This qualitative study explores how 29 Swedish patients with Multiple Endocrine Neoplasia type 1 (MEN1) experience living with the condition, appraisal of the clinical follow-up program, and surveys their future expectations. The aim of this study is to build knowledge about this patient group in order to provide optimal care. The participants describe physical, psychological, and social limitations in their daily activities and how these limitations influence quality of life. Our findings indicate that a majority of patients have adjusted to their situation, describing themselves as being healthy despite physical symptoms and treatment. The participants received decent care in the clinical follow-up program, - however, greater effort should be put into patient information. These patients might benefit from genetic counseling. Health professionals involved should recognize their potential impact and influence on a patient’s ability to adjust to these circumstances. Antonovsky`s Sense of Coherence theory is used to discuss these findings.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
The rapid increase in genetic knowledge and developments in modern gene technology have made it possible to identify individuals with an increased risk for hereditary diseases such as cancer syndromes. Persons at risk for such cancer syndromes may be offered preventive interventions by enrolling in clinical follow-up programs. Since this clinical practice has recently developed, there is a lack of information regarding the psychosocial consequences of living with increased genetic risk of disease and reactions to being involved in a long-term follow- up program. Another key issue awaiting exploration is the effect genetic information has upon family dynamics. Several studies report the need for information about the family perspective (Bottorff et al., 1998; Spijker and Kroode, 1997). The improvement of current clinical practice rests upon building knowledge on these issues.
Berglund et al. (2003) monitored MEN-1 patients with questionnaires concerning psychosocial outcome measures such as anxiety, depression, intrusion, and avoidance. Berglund`s study reported only minor changes in these measures between the visit to the hospital and six months later at home. However, 70% of the participants were defined as pessimists, and those with a high burden of disease and treatment showed an increase in depression levels. This group also scored lower on the General Health and Social Functioning scale than population-based norm values, and Berglund suggests that MEN1 patients who have severe disease and treatment burden should be offered psychosocial support. Winterling et al. (2004) described several ways cancer patients and their spouses handled substantial changes in life. The method most frequently reported by patients was to withhold complaints. Many spouses indicated feelings of hope, and all participants wished to make the best out of the situation.
The purpose of this article is to present and discuss findings from a qualitative study focusing on MEN 1 patient’s quality of life and their expectations for the future. In this study, quality of life (QoL) is conceptualized as the result of a self-assessment made by the patient himself. We understand QoL to be closely related to a view of health as a holistic property of a person, not only concerned with disease, injury, or defect. The concept of health according to this understanding, includes a normative component indicating a person’s general ability to realize his or her vital goals in life (Nordenfelt, 2000). However, a distinction between this idea of health and QoL is acknowledged in that the focus is not directed at the ability to live a good life but rather on the components of that good life itself. For example, given a certain condition or genetic risk, what makes life better or worse for an individual or a group of individuals? There is also a second important distinction. The concept QoL has, like the holistic concept of health a normative element but QoL is a measurement of how the individual patient evaluates life himself at a particular moment, for example, when ill or having received information about a genetic vulnerability (Lindblad et al., 2002). In contrast to many QoL instruments, we have included existential aspects of QoL. With reference to Antonovsky’s theory (Antonovsky, 1987), we suggest that the ability to experience a “sense of coherence” in life may be an important part of having QoL. This may be of particular importance for individuals with inherited diseases where a family is carrying and experiencing a genetic risk throughout life. With reference to Griffin’s theory about prudential values (Griffin, 1986), we suggest that well-being may be built on broader categories than usually considered in QoL instruments.
MEN1
Multiple Endocrine Neoplasia type 1 (MEN1) is a hereditary cancer syndrome defined by the development of endocrinological tumors, which may or may not be malignant. These tumors often arise in the parathyroid glands, entero-pancreatic neuroendocrine system, anterior pituitary, and sometimes also in other tissues (Marx et al., 1998). Various types of tumors in these tissues may occur including gastrinomas, insulinomas, prolactinomas, and carcinoid tumors. Estimated MEN1 prevalence ranges from 0.02 to 0.2 per 1000 (Brandi et al., 1987). The underlying cause of this syndrome is localized to chromsome 11q13, and represents a putative tumor-suppressor gene (Chandrasekharappa et al., 1997; Bassett et al., 1998). Such a mutation is inherited in a dominant fashion, therefore offspring of an affected individual have a 50% chance of inheriting the MEN1 mutation. When a specific mutation can be identified in a family, family members who test negative for the specific mutation will carry the general population risk for this disorder. There is normally no need for specific follow-up or further testing in the test- negative group (Karges et al., 2000). In stark contrast, lifelong clinical surveillance for mutation positive patients is recommended in order to detect early development of tumors that may reduce the morbidity and mortality of MEN1 patients (Brandi et al., 1987; Karges et al., 2000). In approximately 90% of patients, the first manifestations of the disease are parathyroid tumors detected by hypercalcemia (Thakker, 1998).
Penetrance in this disorder is nearly complete and symptoms may occur already from the age of five (Brandi et al., 1987). Approximately 80% of affected individuals will be symptomatic by the age of 50 (Carty et al., 1998 ).
