Abstract
Historically, physicians have expressed concern about their patients’ risk of genetic discrimination, which has acted as a barrier to uptake of genetic services. The Genetic Information Nondiscrimination Act of 2008 (GINA) is intended to protect patients against employer and health insurance discrimination. Physicians’ awareness and knowledge of GINA has yet to be evaluated. In 2009, we mailed surveys to 1500 randomly selected members of the American Academy of Family Physicians. Questions measured physicians’ current knowledge of GINA and their level of concern for genetic discrimination. In total, 401 physicians completed the survey (response rate 26.9%). Approximately half (54.5%) of physicians had no awareness of GINA. Of physicians who reported basic knowledge of GINA, the majority were aware of the protections offered for group health insurance (92.7%), private health insurance (82.9%), and employment (70.7%). Fewer physicians were aware of GINA’s limitations regarding life insurance (53.7%) and long-term care insurance (58.8%). Physicians demonstrated highest levels of concern for health insurance, life insurance, and long-term care insurance discrimination, with less concern for employer and family/social discrimination. Level of concern for the risk of genetic discrimination did not correlate significantly with awareness of GINA. Approximately 17 months after GINA was signed into federal law, physicians’ knowledge remained limited regarding the existence of this legislation and relevant details. Physicians who are aware of GINA continue to have significant concerns regarding the risk of genetic discrimination. This study reveals the need to further educate physicians about the existence of GINA and the protections offered.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Historically, genetic information has been regarded as fundamentally different from other medical information. In part, this perception results from physicians’ concerns about patients’ risk of genetic discrimination (Farndon 2006; Lowstuter et al. 2008; Reilly 1999). Patients (Billings et al. 1992; Hall et al. 2005; Hall and Rich 2000; Lapham et al. 1996) and healthcare providers (Matloff et al. 2000; Nedelcu et al. 2004; Pfeffer et al. 2003) have expressed concerns about genetic discrimination in several contexts including employment, health insurance, and life insurance. In 1992, evidence for genetic discrimination was found in several social institutions for asymptomatic individuals carrying a genetic diagnosis, especially in the health and life insurance industries (Billings et al. 1992). Physicians and nurses surveyed in 2004 had substantial concerns about patients’ risk of genetic discrimination (Nedelcu et al. 2004). Concerns among clinical genetics professionals have decreased, possibly due to awareness of various state and federal laws (Huizenga et al. 2009) or because predictions of widespread genetic discrimination failed to materialize (Stephenson 1999). However, since the recent enactment of cohesive federal legislation, physicians’ concerns about genetic discrimination have not been reported.
Following 13 years of debate in Congress, the Genetic Information Nondiscrimination Act of 2008 (GINA) was enacted with nearly unanimous support (Table 1). GINA addresses the risk of genetic discrimination related to health insurance and employment (Health law 2009), and thus it may assuage patients’ and physicians’ concerns and reduce barriers to referral and uptake of genetic services (Leib et al. 2008; Lowstuter et al. 2008). GINA prohibits a health insurer or employer from discriminating against an individual based on the individual’s genetic risk for future disease and prohibits them from requesting or requiring an individual to undergo a genetic test. Health insurers cannot set eligibility, premiums, or contribution amounts based on genetic test results. Employers cannot base hiring, firing, job assignments, or other terms of employment on genetic test results. In contrast to most previously existing state legislation, GINA also includes family history as genetic information (Hudson et al. 2008) defined as dependents and up to and including 4th degree relatives (Domchek et al. 2010).
Even supporters of GINA concede its shortcomings (Hudson et al. 2008); in particular it is not applicable to life insurance, disability insurance, or long-term care insurance (Rothstein 2008). GINA applies to individuals with a predisposition (genetic tendency) for a disease, but does not apply to individuals with actual manifestation of a disease or condition. An employer may, after conditional offer of employment, lawfully require an individual to disclose all of his or her health records under the Americans with Disabilities Act (Rothstein 2008). Despite these limitations, GINA appears to lessen the risk of misuse of genetic information, and may encourage people to take advantage of genetic technologies (Erwin 2009).
