Abstract
Mucopolysaccharidosis type II (MPS II), also known as Hunter syndrome, is a chronic and progressive X-linked lysosomal disease that mainly affects males. The National MPS Society (2013) reports that MPS II affects 1 in 100,000 to 1 in 150,000 males worldwide. Two distinct forms of the disease are based on age of onset and clinical course: attenuated and severe. MPS II affects many organ systems including the nervous, cardiovascular, gastrointestinal and respiratory systems. Clinical manifestations can include progressive hearing loss, mental impairment, and enlarged liver and spleen. This study focuses on the health-related quality of life of individuals (HRQOL) with MPS II as measured by the parent and self-report versions of the Pediatric Quality of Life Inventory (PedsQL™). Both parents of patients with MPS II as well as patients themselves reported lower scores on all domains of the PedsQL™ (physical, emotional, social and school functioning) indicating that children with MPS II have an overall lower HRQOL when compared to a healthy sample. When compared with patients with other chronic illnesses (cancer, MSUD, galactosemia,), the MPS II sample had significantly lower scores on a number of PedsQL™ scales, suggesting an overall lower HRQOL. No significant relationships were found using scores from parent or self report PedsQL™ measures and length of time on ERT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mucopolysaccharidosis type II, MPS II, (also known as Hunter syndrome) is a chronic and progressive lysosomal storage disease in which there is deficient or absent activity of the enzyme iduronate-2-sulfatase (I2S). This enzyme contributes to the breakdown of the glycosaminoglycans (GAGs) dermatan sulfate and heparan sulfate (Froissart et al. 2007). Defective I2S results in the progressive pathologic accumulation of dermatan and heparan sulfates within the lysosome of all cells, and ultimately leads to cellular dysfunction. MPS II is an X-linked disorder that primarily affects males, although there are rare carrier females with disease-related manifestations. The National MPS Society (2013) reports that MPS II affects 1 in 100,000 to 1 in 150,000 males worldwide. The United States Food and Drug Administration (2006) estimates an incidence between 1/65,000 to 1/132,000 births. Severe (2/3 of patients [Froissart et al. 1998]) and attenuated forms have been described. Both forms present with somatic involvement; the most prominent feature in the severe form is profound central nervous system involvement causing neurological deterioration.
MPS II is a multisystemic disorder displaying a spectrum of clinical involvement with significant variability in age of onset and rate of progression. It can affect the central and peripheral nervous systems, and the cardiovascular, gastrointestinal, respiratory, and musculo-skeletal systems. Frequent clinical manifestations include short stature, progressive airway obstruction, respiratory infections, hepatomegaly, splenomegaly, cardiac disease, thickened and inelastic skin, coarse facial features, elevated intracranial pressure, macrocephaly, mental impairment, seizures, carpal tunnel syndrome, spinal cord compression, and bladder obstruction (Brown 1999; Schwartz et al. 2007). Visual problems, progressive hearing loss and chronic ear infections are also common (Martin et al. 2008; Wraith et al. 2008). Individuals with the severe phenotype possess many of the features described above, including profound central nervous system (CNS) involvement resulting in cognitive impairment and neurological deterioration. Those with the attenuated form of MPS II present with minimal to no neurologic involvement, can have normal intelligence, but may have all the somatic features. Accordingly, attenuated cases may have physical disabilities as severe as those with the severe form of the disease. The average age of diagnosis for the attenuated form is 4.3 years, with an average age of death at 21.7 years (Brown 1999). The severe form has an average age of diagnosis of 2.5 years with an average age of death at 11.8 years (Brown 1999). There is no cure for MPS II.
In 2006, the Food and Drug Administration approved the use of Eleprase® (idursulphase), a recombinant form of I2S for the treatment of MPS II. Weekly, intravenous enzyme replacement therapy (ERT) with Eleprase® results in a decrease in GAG storage potentially ameliorating the severity of some somatic symptoms and prophylactically preventing the development of others (Wraith 2008). Eleprase® does not cross the blood-brain barrier and has no impact on CNS disease.
Although parents often report concerns about their children’s developmental prognoses, psychosocial functioning, and HRQOL, research related to MPS II has largely focused on the medical aspects of the disease rather than psychological or HRQOL aspects. The psychological research has been limited to examination of behavior of people with MPS II, and has revealed that overactivity and aggressiveness are major problems for patients (Bax and Colville 1995; Young and Harper 1981). There has also been an indication that families are impacted psychosocially by MPS II; parents have reported feeling guilty and resentful towards the affected individual (Bax and Colville 1995). In addition, parents have expressed concern regarding a patient’s prognosis, behaviors, and health problems (Bax and Colville 1995; Young and Harper 1981). With respect to HRQOL research, Hale et al. 2008, compared the HRQOL in 4 individuals with severe MPS II before and after ERT. Another study examined HRQOL in patients with attenuated forms of MPS II and their parents (Raluy-Callado et al. 2013). To date, there has been no systematic, comprehensive study examining the HRQOL of people with attenuated and severe forms of MPS II, and examining the effect of ERT on HRQOL in these patients.