Genetic Counseling in Scandinavia
Patient access to genetic counseling services in Scandinavia has been limited by the relatively recent development of the profession in this region. Genetic counseling practice varies significantly between the Scandinavian countries due to differences in educational background, and in some cases drastic differences in legislation regulating genetic testing. A Masters degree program of Health Science in Genetic Counseling was established in Norway at the University of Bergen, in 2001. The first genetic counselors in Sweden completed their training at Uppsala University, in 2005. However, locally trained genetic counselors have been working in both countries for a decade, and also medical geneticists are providing genetic counseling. In Norway, restrictive legislation was introduced in 1994 protecting persons from genetic discrimination. This law mandates genetic counseling prior to and following predictive testing. Genetic counseling and genetic testing are funded by the National Health Service in both Norway and Sweden, theoretically allowing for equal access to such services.
Relevant Literature
Griffin (1986) defines four prudential values, which in individually characteristic combinations constitute essential aspects of a person’s overall quality of life. The four values Griffin defines are: (i) the ability to enjoy a certain sense of autonomy, not merely being victim to circumstances beyond one’s control; (ii) the enjoyment of pleasure, life should not only contain pain and suffering; (iii) the enjoyment of a certain level of deep personal relationships and; (iv) the enjoyment of having accomplished something in life, leaving an imprint. These values correspond well with components identified in quality of life surveys (Lindblad et al., 2002). It is essential to emphasize that each individual may select a personal mix of these values.
Health related quality of life is defined in a multitude of ways. Patrick et al. (1988) refers to how disease, accidents, or treatment may influence a person`s level of well-being, satisfaction, and opportunity. Other definitions of health related quality of life concern internal subjective states such as: well-being, the ability to perform usual daily activities, and perceived health (Stewart and Kings referred in Shumaker and Naughton, 1995).
Antonovsky (1987) claims that in order to establish healthy well-being, emphasis should be placed on resources and capacities rather than on disease. In his study of menopause in Israeli women surviving concentration camps in the Second World War, he surprisingly noticed that these women were in good health in spite of the traumatic experiences they had endured. On this background he developed his salutogenic model called sense of coherence (SOC), a state that develops during childhood and adolescence. In line with Moons and Norekvål (2005), several studies of different populations show that SOC is related to quality of life. New research supports the idea that SOC develops and increases through life, and has strong positive correlations to perceived health, mental health, and quality of life (Lindstrøm and Eriksson, 2005). SOC comprises three dimensions: comprehensibility, manageability, and meaningfulness. Comprehensibility is defined as the extent to which internal and external stimuli experienced are perceived as structured, predictable, and explainable. Manageability concerns the individuals perceived resources to deal with stressful situations or disease. Meaningfulness is the main focus of Antonovsky’s theory. If a person experiences a high degree of meaningfulness in life, comprehensibility and manageability might be changed. The central lifetime elements necessary to achieve meaningfulness are: interpersonal relationships, existential issues, activities, and employment. These aspects of life need to be experienced as meaningful and invested in, otherwise they could be lost over time.
Essential to this concept of meaningfulness is the idea that individuals should participate in shaping their own future (Antonovsky, 1987). As in genetic counseling, the aim is to assist the patient in coming to terms with the situation by strengthening the person’s resources. According to Emanuel and Emanuel (1992), this goal should be recognized by the genetic counselor when helping the patient to adjust to information or an actual medical condition.
Empowerment concerns the ability to mobilize and strengthen personal resources, and to neutralize those forces, which may lead to helplessness (Anderson, 1996). Patient education is often used to achieve this goal (Thesen and Malterud, 2001). One aim of genetic counseling is to aid in empowerment (Emanuel and Emanuel, 1992). This often involves helping patients gain insight into their conditions. Although we possess a great deal of knowledge about how best to provide information about illness and disease in general, the genetic counseling situation represents a new challenge. Genetic counseling often encompasses aspects other than merely providing information to patients. It is defined as a communication process where the aim is to help the individual and the family capable of dealing with issues associated with a heritable condition (Baker et al., 1998). There is also an element of psychotherapy in genetic counseling, as the patient’s coping strategies are explored and interdisciplinary teamwork with psychologists is common.
METHODS
Sample
The respondents in the study (n=29) were recruited through a specialist ward for MEN1 patients at Swedish University hospital. Ninety percent of the Swedish MEN1 patients attend this clinic once or several times per year depending on individual needs. Patients are admitted to the hospital ward for several days, and multiple parameters are evaluated such as blood values and hormone levels. Depending on the severity of the disease, additional tests might be performed such as computer tomography, ultrasound, and PET scans. In cases of tumor development treatment will be initiated. Additional surveillance and treatment may be performed at local hospitals.
Thirty-four of the MEN1 patients who attended the clinical follow-up program over a one-year time period were asked to participate in the study. Two patients were not asked to participate due to recent diagnosis of the condition, and five cases declined participation. The sixteen men and thirteen women participating ranged in age from twenty-eight to eighty-five years. Twenty (69%) were over age fifty, nine had Interferon or chemotherapy treatment, and twenty-five had been treated surgically.
Data Collection
A qualitative research interview was carried out. The respondents were interviewed in the clinic on the day of arrival. Two Swedish psychologists performed the individual interviews. The interviews lasted on average one hour and were audiotaped with consent. Both structured and open-ended questions were used during the interview. A structured interview guide developed from Griffin (1986) focusing on quality of life, ability to affect and control one’s own life, interpersonal relationships, and ability to accomplish personal goals in life was utilized. The open-ended questions focused on the emotional and practical implications of having this condition in the family, such as the effect upon family dynamics. Other questions focused on participation in a clinical follow-up program, and the effect upon daily activites. Participants were also asked about information and care received from the health care providers. According to Kvale (1996), one is more likely to obtain spontaneous, lively, and unexpected answers from open-ended questions. In order to investigate the patients’ experiences of living with MEN1, they were encouraged to expound upon any issues important to them and vital information was obtained from these questions. The interview guide was validated in a pilot study on empirical views of life (Westerlund, 2002).
