Abstract
According to public health research, exposure to casinos is a risk factor for disordered gambling. Consequently, casino self-exclusion programs, which provide gamblers with the opportunity to voluntarily seek limits on their access to gambling venues, can serve as a barometer of the concentration of disordered gambling in an area. This study reports on the distribution, both temporally and geographically, of 6,599 people who applied to exclude themselves from Missouri casinos between November, 1996 and February, 2004. Analyses used Microsoft MapPoint to plot the location of casinos and self-excluders (SEs) across Missouri and its constituent counties. These regional exposure analyses showed that the Western region around Kansas City is an epicenter of disordered gambling as, to a lesser extent, is the Eastern region around St. Louis. The annual number of SE enrollments increased during the first few years of the Missouri self-exclusion program and then leveled off during the later years. These findings have important implications for public health and the development of public health interventions for disordered gamblers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Responsible gambling programs, like casino self-exclusion, are in demand. In short, casino self-exclusion programs are intended to provide individuals with the opportunity to limit their access to gambling venues. Using these programs, individuals voluntarily confirm that they are disordered gamblers, add themselves to a list of “Disassociated Persons” and make a pledge to stay out of gambling venues in a defined area for a specific time period, often for the rest of their lives. Such systems require casinos to remove the self-excluders (SEs) from mailing lists and implement procedures to identify violators and charge them with criminal trespass. Their arrests become a matter of public record, a further deterrent for the SEs to engage in gambling activities.
The first self-exclusion programs worldwide were initiated in the Netherlands and Canada (Nowatzki & Williams, 2002). Currently, all of Canada’s provinces except Quebec have province-wide self-exclusion programs, most of Australia’s states and territories have universal programs, and there are nation-wide programs in other countries, including the Netherlands, France, Poland, Sweden, Switzerland, and South Africa. Some multi-national casino companies make a form of self-exclusion available in all their venues (Nowatzki & Williams, 2002; O’Neil et al., 2003). Missouri implemented the first state-wide program in the United States. Policy makers and gambling industry executives continue to implement and expand SE programs in the United States and throughout the world (Blaszczynski, Ladouceur, & Shaffer, 2004; Nowatzki & Williams, 2002). The current American Gaming Association (AGA) code of conduct assures that patrons can elect to self-exclude themselves from AGA member venues: “Each AGA casino company shall make reasonable efforts to honor a written request from any person that it not knowingly grant that person access to gambling activities at one or more of its facilities” (American Gaming Association, 2005). The rapid, wide-spread acceptance and implementation of self-exclusion programs has occurred despite a paucity of empirical research.
To date, no research has examined how exposure to gambling and regional vulnerability to addictive behavior impacts participation in self-exclusion programs; however, public health research suggests that these factors might be important to consider. For example, some investigators consider regional proximity to casinos as a risk factor for disordered gambling (Volberg, 2000; Welte, Wieczorek, Barnes, Tidwell, & Hoffman, 2004), and exposure to gambling results in a distinct temporal pattern of disordered gambling prevalence: rates increase during initial exposure to new gambling opportunities and then level off once adaptation occurs (Shaffer & Hall, 2001; Shaffer & Korn, 2002; Shaffer, LaBrie, & LaPlante, 2004; Shaffer, LaBrie, Caro, LaPlante, & Nelson, 2004). At the individual level, exposure adversely impacts only those who have an underlying vulnerability but not those who are sufficiently resilient (e.g., Jacobs, 1987; Khantzian, 1975, 1985, 1997). At an aggregate level, in this case regional, the impact of exposure to an object of addiction will depend to some extent on the underlying vulnerability to addiction in a region. Consequently, the effect of exposure should be examined after adjusting for vulnerability.