Quality of Life Framework
Quality of life has been defined as encompassing an individual’s sense of well-being across all major aspects of life including physical health and functioning, emotional, social, psychological, spiritual, and family dimensions (Cohen and Biesecker 2010; DeCivita et al. 2005). Other definitions include individual happiness and satisfaction in relation to important possibilities in life (DeCivita et al. 2005). In an attempt to narrow the quality of life construct, Health-Related Quality of Life (HRQOL) was introduced to emphasize life domains that are directly related to an individual’s health (DeCivita et al. 2005). HRQOL is a multidimensional and comprehensive construct defined as an individual’s subjective perception of his or her functioning and emotional state (Gold et al. 2009). Within the broader HRQOL construct, health status refers to physical functioning. The HRQOL construct also includes the psychosocial dimensions of emotional, social, and role functioning (Varni et al. 2002). In the area of pediatrics, healthcare professionals consider it important to find out how children/adolescents and their parents feel about the impact of disease on different aspects of life.
Pediatric HRQOL must be sensitive to cognitive development and integrate both child/adolescent self-report and parent proxy-report to reflect both perspectives (Varni et al. 2002). With respect to measuring HRQOL, The Pediatric Quality of Life Inventory (PedsQL™) was designed as a generic HRQOL instrument to be used across diverse pediatric populations (Varni et al. 2002). The PedsQL™ 4.0 Generic Core Scales measure the physical, mental, and social health dimensions set forth by the World Health Organization as well as role functioning. The PedsQL™ 4.0 has a school functioning scale to assess role functioning. Comparative HRQOL studies are especially important for vulnerable populations, e.g., individuals with chronic illness or disabilities.
Purpose of the Study
The goal of this study was to investigate the generic HRQOL of individuals with MPS II. To reach this goal, we compared the HRQOL of individuals with MPS II to normative data as well as to other chronic illness samples (MSUD, galactosemia, oncology). Finally, we investigated the relationship between quasi-independent variables (length of time on enzyme replacement therapy and HRQOL). Each patient with this chronic illness may not experience all possible clinical manifestations of MPS II; however, an affected individual still faces numerous chronic medical complications for a progressive, incurable disease.
Methods
Participants and Procedures
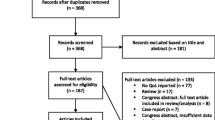
The participants were comprised of patients with MPS II and their parents. Patients were recruited through national MPS societies in English-speaking countries, hunterpatients.com, MPSforum.com, and contact with geneticists in the United States. The majority of participation took place over the phone; thus, most informed consents and assents were obtained verbally. To be eligible for the study, the patient had to have a confirmed biochemical or molecular diagnosis of MPS II. A total of 73 parents of patients with MPS II and 21 patients participated in the total study, which was approved by the University of California, San Francisco Committee on Human Research and the Institutional Review Board of Palo Alto University. One parent did not meet inclusion criteria and five additional parents expressed interest in participating in the study but were lost to follow up and/or limited availability (i.e. scheduling conflicts or limitations). Thus, there were no parents who did not express interest in participating; one parent did not meet inclusion criteria and five parents were lost to follow-up. Participants were equivalent to the nonparticipants in terms of gender, age, ethnicity, education, and utilization of ERT.
Instrumentation
Demographic Questionnaire
A demographic questionnaire gathered background information about the patient and family members. The questionnaire included age at diagnosis, severity of disorder, past and current treatment efforts, and the patient’s medical and mental health history. In 65 cases, parents, not patients, completed the questionnaires. In 8 instances, an adult patient participating in the study completed the questionnaire independent of a parent.