Medical records were reviewed to collect data on age, frequency of follow-up program, genetic testing results, surgeries, treatments, and hospitalization during the past year. The patients were also asked to complete two questionnaires. The first questionnaire was completed during their stay at the hospital, and the second in their homes six months later. (Data from these questionnaires is reported in Berglund et al., 2003).
Approval for this study was obtained through the local Research Ethics Committee at the actual Swedish hospital.
Analysis
Following transcription, the data were analyzed using Giorgi`s four step phenomenological approach (Giorgi, 1985; Kvale, 1996). The aim of this approach is an attempt to see the world from the respondent’s point of view. As described in this approach, the interview transcripts were read repeatedly, and meaning units were identified. The colloquial language was transformed into professional terminology. Finally, the transformed meaning units were synthesized into a consistent description of themes regarding the participant’s experience, and all transformed meaning units were considered. The content of the themes emerged from the data, but the concrete formulations were discussed between the first and last author during the entire process of analysis. In this respect, there is an element of interpretation by the researchers. Antonovsky’s model turned out to be relevant for the discussion of the results of the analysis, but had no influence on the analysis itself.
The data program NUD*IST (Nonnumerical Unstructured Data Indexing Searching and Theorizing) was used to organize and analyze the interviews.
RESULTS
The general structure that emerged from the data represents the participant’s perspective on what impact the condition has had on their quality of life. Four main categories and several subcategories were identified; The mixed feelings of being in a follow-up program, the effect of MEN1 upon daily activities, coming to terms with the condition, and uncertainty concerning the future. These themes are illustrated in excerpts from the transcript where the participants talk about their experiences.
MIXED FEELINGS OF BEING IN A FOLLOW-UP PROGRAM
Being included in the follow-up program seems to be accompanied by mixed feelings. Most of the participants were satisfied with the program in some respects, but they also expressed a need for medical and genetic information.
Satisfaction with the Follow-Up Program
The majority of participants indicated overall satisfaction participating in the clinical follow-up program, and with their healthcare providers. They felt well cared for and safe under the care of specialists. Some of the patients had been ill for several years without receiving the proper diagnosis at their local hospitals.
“Yes, it began with that I had hyperparathyroidism, that is a part of this, it was found sometime maybe at the end of the 1980s and then I was operated on twice at the local hospital but there wasn’t anyone who understood that it was part of the MEN1 syndrome. No, but at least I felt like we did what we could on the surgical side of things at the local hospital. But I felt that there was something that wasn’t quite right and wanted a second professional opinion about what I regarded only as hyperparathyroidism.”
All patients expressed a feeling of trust towards the health care professionals who cared for them in the follow-up program:
“I trust the doctor here. It feels wonderful to come here.”
They described feeling a close relationship between the clinic staff and the patients, and this contributed to feelings of trust and safety:
“I have been here so many years now. Laura and Ann and those that have been here all these years, they are like old friends now.”
There was also a feeling of uncertainty connected to the follow-up program. Several patients mentioned fear of the test results. For many of the participants, earlier visits to the hospital had prompted surgical interventions due to tumor identification:
“As I said, I am thinking the whole time… what will they find this time?”
The mixed feelings of being in the follow-up program shifts between feeling safe and the feeling of frustration due to lack of information.
Lack of Medical and Genetic Information
Twenty-seven (93%) of the participants of the present study reported a need for greater access to understandable medical and genetic information. The lack of information seemed to be frustrating. This subcategory describes how individuals use family and fellow patients as sources of information, and blame themselves for not understanding medical terminology presented to them. They expressed a need for informative communication with the health care providers including better access to test results:
“Yes, I could have wished that someone would be able to sit in peace and quiet with me maybe, in this case, Mary or Joe, and really discuss through the situation.”
The health care providers have given information to the patients, but many have been unable to understand the diagnostic and medical terminology presented:
“I don’t think I have any direct complaints except for the strange words and when I first learned about it they told me that I had MEN1 and then I thought that it must be some kind of Spanish dance or something.”
Some of the participants blamed themselves for not understanding the information:
“No, we haven’t, so it must be our own fault and then.. It is such a complicated topic that you don’t understand all the information that you get. Maybe they.. actually have information so that we can actually understand what they are saying?”
The clinical staff encouraged the patients to ask questions, but in order to do so, the patients must be provided with some basic knowledge:
“The doctors that I have met have been very receptive and had time for questions, but it seems that the less you know about something, the fewer the questions that you have.”
Some tried to learn about the condition themselves by randomly asking available staff in the clinic:
“Yes, one time I went to the reception desk and asked, “what disease do I have?” Then they gave me a piece of paper that said MEA1 and the M stood for multiple, E for endocrine and A, I don’t know what A stood for.”
Others learned from fellow-patients. During the years in the follow-up program, some participants developed close relationships with other patients in the same situation. They also shared medical and genetic information, and learned from one another:
“No, when it came out that I had this, many years passed and I didn’t know it was hereditary. I began to question because I shared a room with someone that had it. I was told that it was hereditary.”
