Abstract
First identified in 1997, cell-free fetal DNA (cffDNA) has just recently been used to detect fetal aneuploidy of chromosomes 13, 18, and 21, showing its potential to revolutionize prenatal genetic testing as a non-invasive screening tool. Although this technological advancement is exciting and has certain medical applications, it has been unclear how it will be implemented in a clinical setting. Genetic counselors will likely be instrumental in answering that question, but to date, there is no published research regarding prenatal counselors’ implementation of and experiences with cffDNA testing. We developed a 67 question survey to gather descriptive information from counselors regarding their personal opinions, experiences, thoughts, and concerns regarding the validity, usefulness, and implementation of this new technology. A total of 236 individuals completed a portion of the survey; not all respondents answered all questions. Qualitative questions complemented quantitative survey items, allowing respondents to voice their thoughts directly. Results indicate that counselors value cffDNA testing as a screening option but are concerned regarding how some obstetricians and patients make use of this testing. Further results, discussion, and practice implications are presented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The presence of cell-free fetal DNA (cffDNA) in maternal circulation was demonstrated in 1997 (Lo et al. 1997). Since that time, the ability to detect cffDNA has been used, primarily in Europe, to determine fetal sex, conduct single gene disorder testing for paternally-inherited alleles, determine fetal Rh factor status, and screen for other pregnancy-related disorders such as preeclampsia (Wright and Burton 2009). Most recently, cffDNA has been used to detect fetal aneuploidy of chromosomes 13, 18, and 21, showing its potential to revolutionize prenatal genetic testing as a non-invasive screening tool (Sayres et al. 2011). CffDNA testing is also commonly referred to as “non-invasive prenatal testing” (NIPT) or “non-invasive prenatal screening” (NIPS) in scientific and lay literature. Several studies have validated cffDNA testing for aneuploidy in high risk populations, reporting greater than 98 % sensitivity for the detection of trisomy 21, greater than 97 % and 78 % sensitivity for the detection of trisomy 18 and 13 respectively, and close to 100 % specificity for all three conditions (Benn et al. 2013; Bianchi et al. 2012; Chen et al. 2011; Chiu et al. 2011; Committee Opinion No. 545 2012; Ehrich et al. 2011; Norton et al. 2012; Palomaki et al. 2011, 2012; Sparks et al. 2012). Although these technological advances are exciting and have certain medical applications, it has been unclear how they will be implemented in a clinical setting as a tool for evaluating the possibility of fetal aneuploidy.
CffDNA testing has several advantages over other prenatal diagnostic tools and screening methods for aneuploidy. It is non-invasive with regard to the fetus, requiring only a maternal blood sample for analysis, and can be performed as early in gestation as chorionic villus sampling (CVS) (10 weeks gestation). CffDNA analysis may eventually have a lower cost than procedures necessary for diagnostic testing and has very high sensitivity and specificity in comparison to other screening methods. Conversely, diagnostic tests such as CVS and amniocentesis offer additional information (e.g. fetal karyotype, acetylcholinesterase level, infection status) that is not gleaned through a maternal blood test. Furthermore, standard screening tests may have shorter turn-around times and less chance for sample failure than cffDNA testing and are commonly covered by health insurance plans.
Several companies have developed validated cffDNA testing for aneuploidy, each attempting to capitalize on the advantages and minimize the drawbacks of this test. Vying for the prenatal screening market, these companies have advertised their tests to genetic counselors working in a prenatal setting, as well as to obstetricians and maternal fetal medicine specialists. However, consistent with recently released guidelines, genetic counseling seems appropriate for patients interested in prenatal cffDNA testing for aneuploidy. The American College of Obstetricians and Gynecologists released a statement in December 2012 emphasizing the need for pretest counseling for noninvasive prenatal testing (NIPT) for fetal aneuploidy and referral to a genetic counselor in the case of a positive test result (Committee Opinion No. 545). The National Society of Genetic Counselors (NSGC) likewise released a position statement in December 2012, urging that cffDNA testing “only be offered in the context of informed consent, education, and counseling by a qualified provider, such as a certified genetic counselor” (Devers et al. 2012). Therefore, although cffDNA testing is made directly available through primary prenatal care providers at some locations, prenatal genetic counselors are a major avenue through which patients have access to this testing option. Consequently, genetic counselors across the country are working to incorporate cffDNA testing into their prenatal counseling sessions and are instrumental in answering the question of how this technology will be implemented clinically.
Similar to any new technology, trial and error are necessary to find the appropriate clinical niche for cffDNA testing. Several factors may influence how genetic counselors are incorporating cffDNA testing, if at all, into their prenatal counseling session. Cost, expectations of insurance coverage, perceived “newness” of the technology, and demand from patients, as well as counselors’ own comfort with and confidence in this testing option, all play a role in setting the clinical stage for cffDNA testing for aneuploidy.
Purpose of the Study
To date, there is no published research regarding prenatal counselors’ implementation of and experiences with cffDNA testing. To address this gap in knowledge, we developed a survey to gather information from prenatal genetic counselors regarding their personal experiences, opinions, thoughts, and concerns regarding the validity, usefulness, and implementation of this new technology. The purpose of this paper is to provide initial insight into how cffDNA testing for aneuploidy is being implemented by prenatal genetic counselors across the country and what concerns need to be addressed.