Purpose of the Present Study
We reasoned that physicians who are aware of GINA and its provisions might have less concern for genetic discrimination than those who are unaware and/or less knowledgeable of GINA. We investigated physicians’ awareness and knowledge of GINA in January 2010, approximately seven months after it went into effect for health insurance (May, 2009) and one month after it went into effect for employment (November, 2009).
Methods
Participants and Procedures
All research activities took place at Northwestern University following Institutional Review Board approval. Three thousand addresses for members of the American Academy of Family Physicians (AAFP) reporting direct patient care were purchased from InFocus, a list management and brokerage service company. InFocus sorts by zip code, then applies random select script to the ratio of addresses ordered to total addresses for random list creation. A cover letter inviting participation was sent to the first 1500 U.S. addresses provided in addition to a paper survey and self-addressed stamped return envelope. Addresses were reviewed to ensure that an array of states were covered. Participants could complete and return the enclosed survey by mail or complete an online version through Surveymonkey.
Surveys were mailed on December 30, 2009 followed by a reminder postcard on January 13, 2010. The last date of eligibility was January 25, 2010. Following survey completion, participants could enroll in a raffle for one of five $50 amazon.com gift cards through a separate Surveymonkey web link where they could provide contact information. This approach ensured anonymity by separating survey responses and identifiers.
Instrumentation: Survey
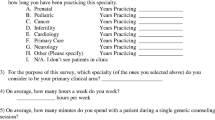
The survey measured awareness and knowledge of GINA, concerns regarding genetic discrimination, preferences for documenting genetic information in an electronic health record (to be reported separately) and basic demographics. This survey was previously used in 2008, to evaluate physicians’ concerns for patients’ risk of genetic discrimination as well as their preferences for how to document genetic information within the electronic health record system at NorthShore University HealthSystem. We modified the 2008 survey to be applicable to a broad, nationwide physician population.
Physicians’ knowledge and awareness were subjectively measured by asking them to choose a category they most closely fit within: 1) no prior awareness of GINA (“no awareness” group); 2) aware of GINA, but lack of knowledge about the specific protections provided (“limited knowledge” group); and 3) aware of GINA and a basic understanding of the Act (“basic knowledge” group). Physicians’ objective knowledge was measured among those in the self-described “limited knowledge” or “basic knowledge” groups. These individuals were queried about whether GINA offered protection against five types of genetic discrimination (health insurance, private health insurance, life insurance, long-term care insurance, and employment). A completely correct answer would specify that GINA protects against group health insurance, private health insurance, and employer discrimination, but not against life insurance or long-term care insurance discrimination. The survey did not address GINA’s lack of protection against disability insurance discrimination.
In order to assess physicians’ level of concern for genetic discrimination, they were asked to review potential forms of discrimination (health insurance, life insurance, long-term care insurance, employment, family/social) and then choose their perceived degree of concern for their patients’ risk: not concerned, slightly concerned, moderately concerned, or highly concerned.
An open comment section was used to capture thoughts and comments of the respondents possibly not addressed in the survey. Physicians were asked to provide additional comments/insights regarding storage of genetic information in the electronic health records (to be reported separately) or comments/insights related to GINA.
Data Analysis
All returned surveys (including partially completed surveys) were included in the analysis. Combined analysis of paper and online survey responses was performed using SPSS for Windows (Version 18.0). Descriptive statistics were computed to describe participant demographics and answer frequencies. Quantitative comparisons between groups were completed using chi-square analyses. Physicians’ knowledge distribution of GINA protection was assessed using Mann–Whitney and Kruskal-Wallis analyses. A p-value of <.05 was considered statistically significant. Themes were created from the free comments section by the primary investigator.