This paper presents data from the Missouri self-exclusion program describing the demographic characteristics of SEs and the distribution of SEs across time and geographic area. We hypothesize that, because SE rates are associated with rates of gambling disorder, SE rates will be higher in areas with proximal access to casinos. We also hypothesize that exposure to new gambling opportunities will result in an initial period of increased SE rates followed by a leveling off of rates during later years. Finally, we hypothesize that regional exposure will have an effect on SE rates after controlling for the regional vulnerability to addiction in general. This study represents an important step toward elucidating the geographic and temporal distribution and determinants of gambling problems at a population level and informing the design of public health interventions.
Methods
Participants
The Missouri Gaming Commission (MGC) provided a censored roster of people who applied to exclude themselves from Missouri casinos from the beginning of the Missouri Voluntary Exclusion Program in November, 1996 to the time of our request, February, 2004. The MGC censored the roster’s demographic information to preclude possible individual identification of SEs. The remaining demographic information about SEs consisted of gender, date of birth, race/ethnicity and residence by city and state. The data also included procedural information about the date of application and application status. The Harvard Medical School Committee on Human Studies approved our request for exemption from review under the Code of Federal Regulations, Title 45, Part 46, Subpart A, Item 101 (b) (4). We eliminated four people from the dataset who terminated their applications before they became effective and seven records identified as invalid applications. The final study roster of valid SEs included 6,599 persons.
Procedures and Measures
The geopolitical areas of interest in Missouri are the 114 counties and the City of St. Louis (hereafter referred to as “counties”) and the six State of Missouri public health planning regions, the areal level of aggregation usually used for public health planning. The information on each SE included the reported city or town name and a postal (ZIP) code. We assigned each SE to the county provided by Microsoft’s Excel ZIP code to county conversion program. Because ZIP code territories do not always match county boundaries—and because of data entry errors—we examined the cities and towns included in each ZIP-code defined county to assure that they matched the official Missouri identification of cities and towns within counties. Non-matching assignments were corrected to Missouri’s county assignment of the city or town. We used the US National Census population estimates of the number of adults (i.e., aged 21 years and older) to generate population-adjusted rates of SEs for Missouri and its constituent counties (United States Census Bureau, 2000), and to compare SEs to the general Missouri population.
We mapped the counties and the coordinates for casino properties in and around Missouri using Microsoft MapPoint. The addresses for the properties were taken from the Gaming Business Online Directory (gbdonline.com), and later re-verified with the casino web sites for each property. There were eleven casinos within Missouri and 91 casinos and racinos (i.e., race tracks with slot machines) within the eight states that abut Missouri. However, for display we present only the 29 non-Missouri casinos that are close to Missouri borders (i.e., included in Fig. 2, an 8 × 10 map centered on Missouri).
We used two exposure measures in our analyses: (1) dose—the distance of the geographic center of each SE'S county of residence to the nearest casino, and (2) potency—the number of casinos clustered with the closest casino.
Measures of regional vulnerability to addiction are scant and numerous ways of estimating a region’s vulnerability are possible. Although a full examination of the myriad vulnerability factors (e.g., population density, socioeconomic characteristics, need for treatment) is beyond the scope of this paper, the ready availability of information related to regional variations in alcohol use and abuse allows for a preliminary examination of vulnerability. In support of this approach, we considered that elevation of the prevalence in an area of one addiction problem is often associated with elevation in other addiction problems (Shaffer, LaBrie, Caro et al., 2004; Shaffer, LaBrie, & LaPlante, 2004). Consequently, regional variability in need for treatment of one type of addictive disorder tends to correlate with need for treatment of any addictive disorder. Since alcohol disorders are perhaps the best-studied form of addictive behavior, and because estimates of regional alcohol use disorders are readily available, in this paper, we use need for treatment of alcohol use disorders for our preliminary estimates of regional vulnerability to addictive disorders.