PedsQL™ Quality of Life
The Pediatric Quality of Life Inventory (PedsQL™) is a modular instrument designed to measure health-related quality of life (HRQOL) in children, adolelscents, and young adults. The 23-item PedsQL™ Generic Core Scales encompass 1) physical functioning (8 items), 2) Emotional Functioning (5 items), 3) Social Functioning (5 items), and 4) School Functioning (5 items). The Psychosocial Health Summary Score is created by combining the scores for three other subscales (i.e., the Emotional Functioning, Social Functioning, and School Functioning subscales). The PedsQL™ Parent Report asks parents to respond to 23 items related to the child’s HRQOL. There are also PedsQL™ Self Report forms for children, which have similar item content worded in an age-appropriate manner. The PedsQL™ has developmentally appropriate forms for people aged newborn to 25 years. In this study, parents completed the PedsQL™ Parent Report form and children/young adult patients who were able to do so completed the PedsQL™ Self Report form. Each PedsQL™ Parent Report requires parents to rate their child’s problems (during the past month) in the following domains: physical, emotional, social, and school functioning. A five-point Likert scale is used to evaluate the frequency of the child’s reported experiences for each item; the range consists of 0 “never” to 4 “almost always.”
Varni et al. (2001) reported that the PedsQL™ demonstrates acceptable internal consistency (alpha = .90 for parent proxy report) and validity. Varni et al. (2007) examined the reliability and validity of the child self-report version of the PedsQL™ and found that the Total Scores across the age subgroups approached or exceeded 0.90.
Results
Description of Sample
A total of 73 parents of patients with MPS II participated in our study, and 65 completed age-appropriate PedsQL™ forms. Additionally, 13 of the patients (with attenuated MPS II) were able to complete the PedsQL™ Self Report. The summary of patient demographic and medical characteristics is in Table 1. Due to the X-linked inheritance of the disorder, all patients included in the present study were male. Study participants came from geographic areas throughout the United States, and also included English-speaking patients and families from the United Kingdom, Canada, Ireland, and Australia. The research findings reported in the present article were part of a broader study on patients with MPS II, which included use of the Vineland Adaptive Behavior Scales, Second Edition, Survey Interview Form (VABS II; Sparrow et al. 2005) to assess adaptive functioning (Needham et al. 2014). Using estimates of variability from the VABS-II manual, the sample size was based on power of 0.8 to detect a difference of 3 points from the norm in the Adaptive Behavior Composite scale. The target N to achieve this power was N = 80. For the actual sample size of this study (N = 73), the minimum detectable difference was 3.1 (Needham et al. 2014).
Within the sample, 22 patients had an attenuated form of MPS II and 29 patients had a severe form of the disease. The parents of the other 22 patients in the sample were unaware as to whether their child’s illness was classified as attenuated or severe. The mean age of the entire patient sample was 12.52 years (SD = 8.88). The mean age of the attenuated group was 17.72 years (SD = 11.87); mean age of the severe group was 8.86 years (SD = 4.76). While the sample reflected some ethnic diversity, the majority of patients were Caucasian (82.2 %, n = 60). Sixty-three of the patients (86.3 %) were enrolled in school at the time of the research interview; many were reported to be in special education classroom environments.
Comparison to Normative Healthy Sample
PedsQL™ Quality of Life Inventory—Parent Report
The HRQOL of patients with MPS II ages 21 and under was assessed through administration of the PedsQL™ HRQOL—Parent Proxy Report. Parent reports for the MPS II group were assessed against parent reports for a normative sample of healthy children (Varni et al. 2002) using one sample t-tests to determine if there were any statistically significant differences between the health dimension scores of the two groups (Table 2). As shown in Table 2, parents reported significantly lower scores for patients with MPS II (indicating a lower parental perceived HRQOL) when compared to the parent reports of healthy patients on all dimensions of the PedsQL™ including: physical functioning and physical health summary (p < .0001), emotional functioning (p < .0001), social functioning (p < .0001), school functioning (p < .0001), psychosocial health (p < .0001), and total score (p < .0001).
PedsQL™ Quality of Life Inventory—Self Report
The HRQOL of patients ages 21 and under was also assessed through administration of the PedsQL™ Quality of Life—Self Report, which was completed by 13 patients. Self-report scores from MPS II patients were assessed against self-report scores from a normative healthy sample (Varni et al. 2002) using one sample t-tests to determine if there were any statistically significant differences between the two samples. It is important to note that while the parent report forms included information for patients with all forms of MPS II (attenuated and severe), only those with attenuated forms of MPS II were able to complete self-report forms. Therefore, the self-report findings reflect differences only between those with attenuated MPS II and a healthy sample. The results for self-report scores show that the mean scores of the patients with MPS II were significantly lower than the mean scores reported by healthy children for the physical health score (p = .0048), the social functioning score (p = .0006), the psychosocial health score (p = 0.0241), and the total score (p = .0057) (Table 3). However, no statistically significant differences were found on the emotional and school functioning scales.
