Abstract
Telegenetics—genetic counseling via live videoconferencing—can improve access to cancer genetic counseling (CGC) in underserved areas, but studies on cancer telegenetics have not applied randomized methodology or assessed cost. We report cost, patient satisfaction and CGC attendance from a randomized trial comparing telegenetics with in-person CGC among individuals referred to CGC in four rural oncology clinics. Participants (n = 162) were randomized to receive CGC at their local oncology clinic in-person or via telegenetics. Cost analyses included telegenetics system; mileage; and personnel costs for genetic counselor, IT specialist, and clinic personnel. CGC attendance was tracked via study database. Patient satisfaction was assessed 1 week post-CGC via telephone survey using validated scales. Total costs were $106 per telegenetics patient and $244 per in-person patient. Patient satisfaction did not differ by group on either satisfaction scale. In-person patients were significantly more likely to attend CGC than telegenetics patients (89 vs. 79 %, p = 0.03), with bivariate analyses showing an association between lesser computer comfort and lower attendance rate (Chi-square = 5.49, p = 0.02). Our randomized trial of telegenetics vs. in-person counseling found that telegenetics cost less than in-person counseling, with high satisfaction among those who attended. This study provides support for future randomized trials comparing multiple service delivery models on longer-term psychosocial and behavioral outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A significant proportion of cancer patients and families stand to benefit from cancer genetic counseling (CGC). Established medical and psychosocial benefits of CGC include adherence to recommended cancer risk management behaviors (Hadley et al. 2004; Watson et al. 2005); risk-based surgical decision making (Schwartz et al. 2004; Weitzel et al. 2003); enhanced family communication of cancer risk (C Hughes et al. 2002); and decreased cancer worry and anxiety (Bish et al. 2002; Braithwaite et al. 2006). In recognition of these benefits, pre- and post-test CGC by a qualified health professional is now considered standard of care for cancer genetic testing (American College of Surgeons 2012; American Society of Clinical Oncology 2003; U. S. Preventive Services Task Force 2005).
At least 15 % of individuals with cancer are candidates for CGC (Hampel et al. 2004), but not all have access to urban medical centers (Olopade et al. 2003; U.S. Department of Health and Human Services 2006) where certified genetic counselors typically practice (Hammers 2009). Genetic counseling via live videoconferencing (telegenetics) can improve access to CGC in underserved areas with high levels of patient satisfaction (Coelho et al. 2005; d’Agincourt-Canning et al. 2008; Gray et al. 2000; Hilgart et al. 2012; Lea et al. 2005; Zilliacus et al. 2010b, 2011). But, no studies have employed a randomized design to compare outcomes between in-person and telegenetics counseling. Neither have studies systematically compared costs of cancer telegenetics vs. in-person counseling—a critical variable for those hoping to implement similar technology clinically (Coelho et al. 2005; d’Agincourt-Canning et al. 2008; Gray et al. 2000; Hilgart et al. 2012; Lea et al. 2005; Zilliacus et al. 2010b, 2011). Finally, most studies of cancer telegenetics were not conducted in the U.S., where practice models may differ from those abroad (Coelho et al. 2005; d’Agincourt-Canning et al. 2008; Gray et al. 2000; Hilgart et al. 2012; Wham et al. 2010; Zilliacus et al. 2010b, 2011).
We performed a randomized trial comparing cancer telegenetics with in-person CGC on short-term process measures: cost, patient satisfaction, and genetic counseling attendance. Each measure is important for establishing the acceptability of telegenetics to patients and health systems. Our intention was to provide a foundation for future studies comparing service delivery models on longer-term behavioral and psychosocial outcomes. Our research questions are:
-
1.
What were the per-patient costs of telegenetics vs. in-person counseling?
-
2.
At 1-week follow-up survey, did patient satisfaction differ between those who received counseling via telegenetics vs. in-person?
-
3.
Did genetic counseling attendance differ by group?
Methods
Study methodology is described in detail elsewhere (Datta et al. 2011) and summarized below. The study was approved by the Duke University Health System Institutional Review Board. Informed consent was obtained from all individual participants included in the study.
Participants
Individuals were eligible if they were referred for CGC in August 2008–January 2011 at one of four rural oncology clinics affiliated with the Duke Cancer Network and preferred to have their appointment locally instead of traveling to our academic medical center. All affected and unaffected individuals appropriate for CGC per published criteria (Daly et al. 2008; Hampel et al. 2004; U. S. Preventive Services Task Force 2005), and who had not had CGC, were eligible.