Specifically, we used Missouri’s county-level estimates of need for alcohol treatment developed through a social indicator modeling procedure by the Center for Substance Abuse Treatment Needs Assessment, of which the senior authors of this report were a part. We have argued that social indicator models should be based on theoretically direct measures that have empirical evidence of reliability and validity (McAuliffe, LaBrie, Lomuto, Betjemann, & Fournier, 1999; McAuliffe et al., 2000; McAuliffe, LaBrie, Woodworth, Zhang, & Dunn, 2003). The alcohol treatment need index developed by applying the suggested model in Missouri included county-level information from 1993 to 1996 on measures with explicit-mention of alcohol, alcohol-related arrests, mortalities, auto accidents, and live births with excessive maternal alcohol use (Zand, Cho, Malmstrom, & Ho, 1998). This methodology produced an Alcohol-Related Relative Needs Assessment Scale (ARNAS) measuring the proportion of people at risk for alcohol-related problems. Each geographic unit (i.e., 114 counties and the city of St. Louis) received a single score on the scale representing its need for alcohol treatment relative to other geographic units. To increase reliability, we merged counties with small populations with other small contiguous counties to compute the ARNAS. We assigned the ARNAS score for the combined counties to each of the counties in the set. We used this measure of regional vulnerability to analyze the relationship between measures of exposure and prevalence of SEs after adjustment for underlying vulnerability.
Analytic Strategy
First, we compared the demographics of Missouri SEs to SEs from other states who enrolled in the Missouri program and to the Missouri population using χ2 analyses and t-tests. Next, to measure the relationship between SE rates and time we used correlation procedures and to measure the effect of location we compared the distribution of SE rates across public health management regions. The introduction of new casinos during the period of this study allowed an examination of the immediate influence of new gambling opportunities on disordered gambling, using χ2 analyses. We conducted multivariate regression analysis to determine how county differences in SE enrollment could be explained uniquely by exposure variables and underlying vulnerability.
Results
Characteristics of Self-excluders
Differences between Resident and Non-resident Self-Excluders
The roster of SEs included residents from states other than Missouri. There were 1,262 SEs (19%) from 18 other states and Canada. Missouri is unique because it borders a large number (eight) of other states. However, only two states, Illinois and Kansas, border Missouri where its riverboat casinos are clustered (i.e., St. Louis and Kansas City). Residents of those states comprise 96% of the non-Missouri SEs; 77% from Kansas and 19% from Illinois. There were 21 SEs from the other contiguous states, 27 from 10 non-contiguous states, and 1 SE from Canada. Table 1 presents the demographic characteristics of adult Missourians according to the 2000 National Census projections, the demographics of SEs from Missouri and the demographics for SEs from outside Missouri. A comparison of the Missouri SEs to those not from Missouri found no significant difference in age or month of enrollment between Missouri resident and non-resident SEs. However, non-Missouri SEs were significantly more likely to be males (χ2 = 14.83, df = 1, p < 0.01). In addition, the distribution of SEs by race was significantly different: Missouri SEs comprised more African-Americans and fewer Asian-Americans than non-Missouri SEs (χ2 = 67.31, df = 7, p < 0.001).
Differences Between the General Population and Self-Excluders
Missouri census data presents a background for considering the characteristics of the SEs. Compared to the state population of adults, Missouri SEs were younger; 83% of the SEs were between 24 and 54 years of age but only 57% of the general population of adults are in that age range. After adjusting for non-disclosure of race (i.e., 6% of SEs chose not to report race and we calculated the race distribution without these SEs), the proportion of minorities was greater among SEs (26%) than the general adult population (13%) and SEs were slightly more likely to be male (52% vs. 49%) (see Table 1).