Methods
Sample and Procedures
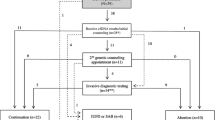
The target population for this study was genetic counselors involved in the care of at least one prenatal patient per week. After securing approval from the Indiana University Institutional Review Board (IRB) in Fall 2012, an invitation was distributed via an advertisement to the NSGC Discussion Forum (~N = 1,300). The invitation explained the nature and purpose of the study and provided genetic counselors with a hyperlink to the online survey. The survey instructions indicated that by choosing to continue, respondents gave their informed consent to be a part of this study. The survey remained open from October 2, 2012 to November 1, 2012. A total of 236 individuals completed a portion of the survey; not all respondents answered all questions. Of note, 237 submissions were recorded; one set of responses was excluded as it was found to be a duplicate by time of submission.
Instrumentation
A survey was developed through collaboration among the authors and was initially piloted on three prenatal genetic counselors not affiliated with the study. Based on pilot participants’ feedback, we adjusted wording for understanding and added questions to be more comprehensive, resulting in a 67-question survey. The survey was divided into five sections: Offering Testing, Perceived Patient Attitudes, Test Results, Counselor Opinions, and Background.Footnote 1 Respondents were given the option to provide free-text comments for several items. Respondents were not required to submit an answer in order to move on to the next question or page of questions. This was done in an effort to maximize the number of respondents and minimize the number of insincere answers given for the sake of expediting the survey. Respondents were able to access and change previous answers prior to submitting their responses. No IP addresses, names, contact information, or other personal identifying information were collected, guaranteeing respondent anonymity; responses from an individual participant were identified using the time of submission only. Upon submission of a survey, the participant’s responses were uploaded and stored by SurveyMonkey.com.
Data Analysis
Because participants were not required to answer all questions, data analysis was conducted individually for each question irrespective of the total respondent pool. Descriptive statistics including means, ranges, and frequencies were calculated by the first author for quantitative survey items. Some quantitative questions allowed respondents to enter a qualitative response in an “other” category in addition to their quantitative answer choices. Some respondents entered free text that matched quantitative answer choices instead of selecting the quantitative choices themselves. In ten cases where the free text was identical or directly analogous to the quantitative answers, respondents’ free text answers were converted to the quantitative format to allow a more accurate capture.
All other qualitative data were analyzed using an interpretive content analysis method (described in Patton 2001). The first author identified free text responses with similar motifs, grouped them together, and described their common themes and sub-themes. As new themes emerged, responses were re-categorized as necessary to accurately describe trends in detail. The last author audited the qualitative analysis; any discrepancies were discussed until resolved. Individual qualitative responses were excluded if they were not germane to the question asked. Frequencies were then calculated, and illustrative examples were chosen to represent themes common to 10 % or more of the responses for a given question. Lastly, for publication, commercial laboratory and test names were substituted with generic terms (e.g. Company X, Test X) both in the survey questions and the qualitative answers that are presented. The views expressed in the qualitative data are those of the respondents and do not necessarily reflect the position or opinions of the authors or this journal.
Results
Genetic Counselors’ Demographics
Thirteen questions collected information regarding respondents’ demographics. Counselors were asked to choose the most appropriate answer from multiple choices; only one answer choice per question was allowed. Some questions also gave counselors the opportunity to enter a quantitative response (e.g. age in years).
As shown in Table 1, 98 % (n = 199) of the respondents were female. The majority (94.6 %; n = 192) identified themselves as being White/Caucasian, and the second largest respondent group identified themselves as Asian/Pacific Islander (2.5 %; n = 5). Most respondents were between 25 and 34 years of age (57.2 %; n = 115), although the distribution is significantly skewed to the right; the mean age for all respondents is 35.2 years.
Eighty-three percent (n = 168) of respondents were American Board of Genetic Counseling (ABGC) certified at the time they completed the survey, and, of those who live in states that license genetic counselors, 81.1 % (n = 60) were licensed. Respondents were fairly well distributed among the six NSGC defined practice regions. The majority of respondents had been practicing for less than 10 years (60.3 %; n = 123) with a mean of 9.1 years. The vast majority of respondents represented four categories of practice settings: university medical center (33.8 %; n = 69), public hospital/medical facility (22.1 %; n = 45), private hospital/medical facility (21.2 %; n = 43), and physician’s private office (15.2 %; n = 31).
Eighty-five percent (n = 174) of respondents indicated that prenatal counseling was their primary area of specialty. The second largest response group was “other” where respondents described their specialty as a combination of prenatal and another area(s) (8.3 %; n = 17). Seventy-three percent (n = 149) of respondents indicated that they see an average of 5–19 prenatal patients per week, with a mean of 13.4 patients per week for all respondents.
Genetic Counselor Experiences Offering Testing
This portion of the survey explored counselors’ self-reported experiences offering cffDNA testing. Respondents were asked to choose the most appropriate answer(s) from multiple choices; several questions allowed respondents to select multiple answer choices. Qualitative questions were used to follow up select quantitative questions. Quantitative data for this section can be found in Table 2.