Participating clinics are located in counties with larger proportions of African Americans, American Indians, and Hispanics than state or national averages (U.S. Census Bureau 2010). Such groups have historically been underserved by CGC (C. Hughes et al. 1997; Olopade et al. 2003; Stacey et al. 2002). Average round-trip travel time from these clinics to our medical center is 3.5 h (range 1.5–5.5 h). Prior to this study, in-person CGC was available at these clinics 1 day per month for 3 years, reaching patients who might not have otherwise received CGC (Buchanan et al. 2009).
Procedures
Recruitment and Randomization
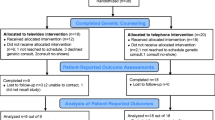
Physicians at participating rural clinics or associated medical offices referred patients according to published criteria (Daly et al. 2008; Hampel et al. 2004; U. S. Preventive Services Task Force 2005). Study staff at the academic medical center (study coordinator and two research assistants) contacted these patients by phone to describe the study and invite participation. Those who agreed were consented verbally and randomly assigned to have standard-of-care CGC (Trepanier et al. 2004) at their local oncology clinic via telegenetics or in-person (Fig. 1). A statistician used a computer program to generate the random assignment within each clinic. We did not stratify on demographic characteristics. Immediately after completing the consent process, study staff informed patients of their group assignment and scheduled a CGC appointment. A single genetic counselor saw all patients in both groups, either via telegenetics from his academic medical center office or by driving to the clinic. In keeping with our existing practice, in-person patients were seen on a monthly basis, increasing the probability of seeing multiple patients on the same day.
Telegenetics System
Counselor and patient communicated in real time on one screen and viewed documents commonly used during in-person CGC sessions (e.g., pedigrees) on a second screen. For each system, there was a one-time purchase of a desktop computer, two monitors, a webcam and external voiceover IP microphone, and SteadyState™ and Deep Freeze™ software to protect from misuse and configuration changes. Ongoing system operating costs included technical support and routine maintenance. We used existing clinic networks (without transmission costs) that were capable of maintaining a stable and reliable 384 kbps connection with sufficient audio and visual clarity (Jarvis-Selinger et al. 2008) and 128-bit AES industry-standard encryption. Clinic personnel (front desk or nursing staff) logged patients onto the system but did not stay with them or provide technical assistance. We tracked the percentage of attempted sessions in which a technical problem prevented a successful call or hampered call quality.
Cost Assessment, Patient Satisfaction, and Attendance
Telegenetics system costs for equipment, software, set-up and maintenance were summed. The genetic counselor used time logs to collect data to compare labor costs by group. Genetic counseling attendance was tracked via study database. One week post-counseling, study staff called participants to administer a survey assessing satisfaction (estimated 15 min/survey). We standardized survey administration by using a survey script, highly trained interviewers and a Computer Assisted Telephone Interviewing system with live data entry.
Instrumentation
Cost
The genetic counselor used a spreadsheet to track the labor, telegenetics system and travel costs. Patient care time pre-, during, and post-appointments was tracked for both groups. For the in-person group, genetic counselor travel time and mileage reimbursement were tracked. Among the telegenetics group we tracked genetic counselor time to train clinic personnel; clinic personnel labor (e.g., logging patients onto system); IT specialist labor (e.g., system set-up and maintenance); mileage to system set-up and training sessions; and telegenetics system cost.
Patient Satisfaction
Patient satisfaction was measured via two validated scales assessing different elements of satisfaction. The 6-item Genetic Counseling Satisfaction Scale (GCSS) uses 5-point Likert-type responses to measure: stress, whether counselor facilitated decision-making, health perception post-counseling, satisfaction with length of counseling, perception of counselor’s concern for patient’s well-being, and perceived value of counseling (Demarco et al. 2004). The GCSS has been validated in a CGC setting (Demarco et al. 2004). The 8-item Visit-Specific Satisfaction Questionnaire (VSQ) uses 5-point Likert-type responses to assess interpersonal care, office waiting time, technical care, and general satisfaction (Ware and Hays 1988). The VSQ has been widely used in primary care but, to our knowledge, has not been used to evaluate satisfaction with CGC. We revised the VSQ to replace ‘physician’ with ‘genetic counselor’ where applicable.