Distributions of Self-excluders Across Time and Space
Differences in Self-Exclusion Rates across Time
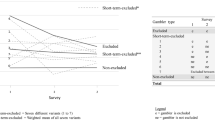
The first calendar year of Missouri’s Voluntary Exclusion Program, 1996, and the most recent year in our information base, 2004, both include only 2 months of enrollment. Therefore, the analyses that follow include only Missouri-resident SE enrollments from the complete calendar years of 1997 through 2003 (n = 5,125). Figure 1 presents the number of Missouri-resident SEs newly enrolled into the self-exclusion program for each of the full calendar years from 1997 to 2003. The annual number of enrolled SEs increased steadily during the first five years of the program. There was nearly a doubling of enrollments from 1999 to 2000. The annual enrollment leveled off during the last 3 years. The correlation between year and SE enrollment was .93 (p < .01) across the seven years, but the correlation increased to .98 (p < .05) when only the first five years were considered and changed to −.56 (p = n.s.) when only the last three years were considered. Non-Missourians enrolled during the years 1997 through 2003 (N = 1,219) showed a similar pattern in enrollment in the earlier years, except there was a steady enrollment increase rather than the leveling off seen among Missourians in recent years (data not shown).
Differences in Self-Exclusion Rates across Areas
To facilitate presentation of areal differences, we calculated the rate of SEs per 100,000 adults for the 82 Missouri counties with SEs; 33 counties had no SEs from 1997 to 2003. We ordered the 82 counties by self-exclusion rate and shaded the SE rates into six groups roughly equal in the number of counties they encompassed (range = 13–15 counties). Results are presented using 7-year aggregate SE rates. Figure 2 is a map of Missouri counties showing the shaded population-adjusted rates of SEs. The 33 counties with no SEs are shown without shading, counties with relatively low rates of SEs are increasingly darker areas represent increasingly higher rates of SEs. The map also shows as light dots the location of casinos in Missouri, and casinos, racinos, and racetracks near the border in neighboring states.
Figure 2 reveals a noticeable geographic clustering of counties with similar levels of SEs as well as a visible relationship between the location of gambling venues and higher SE rates. The counties with the highest rates of SE were Clay, St. Charles, Platte, and Jackson. St. Charles County is in the St. Louis epicenter of gambling venues and the other three counties are in the Kansas City epicenter.
Aggregation at the level of planning region showed the same pattern. The bar graph of SE rates aggregated by health planning region presented in Fig. 3 shows considerable variation in SE rates. The Western region, comprised of the counties around Kansas City, had the highest level of SEs. The Eastern region, comprised of the counties clustering around St. Louis, had the second highest rate of SEs, which is approximately 60% that of the Western region. The Northern and Central regions had rates that were only a third of the Eastern region rate, and the regions in the southern part of the state had the lowest rates. The rate in the Southeast was only a hundredth of the state’s highest rate.
In addition to having the highest rates of SEs, the Eastern and Western regions also are the most populous regions in Missouri. The net effect of the interaction between the SE rate and the population distribution resulted in a concentration of SEs in those regions. Of all the SEs enrolled during the 7 years of program operation, 92% were from the Western or Eastern regions.
Recent Health Region Trends in SE Enrollment
During 2001, two casinos opened in regions that had no previous legal gambling venues. In July of 2001, a casino opened in the Northern Health Planning Region, and in December a casino opened in the Central region. This alteration of the casino environment provided an opportunity to examine the ability of a direct indicator of gambling-related problems (i.e., SE rate) to detect expected changes in problem prevalence. Using the total enrollments from the SE program’s inception in 1996 to 2003, we calculated the percent of enrollments in each Health Planning Region that occurred during 2002 and 2003, the years immediately after the opening of the new casinos. χ2 analyses revealed that, as shown in Fig. 4, the Eastern and Western regions enrolled most of their SEs during the early years of the self-exclusion program, but the Northern and Central regions enrolled the majority of SEs more recently, after casinos opened in those regions (χ2 = 69.64, df = 5, p < .001). The Southwestern region persists as the region with the second lowest rate of SEs and has the lowest growth rate for SEs during recent years. This region is now the only region without a casino. However, there are neighboring casinos in Oklahoma (see Fig. 2).