Institutional Decisions
As show in Table 2, of 236 respondents, 95.3 % (n = 224) indicated that their institution had made a decision whether or not to offer cell-free fetal DNA (cffDNA) testing for aneuploidy to patients. Ninety percent (n = 211) were offering cffDNA testing, while approximately 5.0 % (n = 11) responded that their institution decided not to offer cffDNA testing at this time. Seventy-nine counselors cited a number of reasons for their institution’s decision regarding offering cffDNA testing. Common themes (present in ≥10 % of responses) included: 1) All testing options should be made available to patients (26.6 %; n = 21); 2) CffDNA testing is a good alternative to invasive testing (24.1 %; n = 19); 3) Patient demand for cffDNA testing (21.5 %; n = 17); 4) Good data/technology to support the testing (19.0 %; n = 15); 5) CffDNA testing is “better” than other screening options (13.9 %; n = 11); 6) CffDNA testing is an option for high risk patients (12.7 %; n = 10); and 7) Need to stay competitive (11.4 %; n = 9). Further delineation of themes and illustrative examples can be found in Table 3.
Choice of Test/Lab
When asked to identify which lab(s) their institution used (multiple answers were allowed), 66.4 % (n = 154) chose Company X1’s testing in comparison to 43.1 % (n = 100) using Company X2 and 38.4 % (n = 89) using Company X3 as shown in Table 2.
When considering billing, 8.2 % (n = 19) and 37.8 % (n = 88) of counselors felt that it was the main factor, or strongly influenced their institution’s choice of laboratory, respectively. An additional 17.6 % (n = 41) felt it moderately influenced the choice of lab. Approximately 16.3 % (n = 38) and 15.5 % (n = 36) reported billing considerations impacted lab choice to some degree, or little to none, respectively. A wide variety of influencing factors for lab choice were reported (n = 193), including: 1) Insurance and billing (55.4 %; n = 107); 2) Good data/technology to support the testing (28.0 %; n = 54); 3) Result format/reporting process (24.4 %; n = 47); 4) First cffDNA test available (21.2 %; n = 41); 5) Clinical indications accepted (21.2 %; n = 41); 6) Customer service (15.0 %; n = 29); and 7) Logistics (10.4 %; n = 20). Further delineation of themes and illustrative examples can be found in Table 4.
Offering and Ordering Testing
At the time they were surveyed, 91.4 % (n = 213) of respondents had experienced offering cffDNA testing to a patient, and over half had been offering the test for at least 6 months (59.7 %; n = 126) (see Table 2). Seventy-six percent (n = 159) of respondents indicated that they order between one and five cffDNA tests per week.
When counselors were asked to whom do they offer cffDNA testing, 88.2 % (n = 202) responded that they only offer this testing to high risk patients in comparison to 3.9 % (n = 9) who offer cffDNA testing to all prenatal patients. When asked to define “high risk,” counselors provided answers including: 1) Abnormal maternal serum screen (88.9 %; n = 177); 2) Advanced maternal age (88.4 %; n = 176); 3) Abnormal ultrasound (86.4 %; n = 172); and 4) Positive history (60.8 %; n = 121) (see Table 5).
Insurance Considerations
When asked their personal experiences, although the majority of counselors felt that insurance considerations did not restrict the frequency with which they offered cffDNA testing (68.7 %; n = 158), 25.7 % of respondents (n = 59) felt that it did impact their ability to offer testing to patients (see Table 2). Forty-three percent (n = 98) of counselors indicated that they did not expect insurance coverage of cffDNA testing for the majority of their patients. However, 38.9 % (n = 88) felt cost or insurance coverage considerations only caused patients to decline cffDNA testing “occasionally” (1–25 % of the time). Twenty-eight percent (n = 62) felt their patients decline cffDNA testing due to cost or insurance coverage considerations greater than 50 % of the time.
Other Testing Options
When offering cffDNA testing to high risk patients in the first trimester, counselors most often offer chorionic villi sampling (CVS) (85.3 %; n = 198), amniocentesis (73.3 %; n = 170), and the first trimester screen (68.1 %; n = 158) as additional options. In the second trimester, amniocentesis (87.6 %; n = 204), extensive ultrasound (82.8 %; n = 193), and a quad screen (64.4 %; n = 150) were the most common concurrent options presented to high risk patients (see Table 2).
When asked if patients are given the option of choosing both maternal serum screening (e.g. sequential screening, quad screen) and cell-free fetal DNA testing at the same time, respondents were almost equally split: 47.2 % (n = 110) responded “No,” while 45.9 % (n = 107) responded “Yes.” However, when asked if patients are given the option of choosing a nuchal translucency ultrasound only (without blood work) and cffDNA testing at the same time, 65.1 % (n = 151) of counselors responded “Yes,” and only 27.6 % (n = 64) responded “No.”
Genetic Counselor Perceptions of Patient Choices and Attitudes
Counselors were asked to report on their observations of patient choices and perceptions of patient attitudes with regard to cffDNA testing. Respondents were asked to choose the most appropriate answer from multiple choices; only one answer choice per question was allowed. Additional questions allowed respondents to indicate their opinion regarding a number of statements (using a seven point Likert scale: Strongly disagree, Disagree, Slightly disagree, Neutral, Slightly agree, Agree, Strongly agree). One question asked counselors to rank multiple answer choices by entering a quantitative response. Quantitative data from this section can be found in Table 6.
Patients’ Choice of Test
The majority of respondents (55.2 %; n = 116) indicated that greater than 50 % of patients choose to pursue cffDNA testing when it is offered, and when patients choose an alternative testing option, it is more often a different screening test (66.8 %; n = 147). Counselors felt the most common reason patients choose cffDNA testing is that it is a non-invasive test (78.1 %; n = 164). High detection rates were the next most commonly chosen reason at 16.7 % (n = 35), and several counselors cited the combination of cffDNA testing’s non-invasive nature and high-detection rates as its appeal to patients (n = 7). One counselor commented: “[Patients] want [the] highest detection rates they can get with the least invasive testing.”