Genetic Counseling Attendance
Participants who never attended a scheduled genetic counseling session were recorded as non-attenders. Those who attended a session, even if they missed a previous appointment, were counted as attenders.
Other Measures
Demographic characteristics (age, education level, ethnicity, race, marital status, employment, and household income) were assessed during the initial telephone call using measures from our previous work (Buchanan et al. 2009). During the same call, we asked three close-ended “computer comfort” questions, the first two of which were drawn from the Computer-Email-Web Fluency Scale (Bunz 2004): “How comfortable do you feel using computers, in general?”; “How many hours per week do you use the Internet?”; and “Do you get anxious every time you learn something new about computers?” (Levine and Donitsa-Schmidt 1998) Collecting these data at baseline allowed analysis among attenders and non-attenders.
Knowledge of breast cancer genetics was measured in 1-week follow-up survey via the Breast Cancer Genetic Counseling Knowledge Questionnaire, a validated 27-item scale (Erblich et al. 2005). All participants completed the scale; analyses were limited to patients with a hereditary breast cancer indication.
We queried our clinical database to assess participants’ gender, cancer status (affected vs. unaffected), insurance status (private, Medicaid, Medicare, Tricare, none), referral indication (Hereditary Breast/Ovarian Cancer (HBOC) syndrome, Lynch syndrome and other/multiple indications) and genetic testing uptake (yes/no). If applicable, we also assessed participants’ risk score—prior probability of having HBOC or Lynch syndrome via BRCAPRO (Berry et al. 2002) or MMRPRO (Chen et al. 2006), respectively.
Data Analyses
Cost
To calculate labor costs, we collected salary and benefit data for the genetic counselor, clinic personnel, and IT specialists, then derived cost-per-minute wage rates and multiplied by the total number of minutes each person spent for in-person and telegenetics counseling, respectively. To calculate a per-patient cost, the sum was divided by the number of participants in each group.
To calculate telegenetics system costs, we collected prices paid for each item of telegenetics equipment and software ($2,400 per system), the one-time labor cost to set up the videoconferencing system ($831 per system), and annual maintenance cost ($161 per system). Because a telegenetics system has usefulness beyond the study, attributing all equipment, setup, and maintenance costs to only study participants would greatly overestimate the per-patient cost of the system (Drummond et al. 1999). Therefore, we fully depreciated each system’s costs (equipment, software, set-up and maintenance) over an assumed 5 years of useful life—operating 50 weeks per year, 5 days per week, with two sessions per day, for a total of 2500 patients per system. Thus, the total telegenetics system cost per patient was $1.61.
Patient Satisfaction
Values of 1–5 were assigned for VSQ and GCSS responses and summed for each scale to create an overall VSQ score and overall GCSS score for each participant. Two-sided pooled t-test was used to compare VSQ summary scores by group. Two-sided Satterthwaite t-test was used to compare GCSS summary scores by group.
To determine whether satisfaction varied by participant characteristics, we ran overall and within-group analyses for each satisfaction scale, using Chi-square or ANOVA tests for categorical or ordinal characteristics (e.g., race, income) and Pearson correlation coefficients for continuous characteristics (e.g., age, knowledge). Analyses were restricted to participants who completed both scales (GCSS and VSQ) because each scale measures different elements of satisfaction.
Genetic Counseling Attendance
We used Chi-square test to compare attendance by group. To determine whether attendance varied overall and within groups by participant characteristics measured at enrollment, we used Chi-square or Fisher’s Exact tests for categorical or ordinal variables and a two-sided pooled t-test for age. Categorical or ordinal variable responses were collapsed where necessary to achieve sufficient cell sizes (e.g., some Internet use vs. none).
Other Measures
Summary statistics were calculated within each group. To quantify probability of differences, we calculated P-values using Chi-square or Fisher’s Exact tests for dichotomous or ordinal variables and t-tests for continuous variables. Where necessary to achieve large enough expected cell sizes for Chi-square analyses, we collapsed responses into meaningful categories.
Results
Participant Characteristics
Participants were diverse in race, education, income, insurance status, computer comfort, computer anxiety and Internet use (Table 1). There were no significant differences by group in genetic testing uptake, referral indication or breast cancer genetics knowledge. Telegenetics participants were significantly more likely than in-person participants to be older, unemployed, and have an income below $30,000, and less likely to be “very” or “somewhat comfortable” with computers.