Integrating Exposure and Vulnerability
We used multivariate regression to test the effect of regional exposure and vulnerability on SE rates. The rate of SEs was significantly correlated with the measure of regional vulnerability to addiction, the ARNAS (r = .46, p < .01.), with exposure dose (distance of SE from the nearest casino) (r = .54, p < .01), and with exposure potency (the number of casinos clustered with the closest casino) (r = .46, p < .01). The expectation that exposure would contribute to SE estimation independent of vulnerability was strengthened by the lack of significant correlations between the ARNAS and both exposure dose and potency. The correlation was .12 for both exposure measures.
A multivariate model estimating prevalence of SE from the vulnerability, dose, and potency measures indicated that vulnerability was a good predictor of SE rates (R 2 = .21, p < .001). Adding dose and potency added considerably to estimation (R 2 = .51, p < .001). An examination of the components of variance indicated that all effects made significant unique contributions to estimation. Vulnerability uniquely explained 27% of the total explained variance (p < .001), dose explained 39% (p < .001) and potency explained 12% (p < .05). The interaction of dose and potency explained 10% (p < .05) but none of the other interactions, which in total explained the remaining 12%, was significant.
Discussion
By describing not only the characteristics of SEs, but also the enrollment distribution of SEs across time and space, this study makes an important contribution to the sparse body of research focusing on self-exclusion. The results reported above suggest a relationship between gambling proximity, gambling availability, and SE rates. This relationship persisted after taking into account the underlying regional vulnerability to disordered behaviors. This finding can inform the allocation of public health resources (e.g., which areas need more public health resources for SEs) and the creation of new interventions for disordered gambling in Missouri and beyond.
Given the high rate of disordered gambling among SEs (Ladouceur, Jacques, Giroux, Ferland, & Leblond, 2000), it follows that SEs might serve as a useful barometer for the temporal and geographic distribution of disordered gambling (Shaffer, LaBrie, Caro et al., 2004; Shaffer, LaBrie, & LaPlante, 2004). Analyses of the enrollment characteristics of Missouri SE for the years 1997 through 2003 revealed characteristics similar to the characteristics of both non-Missouri SEs and the general population. However, Missouri SEs were younger, slightly more likely to be male and more likely to be non-Caucasian than the general population (see Table 1). These differences reflect differences often found between disordered gamblers and the general population (e.g., Petry, Stinson, & Grant, 2005), supporting the argument that SEs might be good indicators of disordered gambling in a region.
The aggregation of the cumulative Missouri SEs over county and the 7 years of the self-exclusion program experience demonstrates quite clearly that the Western region around Kansas City is an epicenter of disordered gambling as, to a lesser extent, is the Eastern region around St. Louis. Four counties have extremely high rates: Clay, Platte and Jackson in the Western region and St. Charles in the Eastern region. The remaining counties show a more gradual decline in the population adjusted rates of SEs. The Western and Eastern regions also are the most populous regions; the combined high rate of SEs and the high population density results in these two regions being the residence of 92% of the Missouri SEs. The Southeast region has a low rate of SEs despite the presence of a casino in that region (see Fig. 2). Interestingly, the fiscal year 2003 report of the MGC indicated that the casino in that region, “posted weak results for the fiscal year as the regional Carruthersville economy continues to struggle” (Mullaly, 2003). This observation is consistent with the low SE rate but inconsistent with the proposition that proximal access to casinos is necessarily a risk factor for disordered gambling (see discussion below).
SE enrollment patterns were consistent with prototypical exposure patterns of other disorders (i.e., steep initial increase followed by a gradual leveling). The annual number of SEs enrolled in each of the seven years of study (see Fig. 3) followed a pattern of steady increases in the first few years followed by a leveling off in the later years. If we consider that self-exclusion might be an accurate social indicator of disordered gambling, this pattern might represent a typical course for illness (Shaffer, LaBrie, Caro et al., 2004; Shaffer, LaBrie, & LaPlante, 2004). The course of epidemic infections provides an analogous situation: the early stages of infection have higher incidence rates because of the rapid infection of those people most vulnerable to infection. The rate slows as the people not yet infected represent a more resistant segment of the population. The infection course paradigm applied to disordered gambling suggests that the novelty of new gambling opportunities exploits some population vulnerability; for example, the early gambling behaviour is not accompanied by adequate coping strategies or informal social controls that will limit gambling. Gradually, people adapt to a no longer novel experience and develop personal and social strategies to prevent excessive and disordered behaviour. SE enrollment follows this pattern. One caveat to this reasoning is necessary. We should note that, for gambling disorders in Missouri, the experience during the early years includes the added effect of increasing exposure to and awareness of the Voluntary Exclusion Program.