Patients’ Use of cffDNA Testing
When asked, “In your opinion, patients often use cffDNA testing for making a diagnosis,” 74.8 % (n = 151) of respondents chose some gradation of agree (Slightly agree, Agree, or Strongly agree). An even larger percentage, 86.6 % (n = 175), agreed with the statement “In your opinion, patients often use cffDNA testing for ruling out chromosome abnormalities.” Furthermore, 75.7 % (n = 153) of counselors chose some gradation of agree to the statement “In your opinion, patients often use cffDNA testing for adjusting risk of chromosome abnormalities.”
Patient Knowledge and Sources of Information About cffDNA Testing
The majority of counselors reported that their patients had heard about cffDNA testing from another source prior to counseling less than 50 % of the time (85.4 %; n = 182). Their most common sources of information were their obstetrician/gynecologist (OB/GYN) (n = 137), the internet (n = 118), and friends and family (n = 69). Even after genetic counseling, 45.1 % (n = 92) of counselors indicated patient perceptions of their OB/GYN’s preference or instructions caused them to decline cffDNA testing “occasionally” (1–25 % of the time). Twenty-six percent (n = 52) reported it caused patients to decline more frequently. Similarly, 49.5 % (n = 102) of respondents indicated patients decline cffDNA testing occasionally (1–25 % of the time) because it is “too new,” with 19.4 % (n = 40) of respondents reporting the test’s newness causes patients to decline more frequently.
Test Results
Respondents were asked to estimate frequencies of test results and enter a discrete quantitative answer. Data from this section can be found in Tables 7.
Test Failures
Forty- two percent (n = 79) of respondents indicated that, in their experience, cffDNA testing for aneuploidy fails 1 % or less of the time. Eighty-nine percent (n = 168) indicated that cffDNA testing fails 5 % or less of the time, and 96.8 % (n = 183) indicated that cffDNA testing fails 10 % or less of the time.
Abnormal Results
Thirty-seven percent (n = 68) of respondents indicated that their patients that choose cffDNA testing receive an abnormal/high risk/positive test result 1 % or less of the time. Seventy-eight percent (n = 143) indicated that their patients receive an abnormal result 5 % or less of the time, and 94.0 % (n = 172) indicated that they receive an abnormal result 10 % or less of the time.
Confirmatory Testing
Forty-four percent (n = 78) of respondents reported that 90–100 % of their patients who receive an abnormal/high risk/positive test result choose additional diagnostic testing. Twenty-seven percent (n = 47) of respondents reported that 50–75 % of their patients choose additional diagnostic testing. Interestingly, 15.8 % (n = 28) of respondents have never had patients choose additional diagnostic testing after an abnormal cffDNA test result. Forty-two percent (n = 69) reported that, for those patients who do choose additional diagnostic testing, their abnormal cffDNA test result is confirmed 100 % of the time. Sixty percent (n = 97) of respondents reported abnormal cffDNA test results are confirmed at least 99 % of the time, and 74.2 % (n = 121) of respondents reported confirmation at least 95 % of the time.
Counselor Opinions
This portion of the survey asked counselors to indicate their opinion regarding a number of statements using a seven point Likert scale (Strongly disagree, Disagree, Slightly disagree, Neutral, Slightly agree, Agree, Strongly agree). Data from this section can be found in Table 8.
Genetic Counselor Confidence in and Knowledge of cffDNA Testing
When asked their opinion on the statement “Cell-free fetal DNA testing is accurate and well validated,” a total of 93.7 % (n = 194) of counselors chose some gradation of agree (either “Slightly agree,” “Agree,” or “Strongly agree”). However, 87.0 % (n = 180) of counselors chose some gradation of agree for the statement “CffDNA testing needs further validation.”
A total of 96.1 % (n = 199) of counselors chose some gradation of agree to the statement “I feel knowledgeable about cffDNA testing.” Similarly, a total of 94.2 % (n = 195) of counselors chose some gradation of agree to the statement “I feel confident offering cffDNA to patients.” Lastly, 93.2 % (n = 191) of counselors chose some gradation of agree to the statement “I feel confident explaining how cffDNA testing is performed”, with 35.3 % (n = 73) choosing “Strongly agree.”
CffDNA Versus Other Testing Options
A total of 77.8 % (n = 161) of counselors chose some gradation of agree for the statement “I feel cffDNA testing is a good alternative to invasive testing,” although only 13.5 % (n = 28) chose “Strongly agree.” When asked their opinion about the statement “I believe cffDNA testing will largely replace invasive testing,” counselors were more divided, with the largest response group being “Slightly agree” (28.0 %, n = 58) and the second largest response group being “Disagree” (20.3 %, n = 42). However, the vast majority of counselors, 89.4 % (n = 185) chose some gradation of agree to the statement “I believe cffDNA testing will largely replace other screening testing.” There was a wide spread of counselor responses to “Our institution has seen the number of invasive diagnostic tests being ordered decrease since the advent of cffDNA testing.” The largest response group was “Agree” with 29.8 % (n = 61) of respondents choosing this answer. In contrast, the largest response group to “Our institution has seen the number of screening tests being ordered fall since the advent of cffDNA testing” was “Disagree” with 29.1 % (n = 60).