Results
Sample Characteristics
Of the 1,500 mailed surveys, eight were returned to sender. A total of 401 surveys were returned by the given deadline, for a response rate of 26.9% (401/1492). The majority (n = 323, 80.5%) of surveys were returned via postage mailing with the remainder (n = 78, 19.5%) completed via internet link. Six surveys were received after the final collection date and were not included in the analyses or response rate. The demographics of both the entire AAFP population and the random sample of AAFP physicians are unknown. For responding physicians, most were male (67.2%), primary care/family medicine physicians (96.2%) with over 15 years of experience in medical practice (70.4%) (Table 2). Several physicians (3.8%) reported that they practice outside of primary care, such as emergency medicine, occupational medicine, and hospice care. Several participants (10.6%) indicated a medical practice other than those listed, such as the military, free clinics, or community centers.
GINA Knowledge and Discrimination Concerns
More than half (n = 217, 54.5%) of physicians indicated they had no prior awareness of GINA (“no awareness” group), 35.2% (n = 140) were aware of GINA, but did not know the specific protections provided (“limited knowledge” group), and 10.3% (n = 41)were aware of GINA and claimed a basic understanding (“basic knowledge” group). Overall, physicians who self-reported awareness of GINA with either limited knowledge or basic knowledge responded correctly more often than incorrectly about GINA’s coverage for the five types of genetic discrimination (Fig. 1).
Physicians with limited knowledge of GINA were compared to physicians with basic knowledge of GINA to determine differences in the rate of correct responses regarding GINA’s protection for each type of genetic discrimination. No statistically significant differences were found in the rate of correct responses for private health insurance, life insurance, long-term care insurance, or employment. However, physicians with basic GINA knowledge were significantly more likely to know about GINA’s protections for group health insurance compared to physicians with limited GINA knowledge (Fisher’s exact test, p < .001; 92.7% vs. 60%).
Among all surveyed physicians, the most common response for level of concern for discrimination was “highly concerned” in areas of life insurance (49.6%), health insurance (44.0%), and long term care insurance (41.9%) discrimination. The most common response was “slightly concerned” in the areas of family/social (37.1%) and employer (28.8%) discrimination. Two physicians were highly concerned about an “other” kind of discrimination stated as, “children,” and “death panels.”
We compared physicians’ awareness of GINA (no awareness group versus the limited and basic knowledge groups, combined) to evaluate whether there were differences in physicians’ level of concern (low versus high) for each type of genetic discrimination. Physicians who were either not concerned or slightly concerned for a type of discrimination were grouped together as “low concern” and physicians who were either moderately concerned or highly concerned for a type of discrimination were grouped together as “high concern” (Fig. 2). Regardless of physicians’ awareness of GINA, no statistically significant differences were found in the level of discrimination concern for any of the five forms of genetic discrimination
For physicians reporting awareness of GINA, distributions of objective knowledge scores (ranging from zero to five correct responses) were compared between physicians with low versus high concern about genetic discrimination in the five domains using the Mann–Whitney test. No significant differences in distribution of knowledge scores were observed between these two groups of physicians for health insurance, life insurance, long term insurance, employment, or family/social discrimination.
Physicians who self-reported basic GINA knowledge had significantly higher objective knowledge scores compared to physicians who self-reported limited GINA knowledge (Mann–Whitney, p = .031). Physicians who reported 6 to 10 years of experience had significantly higher objective knowledge scores compared to those with other years of experience (0–5, 6–10, 11–15, and >15) (Kruskal-Wallis, p = .036). Finally, physicians who refer patients to a genetics specialist annually (1–10 or 11–20 per year) had significantly higher objective knowledge compared to physicians who never referred patients to genetics specialists (Kruskal-Wallis, p = .033).
Review of additional comments provided by participants revealed several themes including continued concerns about insurance discrimination, the costs of genetic counseling and testing, and the need for more physician knowledge about GINA (Table 3).