Telegenetics System Performance
Among the 74 attempted telegenetics consults, 15 % (n = 11) were hampered by technical problems, including 7 % in which a counseling session could not be completed and had to be rescheduled. Reasons include a hard drive crash and accidental assignment of the system’s IP address to another computer.
Research Question 1: What Were the Per-Patient Costs of Telegenetics vs. In-Person Counseling?
Total costs to provide CGC were $106.19 per telegenetics patient and $244.33 per in-person patient. Telegenetics system costs for each of the four rural clinics included one-time equipment and software costs of $2,400 and system-build and deployment labor costs of $831; annual maintenance cost was $161. As calculated above, the telegenetics system cost per telegenetics patient was $1.61. Including training time, clinic personnel at study clinics required a total of 13.2 h to log patients into their telegenetics sessions, a cost of $2.82 per telegenetics patient in facilitation costs. The genetic counselor spent a total of 201.4 h on pre-, peri-, and post-appointment genetic counseling for telegenetics patients, at a cost of $101.76 per patient.
For in-person counseling, the genetic counselor spent 158.2 h traveling to the four oncology clinics, a travel time cost of $77.03 per patient. He traveled 10,360 miles to provide CGC and was reimbursed $0.50 per mile traveled, for a per-patient travel mileage reimbursement of $63.95. He spent a total of 203 h on genetic counseling for in-person patients, at a cost of $103.35 per patient.
Research Question 2: At 1-Week Follow-Up Survey, Did Patient Satisfaction Differ Between Those who Received Counseling via Telegenetics vs. In-Person?
Satisfaction with CGC was high in both groups, on both scales, with no significant difference by group (Table 2). Cronbach’s alphas for the VSQ and GCSS were 0.88 and 0.82, respectively. Age, marital status, computer anxiety, Internet use, insurance status, referral indication, genetic testing uptake and risk score were not significantly associated with satisfaction overall or within either group. Within the telegenetics group, none of the variables analyzed was associated with satisfaction on either scale (Table 3). After applying the Bonferroni correction for multiple comparisons, education remained significantly associated with satisfaction (VSQ, in-person group, only).
Nearly all telegenetics participants reported that they could hear and see the genetic counselor clearly (95 and 96 %, respectively); 91 and 96 % of telegenetics participants thought the genetic counselor could hear and see them clearly. A majority of telegenetics participants (64 %) reported needing no help to use the system; 18 % needed a little help. Nearly all (98 %) reported being comfortable using the telegenetics system to talk with the genetic counselor, but 32 % would have preferred to see the genetic counselor in person.
Research Question 3: Did Genetic Counseling Attendance Differ by Group?
Participants assigned to in-person CGC were significantly more likely to attend their appointment than their telegenetics counterparts (89 vs. 79 %, p = 0.03). For all appointments (in-person and telegenetics), non-attenders were significantly more likely to have less than college education, be non-white, not married or living with a partner, unemployed, and have less than $50,000 household income (Table 4). They were less likely to be very or somewhat comfortable with computers and to use the Internet. After applying the Bonferroni correction for multiple comparisons, race, income and computer comfort remained significantly associated with attendance for all appointments.
To determine whether these factors were differentially associated with attending a telegenetics vs. in-person appointment, we assessed them within groups (Table 4). Participants who were very or somewhat comfortable with computers were significantly more likely to attend a telegenetics appointment. In-person participants who were married/living with a partner and employed were significantly more likely to attend. After applying the Bonferroni correction for multiple comparisons within groups, only race remained associated with attendance (in-person group, only).
Discussion
Cancer genetic counseling is standard of care for individuals at increased risk of hereditary cancer (American College of Surgeons 2012; U. S. Preventive Services Task Force 2005). But, CGC is a scarce medical resource in rural communities. Telegenetics via live videoconferencing can improve rural access to CGC (Coelho et al. 2005; d’Agincourt-Canning et al. 2008; Gray et al. 2000; Lea et al. 2005; Zilliacus et al. 2010b, 2011), but lack of randomization, cost analyses and U.S. studies have limited rigorous evaluation of this service delivery model in the U.S.
We designed a preliminary step in testing the feasibility of cancer telegenetics in a community oncology setting, with study measures informed by this conception. Telegenetics would not improve access to CGC if it were not less expensive than in-person counseling, or if patients did not attend CGC or were dissatisfied with it.