Comparison to Other Chronic Illness Samples
Data collected from parents were compared to scores reported by the parents of cancer patients (Varni et al. 2002) and to parent-report scores of other metabolic disorders: galactosemia and maple syrup urine disease (MSUD) (Vierling 2011) through separate one sample t-tests. The self-report scores of patients with MPS II were also assessed against the self-report scores of oncology patients (Varni et al. 2002). No patients with severe MPS II were able to complete self-report measures, so the findings reflect a comparison only of patients with attenuated forms of MPS II as compared to the scores of the oncology sample.
Parent Report
The parent report scores for patients with MPS II were lower than the parent report scores for the oncology sample for all scales, indicating a lower parental perceived HRQOL for the MPS II sample in nearly all domains (Table 4). Notably, the means for the MPS II sample were significantly lower than the oncology sample, (p < .0001 for total score, physical health, psychosocial health, social, and school functioning). The emotional functioning of the MPS II sample was not found to be significantly different from the oncology sample (p = .2442).
For the comparison of parent-report scores for patients with MPS II and patients with galactosemia, the parent scores for individuals with MPS II were lower on all scales, indicating a lesser parental perceived HRQOL (Table 5). There were sufficiently large differences between the two groups to show significance for physical health (p < .0001); psychosocial summary (p = .0035); total score (p < .0001); social functioning (p = .0116); and school functioning (p < .0001). Similarly, for the comparison of parent-report scores for patients with MPS II and patients with MSUD the MPS II parent scores were lower on all scales. There were statistically significant differences between the two groups for physical health (p = .005), indicating a lower parental perceived HRQOL in terms of physical health for MPS II patients. All other scales (psychosocial health; total scale; and emotional, social, and school functioning) did not reveal any significant differences between the two groups.
Self Report
The patients who completed self-report forms of the PedsQL™ (N = 13) represent those with attenuated forms of MPS II. There were no notable differences between the MPS II and oncology groups in any of the PedsQL™ domains, indicating a similar HRQOL for the two groups from the patient perspective.
Comparison of Attenuated and Severe MPS II
Comparisons between patients with MPS II in this study based on level of severity were made for the PedsQL™ Parent Report. The results were calculated using analysis of covariance (ANCOVA) with severity of illness as the primary independent variable and patient age as the covariate; analyses included a Bonferroni correction. The scores of patients with the severe form of MPS II were significantly lower than the scores reported for those with the attenuated form of MPS II for the patients’ physical health [F(1,42) = 31.2, p < .0001], total score [F(1,41) = 14.9, p = .0028], and school functioning [F(1,41) = 18.4, p = .0008], indicating lower functioning and HRQOL for these domains. For emotional functioning [F(1,41) = 0.4, p = 3.6947], social functioning [F(1, 41) = 3.2, p = .5720], and psychosocial health summary [F(1,41) = 4.9, p = .2236], there were no significant differences between patients with attenuated versus severe MPS II, as reported by parents.
Length of Time on ERT and HRQOL
Parent Report
Spearman partial correlations were conducted to explore the relationship between HRQOL and length of time on ERT, controlling for age. No statistically significant relationships were found between length of time on ERT and HRQOL on any scales, with Bonferroni p values of 1.00 for all but one domain (which was school functioning, p = .727).
Self Report
The relationship between HRQOL and length of time on ERT was further investigated through Spearman partial correlations calculated using patient self-report scores provided on the PedsQL™ Self Report (N = 12), also controlling for age. These results are limited to patients with more attenuated forms of MPS II, as no patients with severe MPS II completed the measure. The results revealed no significant findings in regards to length of time on ERT and self-report ratings of HRQOL when controlling for age.
Severity of Illness and Quality of Life
Parent-Report
Spearman partial correlations were conducted to investigate the relationship between severity of illness and HRQOL reported by parents on the PedsQL™ Parent Report. A significant relationship was not found between severity of illness and any of the domains measured by the PedsQL™ (p = 1.00 for all domains).
Self-Report
Spearman rank correlations were conducted to investigate the relationship between severity of ERT and HRQOL reported by patients on the PedsQL™ -Self Report. Thirteen patients completed the PedsQL™; no patients completing the PedsQL™ had the severe form of MPS II, so results consider only those with attenuated forms of the disease. Scores reported by patients with MPS II were found to have a significant negative correlation with severity of illness for the following domains: physical health summary (r = −0.597, p < .0001), total score (r = −0.475, p = .0009) and school functioning (r = −0.482, p = .0007), indicating that as severity increases, HRQOL decreases and vice versa. Although there were also negative correlations between severity of illness with social functioning and psychosocial health, the relationships were not significant. The correlation between severity of illness and emotional functioning was also not significant.