The analysis of the proportion of total SEs added in later years (see Fig. 4) shows that in the regions where casinos were present in all years there were fewer enrollments in the later years. This pattern is consistent with the major effect of adaptation on gambling-related behaviour discussed above (Shaffer, LaBrie, Caro et al., 2004; Shaffer, LaBrie, & LaPlante, 2004). The results also indicate an increase in the rate of enrollment within the regions where casinos were introduced during the later years, which is consistent with the effect of novelty on gambling behavior. The low rate of SEs and low growth rate for SEs during recent years in the Southwestern region, the only region without a casino, could be due to close proximity to neighboring casinos in Oklahoma (see Fig. 2). It is possible that problem gamblers in this region access Oklahoma casinos and might enroll in Oklahoma self-exclusion programs rather than the Missouri program. This would suggest that the SE rates observed in this study are conservative because the rates do not include Missouri residents who exclude from entry into casinos outside of Missouri.
Our analysis of the role of underlying vulnerability within regions indicates that general vulnerability to addiction as measured by untoward events subsequent to alcohol abuse is a significant influence on the prevalence of disordered gambling. However, vulnerability was not related to dose or potency of exposure. Approximately a quarter (27%) of the explained variance in SE rates was due to differences among areas in underlying vulnerability. The interactions between vulnerability and the exposure measures accounted for another 10% of the explained variance. The remaining, roughly two-thirds, of the explained variance was due to dose (39%), potency (12%), and the interaction of dose and potency (10%). In Missouri, distance to the nearest casino (dose) is a much stronger predictor than the number of casinos available at that distance (potency). This may be an artifact of the distribution of casinos into two major clusters with large populations and several areas with less population density served by a single casino.
Despite the utility of these findings for examining characteristics and distribution of SEs in Missouri, the study has some potential limitations. One limitation is the gambling venues’ lack of enforcement of self-exclusion. The South Australian Center for Economic Studies (2003) examined the self-perceived ability of gambling venues in Victoria, Australia to enforce self-exclusion. Of the 93 responding gambling venues, 71% reported it was “difficult” or “very difficult” to identify a SE. The findings from this study suggest a need to improve methods for gambling venues to enforce self-exclusion programs. In addition, findings from the present study of Missouri SEs might have limited generalizability to the study of SEs in other geographic areas. Furthermore, studies of SEs only present findings for a fraction of problem gamblers in the general population. For example, the number of SE contracts corresponded to between 0.4% and 1.5% of the number of disordered gamblers in Canada (Nowatzki & Williams, 2002). However, SE data are more readily accessible measures of disordered gambling prevalence than other more costly and time-consuming measures such as household surveys. As the correspondence between SEs and disordered gamblers becomes better defined, SE data might be a very valuable research tool. One additional limitation is that our estimate of vulnerability is restricted to the need for treatment for alcohol disorders. However, the vulnerability indicator was robust despite aging and despite the focus on alcohol-related parameters. The use of direct indicators specific to vulnerability to gambling problems such as treatment admissions and gambling-related crimes and inclusion of indirect indicators of general vulnerability to addiction, such as population density, the prevalence of psychiatric disorders, socioeconomic variability, and quality of education, could improve and might even change the reported results.