Presentation and Use of cffDNA Testing
When asked their opinion regarding the statement “I believe cffDNA testing should be presented as a diagnostic test, 87.9 % (n = 182) chose some gradation of disagree, with 55.6 % (n = 115) choosing “Strongly disagree.” Interestingly, an appreciable percentage of counselors chose some gradation of agree (8.2 %; n = 17), including “Strongly agree.” When asked their opinion about the statement “In your opinion, cffDNA testing should be used for making a diagnosis,” 74.9 % (n = 155) of counselors chose some gradation of disagree, with the largest group choosing “Strongly disagree.” However, over one fifth of respondents (21.3 %; n = 44) chose some gradation of agree, with four counselors choosing “Strongly agree.” Similarly, for the statement “In your opinion, cffDNA testing should be used for ruling out chromosome abnormalities,” the majority chose some gradation of disagree at 60.1 % (n = 125), but over one third (35.6 %; n = 74) chose some gradation of agree, with six counselors choosing “Strongly agree.” Lastly, when asked their opinion of the statement “In your opinion, cffDNA testing should be used for adjusting the risk of chromosome abnormalities,” counselors were more united with 89.4 % (n = 186) choosing some gradation of agree.
Pre- and Post-Test Counseling
Ninety-eight percent of counselors (n = 164) chose some gradation of agree for the statement “Pretest counseling is necessary for cffDNA testing,” with 79.2 % choosing “Strongly agree.” Similarly, 92.3 % (n = 191) of counselors chose some gradation of agree for the statement “The physicians I work with believe patients should have genetic counseling before offering cffDNA testing,” with 53.1 % (n = 110) choosing “Strongly agree.” Respondents were quite divided, however, regarding the statement “Pretest counseling for cffDNA testing could be administered by a health professional other than a genetic counselor equally well.” Most respondents (63.1 %; n = 120) disagreed with this statement to some extent. However, a majority of counselors gave less committal answers of “Slightly disagree,” “Neutral,” or “Slightly agree” and represented 51.5 % (n = 106) of respondents. Interestingly, when asked their opinion about the statement, “I am confident that patients get appropriate post-test counseling from other medical professionals when cffDNA testing is ordered without genetic counseling,” 87.7 % (n = 179) chose some gradation of disagree.
The majority of counselors had not counseled a high risk patient who had already received cffDNA testing through another office (PCP, OB/GYN, etc.) (59.2 %; n = 125). However, 35.1 % (n = 74) indicated that those patients (who have already had cffDNA testing) comprise up to 10 % of the high risk patients that they counsel.
Additional Thoughts Regarding cffDNA Testing
Genetic counselors were given the opportunity to express any additional comments they had regarding cffDNA testing in a free-text response question (limited to 1000 characters). Seventy-four counselors (31.4 %) entered qualitative responses, which were analyzed as described in the “Methods” section. Numerous themes and sub-themes relative to cffDNA testing emerged, including: 1) Limited experience with cffDNA testing (34.7 %; n = 25); 2) Use of cffDNA testing as an alternative to, not a substitute for, diagnostic testing, (26.4 %; n = 19); 3) Test failure rate and false positive and negative results (18.1 %; n = 13); 4) Use of cffDNA testing as an additional screening option (15.3 %; n = 11); 5) CffDNA testing as a source of optimism/excitement for prenatal counselors (13.9 %; n = 10); 6) A requirement for counseling (13.9 %; n = 10); 7) The impact of obstetricians on patient choices (12.5 %; n = 9); 8) Concerns regarding insurance/billing (11.1 %; n = 8); and 9) Use of cffDNA testing as a good option for patients who wish to avoid invasive procedures (11.1 %; n = 8). Further delineation of themes and illustrative examples can be found in Table 9.
Discussion
This study was developed to address the paucity of information regarding the implementation of cffDNA testing as a screening tool for aneuploidy. Prenatal genetic counselors were questioned regarding their personal experience, opinions, thoughts and concerns regarding the use of this new technology.
Genetic Counselor Personal Experiences and Opinions Regarding Offering Testing
The most common theme in respondents’ explanations of institutional decisions whether or not to offer cffDNA testing was, “All testing options should be made available to patients.” Although counselors elaborated about several considerations when discussing their choice of lab, particularly insurance and billing practices, it seems that despite the inconveniences, counselors value the equity of making all testing options available to their patients. On a more practical note, many counselors discussed the need to stay competitive with other institutions and patient and physician demand for cffDNA testing as factors that led to offering this testing at their institutions.
Although most counselors indicated that they offer testing to high risk patients only, respondents’ definitions of “high risk” revealed that a number of counselors include unique clinical indications beyond the highly recognized four: abnormal maternal serum screen, advanced maternal age, abnormal ultrasound and positive history. For example, some counselors included patients who are not eligible for CVS or amniocentesis, IVF patients, HIV positive patients, or even any patients that express interest in cffDNA testing or were referred for it.