Some of the younger participants learned from their parents who had engaged themselves deeply in order to avoid uncertainty and fear by providing their children with information. One source of frustration was the uncertainty after the visits to the clinic. For most of the patients, the medical test results were not immediately available when they left the hospital, and they spent several weeks waiting and worrying about the results. When the letter finally arrived after eight weeks, the medical terminology made it difficult to understand:
“Yes, and there is also a difference when I read and understand it in one way and then my husband reads and understands it in a completely different way… It is almost like a horoscope, you can interpret it however you want.”
This uncertainty lasted until the next visit to the hospital:
“When I come here I usually ask “how am I doing?” instead of them asking me.”
Several participants reported that not knowing what to expect in the future made it difficult to inform close family members:
“I can’t blame them in any way, but I could have wanted to maybe discuss things a little more with my family… my wife could have more easily understood the situation. What was going to happen and what might happen etc.”
In most families, blood samples had been collected from several family members, but the family mutation was identified in only 22% of these families. In cases where a mutation was not detected, many of the participants were not informed of their test results. Some were concerned about what future impact the test result might have upon their children’s future if a mutation was detected:
“Yes, exactly … and the girls don’t know how long they have progressed with the kind of tests that can be done on them. They are a little worried about the test they might have taken in regards to insurance, changing jobs, and that kind of thing. Are they gene tested or not?”
THE EFFECT OF MEN1 UPON DAILY ACTIVITIES
The participants described certain issues that influenced their everyday life. The main issues were; physical and psychological pain, job insecurity, and feelings of guilt:
Physical and Psychological Pain
Many patients reported that they had to cope with physical and psychological pain, but most of them had found a way of dealing with the condition. The patients described a wide spectrum of symptoms ranging from being asymptomatic to having debilitating physical and psychological burdens. A variety of physical symptoms were reported. The participants described abdominal pain, diarrhea, and sweating, due to hormonal effects. In addition, some individuals had to cope with the side effects of cancer treatment. Several of the participants in the present study reported headaches as a limitation in their daily activities:
“Yes, I have had three or four different types of headaches then … like, sometimes I have one nail that sits “right” in here. It feels like being struck with a hammer. Since then I have had headaches above my eyes and then also stress headaches and migraines.”
Many participants developed diabetes and need-ed to regulate their daily activities strictly:
“Yes, it feels heavy in my chest and … and later yes, the diabetes can make itself known too if you are not careful with your diet and maybe work too much in the garden or with something else at the same time. Physical work can make your blood sugar go down, but I have learned now that you need to eat a little snack in between and not neglect it.”
The participants described psychological symptoms, which ranged from light changes in mood to depression. A young man was commenting on the emotional impact of hormonal disturbances:
“I could have stabbed through a wall. I became angry, not at anything in specific. Instead I almost can’t hold back the tears. It swings back and forth.”
Some patients reported depression. One woman expressed how she now was able to recognize her mother’s symptoms:
“Nothing, no other symptom aside from that I thought that I became more and more like my mother in mood. Heavy, I can’t really say. I didn’t understand that it was depression, I can’t say that I had the words, or, but it was like that she was heavy in her moods, like, yes, I might call it, “sad.”
The patients also experienced grief due to the substantial changes and limitations the condition had imposed on their future options. For some of the patients the condition has caused infertility:
“Yes, of course it would have been very nice if we had had children. I feel that we both missed out on that.”
Other participants felt stigmatized by insurance companies and were excluded from certain occupations:
“It has stopped me from doing some things, like, I can’t apply for some types of health insurance and things like that. I can’t apply to the police academy or for pilot training.”
Job Insecurity
The clinical follow-up program, treatment, and surgeries resulted in absence from work or studies for periods of varying duration. Some patients could only maintain part-time employment due to their health condition. Others were not capable of working at all. Some participants experienced conflict with their employer related to their condition, and one even lost his job. In contrast, others viewed their employer and colleagues as being supportive. Capacity to maintain employment and to sustain social relationships with colleagues seemed very important.
For several of the participants, the disease has limited educational and career options:
“Yes, obviously after these operations you will be on sick leave for quite some time, and then you will work part-time, you are put into a position at work instead of being able to work full-time and put your heart into something .. …”
The health of other family members might also have had an impact upon their options:
“I have taken care of my mother for 36 years and also my father when he got old. I was 19 years old when I was accepted as a student, but I didn’t pursue studies so I could be home and help my parents.”
For some of the participants the condition has had a negative impact on personal finance:
“Yes, there are many issues … There is a financial side in this as well, even if one has previously been financially solid because a lot of this comes at a price. It sometimes costs for example, 1900 Swedish Crowns per year for medications and then you take that for ten years, that comes to 19,000 Swedish Crowns and then comes the traveling. There are always some bills and since I am alone and have never had a real job, I can’t collect a proper pension so it is a very low sum. So, this financial side can become worrisome, yes.”
Feelings of Guilt
This subtheme describes how feelings of guilt influenced reproductive decision-making, uncertainty towards in-laws, and difficulties in informing both close and extended family members. Many respondents described the possibility that other family members may also be affected as being the worst aspect of living with the condition. Knowing that they might have transmitted the potential to develop MEN1 to their children was a heavy psychological burden. These patients were afraid that their children might suffer in the future, and felt guilty of having brought this situation into their children’s lives:
“It is indirectly my fault, if she needs to have these major operations that I have had, right?”