Clearly, an updated treatment need index as a measure of vulnerability would improve the precision of the relationships among measures. Nonetheless, the inclusion of a vulnerability component is important to an understanding of the independent effects of exposure. This study, takes a preliminary step in highlighting that importance by demonstrating that a measure of vulnerability, independent of gambling exposure, relates to the prevalence of gambling-related disorders. This provides important evidence for the confluence of antecedent events that are associated with the emergence of complex syndromes in general and addictive behavior patterns in particular. Further, demonstrating that exposure is related to variability in the underlying rate of problem gamblers beyond that attributable to underlying vulnerability provides important evidence for the independent role of exposure as a risk factor for problem gambling.
Further research is needed to elucidate the distribution and determinants of problem gambling at the population level and inform the design of evidenced-based public health interventions. One way to address this objective is to conduct research using the social indicator strategy. McRae, Beebe, and Harrison (2001) describe the social indicator approach as “... using data collected by various governmental agencies for diverse purposes to estimate indirectly the prevalence of substance abuse. The variables employed might be demographic factors (e.g., sex and age distributions), indicators of social disorganisation (e.g., poverty and school dropout rates), or more direct indicators of substance use (e.g., drug and DWI arrest rates)” (McRae et al., 2001). The social indicator approach considers gambling-related health problems from a public health perspective by examining these harms through a population-based lens (Korn, 2000; Korn & Shaffer, 1999; Korn & Skinner, 2000; Shaffer & Korn, 2002; Shaffer, LaBrie, LaPlante, & Kidman, 2002; Skinner, 1999). A robust finding of how SE data relates to disordered gambling could bolster arguments that SE data might serve as a direct social indicator of the prevalence and relative distribution of general population gambling disorders.
References
American Gaming Association (2005). Responsible gaming rules of conduct. Retrieved June 9, 2005, from http://www.americangaming.org/programs/responsiblegaming/code_public.cfm.
Blaszczynski, A., Ladouceur, R., & Shaffer, H. J. (2004). A science-based framework for responsible gambling: The Reno model. Journal of Gambling Studies, 20(3), 301–317.
Jacobs, D. F. (1987). A general theory of addictions: Application to treatment and rehabilitation planning for pathological gamblers. In T. Galski (Ed.), The handbook of pathological gambling (pp. 169–194). Springfield, Illinois: Charles C. Thomas.
Khantzian, E. J. (1975). Self selection and progression in drug dependence. Psychiatry Digest, 36, 19–22.
Khantzian, E. J. (1985). Psychotherapeutic interventions with substance abusers: The clinical context. Journal of Substance Abuse Treatment, 2, 83–88.
Khantzian, E. J. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231–244.
Korn, D. A. (2000). Expansion of gambling in Canada: Implications for health and social policy. Canadian Medical Association Journal, 163(1), 61–64.
Korn, D. A., & Shaffer, H. J. (1999). Gambling and the health of the public: Adopting a public health perspective. Journal of Gambling Studies, 15(4), 289–365.
Korn, D. A., & Skinner, H. A. (2000, Autumn 2000). Gambling expansion in Canada: An emerging public health issue. CPHA Health Digest, XXIV, 10.
Ladouceur, R., Jacques, C., Giroux, I., Ferland, F., & Leblond, J. (2000). Analysis of a casino’s self-exclusion program. Journal of Gambling Studies, 16(4), 453–460.
McAuliffe, W. E., LaBrie, R. A., Lomuto, N., Betjemann, R., & Fournier, E. A. (1999). Measuring interstate variations in drug problems. Drug & Alcohol Dependence, 53(2), 125–145.
McAuliffe, W. E., LaBrie, R. A., Lomuto, N., Pollock, N., Betjemann, R., & Fournier, E. A. (2000). Measuring interstate variations in problems related to alcohol use disorders. In R. Wilson & M. Dufour (Eds.), The epidemiology of alcohol problems in small geographic areas. National Institute on Alcohol Abuse and Alcoholism.
McAuliffe, W. E., LaBrie, R. A., Woodworth, R., Zhang, C., & Dunn, R. P. (2003). State substance abuse treatment gaps. American Journal on Addictions, 12(2), 101–121.