Lastly, many counselors commented on the continuing value of information gleaned from other screening tests. For example, as presented by McPherson et al. (2011), second trimester maternal serum screens can provide information with pregnancy management implications outside of trisomy 21, trisomy 18 and open neural tube defects. They were able to identify pregnancies at an increased risk for other birth defects, placental insufficiency, intra-uterine growth restriction, and pregnancy loss using abnormal analyte levels (McPherson et al. 2011). However, while the majority of counselors gave their patients the option of choosing a nuchal translucency ultrasound and cffDNA testing at the same time, fewer offered maternal serum screening and cffDNA testing as simultaneously ordered tests. It is conceivable that counselors may avoid ordering maternal serum screening and cffDNA simultaneously because of the possibility that the two screening tests may give widely different results for the same conditions. With regard to ordering a nuchal translucency (NT) ultrasound and cffDNA testing at the same time, it is possible that the immediacy of information returned from a NT ultrasound, which allows patients the opportunity to choose an elective diagnostic procedure in the event of a large NT measurement, generally outweighs the concern for conflicting results.
Genetic Counselor Perceptions of Patient Attitudes
The majority of respondents indicated that greater than 50 % of patients choose to pursue cffDNA testing when it is offered, and when they choose an alternative testing option, it is more often another type of screening test, suggesting that patients are using cffDNA testing as an alternative to invasive diagnostic testing much like other screening options. However, counselors also reported that they have seen a decrease in the number of diagnostic tests ordered since offering cffDNA testing, rather than a drop in other screening tests. This could suggest that the difference in specificity between cffDNA testing (which only assesses trisomy 13,18 and 21) and serum screening, rather than sensitivity, is responsible for the decline in the number of diagnostic tests being ordered. As cffDNA testing returns far more negative test results than serum screening, it results in far fewer indications for invasive testing. Alternatively, however, is the possibility that while patients may be choosing cffDNA testing due to its non-invasive nature, they are often satisfied with its high detection rate and do not proceed to a diagnostic test. Many counselors seem to agree; the majority of respondents indicated that patients often use cffDNA testing for making a diagnosis or ruling out chromosome abnormalities despite the fact that it is not a diagnostic test and does not analyze all chromosomes or all possible chromosomal anomalies.
Prenatal karyotype through amniocentesis or CVS is currently the gold standard, providing information on the full complement of fetal (or placental) chromosomes from the pregnancy. Prenatal microarray has recently been shown to reveal clinically relevant information in an additional “1.7 % of pregnancies with standard indications for prenatal diagnosis (such as advanced maternal age and positive aneuploidy screening result) and in 6.0 % of cases with an anomaly on ultrasonography” (Wapner et al. 2012, p. 2181). At a time when the diagnostic standard is perhaps being raised by a new technology, it is concerning that patients seem to be using screening test results (with much greater limitations) as diagnostic information.
Additionally, counselors must not only address with patients what information cffDNA testing does not provide, but also the possibility that the results returned are false. Recent concerns regarding false positive cffDNA testing results have surfaced, echoing respondents’ qualitative responses. Cases of low percentage mosaicism and confined placental mosaicism emphasize the importance of invasive diagnostic testing to confirm cffDNA test results before decision making (Hall et al. 2013; Mennuti et al. 2013; Taylor et al. 2013).
Genetic Counselor Experiences with Test Results
Although some counselors reported high rates of abnormal test results as well as test failures, many also commented that their experience ordering cffDNA testing at the time was too limited to provide accurate proportions. However, higher failure rates were also cited by some counselors as factors that influenced their choice of lab, indicating they have perhaps had enough experience with cffDNA testing to document a true difference between tests. Regardless of the choice of lab, genetic counselors will have to navigate, counsel about, and advocate for their patients with regard to rates of test failure in cffDNA testing uniquely from other screening tests, which rarely report failure to obtain a result (Benn et al. 2013).
Counselor Opinions Regarding cffDNA Testing
Respondents generally indicated that they support cffDNA testing as a good alternative to invasive testing and believe it has been well validated; however, many are still looking for further validation and research to solidify confidence in this technology. Research corroborating the currently reported data in other patient populations and in larger, independent cohorts may perhaps bestow that needed confidence. Although the majority of counselors indicated they believe cffDNA testing should be presented only as an advanced screening test (rather than a diagnostic option), an appreciable number of counselors indicated that cffDNA testing should be used for making a diagnosis (21.3 %) and ruling out chromosome abnormalities (35.6 %) in addition to its intended use for adjusting the risk of chromosome abnormalities, and that it should be presented as a diagnostic test (8.2 %). Overall, counselor responses implied that they were more comfortable accepting a negative cffDNA test as diagnostic than a positive one.
Insurance coverage, billing policies, reimbursement, and price of cffDNA testing surfaced multiple times as issues genetic counselors were concerned with in regard to offering cffDNA testing. In some cases difficulty with coverage caused counselors to use a different lab depending on patient insurance, or to switch labs entirely. Although the majority of respondents expected insurance coverage of cffDNA testing for most of their patients, many also reported that cost or lack of coverage caused patients to decline cffDNA testing. Consistent with our study, Vahanian et al. (2013) reported that patients with public insurance were 83 % less likely to choose to proceed with NIPT than patients with private insurance, suggesting unequal access due to insurance coverage and cost.