Discussion
Genetic testing for inherited predisposition is clinically available for nearly 2071 diseases (“Gene Tests Database 2009,” 1993–2010) and in certain instances can significantly reduce morbidity and mortality (Domchek et al. 2010). However, physicians’ concern for a patient’s risk of genetic discrimination can act as a barrier to referring patients to genetics centers (Lowstuter et al. 2008). The recently enacted Genetic Information Nondiscrimination Act (GINA) may help allay these concerns and provide clearer protections than the patchwork of state regulations already in effect (Genetic Information: Legal Issues Relating to Discrimination and Privacy 2010). We surveyed a national sample of family physicians to assess their awareness and knowledge of the new federal legislation and whether they have persistent concerns for genetic discrimination.
Although GINA was prominently featured by the news media as well as leading medical journals (Hudson et al. 2008), about half (54.5%) of the present sample reported no awareness of GINA. Only 10.3% of respondents self-reported basic knowledge of GINA, and less than half (43.9%) of physicians who were aware of GINA were completely correct about the types of protections that GINA offers. Knowledge deficiencies about genetics among primary care physicians have long been recognized (Aalfs et al. 2003; Baars et al. 2005; Hayflick et al. 1998). While it is encouraging that almost half of the physicians had heard of GINA, this study illustrates the need to raise awareness of the Act and its specific protections. Physicians reporting basic knowledge were significantly more likely to respond correctly about GINA’s protections; however even in this group, specific elements of GINA were routinely misconstrued [e.g. protections against life insurance (46.3%) and long-term care insurance (41.5%) discrimination]. Furthermore, even those who reported basic knowledge had a similar level of misunderstanding about the employment aspect of GINA as compared with those who reported limited knowledge.
These results provide evidence that not only is there a need for knowledge dissemination among physicians about the existence of GINA, but that content should emphasize the applicability of GINA to employment discrimination and limitations in regards to life insurance and long-term care insurance. A fact sheet developed by the Department of Health and Human Services (“Genetic Information Nondiscrimination Act of 2008, Information for Researchers and Health Care Professionals” 2009) is a step in this direction, but dissemination of this information may not have been effective.
Although we anticipated that awareness of GINA would correlate with less concern about those areas of discrimination specifically protected by GINA, we found no evidence in this regard. Even physicians who reported basic knowledge of the legislation expressed doubts about its utility in written comments and they reported high levels of concern about patients’ risk of genetic discrimination. These findings suggest it may take time before awareness of GINA’s protections, coupled with evidence of its efficacy in practice, will allay physicians’ concerns. For instance, the first lawsuit under GINA has been made by a woman who alleges she was fired after she tested positive for a BRCA2 mutation and underwent prophylactic bilateral mastectomy (Associated Press, April 28, 2010).
Study Limitations and Research Recommendations
This study obtained a response rate (26.9%) comparable to other study of physicians nationwide. The majority were primary care or family medicine physicians and thus our results may provide a good representation of primary care physician’s opinions. Limitations of this study include selection bias and population skewing: physicians who have an interest in genetics, or those who are highly concerned about genetic discrimination or issues relating to documentation in the medical record, may have been much more inclined to complete the survey. Most participants had been practicing for more than 15 years, and therefore they may have received less information about genetics in their training.
These results are based on physicians’ opinions reported at a single point in time. Future research should re-evaluate this issue over time and survey other specialists, such as oncologists, gynecologists, and surgeons, who may have more experience with cancer genetic testing (where rates of genetic testing are high) and perhaps GINA. In addition, we surveyed physicians, but not patients. The public’s knowledge and opinions about GINA protection require evaluation and may provide information about the need for patient education.
Practice and Policy Implications
The passage of GINA is a ‘sentinel step’ in a process whereby society learns about genetic diversity and the value of knowing one’s genetic predisposition to disease, but is not a panacea for genetic discrimination (Billings 2008). Massive studies such as the 1000 Genomes Project make it clear that all human beings carry many genetic variants implicated in clear-cut genetic disorders, about 50–100 per individual (Durbin et al. 2010). The awakening of society to our common bond of genetic imperfection could promote greater tolerance as effectively as federal legislation.