Discussion
This is the first study to comprehensively investigate the Health-Related Quality of Life (HRQOL) of patients with all forms of MPS II. The study provided comparisons between HRQOL of patients with MPS II and those with other chronic illnesses, including heritable inborn errors of metabolism requiring complex, intrusive, and ongoing therapeutic interventions. In addition to exploring these factors, this study also examined the relationship between length of time on ERT and HRQOL.
The HRQOL of patients ages 21 years and younger was measured through administration of parent and self-report forms of the PedsQL™ Quality of Life Inventory. Parents reported significantly lower scores for patients with MPS II (attenuated and severe) when compared to the normative sample of healthy patients for all dimensions of the PedsQL™. Thus, parents perceive a lower HRQOL for patients with MPS II than healthy children and young adults in terms of overall physical and psychosocial health, as well as lower emotional, social, and school functioning. Likewise, on the self-report form of the PedsQL™, patients with attenuated MPS II also reported significantly lower scores regarding overall physical and psychosocial health, as well as overall HRQOL when compared with healthy children and young adults. This indicates a lower HRQOL overall from the patient perspective as well.
A comparison of the HRQOL of patients with attenuated and severe MPS II on the PedsQL™ showed that those with the severe form had significantly lower scores than those with the attenuated form for overall physical health, overall HRQOL, and school functioning (based on parent reports). However, according to parent reports, patients with attenuated and severe MPS II had the same level of functioning in the emotional and social domains.
The PedsQL™ parent report scores were compared to several other chronic illness samples: cancer, galactosemia and MSUD. Analysis of parent-reports showed that the MPS II sample had significantly lower scores on all scales of the PedsQL™ compared to a cancer sample. Scores were lower in all domains except emotional functioning, indicating a lower HRQOL in terms of physical, social, and school functioning. The MPS II sample group scored lower than the cancer group despite both sample groups having significant discomfort because of somatic manifestations, as well as significant risk of premature death. The broad nature of physical and cognitive disability associated with severe MPS II appears to negatively impact HRQOL to a greater extent than cancer. However, self-report scores (from reports by patients with attenuated forms of MPS II) indicated a similar HRQOL for the two groups in all domains. So patients with relatively normal cognitive function and likely less physical disability rated their own HRQOL in a similar fashion as did cancer patients.
When compared to a galactosemia sample through PedsQL™ parent reports, patients with MPS II scored significantly lower for overall physical and psychosocial health, as well as total score, social and school functioning, indicating that parents perceived a poorer HRQOL for MPS II patients in all domains except emotional functioning. When compared to parent-reports of an MSUD sample, the patients with MPS II (attenuated and severe) scored significantly lower for HRQOL in terms of overall physical health functioning. Galactosemia and MSUD, like MPS II, are inborn errors of metabolism requiring ongoing, complex and intensive therapeutic intervention to reduce morbidity and mortality. All these conditions have a significant risk of neurologic impairment and death if strict therapeutic regimens are not followed. These conditions can even have significant morbidity, including neurologic decline, despite the strictest adherence to a prescribed therapeutic regimen. Yet, even with the potentially poor outcomes in patients with galactosemia and MSUD the MPS II patient population was rated lower on most aspects of HRQOL. It is possible the multiorgan involvement and trajectory of cognitive decline in MPS II leads to the lower HRQOL scores than those of MSUD and galactosemia.
The impact of MPS II on physical functioning (i.e., pain; low energy; and difficulty exercising or doing sports, lifting, bathing, doing chores) is likely a direct consequence of disease manifestations (Brown 1999; Martin et al. 2008; Schwartz et al. 2007). Other dimensions pertaining to HRQOL (such as school, emotional and social functioning) may be impacted on a secondary level for MPS II youth. In terms of school functioning, many parents and child participants reported that the patient was frequently absent from school because of medical appointments and/or the child not feeling well. This impact on school functioning as a result of MPS II is highlighted by the poorer HRQOL in regard to school functioning revealed when comparing children with attenuated MPS II to those with severe MPS II, i.e., children with the severe form have notably lower functioning.
In the realm of social functioning, previous research in chronic illness (Grootenhuis et al. 2007) suggested significant differences in the social functioning of patients with chronic illness, as compared to healthy children, which is consistent with youth patients and parent reports in the present study. Meijer et al. (2000) found that physical restrictions and pain in chronically ill children were associated with a lower level of social activities. Similarly, the physical limitations and pain caused by MPS II may be linked to the reportedly lower social functioning of youth with MPS II. Children with MPS II may not be able to run or move as fluidly as well as their peers or for as long, which would limit their engagement in social activities (e.g. sports and social games), thereby decreasing overall peer interaction and possibly creating some social isolation. Additionally, differences in physical appearance and basic self-care and communication skills between patients and their healthy peers could lead to teasing or social isolation.