Counselors also raised concerns regarding the impact of obstetricians’ influence on patient decisions regarding cffDNA testing. Respondents indicated that OB/GYNs were patients’ most common source of information if they had already heard about cffDNA testing prior to counseling, and a substantial number felt that patient perceptions of their OB/GYN’s preferences or instructions caused patients to decline cffDNA testing even after counseling. Moreover, other counselors felt that OB/GYNs do not provide proper pre-test counseling to ensure informed consent when offering cffDNA directly to patients. Bensend et al. (2013) explored the perceived effects of patients receiving genetic information from non-genetic professionals, which included adverse psychosocial effects, inadequate genetic counseling, genetic testing and screening errors, and medical mismanagement. With high proportions of obstetricians planning to offer NIPT increasingly to not only high-risk patients but also “average-risk” women, the quality of pre-test counseling patients receive and the influence their providers have on their decisions regarding cffDNA testing will become even greater concerns (Musci et al. 2013). Norton et al. (2013) made a plea for restraint from so freely integrating cffDNA testing as a primary screening test so the education of patients and health care providers can keep pace with the rapid developments in this field.
Study Limitations
Due to the nature of the dissemination method used, the possible respondent pool was limited to genetic counselors who are current members of the National Society of Genetic Counselors. Additionally, as with any survey, those participants who were interested in the subject matter and in contributing their opinions are presumably those who chose to respond thus limiting generalizability of the findings. Validity of the quantitative data may have been limited by the self-report format used. The majority of respondents had 6 months or more of experience offering cffDNA testing; however, it is important to note that a small number (8 %) who were contributing their thoughts and opinions on cffDNA testing had not yet had the opportunity to offer it. Although every effort was made to ensure survey questions were formulated without bias, not all questions were presented with an inverse query, which may have inadvertently introduced bias or the appearance of bias into the survey-taking experience. Finally, this study is purely descriptive as no inferential statistics were conducted on the quantitative data. Therefore relationships among the participants’ responses could not be determined.
Practice Implications
Education of other providers, perhaps by genetic counselors, may help ensure that patients are receiving necessary pre-test counseling and giving informed consent, consistent with ACOG and NSGC guidelines. Additionally, as cffDNA testing becomes more ubiquitous, it is likely that insurance considerations will become a less prominent factor in offering and ordering testing for patients. In the meantime, working as an advocate for patients who do not expect sufficient coverage and explaining the medical benefit to insurance companies may allow genetic counselors to offer all testing options to all patients and push towards equity.
Research Recommendations
This research was designed as an initial study. Further investigation regarding the use of cffDNA testing without the involvement of a genetic counselor, as well as direct surveying of patients as to their understanding and use of cell-free fetal DNA testing, may help to provide a more complete picture of practice implications for genetic counselors. Additionally, a purely quantitative follow-up study investigating genetic counselors’ experience with cffDNA testing as new labs offer this testing and more patients are interested in pursuing it will help demonstrate how implementation is changing over time and point to what we may expect in the future.
Conclusions
Cell-free fetal DNA testing represents another step forward in the technological and scientific advancement of prenatal testing. To date, there has not been another screening test that provides a near diagnostic result for trisomy 21 and trisomy 18 without the risk of an invasive procedure. Genetic counselors will play a large role in defining how cell-free fetal DNA testing is incorporated into the prenatal clinical setting and therefore need to be comfortable and familiar with the various test options and their intended use. This study was designed as a preliminary investigation into counselors’ experiences with and implementation of cell-free fetal DNA testing and therefore conclusions must remain general. At this time, counselors seem to value this testing as a screening option but have voiced concern regarding how some obstetricians and patients currently make use of this testing or may use this testing in the future. By taking on the responsibility of educating other providers, patients, and the public with balanced information regarding cell-fee fetal DNA testing, genetic counselors may help decrease misconceptions regarding its intended use and capabilities.
Notes
Survey available upon request from the authors
References
American College of Obstetricians and Gynecologists. (2012). Noninvasive prenatal testing for fetal aneuploidy. Committee Opinion No. 545. Obstetrics and Gynecology, 120, 1532–1534.
Benn, P., Cuckle, H., & Pergament, E. (2013). Non-invasive prenatal testing for aneuploidy: current status and future prospects. Ultrasound in Obstetrics and Gynecology. doi:10.1002/uog.12513.
Bensend, T. A., Veach, P. M., & Niendorf, K. B. (2013). What’s the harm? Genetic counselor perceptions of adverse effects of genetics service provision by non-genetics professionals. Journal of Genetic Counseling. doi:10.1007/s10897-013-9605-3.
Bianchi, D. W., Platt, L. D., Goldberg, J. D., Abuhamad, A. Z., Sehnert, A. J., & Rava, R. P. (2012). Genome-wide fetal aneuploidy detection by maternal plasma DNA sequencing. MatErnal Blood Is Source to Accurately diagnose fetal aneuploidy (MELISSA) Study Group. Obstetrics and Gynecology, 119, 890–901.
Chen, E. Z., Chiu, R. W., SUN, H., Akolekar, R., Chan, K. C., Leung, T. Y., et al. (2011). Noninvasive prenatal diagnosis of fetal trisomy 18 and trisomy 13 by maternal plasma DNA sequencing. PLoS ONE, 6, e21791.
Chiu, R. W., Akolekar, R., Zheng, Y. W., LeungTY, S. H., Chan, K. C., et al. (2011). Non-invasive prenatal assessment of trisomy 21 by multiplexed maternal plasma DNA sequencing: large scale validation study. BMJ, 342, c7401.
Devers, P. L., Cronister, A., Ormond, K. E., Facio, F., Brasington, C. K., & Flodman, P. (2012). Noninvasive prenatal testing/noninvasive prenatal diagnosis: the position of the national society of genetic counselors. Journal of Genetic Counseling. doi:10.1007/s10897-012-9564-0.