In our randomized trial comparing telegenetics with in-person CGC, we found the cost of cancer telegenetics was less than half that of in-person counseling. This difference was driven primarily by the genetic counselor’s travel cost (in mileage reimbursement and personnel cost while traveling); cost for the genetic counselor’s patient care time was nearly identical between groups. Telegenetics system and clinic personnel costs had minimal impacts on telegenetics cost.
We found no between-group difference in patient satisfaction. Although previous studies of cancer telegenetics have reported high satisfaction with CGC (Coelho et al. 2005; d’Agincourt-Canning et al. 2008; Gray et al. 2000; Lea et al. 2005; Zilliacus et al. 2010b, 2011), ours is the first to do so via a randomized trial. Further, our use of a genetic counseling model commonly used in the U.S. (genetic counselor sees patients independently, with prior consult with attending physician) (Wham et al. 2010) and diverse study sample supplement existing literature such that results can be readily applicable to CGC practice in the U.S.
Study Limitations
It is important to not over-emphasize the lack of significant difference in satisfaction by group. Patients were more likely to attend in-person counseling versus telegenetics sessions, raising the possibility that high post-counseling patient satisfaction in the telegenetics group may have occurred due to selection bias. Bivariate analyses showed that this differential attendance might have been due to greater computer comfort among telegenetics attenders, though this association did not persist after performing the Bonferroni correction for multiple comparisons. Additionally, the study was not designed to test equivalence or non-inferiority of telegenetics vs. in-person counseling. Further, the lack of difference may have been the result of a ceiling effect due to high patient satisfaction in both groups. Therefore, a conservative interpretation of the satisfaction data is simply that those who attended genetic counseling via either service delivery model were highly satisfied.
In-person counseling cost was heavily dependent on the genetic counselor’s travel costs of mileage reimbursement and personnel cost while traveling. These findings may not be generalizable to institutions with different personnel costs or distances to outlying clinics.
Although breast cancer genetics knowledge did not differ by group, knowledge in both groups was lower than in the knowledge scale’s validation study (Erblich et al. 2005). Education level appeared to be lower among our participants compared with those in the validation study (Erblich et al. 2005). It is unclear whether this difference in education level or another factor such as the effectiveness of the genetic counselor explains the lower knowledge scores in our study.
Neither is it clear why baseline characteristics differed significantly by group on several variables in spite of random assignment. Notably, there was no difference in satisfaction by group even though factors such as older age and less computer comfort in the telegenetics group could conceivably be associated with less satisfaction with telegenetics.
Practice Implications and Research Recommendations
With caveats noted above regarding attendance and satisfaction, we have found that telegenetics is acceptable to patients at lower cost than in-person counseling. And, the lack of difference by group in genetic testing uptake and breast cancer genetics knowledge suggests that the education capabilities of telegenetics may be similar to those of in-person counseling. These findings lay the foundation for further examination of telegenetics as a service delivery model for CGC (Hilgart et al. 2012). Given the recent success of telephone CGC in a randomized trial (Schwartz et al. 2014), a valuable next step would be a randomized trial comparing in-person vs. telegenetics vs. telephone CGC on a wide range of system-, patient- and clinician-level variables, including reimbursement for CGC, psychosocial outcomes (Zilliacus et al. 2011), behavioral outcomes such as adherence to recommended risk management (Hilgart et al. 2012), genetic testing uptake, and clinician comfort with service delivery model (Zilliacus et al. 2010a).
Future research focused on telegenetics could investigate methods for reducing technical difficulties (e.g., using dedicated videoconferencing systems, trained support personnel or a backup system) and compare costs of computers vs. dedicated videoconferencing systems on lost clinical hours and support cost hours. Methods for increasing attendance (e.g., patient education materials or secure videoconferencing to patients’ homes) also merit further study. A more extensive cost effectiveness study could test telegenetics costs in a geographic area different from ours in distance between clinics and overall size. Finally, studies could model the potential reach of telegenetics by accounting for differential drop in attendance compared with in-person counseling.
Conclusions
In summary, this is the only randomized trial of which we are aware that compares telegenetics with in-person cancer genetic counseling, and the only one to report a cost comparison by service delivery model (Hilgart et al. 2012). Our finding that the cost of CGC via telegenetics was less than half that of in-person CGC provides hope for oncology clinics who want access to CGC but cannot fund an in-person genetic counselor. Telegenetics may not be acceptable to all underserved individuals. However, patient satisfaction was high among those who did attend a telegenetics session, even among individuals who might not be expected to be comfortable with computers. Findings support the development of randomized trials that test the equivalence of multiple service delivery models on important longer-term behavioral and psychosocial outcomes.