In terms of emotional functioning, which is also a part of the patients’ overall psychosocial functioning, Taylor and Aspinwall (1996) noted that chronic illness “can produce…adverse emotional effects” (p. 22). In contrast, Grootenhuis et al. (2007) examined HRQOL in children with chronic illness and did not find any differences from healthy children in regards to the experience of negative emotions. Self-reports from patients in the present study were in accordance with Grootenhuis et al. (2007) findings. On the other hand, parent reports were consistent with Taylor and Aspinwall (1996) assertion -- that is, parent reports indicated that the emotional functioning of youth with MPS II is significantly lower than that of healthy youth. It is possible that youth may disproportionately experience negative emotions such as worry, sadness, fear, or anger. These emotions may be linked to the physical experience and intellectual knowledge of the progressive nature of MPS II; difficulties in every day physical, social, and adaptive functioning; the frequency and intensity of treatments and medical appointments; the experience of physical pain; and/or knowledge of potential premature death caused by their illness. Differences in reporting may simply be a reflection of the higher level of overall functioning of patients (attenuated form of MPS II) who were able to participate in the study as compared to those who were not, reiterating the heterogeneity of the disease.
Of interest, within the MPS II sample, there were no notable differences in social and emotional functioning based on severity of illness, per parent report. It is possible that factors such as coping style and family functioning may influence a parent’s perception of HRQOL; if so, such factors could account for this finding. Living with a chronic, progressive disease, such as MPS II, may change parents’ perspective. As a result of this experience, there may be a reframing to adjust expectations and satisfaction (Cohen and Biesecker 2010; Grootenhuis et al. 2007). Thus, some coping strategies that parents use may be more effective than others in adapting to live with MPS II and this could influence their perception of HRQOL. In addition, family functioning may also impact one’s perception of HRQOL. It has been found that families that are cohesive and that have little conflict have better HRQOL (Cohen and Biesecker 2010). In sum, psychosocial factors, beyond physical manifestation of the disease may influence the parent’s perception of HRQOL.
We also investigated the relationship of length of time on ERT and HRQOL and determined that no significant relationships exist using scores from parent or self-report PedsQL™ measures. In severe cases, with CNS involvement, Eleprase® has been used to stabilize and possibly improve some somatic signs symptoms but has no effect on cognitive status or neurodegeneration. Additionally, in some cases Eleprase® has not had any significant benefit on somatic symptoms and has been discontinued (Muenzer et al. 2012). Since this study is the first to include severely affected MPS II patients in HRQOL assessments, it is possible that those without measurable improvements after ERT or those experiencing cognitive decline while on treatment are contributing to the equal scores in this part of the study.
In severely affected cases Eleprase® is almost always infused in a medically supervised setting, such as a hospital or infusion center. This requires travel to infusion sites and additional time for transportation, pre-infusion set-up and post-infusion monitoring. The time commitment involved in ERT may also influence the psychological HRQOL in patients receiving ERT and offset any other gains in HRQOL achieved with ERT.
The documentation that there is no relationship between length of time on ERT and HRQOL may also be a reflection of the fact that, although ERT may slow the progression of the disease, the disease still progresses over time. The data from parents also indicate that—regardless of any improvements related to ERT for individuals—overall, the health of MPS II patients adversely impacts the patients’ HRQOL in terms of physical and psychosocial functioning (school, emotional, and social).
Finally, we examined the relationship between severity of illness and the outcome variables. Although parent-report PedsQL™ scores did not indicate any correlation between severity of illness and HRQOL, self-report scores indicated that severity of illness was inversely related to physical functioning, total HRQOL, and school functioning (i.e., less severe illness, higher HRQOL scores).
Summary and Implications of Results for Genetic Counseling
The HRQOL of patients with MPS II is significantly lower than it is for healthy individuals. Reports indicate that in general the physical health of these patients does adversely impact their HRQOL, even more so than youth with other chronic illness (cancer) and other inborn errors (galactosemia, MSUD). The findings of this study should lead to more awareness among patients, families, and service providers about the impact the illness has on the patient’s HRQOL across a number of domains. Likewise, these findings might help those with a connection to MPS II to better understand and relate to each other, and encourage more open conversation about non-medical challenges that occur for the patients and families. The results also contribute to expanding knowledge about the HRQOL of MPS II patients for physicians, teachers, and mental health professionals who work with this population at one level or another. It is hoped that these findings will be useful in educating and preparing families whose child is newly diagnosed, and in the future may contribute to the development of programs or specific treatment recommendations that seek to address, or improve the HRQOL for individuals with this illness.