Some of the patients felt the need of explaining that they did not have this knowledge when they decided on starting a family. Others had consulted their doctors about the issue of childbearing:
“It was one of the first things we asked our doctors, what they thought about us having children.”
Some participants commented on their children’s reproductive decision-making:
“Partly, they are relatively still young and at a fertile age, so they can still have children and maybe they need to make some kind of a decision.”
One patient worried about what her daughter-in-law thought about her since she has brought the condition into her life and potentially put her grandchildren at risk. Another mother worried about whether her daughters would be accepted by other families:
“Boyfriend’s parents, will they want their sons marrying girls who know that they have this kind of disease?”
An unpleasant challenge in the future is informing children about the condition in the family. One of the patients found it hard to tell her children about the disease:
“And it also feels difficult. I haven’t yet told them that I have a heritable disease. And when I am going to do it? and how I am going to do it?, I think that is extremely difficult.”
She continues:
“Yes, exactly, and then I feel worried about how much I should or shouldn’t tell now.”
Knowledge about MEN1 in the family will also impose a burden upon other family members. In many cases, extended family members will need to be informed about the genetic condition and about the possibility to enroll in a follow-up program or to be tested. Not all family members are pleased when the information has been passed on, and sometimes it has caused communication problems within the family. Some individuals may become angered by this information and become angry with its messenger.
COMING TO TERMS WITH THE CONDITION
The participants described how they have adjusted to the situation after some time, and expressed a change in values, but not in religious belief. They also described social relationships as the most important facet of their lives.
Change in Values
Most of the patients seemed to have found a way of dealing with the condition in their everyday lives. For several of the patients it was hard to learn about the condition and its consequences. One of the young women needed professional psychological help to accept the situation:
“Yes, yes it is again, now it feels like there is so much else happening, and a lot of time has passed and everything seems to be working pretty well. But in the beginning, then it was really hard and I remember when I had just been at the cancer hospital and spoke with her there, I couldn’t imagine that I would live to be 40. I could only think, then I don’t know any more, but now, yes, now there is so much else happening, we are expecting a child and everything.”
Several described that they have worked hard to adjust to the situation:
“Yes, but it isn’t an obvious process or an easy process either. You also need to struggle a little to be able to think that you are actually doing well. It doesn’t happen on its own.”
Despite severe disease, surgery, and other treatment, most of the patients described themselves as healthy. Some expressed that they had never felt sick, not even during treatment. Many of the patients defined the concept of health and well-being in a subjective manner.
“Health is when you feel good.”
Some claimed that health care providers defined the concept of health differently:
“No, I have never been sick otherwise. It is the doctors here who say that I am ill, but I haven’t been. The drawback is the diabetes that I have and also of course that the children can be affected.”
They often prioritized differently after adjusting to their present situation. Small, everyday issues such as being able to get out of bed in the morning, being able to walk, maintaining daily activities and employment became essential:
“These small things are taken care of in a totally different way. You have a different perspective about living.”
Some of the participants had religious beliefs, but most of them did not. The condition did not seem to have altered their religious beliefs. However, most of the patients believed that some kind of life after death exists. Several expressed a wish of meeting deceased friends and relatives after death. One way of accepting the situation is to find meaning in the situation:
“As it feels now I think about how much you have to go through with losing relatives. With illness you become really… It is a tired expression but it is really true that you become strong. Every difficult setback that you manage to tackle, you believe that it can’t get any worse than it already is, and then, that you can handle almost anything.”
Two of the participants felt like they were being punished. Others described the situation as meaningless:
“I don’t think there is any meaning to be found in becoming sick.”
Social Relationships
The majority of the participants in the present study reported that social relationships with friends and relatives were one of the most important issues in their lives:
“Yes, logically it is about the relationships. They are the most important. I think that if you don’t have relationships with other people, then you have nothing to live for.”
The condition has brought close family members even closer together:
“You might not think it yourself, but my husband thinks that the girls have grown closer in some way and that it maybe touches on that both of them are more protective about me or that they are more worried about me in some way. I have become also a kind of information source.”
They experienced support from friends:
“…Which comes to me and I haven’t been abandoned by my friends, neither when I became a widow, nor when I got this illness without them carrying me in some way.”
They recognized true friends:
“Well, I had close friends that disappeared when I got sick. We were never close after that.”
UNCERTAINTY CONCERNING THE FUTURE
In this category the patients described certain issues concerning an uncertain future, and their own ability to influence and control their lives.
Shorter Perspective
Many reported concern about an uncertain future, and had a short-term perspective in future planning. They described experiencing lack of control and uncertainty since their physical condition may vary on a daily basis, making it difficult to plan for longer periods:
“Yes, possibly. When you get an illness like this you tend not to plan so far in advance. That’s why I go by how I feel day by day, so that I might want to … Yes, today I feel good, today we can do this and that, today we can find things to do, but it is difficult to say for example, in three months that we could reserve this trip and.. I have difficulty in deciding in advance or to plan too far ahead.”
They reported uncertainty regarding the progression of the disease and whether they would develop cancer in the future. Many of the participant’s concerns about the future were also connected to family issues. Family history and personal experience with illness in the family seemed to influence perspectives about the future:
“It’s as, as I experienced the last year my father lived, it wasn’t really very fun.”