Genetic tests have been available ‘direct-to-consumer’ without involvement of a physician (Kaphingst et al. 2010) and whole genome sequencing is commercially available at costs affordable to some consumers. Many individuals feel they have a right to learn their genetic information without hindrance of regulations such as the requirement for a doctor’s involvement. The challenge to physicians is to stay engaged with the explosion of genetic knowledge, including legislative and regulatory issues, in order to play a role in translating genomic information into improved health.
In summary, the results of this study reveal the need to continue to educate primary care physicians about the existence of GINA and about the specific protections offered. Genetic counselors can offer education in a concise and direct manor to primary care physicians. We encourage genetic counselors to act to disseminate information about GINA and general genetics to primary care physicians. Physician education is also a step towards disseminating information about GINA to patients. Raising awareness of the Act may help to address concerns related to genetic discrimination and allow the medical community to overcome this prevalent barrier toward use of genetic services.
References
Aalfs, C. M., Smets, E. M., de Haes, H. C., & Leschot, N. J. (2003). Referral for genetic counselling during pregnancy: limited alertness and awareness about genetic risk factors among GPs. Family Practice, 20(2), 135–141.
Associated Press (April 28, 2010). Conn. woman alleges genetic discrimination at work. Boston Herald.com. Retrieved from: https://doi.org/www.bostonherald.com/news/national/northeast/view/20100428conn_woman_alleges_genetic_discrimination_at_work/srvc=home&position=recent
Baars, M. J., Henneman, L., & Ten Kate, L. P. (2005). Deficiency of knowledge of genetics and genetic tests among general practitioners, gynecologists, and pediatricians: a global problem. Genetics in Medicine, 7(9), 605–610.
Baruch, S., & Hudson, K. (2008). Civilian and Military genetics: nondiscrimination policy in a post-GINA world. American Journal of Human Genetics, 83(4), 435–444.
Billings, P. R. (2008). Beyond GINA. Nature Medicine, 14(8), 806.
Billings, P. R., Kohn, M. A., de Cuevas, M., Beckwith, J., Alper, J. S., & Natowicz, M. R. (1992). Discrimination as a consequence of genetic testing. American Journal of Human Genetics, 50(3), 476–482.
Domchek, S. M., Friebel, T. M., Singer, C. F., Evans, D. G., Lynch, H. T., Isaacs, C., et al. (2010). Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA, 304(9), 967–975. Retrieved from: https://doi.org/www.ncbi.nlm.nih.gov/projects/GeneTests/static/whatsnew/labdirgrowth.shtml
Durbin, R. M., Abecasis, G. R., Altshuler, D. L., Auton, A., Brooks, L. D., Gibbs, R. A., et al. (2010). A map of human genome variation from population-scale sequencing. Nature, 467(7319), 1061–1073.
Erwin, C. (2009). Behind of Genetic Information Nondiscrimination Act of 2008. American Journal of Nursing, 109(12).
Farndon, P. A. (2006). Recording, using and sharing genetic information and test results: consent is the key in all medical specialties. Clinical Medicine, 6(3), 236–238.
Gene Tests Database 2009. (1993–2010). National Institues of Health 2010. Retrieved from https://doi.org/www.ncbi.nlm.nih.gov/projects/GeneTests/static/whatsnew/labdirgrowth.shtml.
Genetic Information: Legal Issues Relating to Discrimination and Privacy. (2010). Paper presented at the National Conference of State Legislatures. Retrieved from: https://doi.org/www.ncsl.org/default.aspx?tabid=14374.
Genetic Information Nondiscrimination Act of 2008, Information for Researchers and Health Care Professionals (2009). Retrieved from: https://doi.org/www.genome.gov/Pages/PolicyEthics/GeneticDiscrimination/GINAInfoDoc.pdf.
Hall, M. A., & Rich, S. S. (2000). Patients’ fear of genetic discrimination by health insurers: the impact of legal protections. Genetics in Medicine, 2(4), 214–221.
Hall, M. A., McEwen, J. E., Barton, J. C., Walker, A. P., Howe, E. G., Reiss, J. A., et al. (2005). Concerns in a primary care population about genetic discrimination by insurers. Genetics in Medicine, 7(5), 311–316.