Strengths and Limitations of Research
There were several limitations in this study. First, the administration of measures was not ideal because it strayed from the standardized method of administration for some measures. There was also a small sample size for self-report measures, limiting the statistical power and generalizability; the findings only reflect a trend in the population. Another limitation of this study is that the comparison to other chronic illness groups was based on previously published data. Therefore, there are inconsistencies between some of the samples in recruitment, administration of the measures, and other external factors. Another limitation of this study includes uncontrolled variables specific to individual patients and families, such as specific genotype and mutation type, medical history not related to MPS II, and patient mental health history; differences in any of these variables could impact scores on the outcome measures.
The comparisons based on severity also have to be interpreted with caution, as there is no standardized measurement of severity for MPS II (Froissart et al. 2007). The severity of MPS II for the patients in this study were determined by patient’s own doctors, genetic counselors, and in some cases by the parents themselves based on the known characteristics of severe versus attenuated MPS II (e.g. cognitive deterioration).
Recommendations for Future Research
As one of the first studies in the field of psychology to focus solely on MPS II, these research findings pave the path for future MPS II research. Future research with this population may more closely examine differences based on age and culture or explicitly explore the differences between parent report and child reports on HRQOL measures.
This study utilized a cross-sectional design. A longitudinal study would be interesting to examine the changes in HRQOL and psychosocial functioning for MPS II patients over time, as the disease progresses. As ERT has become available to many patients at a young age, it would be interesting to explore the psychological aspects of patients in the future and see how severity and length of time on ERT might then interact with one another.
This study relied on parent reports, which were primarily mothers. It would be interesting to compare reports of multiple parents within the same family. There is also the opportunity for future studies to examine resiliency and coping skills for these patients, which could further inform treatment recommendations.
In summary, the findings in this study add to the literature on chronic illness and HRQOL. The challenges identified for this population through this research should inform treatment recommendations made for MPS II patients and families in the future.
References
Bax, M. C., & Colville, G. A. (1995). Behavior in mucopolysaccharide disorders. Archives of Disease in Childhood, 73, 77–81.
Brown, M. B. (1999). The mucopolysaccharidoses. In S. Goldstein & C. R. Reynolds (Eds.), Handbook of neurodevelopmental and genetic disorders in children (pp. 317–336). New York: The Guilford Press.
Cohen, J. S., & Biesecker, B. S. (2010). Quality of life in rare genetic conditions: a systematic review of the literature. American Journal of Medicine and Genetic A, 152A(5), 1136–1156.
DeCivita, M., Regier, D., Alamagir, A. H., Anis, A. H., Fitzgerald, M. J., & Marra, C. A. (2005). Evaluating health-related quality-of-life studies in paediatric populations. Pharmaco Economics, 23, 659–685.
Food and Drug Administration. (2006). Treatment for Hunter syndrome approved. FDA Consumer, September-October 2006:4.
Froissart, R., Maire, I., Millat, G., Cudry, S., Birot, A. M., Bonnett, V., Bouton, O., & Boson, D. (1998). Identification of iduronate sulftatase gene alterations in 70 unrelated Hunter patients. Clinical Genetics, 53, 362–368.
Froissart, R., Da Silva, I. M., & Maire, I. (2007). Mucopolysaccharidosis type II: an update on mutation spectrum. Acta Pædactrica, 96, 71–77.
Gold, J. I., Yetwin, A. K., Mahrer, N. E., Carson, M. C., Griffin, A. T., Palmer, S. N., & Joseph, M. H. (2009). Pediatric chronic pain and health-related quality of life. Journal of Pediatric Nursing, 24(2), 141–150.
Grootenhuis, M. A., Koopman, H. M., Verrips, E. G. H., Vogels, A. G. C., & Last, B. F. (2007). Health-related quality of life problems of children aged 8–11 years with a chronic disease. Developmental Neurorehabilitation, 10, 27–33.
Hale S., Merritt J. L., Scott C. R., Hahn S., Schubert P., Raff M. 2008. Quality-of-life changes in MPS II patients receiving enzyme replacement therapy. Poster presentation at Lysosomal Disease Network (WORLD) Symposium.
Martin, R., Beck, M., Eng, C., Giugliani, R., Harmatz, P., & Muñoz, V. (2008). Recognition and diagnosis of mucopolysaccharidosis II (Hunter Syndrome). Pediatrics, 121, 377–386.
Meijer, S. A., Sinnema, G., Bijstra, J. O., Mellenbergh, G. J., & Wolters, W. H. G. (2000). Social functioning in children with a chronic illness. The Journal of Child Psychology and Psychiatry, 41, 309–317.