The uncertain future seemed to be related to not knowing what might happen to themselves, their children, or other close family members. Many of the patients expressed a fear that the condition might worsen. Progression of the disease would make life even more difficult:
“Yes, it’s as if someone would say that it would flare up again now, and then I become sad and afraid. What are they going to do? Now I am undergoing chemotherapy, what else can you do?”
There was also fear for those who have already experienced the burdens of treatments and invasive procedures that they might have to undergo further treatments or surgeries in the future. Another important issue in the patient’s lives was the ability to maintain their professional career. It would be a heavy burden if the progression of the disease made them unable to carry on with their jobs. Some of the elderly participants expressed gratitude for having reached a certain age, and did not seem to have any future expectations.
Ability to Influence and Control One’s Life
Most participants expressed feeling a lack of control over their situation due to the development of the disease:
“Yes, I can’t decide over the progression of the tumor that is in my pancreas for example.”
They seemed to rely on the follow-up program’s ability to detect tumors at an early stage:
“I am in the hands of the doctor.”
On the other hand, most patients reported a change in lifestyle, and several seemed to think that they had influence on some issues:
“Yes, you don’t have total freedom of choice, I don’t have it but I think … I still think you can have quite a bit of influence on your own life.”
Some reported that they intended to live a healthier life, and were more focused on nutrition and physical activity than they had been earlier in life. Many commented on giving up smoking, and reducing intake of alcohol. One man compared his body with a car:
“Yes, because.. many think that the car has to have the absolute best oil, best gasoline but how is your own fuel intake? That’s why my wife and I, we try to be a little more careful about what we put into ourselves.”
Most patients claimed that they were able to control important issues in their lives:
“Yes, of course I have. I can decide about myself and how I am feeling and such things.”
Not everybody desired control:
“But it is not certain that you would WANT to have control over everything.”
DISCUSSION
Findings from the present study revealed some of the issues these patients face routinely in their everyday lives. The participants described physical, psychological, and social limitations in their daily activities and how these limitations had influenced their quality of life. Patients expressed a need for risk information, diagnostic information, and future surveillance plans. The clinical follow-up program seemed to play a central part in the participant’s lives. The majority of participants indicated overall satisfaction with being in a clinical follow-up program, and with the health care providers. However, the lack of understandable medical and genetic information seemed to be frustrating, and they were not able to clearly identify those life circumstances connected to MEN1 and act upon them. Patients who are unable to take control of such issues will be unable to achieve their fullest health potential. According to Glanz et al. (2002), coping strategies among patients and persons at risk may have a significant influence on psychological and physical health outcomes.
Though most participants expressed feeling a lack of control over their circumstances, they tried to influence the situation by changing lifestyle and focusing on nutrition and physical activity. According to Griffin (1986), it is important to maintain a certain sense of autonomy instead of solely being victim to circumstances beyond one’s control. This aids in achieving quality of life. This concurs in many respects with Antonovsky`s (1987) view that in order to experience meaningfulness, it is important for individuals to feel that they have control over their own fate. This aspect of health behavior may also be explained by Leventhal’s self-regulation model of illness perception (described in Chapman and Bilton, 2004), whereby controllability relates to whether or not the illness is treatable and/or curable. The patients felt it was important to be included in the follow up program because if tumors developed, treatment would be started and they would be cured.
In the present study, employment and the work situation seemed to be essential in sustaining the patient’s sense of control. We have seen that patients fear limitations MEN1 might impose on their professional lives and employability. Inability to maintain or fulfil future career plans are real issues for these individuals. This aspect may also be important to accomplish something in life as viewed as an element in overall quality of life (Griffin, 1986). According to Antonovsky (1987), employment is an important issue in life that needs to be experienced as meaningful, and needs to be invested in. If not, resources will be lost over time. It is essential to the concept of meaningfulness, that individuals participate in shaping their own future (Antonovsky, 1987). Berglund et al. (2003), claims that 70% of MEN1 patients were defined as pessimists. In this qualitative study, the pessimistic outlook seems to be related to difficulties in coping with an uncertain future. The patients reported shorter perspective in future planning and described fear of what might happen to their children and other relatives. This pessimism may also concern the uncertainty regarding the progression of the disease and how this might impact negatively upon their daily activities, and their ability to maintain their present work situation. Pessimism seems to be a natural element of coping with a genetic disease of this kind rather than a personal characteristic (Berglund et al., 2003).
According to Antonovsky (1987), comprehensibility is another important issue in coping with illness. Providing these families with knowledge about the condition might aid in making the future more predictable and thereby enhancing comprehensibility.
Antonovsky’s concept of manageability requires that clients are able to perceive available resources. In this study we have learned that patients had confidence in their health care providers and felt well cared for but at the same time often felt frustrated about a lack of understanding. By providing more medical and genetic information these professionals may teach patients how to deal with issues associated with MEN1. For improving manageability in children and adolescents, parents may be perceived as available resources. Teaching family members about their condition might contribute to improve the quality of life for all members of the family. Further, we have learned that several patients commented on reproductive issues, and how feelings of guilt influenced reproductive decision-making, uncertainty towards in-laws, and the difficulties informing both close and extended family members. In cases of discussing issues related to family dynamics or reproductive decision-making, nondirective genetic counseling is important (Resta, 2000). A critical element in decision-making is having relevant information about the actual genetic condition, the pattern of inheritance, and how to deal with the risk. It also concerns the understanding of personal consequences, and the implications on the family. Issues such as family dynamics, feelings of guilt, and future perspective, are natural parts of a genetic counseling session. Addressing these issues might contribute in strengthening the patient’s resources and help to develop meaningfulness by supporting them to take control of their lives. Having some influence over one’s own future is essential for developing meaningfulness according to Antonovsky (1987).