References
American College of Surgeons (2012). Cancer program standards 2012: Ensuring patient-centered care. Retrieved from http://www.facs.org.
American Society of Clinical Oncology. (2003). American Society of Clinical Oncology policy statement update: genetic testing for cancer susceptibility. Journal of Clinical Oncology, 21(12), 2397–2406.
Berry, D. A., Iversen, E. S., Jr., Gudbjartsson, D. F., Hiller, E. H., Garber, J. E., Peshkin, B. N., Lerman, C., Watson, P., Lynch, H. T., Hilsenbeck, S. G., Rubinstein, W. S., Hughes, K. S., & Parmigiani, G. (2002). BRCAPRO validation, sensitivity of genetic testing of BRCA1/BRCA2, and prevalence of other breast cancer susceptibility genes. Journal of Clinical Oncology, 20(11), 2701–2712.
Bish, A., Sutton, S., Jacobs, C., Levene, S., Ramirez, A., & Hodgson, S. (2002). Changes in psychological distress after cancer genetic counseling: a comparison of affected and unaffected women. British Journal of Cancer, 86, 43–50.
Braithwaite, D., Emery, J., Walter, F., Prevost, A. T., & Sutton, S. (2006). Psychological impact of genetic counseling for familial cancer: a systematic review and meta-analysis. Familial Cancer, 5(1), 61–75.
Buchanan, A. H., Skinner, C. E., Calingaert, B., Schildkraut, J. M., King, R. H., & Marcom, P. K. (2009). Cancer genetic counseling in rural North Carolina oncology clinics: program establishment and patient characteristics. Community Oncology, 6, 70–77.
Bunz, U. (2004). The Computer-Email-Web (CEW) fluency scale-development and validation. International Journal of Human Computer Interaction, 17(4), 479–506.
Chen, S., Wang, W., Lee, S., Nafa, K., Lee, J., Romans, K., Watson, P., Gruber, S. B., Euhus, D., Kinzler, K. W., Jass, J., Gallinger, S., Lindor, N. M., Casey, G., Ellis, N., Giardiello, F. M., Offit, K., Parmigiani, G., & Colon Cancer Family, R. (2006). Prediction of germline mutations and cancer risk in the Lynch syndrome. JAMA, 296(12), 1479–1487.
Coelho, J. J., Arnold, A., Nayler, J., Tischkowitz, M., & MacKay, J. (2005). An assessment of the efficacy of cancer genetic counselling using real-time videoconferencing technology (telemedicine) compared to face-to-face consultations. European Journal of Cancer, 41(15), 2257–2261.
d’Agincourt-Canning, L., McGillivray, B., Panabaker, K., Scott, J., Pearn, A., Ridge, Y., & Portigal-Todd, C. (2008). Evaluation of genetic counseling for hereditary cancer by videoconference in British Columbia. British Columbia Medical Journal, 50(10), 554–559.
Daly, M., Axilbund, J., Bryant, E., Buys, S., Esserman, L., Farrell, C., et al. (2008). NCCN practice guidelines in oncology: Genetic/familial high-risk assessment: breast and ovarian. Version 1.2008. Retrieved Feb 11, 2011, from http://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf. Accessed 11 Feb 2011.
Datta, S. K., Buchanan, A. H., Hollowell, G. P., Bereford, H. F., Marcom, P. K., & Adams, M. B. (2011). Telemedicine vs in-person cancer genetic counseling: measuring satisfaction and conducting economic analysis. Journal of Comparative Effectiveness Research, 1, 43–50.
Demarco, T., Peshkin, B., Mars, B., & Tercyak, K. (2004). Patient satisfaction with cancer genetic counseling: a pyschometric analysis of the genetic counseling satisfaction scale. Journal of Genetic Counseling, 13(4), 293–304.
Drummond, M. F., O'Brien, B. J., Stoddart, G. L., & Torrance, G. W. (1999). Chapter 4: Cost analysis. In Methods for the economic evaluation of health care programmes (2nd ed.). Oxford: Oxford University Press.
Erblich, J., Brown, K., Kim, Y., Valdimarsdottir, H. B., Livingston, B. E., & Bovbjerg, D. H. (2005). Development and validation of a Breast Cancer Genetic Counseling Knowledge Questionnaire. Patient Education and Counseling, 56(2), 182–191.