Muenzer, J., Bodamer, O., Burton, B., Clarke, L., Frenking, G. S., Giugliani, R., Jones, S., Rojas, M. V. M., Scarpa, M., Beck, M., & Harmatz, P. (2012). The role of enzyme replacement therapy in severe Hunter syndrome—an expert panel consensus. European Journal of Pediatrics, 171, 181–188.
National MPS Society. (2013). MPS II (Hunter syndrome). Retrieved from: http://www.mpssociety.org/mps/mps-ii/.
Needham, M. C., Packman, W., Rappoport, M., Quinn, N., Morgan, C., Cordova, M., Macias, S., & Packman, S. (2014). MPS II: adaptive functioning of patients and impact on the family system. Journal of Genetic Counseling, 23(3), 330–338. doi:10.1007/s10897–013–9665–4.
Raluy-Callado, M., Chen, W. H., Whiteman, D. A., Fang, J., & Wiklund, I. (2013). The impact of Hunter syndrome (mucopolyasccharidosis type II) on health-related quality of life. Orphanet Journal of Rare Diseases, 8, 1–10.
Schwartz, I., Ribeiro, M. G., Mota, J. G., Toralles, M. B. P., Correia, P., & Horovitz, D. (2007). A clinical study of 77 patients with mucopolysaccharidosis type II. Acta Pædactrica, 96, 63–70.
Sparrow S. S., Cicchetti D. V., Balla D. A. (2005). Vineland adaptive behavior scales (2nd ed.): survey forms manual. Circle Pines; AGS Publishing.
Taylor S. E., Aspinwall L. G. (1996). Psychosocial aspects of chronic illness. In P. T. Costa & G. R. VandenBos (Eds.), Psychological aspects of serious illness: Chronic conditions, fatal diseases, and clinical care: 7–60.
Varni, J. W., Seid, M., & Kurtin, P. S. (2001). The PedsQL™™ 4.0: reliability and validity of the pediatric quality of life inventory™ version 4.0 generic core scales in healthy and patient populations. Medical Care, 39, 800–812.
Varni, J. W., Burwinkle, T. M., Katz, E. R., Meeske, K., & Dickinson, P. (2002). The PedsQL™ in pediatric cancer: reliability and validity of the pediatric quality of life inventoryTM generic core scale, multidimensional fatigue scale, and cancer module. Cancer, 94, 2090–2106.
Varni, J. W., Limbers, C. A., & Burwinkle, T. M. (2007). How young can children reliably and validly self-report their health-related quality of life?: An analysis of 8,591 children across age subgroups with the PedsQL™ 4.0 generic core scales. Health and Quality of Life Outcomes, 5, 1.
Vierling S. C. (2011). Psychosocial functioning, health-related quality of life, and family impact in patients with classical galactosemia (Doctoral dissertation). Retrieved from Palo Alto University.
Wraith, J. E. (2008). Enzyme replacement therapy with idursulfase in patients with mucopolysaccharidosis type 2. Acta Paedactrica, 97, 76–78.
Wraith, J. E., Scarpa, M., Beck, M., Bodamer, O. A., De Meirleir, L., & Guffon, N. (2008). Mucopolysaccharidosis type II (Hunter syndrome): a clinical review and recommendations for treatment in the era of enzyme replacement therapy. European Journal of Pediatrics, 167, 267.
Young, I. D., & Harper, P. S. (1981). Psychosocial problems in Hunter syndrome. Child Care Health Development, 7, 201–209.
Acknowledgements
This project was supported in part by a grant from the Shire Human Genetic Therapies, Inc. No personnel from Shire Human Genetic Therapies, Inc. participated in the design, data analyses, or interpretation of the results of this study. This work was performed under the auspices of the UCSF-Stanford Lysosomal Disease Center. The Center has received support from the Niemann-Pick Disease Foundation, the Mt. Zion Health Fund, the Jewish Community Federation, the State of California Genetic Disease Branch, the Genzyme Corporation, the BioMarin Corporation, the Nutricia Corporation, Shire HGT, the Actelion Corporation, and Amicus Therapeutics. Most importantly, we would like to thank all participants for their cooperation.
Conflict of Interest
Authors Mary Needham, Wendy Packman, Natasha Quinn, Maxwell Rappoport, Christa Aoki, Alan Bostrom, Matthew Cordova, Sandra Macias, Cynthia Morgan, and Seymour Packman declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Animal Studies
This article does not contain any studies with animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Needham, M., Packman, W., Quinn, N. et al. Health-Related Quality of Life in Patients with MPS II. J Genet Counsel 24, 635–644 (2015). https://doi.org/10.1007/s10897-014-9791-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-014-9791-7