Despite disease severity, surgery, and other physical and psychological symptoms, most of the patients described themselves as healthy. Some expressed that they had never felt sick, not even during treatment. Many of the patients defined the concept of health and well-being in a subjective manner. They reported a shift in priorities after developing MEN1 or learning about their personal risk, much in line with what is predicted by Antonovsky (1987), Griffin (1986). Changing values helps the patients to find meaning in the situation. The patients also tried to explain why this situation had occurred. Finding an explanation is a way to find meaning in the situation, and is according to Arman et al. (2002) common among cancer patients in general. According to Antonovsky (1987), one is able to maintain health and thereby adapt to illness by altering expectations. However, existential issues seem to remain unchanged during the progression of the illness. None of the participants altered their religious beliefs. Not all patients could find meaning in the situation, and two of the participants felt that they were being punished.
The participants in the present study reported that interpersonal relationships with family and friends were one of the most valuable aspects in their lives. This is in line with the Antonovsky model where interpersonal relationships are central for achieving meaning. This is also in line with Griffin’s definition of quality of life. According to Glanz et al. (2002) several studies show that the influence of social support can have profound effects on dealing with disease-related stress.
Genetic counseling and empowerment will likely not solve all of the patient’s problems, or might not have the intended effect. For example, if the timing of the information presented is not optimal. Patients in crisis may not have the capacity to understand or take in information when presented to them. However, some of the participants who had been in the program for many years still felt they were lacking information.
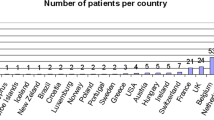
According to Antonovsky (1987), the experience of meaningfulness is the most important issue in creating well-being and health. Receiving adequate information is probably an important step on the road to achieving meaningfulness. In addition it may be a crucial component of living a good life in spite of their genetic condition (Fig. 1).

STUDY LIMITATIONS
Data analysis in this study was performed by the first author, a Norwegian, and the interviews were carried out by Swedish interviewers. Having another person analyze the data might strengthen the objectivity of this study. However, drawbacks might include the cultural differences between Swedish and Norwegian conditions, and differences in medical and genetic clinical practice and legislation. Therefore, the first author had to study the Swedish health care system and routines related to genetic counseling prior to the analysis. Language differences may also represent some barriers, but having Swedish co-authors contributed to confirm the understanding. Another issue may be the loss of non-verbal cues during the interviewing process. To compensate, the interviews have been listened through carefully.
The sample in this study may be representative of the population as twenty-nine out of thirty-six patients (80.5%) participated. Ninety percent of the Swedish MEN1 patients attend this clinic once or several times a year. In addition there are variation concerning gender, age and treatment. The interviews reached the point of saturation where further interviews obtain little new knowledge. According to Kvale (1996) saturation tend to be reached around 10–15 interviews. However, in a qualitative study there will always be a limitation of generalizabilty concerning the study findings. Therefore it would be useful to explore further the themes described in this study in a similar setting in order to help confirm the results from this study.
In the present study only 22% of the participants were mutation positive. The low value of mutation positive participants might be explained by the timeframe the data collection was performed.
CONCLUSION
This study indicates that MEN1 patients are in need of medical and genetic information. The patients should have access to genetic counseling. The clinical follow-up program seems to play an essential part in the patient’s lives, and health professionals involved may have a significant impact on how patients adjust to their situation. By providing adequate information the patients may be assisted in enhancing comprehensibility. Despite the fact that most of the patients have found a way of dealing with the condition in their everyday lives, they still have to cope with physical and psychological pain. They also have to cope with lack of control of the situation and the uncertainty regarding the future. To achieve manageability it is essential that the patients regard the health care providers as available resources. Future studies should explore how patients with high risk of hereditary disease might profit from genetic counseling, and whether or not genetic counseling may be used to help patients achieve meaningfulness in accordance with Antonovsky’s model.
REFERENCES
Anderson, J. M. (1996). Empowering patients: Issues and strategies. Social Science and Medicine, Sept, 43.
Antonovsky, A. (1987). Unraveling the mystery of health: How people manage stress and stay well. San Francisco: Jossey Bass.
Arman, M., Rehnsfeldt, A., Lindholm, L., & Hamrin, E. (2002). The face of suffering among women with breast cancer –being in a field of forces. Cancer Nurs, 25, 429–438.
Baker, D. L., Schuette, L., & Uhlman, W. R. (1998). A guide to genetic counseling. Wiley-Liss, Inc.
Bassett, J., Forbes, S. A., Pannett, A. A. J., Lloyd. S. E., Christie, P. T., Wooding, C., Christie, P. T., et al. (1998). Characterization of Mutations in Patients with Multiple Endocrine Neoplasia Type 1. Am J Hum Genet, 62, 232–244.
Berglund, G., Liden, A., Hansson, M. G., Øberg, K., & Sjøden, P. O. (2003). Quality of life in patients with multiple endocrine neoplasia type 1 (MEN1). Familial Cancer, 2, 27–33.
