corporation.
Blaszczynski, A., & Nower, L. (2002). A pathways model of problem and pathological gambling. Addiction, 97, 487–499.
Blaszczynski, A., Steel, Z., & McConaghy, N. (1997). Impulsivity in pathological gambling: The antisocial impulsivist. Addiction, 92, 75–87.
Bonnaire, C., Bungener, C., & Varescon, I. (2009). Subtypes of French pathological gamblers: Comparison of sensation seeking, alexithymia and depression scores. Journal of Gambling Studies, 25, 455–471.
Connors, C. K., Erhardt, D., & Sparrow, E. (1999). Conners’ adult ADHD rating scales (CAARS). North Tonawanda, NY: Multi-Health Systems.
Ferris, J., & Wynne, H. (2001). The Canadian Problem Gambling Index: Final Report. Ottawa: Canadian Center on Substance Abuse.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (1996). Structured clinical interview for DSM-IV Axis I disorders, patient edition (SCID-P). New York: New York State Psychiatric Institute.
Gerstein, D., Murphy, S., Toce, M., Hoffman, J., Palmer, A., Johnson, R., et al. (1999). Gambling impact and behavior study. Chicago: University of Chicago.
Gonzalez-Ibanez, A., Aymani, M. N., Jimenez, S., Domenech, J. M., Granero, R., & Lourido-Ferreira, M. R. (2003). Psychological Reports, 93, 707–716.
Granero, R., Fernández-Aranda, F., Aymamí, N., Gómez-Peña, M., Fagundo, A. B., Sauchelli, S., et al. (2015). Subtypes of pathological gambling with concurrent illegal behaviors. Journal of Gambling Studies, 31(4), 1161–1178.
Hair, J. F., Jr., & Black, W. C. (2000). Cluster analysis. In L. G. Grimm & P. R. Yarnold (Eds.), Reading and understanding more multivariate statistics (pp. 147–205). Washington, DC: American Psychological Association.
Hodgins, D. C., & el-Guebaly, N. (2000). Natural and treatment-assisted recovery from gambling problems: A comparison of resolved and active gamblers. Addiction, 95(5), 777–789.
Hodgins, D. C., & el-Guebaly, N. (2010). The influence of substance dependence and mood disorders on outcome from pathological gambling: Five year follow. Journal of Gambling Studies, 26(1), 117–127.
Jacobs, D. F. (1986). A general theory of addictions: a new theoretical model. Journal of Gambling Behavior, 2, 15–31.
Jobes, D. A. (2006). Managing suicidal risk: A collaborative approach. New York: The Guilford Press.
Joiner, T. E., Walker, R. L., Rudd, M. D., & Jobes, D. A. (1999). Scientizing and routinizing the assessment of suicidality in outpatient practice. Professional Psychology: Research and Practice, 30, 447–453.
Knezevic, B., & Ledgerwood, D. M. (2012). Gambling severity, impulsivity, and psychopathology: Comparison of treatment- and community-recruited pathological gamblers. American Journal on Addictions, 21(6), 508–515.
Ledgerwood, D. M., Alessi, S. M., Phoenix, N., & Petry, N. M. (2009). Behavioral assessment of impulsivity in pathological gamblers with and without substance use disorder histories versus healthy controls. Drug and Alcohol Dependence, 105, 89–96.
Ledgerwood, D. M., Arfken, C. L., Wiedemann, A., Bates, K. E., Holmes, D., & Jones, L. (2013). Who goes to treatment? Predictors of treatment initiation among gambling helpline callers. American Journal on Addictions, 22(1), 33–38.
Ledgerwood, D. M., & Petry, N. M. (2006). Psychological experience of gambling and subtypes of pathological gamblers. Psychiatry Research, 144, 17–27.
Ledgerwood, D. M., & Petry, N. M. (2010). Subtyping pathological gamblers based on impulsivity, depression and anxiety. Psychology of Addictive Behaviors, 24(4), 680–688.
Lesieur, H. R. (2001). Cluster analysis of types of inpatient pathological gamblers. Dissertation Abstracts International, 62B, 2065.
Lister, J. J., Milosevic, A., & Ledgerwood, D. M. (2015a). Psychological characteristics of problem gamblers with and without mood disorder. Canadian Journal of Psychiatry, 60(8), 369–376.