Gray, J., Brain, K., Iredale, R., Alderman, J., France, E., & Hughes, H. (2000). A pilot study of telegenetics. Journal of Telemedicine and Telecare, 6(4), 245–247.
Hadley, D. W., Jenkins, J. F., Dimond, E., de Carvalho, M., Kirsch, I., & Palmer, C. G. (2004). Colon cancer screening practices after genetic counseling and testing for hereditary nonpolyposis colorectal cancer. Journal of Clinical Oncology, 22(1), 39–44.
Hammers, E. (2009). Innovations in service delivery in the age of genomics: Workshop summary. Washington, D. C.: National Academy of Sciences.
Hampel, H., Sweet, K., Westman, J. A., Offit, K., & Eng, C. (2004). Referral for cancer genetics consultation: a review and compilation of risk assessment criteria. Journal of Medical Genetics, 41(2), 81–91.
Hilgart, J. S., Hayward, J. A., Coles, B., & Iredale, R. (2012). Telegenetics: a systematic review of telemedicine in genetics services. Genetics in Medicine, 14(9), 765–776.
Hughes, C., Gomez-Caminero, A., Benkendorf, J., Kerner, J., Isaacs, C., Barter, J., & Lerman, C. (1997). Ethnic differences in knowledge and attitudes about BRCA1 testing in women at increased risk. Patient Education and Counseling, 32(1–2), 51–62.
Hughes, C., Lerman, C., Schwartz, M., Peshkin, B., Wenzel, L., Narod, S., Corio, C., Tercyak, K. P., Hanna, D., Main, D., & Isaacs, C. (2002). All in the family: Evaluation of the processand content of sisters’ communication about BRCA1 and BRCA2 genetic test results. American Journal of Medical Genetics, 107, 143–150.
Jarvis-Selinger, S., Chan, E., Payne, R., Plohman, K., & Ho, K. (2008). Clinical telehealth across the disciplines: lessons learned. Telemedicine Journal and e-Health, 14(7), 720–725.
Lea, D. H., Johnson, J. L., Ellingwood, S., Allan, W., Patel, A., & Smith, R. (2005). Telegenetics in Maine: Successful clinical and educational service delivery model developed from a 3-year pilot project. Genetics in Medicine, 7(1), 21–27.
Levine, T., & Donitsa-Schmidt, S. (1998). Computer use, confidence, attitudes, and knowledge: a causal analysis. Computers in Human Behavior, 14(1), 125–146.
Olopade, O. I., Fackenthal, J. D., Dunston, G., Tainsky, M. A., Collins, F., & Whitfield-Broome, C. (2003). Breast cancer genetics in African Americans. Cancer, 97(1 Suppl), 236–245.
Schwartz, M. D., Lerman, C., Brogan, B., Peshkin, B. N., Halbert, C. H., DeMarco, T., et al. (2004). Impact of BRCA1/BRCA2 counseling and testing on newly diagnosed breast cancer patients. Journal of Clinical Oncology, 22(10), 1823–1829.
Schwartz, M. D., Valdimarsdottir, H. B., Peshkin, B. N., Mandelblatt, J., Nusbaum, R., Huang, A. T., Chang, Y., Graves, K., Isaacs, C., Wood, M., McKinnon, W., Garber, J., McCormick, S., Kinney, A. Y., Luta, G., Kelleher, S., Leventhal, K.-G., Vegella, P., Tong, A., & King, L. (2014). Randomized noninferiority trial of telephone versus in-person genetic counseling for hereditary breast and ovarian cancer. Journal of Clinical Oncology, 32(7), 618–626.
Stacey, D., DeGrasse, C., & Johnston, L. (2002). Addressing the support needs of women at high risk for breast cancer: evidence-based care by advanced practice nurses. Oncology Nursing Forum, 29(6), E77–E84.
Trepanier, A., Ahrens, M., McKinnon, W., Peters, J., Stopfer, J., Grumet, S. C., Manley, S., Culver, J. O., Acton, R., Larsen-Haidle, J., Correia, L. A., Bennett, R., Pettersen, B., Ferlita, T. D., Costalas, J. W., Hunt, K., Donlon, S., Skrzynia, C., Farrell, C., Callif-Daley, F., Vockley, C. W., & National Society of Genetic, C. (2004). Genetic cancer risk assessment and counseling: recommendations of the National Society of Genetic Counselors. Journal of Genetic Counseling, 13(2), 83–114.