Bottorff, J. L., Ratner, P., Johnson, J., Lovato, C., & Joab, A. (1998). Communicating cancer risk information: The challenges of uncertainty. Patient Educ Couns, 33, 67–81.
Brandi, M. L., Marx, S. J., Aurbach, G. D., & Fitzpatrick, L. A. (1987). Familial multiple endocrineneoplasia type I: A new look at pathophysiology. Endocr Rev, 8, 391–405.
Carty, S., Helm, A. K., Amico, J. A., Clarke, M. R., Foley, T. P., Watson, C. G., & Mulvihill, J. J. (1998). The variable penetrance and spectrum of manifestations of multiple endocrine neoplasia type 1. Surgery, 124(6), 1106–1114.
Chandrasekharappa, S. C., Guru, S. C., Manickam, P., Olufemi, S. E., Collins, F. S., Emmert-Buck, M. R., Debelenko, L. V., et al. (1997). Positional cloning of the gene for multiple endocrineneoplasia-type 1. Science, 276(5311), 404–407.
Chapman, E., & Bilton, D. (2004). Patients’ Knowledge of Cystic Fibrosis: Genetic Determinismand Implications for Treatment. J Genet Couns, 13(5), 369–385.
Emanuel, J. E., & Emanuel, L. L. (1992). Four models of the physician-patient relationship. J Am Med Assoc, 267(16), 2221–2226.
Giorgi, A. (ed.). (1985). Phenomeology and psychological research. Pittsburgh: Duquesne University Press.
Glanz, K., Rimer, B. K., & Lewis, F. M. (2002). Health behavior and health education: Theory, research, and practice. 3rd edition.
Griffin, J. (1986). Well-being. Its meaning, measurement and moral importance. Oxford: Clarendon Press.
Karges, W., Schaaf, L., Dralle, H., & Boehm, B. O. (2000). Concepts for screening and diagnostic follow-up in multiple endocrine neoplasia type 1 (MEN1). Exp Clin Endocrinol Diabetes, 108(5), 334–340.
Kvale, S. (1996). InterViews. An introduction to qualitative research interviewing. Sage Publcations.
Lindblad, K., Ring, Å. L., Glimelius, B., & Hansson, M. G. (2002). Focus on the individual. Quality of life assessments in Oncology. Acta Oncologica, 41, 507–516.
Lindstrøm, B., & Eriksson, M. (2005). Salutogenesis. Professor Aaron Antonovsky (1923–1994): The father of the salutogenesis. J Epidemiol Commun Health, 59(6), 440–442.
Marx, S., Spiegel, A. M., Skarulis, M. C., Doppman, J. L., Collins, F. S., & Liotta, L. A. (1998). Multiple endocrine neoplasia type 1: Clinical and genetic topics. Ann Intern Med, 129(6), 484–494.
Moons, P., & Norekvål, T. M. (2005). Is sense of coherence a pathway for improving the quality of life of patients who grow up with chronic diseases? A hypothesis. Eur J Cardiovasc Nurs, 5(1), 16–20.
Nordenfelt, L. (2000). Action, Ability and Health. Essays in the philosophy of action and welfare, Dordrecht: Kluwer Academic Publishers.
Patrick, D. L., Danis, M., Southerland, L. I., & Hong, G. (1988). Quality of life following intensive care. J Gen Intern Med, (3), 218–223.
Resta, R. G. (2000). Psyche and helix. Psychological aspects of genetic counseling. Essays by Seymor Kessler, Wiley-Liss Inc.
Shumaker, S. A., & Naughton, M. J. (1995). The international assessment of health-related quality of life: A theoretical perspective. Oxford: Rapid Communication of Oxford Ltd.
Spijker, V. A., & Kroode, H. F. J. (1997). Psychological aspects of genetic counselling: A review of the experience with Huntington’s disease. Patient Educ Couns, 32, 33–40.
Thakker, R. V. (1998). Multiple endocrine neoplasia: Syndromes of the twentieth century. (Editorial). J Clin Endocrinol Metabol, 83, 2617–2620.
Thesen, J., & Malteud, K. (2001). “Empowerment” og pasientstyrking- et undervisningsopplegg. Tidsskrift for den Norske Legeforening, Nr. 13, 121, 1624–1628.
Westerlund, K. (2002). The meaning of Context: An empirical study of Views of Life in Perceptions of Gene Technology and in Narratives about Childlessness, Assisted onception and Adoption. Acta Universitas Upsaliensis, Uppsala Studies in Faiths and Ideologies 10, 296pp, Uppsala, ISBN 91–554-5360–0.
Winterling, J., Wasteson, B. G., & Sjøden, P. O. (2004). Substantial Changes in Life. Cancer Nurs, 27(3), 381–388.
ACKNOWLEDGMENTS
We acknowledge the Norwegian Cancer Society, the Functional Genomics (FUGE) network and the University of Uppsala for financial support. Special thanks also to the two anonymous reviewers and the editor for their helpful comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Strømsvik, N., Nordin, K., Berglund, G. et al. Living with Multiple Endocrine Neoplasia Type 1: Decent Care-Insufficient Medical and Genetic Information A Qualitative Study of MEN 1 Patients in a Swedish Hospital. J Genet Counsel 16, 105–117 (2007). https://doi.org/10.1007/s10897-006-9047-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-006-9047-2