Hayflick, S. J., Eiff, M. P., Carpenter, L., & Steinberger, J. (1998). Primary care physicians’ utilization and perceptions of genetics services. Genetics in Medicine, 1(1), 13–21.
Health law - genetics - Congress restricts use of genetic information by insurers and employers. - Genetic Information Nondiscrimination Act of 2008, Harvard Law Review, 122(3), 1038–1045.
Hudson, K. L., Holohan, M. K., & Collins, F. S. (2008). Keeping pace with the times–the Genetic Information Nondiscrimination Act of 2008. The New England Journal of Medicine, 358(25), 2661–2663.
Huizenga, C. R., Lowstuter, K., Banks, K. C., Lagos, V. I., Vandergon, V. O., & Weitzel, J. N. (2009). Evolving perspectives on genetic discrimination in health insurance among health care providers. Familial Cancer.
Kaphingst, K. A., McBride, C. M., Wade, C., Alford, S. H., Brody, L. C., & Baxevanis, A. D. (2010). Consumers’ use of web-based information and their decisions about multiplex genetic susceptibility testing. Journal of Medical Internet Research, 12(3), e41.
Lapham, E. V., Kozma, C., & Weiss, J. O. (1996). Genetic discrimination: perspectives of consumers. Science, 274(5287), 621–624.
Leib, J. R., Hoodfar, E., Haidle, J. L., & Nagy, R. (2008). The new genetic privacy law: How GINA will affect patients seeking counseling and testing for inherited cancer risk. Community Oncology, 5, 351–354.
Lowstuter, K. J., Sand, S., Blazer, K. R., MacDonald, D. J., Banks, K. C., Lee, C. A., et al. (2008). Influence of genetic discrimination perceptions and knowledge on cancer genetics referral practice among clinicians. Genetics in Medicine, 10(9), 691–698.
Matloff, E. T., Shappell, H., Brierley, K., Bernhardt, B. A., McKinnon, W., & Peshkin, B. N. (2000). What would you do? Specialists’ perspectives on cancer genetic testing, prophylactic surgery, and insurance discrimination. Journal of Clinical Oncology, 18(12), 2484–2492.
Nedelcu, R., Blazer, K. R., Schwerin, B. U., Gambol, P., Mantha, P., Uman, G. C., et al. (2004). Genetic discrimination: the clinician perspective. Clinical Genetics, 66(4), 311–317.
Pfeffer, N. L., Veach, P. M., & LeRoy, B. S. (2003). An investigation of genetic counselors’ discussion of genetic discrimination with cancer risk patients. Journal of Genetic Counseling, 12(5), 419–438.
Reilly, P. R. (1999). Efforts to regulate the collection and use of genetic information. Archives of Pathology & Laboratory Medicine, 123(11), 1066–1070.
Rothstein, M. A. (2008). Currents in contemporary ethics. GINA, the ADA, and genetic discrimination in employment. The Journal of Law, Medicine & Ethics, 36(4), 837–840.
Stephenson, J. (1999). Genetic test information fears unfounded. JAMA, 282(23), 2197–2198.
Author information
Authors and Affiliations
Corresponding author
Additional information
Support
Northwestern University Graduate Program of Genetic Counseling and Center for Medical Genetics, NorthShore University HealthSystem. This work was performed in partial fulfillment for a Master’s degree (ALL).
Prior Presentation
Family Practice Physicians’ Awareness and Knowledge of GINA. Platform presentation at the National Society of Genetic Counselors Annual Education Conference, October 17th, 2010. Dallas, TX.
Rights and permissions
About this article
Cite this article
Laedtke, A.L., O’Neill, S.M., Rubinstein, W.S. et al. Family Physicians’ Awareness and Knowledge of the Genetic Information Non-Discrimination Act (GINA). J Genet Counsel 21, 345–352 (2012). https://doi.org/10.1007/s10897-011-9405-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-011-9405-6