McRae, J. A. Jr., Beebe, T. J., & Harrison, P. A. (2001). Estimating the prevalence of substance abuse with social indicators. Journal of Drug Issues, 31(4), 977–988.
Mullaly K. (2003). Missouri gaming commission fund balance report—Fiscal Year 2003. Kansas City, Missouri: Missouri Gaming Commission.
Nowatzki, N. R., & Williams, R. J. (2002). Casino self-exclusion programmes: A review of the issues. Inernational Gambling Studies, 2, 3–26.
O’Neil, M., Whetton, S., Dolman, B., Herbert, M., Giannopoulos, V., O’Neil, D., et al. (2003). Gambling research panel report no. 2: Evaluation of self-exclusion programs (report). South Australian Centre for Economic Studies.
Petry, N. M., Stinson, F. S., & Grant, B. F. (2005). Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry, 66(5), 564–574.
Shaffer, H. J., & Hall, M. N. (2001). Updating and refining prevalence estimates of disordered gambling behaviour in the United States and Canada. Canadian Journal of Public Health, 92(3), 168–172.
Shaffer, H. J., & Korn, D. A. (2002). Gambling and related mental disorders: A public health analysis. Annual Review of Public Health, 23, 171–212.
Shaffer, H. J., LaBrie, R. A., & LaPlante, D. A. (2004). Laying the foundation for quantifying regional exposure to social phenomena: Considering the case of legalized gambling as a public health toxin. Psychology of Addictive Behaviors, 18(1), 40–48.
Shaffer H. J., LaBrie R. A., LaPlante D. A., & Kidman R. C. (2002). The Iowa Department of public health gambling treatment services: Four years of evidence (No. 101102–200). Boston: Division on Addiction, Harvard Medical School.
Shaffer, H. J., LaBrie, R. A., Caro, G., LaPlante, D. A., & Nelson, S. E. (2004). Disordered gambling in Missouri: Regional differences in the need for treatment. Division on Addictions, Harvard Medical School.
Skinner, H. A. (1999). Gambling: Achieving the right balance. Journal of Gambling Studies, 15(4), 285–287.
South Australian Centre for Economic Studies (2003). Evaluation of self-exclusion programs (Part A: Evaluation of self-exclusion programs in Victoria) (No. 2). Victoria, Australia: The Victorian Gambling Research Panel.
United States Census Bureau (2000). United States Census 2000. Retrieved June, 2004, from http://www.census.gov/main/www/cen2000.html.
Volberg, R. A. (2000). The future of gambling in the United Kingdom: Increasing access creates more problem gamblers. British Medical Journal, 320(7249), 1556.
Welte, J. W., Wieczorek, W., Barnes, G., Tidwell, M.-C., & Hoffman, J. (2004). The relationship of ecological and geographic factors to gambling behavior and pathology. Journal of Gambling Studies, 20(4), 405–423.
Zand, D., Cho, D., Malmstrom, T., & Ho, L. (1998). Estimating substance abuse treatment needs using social indicators, 1993–1996 (Final Report). The Missouri Institute of Mental Health, Social Indicators Project Work Group.
Acknowledgments
The authors thank the Missouri Gaming Commission’s Voluntary Exclusion Program for providing the information for this study, Bryan Nehl at the Missouri Gaming Commission for his help in facilitating the data transfer, Eric Fleegler for his assistance with the geocoding of gambling venues, and Christine Reilly and Christine Thurmond for their effective management of the project. This project was supported, in part, by grants from the Kansas City Community Foundation’s Port Authority Problem Gambling Fund, and the National Center for Responsible Gaming.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
LaBrie, R.A., Nelson, S.E., LaPlante, D.A. et al. Missouri Casino Self-Excluders: Distributions Across Time and Space. J Gambl Stud 23, 231–243 (2007). https://doi.org/10.1007/s10899-006-9037-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10899-006-9037-1