Ehrich, M., Deciu, C., Zwiefelhofer, T., Tynan, J. A., Cagasan, L., Tim, R., et al. (2011). Noninvasive detection of fetal trisomy 21 by sequencing of DNA in maternal blood: a study in a clinical setting. American Journal of Obstetrics and Gynecology, 204, 205.e1–11.
Hall, A. L., Drendel, H. M., Verbrugge, J. L., Reese, A. M., Schumacher, K. L., Griffith, C. B., et al. (2013). Positive cell-free fetal DNA testing for trisomy 13 reveals confined placental mosaicism. Genetics in Medicine. doi:10.1038/gim.2013.26.
Lo, Y. M., Corbetta, N., Chamberlain, P. F., Rai, V., Sargent, I. L., Redman, C. W., et al. (1997). Presence of fetal DNA in maternal plasma and serum. Lancet, 350, 485–487.
McPherson, E., Thomas, G. D., Manlick, C., Zaleski, C. A., Reynolds, K. K., Rasmussen, K., et al. (2011). Extreme values of maternal serum analytes in second trimester screening: Looking beyond trisomy and NTD’s. Journal of Genetic Counseling, 20, 396–403.
Mennuti, M. T., Cherry, A. M., Morrissette, J. J., & Dugoff, L. (2013). Is it time to sound an alarm about false positive cell-free DNA testing for fetal aneuploidy? American Journal of Obstetrics and Gynecology. doi:10.1016/j.ajog.2013.03.027.
Musci, T. J., Fairbrother, G., Batey, A., Bruursema, J., Struble, C., & Song, K. (2013). Non-invasive prenatal testing with cell-free DNA: US physician attitudes toward implementation in clinical practice. Prenatal Diagnosis, 33(5), 424–428.
Norton, M. E., Brar, H., Meiss, J., Karimi, A., Laurent, L. C., Caughey, A. B., et al. (2012). Non-Invasive Chromosomal Evaluation (NICE) study: results of a multicenter, prospective, cohort study for detection of fetal trisomy 18. American Journal of Obstetrics and Gynecology, 207(2), 137.e1–137.e8.
Norton, M. E., Rose, N. C., & Benn, P. (2013). Noninvasive prenatal testing for fetal aneuploidy: clinical assessment and a plea for restraint. Obstetrics and Gynecology, 121(4), 847–850.
Palomaki, G. E., Kloza, E. M., Lambert-Messerlian, G. M., Haddow, J. E., Neveux, L. M., Ehrich, M., et al. (2011). DNA sequencing of maternal plasma to detect Down syndrome: an international clinical validation study. Genetics in Medicine, 13, 913–920.
Palomaki, G. E., Deciu, C., Kloza, E. M., Lambert-Messerlian, G. M., Haddow, J. E., Neveux, L. M., et al. (2012). DNA sequencing of maternal plasma reliably identifies trisomy 18 and trisomy 13 as well as Down syndrome: an international collaborative study. Genetics in Medicine, 14, 296–305.
Patton, M. Q. (2001). Qualitative evaluation and research methods. Thousand Oaks: Sage.
Sayres, L., Allyse, M., Norton, M., & Cho, M. (2011). Cell-free fetal DNA testing: A pilot study of obstetric healthcare provider attitudes towards clinical implementation. Prenatal Diagnosis, 31(11), 1070–1076.
Sparks, A. B., Wang, E. T., Struble, C. A., Barrett, W., Stolowski, R., McBride, C., et al. (2012). Selective analysis of cell-free DNA in maternal blood for evaluation of fetal trisomy. Prenatal Diagnosis, 32, 3–9.
Taylor, J.B., Chock, V.Y., Hudgins, L. (2013). NIPT in a clinical setting: an analysis of uptake in the first months of clinical availability. Journal of Genetic Counseling [Epub ahead of print].
Vahanian, S.A., Baraa, A.M., Yeh, C., Chavez, M.R., Kinzler, W.L., Vintzileos, A.M. (2013). Patient acceptance of non-invasive testing for fetal aneuploidy via cell-free fetal DNA. Journal of Maternal-Fetal and Neonatal Medicine. PMID: 23687914.
Wapner, R. J., Martin, C. L., Levy, B., Ballif, B. C., Eng, C. M., Zachary, J. M., et al. (2012). Chromosomal microarray versus karyotyping for prenatal diagnosis. The New England Journal of Medicine, 367(23), 2175–2184.
Wright, C. F., & Burton, H. (2009). The use of cell-free fetal nucleic acids in maternal blood for non-invasive prenatal diagnosis. Human Reproduction Update, 15(1), 139–151.
Acknowledgments
This study was completed in partial fulfillment of the requirements for the first author’s Master of Science degree. The authors would like to thank the respondents for their insightful comments.
Conflict of Interest
Authors Julie M. H. Horsting, Stephen R. Dlouhy, Katelyn Hanson, Kimberly Quaid, Shaochun Bai, and Karrie A. Hines declare they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horsting, J.M.H., Dlouhy, S.R., Hanson, K. et al. Genetic Counselors’ Experience with Cell-Free Fetal DNA Testing as a Prenatal Screening Option for Aneuploidy. J Genet Counsel 23, 377–400 (2014). https://doi.org/10.1007/s10897-013-9673-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-013-9673-4