U. S. Preventive Services Task Force. (2005). Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: recommendation statement. Annals of Internal Medicine, 143(5), 355–361.
U.S. Census Bureau (2010). North Carolina QuickFacts. 2010 Census of Population and Housing, Demographic Profile,. Retrieved May 10, 2013, from http://www.quickfacts.census.gov/qfd/states/37000.html.
U.S. Department of Health & Human Services (2006). Coverage and reimbursement of genetic tests and services: Report of the Secretary’s Advisory Committee on Genetics, Health, and Society. http://oba.od.nih.gov/oba/sacghs/reports/CR_report.pdf.
Ware, J. E., Jr., & Hays, R. D. (1988). Methods for measuring patient satisfaction with specific medical encounters. Medical Care, 26(4), 393–402.
Watson, M., Kash, K. M., Homewood, J., Ebbs, S., Murday, V., & Eeles, R. (2005). Does genetic counseling have any impact on management of breast cancer risk? Genetic Testing, 9(2), 167–174.
Weitzel, J. N., McCaffrey, S. M., Nedelcu, R., MacDonald, D. J., Blazer, K. R., & Cullinane, C. A. (2003). Effect of genetic cancer risk assessment on surgical decisions at breast cancer diagnosis. Archives of Surgery, 138(12), 1323–1328. discussion 1329.
Wham, D., Vu, T., Chan-Smutko, G., Kobelka, C., Urbauer, D., & Heald, B. (2010). Assessment of clinical practices among cancer genetic counselors. Familial Cancer, 9(3), 459–468.
Zilliacus, E., Meiser, B., Lobb, E., Dudding, T. E., Barlow-Stewart, K., & Tucker, K. (2010a). The virtual consultation: practitioners’ experiences of genetic counseling by videoconferencing in Australia. Telemedicine Journal and e-Health, 16(3), 350–357.
Zilliacus, E. M., Meiser, B., Lobb, E. A., Kirk, J., Warwick, L., & Tucker, K. (2010b). Women’s experience of telehealth cancer genetic counseling. Journal of Genetic Counseling, 19(5), 463–472.
Zilliacus, E. M., Meiser, B., Lobb, E. A., Kelly, P. J., Barlow-Stewart, K., Kirk, J. A., Spigelman, A. D., Warwick, L. J., & Tucker, K. M. (2011). Are videoconferenced consultations as effective as face-to-face consultations for hereditary breast and ovarian cancer genetic counseling? Genetics in Medicine, 13(11), 933–941.
Acknowledgments
The authors wish to thank the Duke Cancer Network and participating clinics for their support of this study, and of genetic counseling in underserved communities.
Funding
The study described here was supported by grant DISP0707781 from Susan G. Komen for the Cure, which had no role in the design of the study described here or in the development or approval of this manuscript. Portions of the salaries of Mr. Buchanan, Drs. Datta, Hollowell, and Adams, and Mr. Beresford, Mr. Freeland, Mr. Rogers, and Mr. Boling were funded by this grant. Drs. Skinner and Marcom did not receive salary or other support from this grant.
This manuscript was made possible by Grant Number 1 UL1 RR024128-01 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Conflict of Interest
Mr. Buchanan’s work has been funded by the NIH. Dr. Datta’s work has been funded by the Department of Defense and VA Health Services Research & Development. Dr. Skinner’s work has been funded by the NIH and the Cancer Prevention Research Institute of Texas. Dr. Hollowell’s work has been funded by the Howard Hughes Medical Institute. Mr. Rogers’ work has been funded by the Alpha-1 Foundation. Dr. Marcom’s work has been funded by the NIH and Department of Defense. Dr. Adams has served as a consultant to Sanofi, Drexel University, CustomID and MED-IQ. The authors declare that these relationships are not directly or indirectly related to the research described in this manuscript.
Human Studies and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Animal Studies
This article does not contain any studies with animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
ClinicalTrials.gov Identifier: NCT00609505
Rights and permissions
About this article
Cite this article
Buchanan, A.H., Datta, S.K., Skinner, C.S. et al. Randomized Trial of Telegenetics vs. In-Person Cancer Genetic Counseling: Cost, Patient Satisfaction and Attendance. J Genet Counsel 24, 961–970 (2015). https://doi.org/10.1007/s10897-015-9836-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-015-9836-6