Lister, J. J., Milosevic, A., & Ledgerwood, D. M. (2015b). Personality traits of problem gamblers with and without alcohol dependence. Addictive Behaviors, 47, 48–54.
Lobo, D. S. S., Quilty, L. C., Martins, S. S., Tavares, H., Vallada, H., Kennedy, J. L., et al. (2014). Pathological gambling subtypes: a comparison of treatment-seeking and non-treatment-seeking samples from Brazil and Canada. Addictive Behaviors, 39(7), 1172–1175.
Milligan, G. W., & Cooper, M. C. (1988). A study of standardization of variables in cluster analysis. Journal of Classification, 5, 181.
Milosevic, A., & Ledgerwood, D. M. (2010). The subtyping of pathological gambling: A comprehensive review. Clinical Psychology Review, 30(8), 988–998.
Mooi, E., & Sarstedt, M. (2011). Understanding cluster-analysis. In E. Mooi & M. Sarstedt (Eds.), A concise guide to market research: The process, data, and methods using IBM SPSS statistics (pp. 259–283). Berlin: Springer.
Najavits, L. M., Smylie, D., Johnson, K., Lung, J., & Classen, C. (2013). Seeking safety therapy for pathological gambling and PTSD: A pilot outcome study. Journal of Psychoactive Drugs, 45, 10–16.
Petry, N. M., & Casarella, T. (1999). Excessive discounting of delayed rewards in substance abusers with gambling problems. Drug and Alcohol Dependence, 56(1), 25–32.
Sharpe, L. (2002). A reformulated cognitive–behavioral model of problem gambling: a biopsychosocial perspective. Clinical Psychology Review, 22, 1–25.
Steel, Z., & Blaszczynski, A. (1996). The factorial structure of pathological gambling. Journal of Gambling Studies, 12, 3–20.
Stewart, S. H., & Zack, M. (2008). Development and psychometric evaluation of a three dimensional Gambling Motives Questionnaire. Addiction, 103, 1110–1117.
Stewart, S. H., Zack, M., Collins, P., Klein, R. M., & Fragopoulos, F. (2008). Subtyping pathological gamblers on the basis of affective motivations for gambling: Relations to gambling problems, drinking problems, and affective motivations for drinking. Psychology of Addictive Behaviors, 22, 257–268.
Suomi, A., Dowling, N. A., & Jackson, A. C. (2014). Problem gambling subtypes based on psychological distress, alcohol abuse and impulsivity. Addictive Behaviors, 39(12), 1741–1745.
Tellegan, A. (2000). Manual for the multidimensional personality questionnaire. Minneapolis: University of Minnesota Press.
Turner, N. E., Jain, U., Spence, W., & Zangeneh, M. (2008). Pathways to pathological gambling: Component analysis of variables related to pathological gambling. International Gambling Studies, 8, 281–298.
Vachon, D. D., & Bagby, R. M. (2009). Pathological gambling subtypes. Psychological Assessment, 21, 608–615.
Valleur, M., Codina, I., Vénisse, J. L., Romo, L., Magalon, D., Fatséas, M., et al. (2016). Towards a validation of the three pathways model of pathological gambling. Journal of Gambling Studies, 32(2), 751–771.
Waluk, O. R., Youssef, G. J., & Dowling, N. A. (2016). The relationship between problem gambling and attention deficit hyperactivity disorder. Journal of Gambling Studies, 32(2), 591–604.
Whiteside, S. P., & Lynam, D. R. (2001). The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30(4), 669–689.
Yim, O., & Ramdeen, K. T. (2015). Hierarchical cluster analysis: Comparison of three linkage measures and application to psychological data. The Quantitative Methods for Psychology, 11(1), 8–21.
Acknowledgements
This research was supported by the Ontario Problem Gambling Research Centre, the Joe Young Sr–Helene Lycaki Funds from the State of Michigan, and the Detroit Wayne Mental Health Authority. Aleks Milosevic collected the data during his doctoral studies at the University of Windsor Department of Psychology. We thank Ron Frisch for his assistance with this study. All authors contributed to writing and data analysis processes during the preparation of this manuscript. All authors have read and approved of this manuscript. There are no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Moon, M., Lister, J.J., Milosevic, A. et al. Subtyping Non-treatment-seeking Problem Gamblers Using the Pathways Model. J Gambl Stud 33, 841–853 (2017). https://doi.org/10.1007/s10899-016-9658-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10899-016-9658-y