Abstract
This study aims to examine the associations between child maltreatment (physical and psychological neglect and abuse), dysfunctional family environment (inter-parental violence, parental substance abuse), post-traumatic stress disorder (PTSD), and children’s bullying perpetration, and the potential mediating effect of PTSD in the associations. We collected data using a self-report questionnaire with a nation-wide, proportionately stratified random sample of 6233 fourth-grade students in Taiwan. We performed hierarchical regression analysis and mediation analysis to test the research hypotheses. The results indicate that parental substance abuse, physical and psychological neglect, physical and psychological abuse, witness of inter-parental violence, and PTSD are positively associated with child bullying (p < .001), after controlling for gender. These variables, referred to as adverse childhood experiences (ACEs), explain 23% of the variance, and the results are statistically significant. PTSD fully mediated the relationship between psychological neglect and child bullying and partially mediated the associations between other ACE variables and child bullying. Children with higher levels of bullying perpetration reported more family violence and neglect at home and parental substance abuse problems. These ACEs also indirectly affect child bullying through PTSD. Among school-age children in Taiwan, children who had these adverse experiences were more likely to have PTSD symptoms, which in turn can lead to externalizing problems that increase the risk of exhibiting bullying perpetration toward others. In addition to behavioral modeling and corrections as strategies to combat bullying in schools, prevention and intervention efforts should address and screen for ACEs and tackle psychological problems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adverse childhood experiences (ACEs) include different types of child maltreatment (e.g., physical and psychological neglect, physical and psychological abuse) and dysfunctional family environments (e.g., witnessing interparental violence, parental substance abuse, etc.). ACEs are significant predictors of both internalizing problems (e.g., depression and anxiety) (Balistreri and Alvira-Hammond 2016; Barber et al. 2014) and externalizing behaviors and problems (e.g., aggression, violent delinquency) (Mumford et al. 2019; Perez et al. 2018). Researchers have shown that child maltreatment has strong associations with later conduct disorders, aggression, and violent behavior in American adult samples (Afifi et al. 2011; Harford et al. 2014). Although research has found correlations between child maltreatment and externalizing problems in adolescents (Ryan et al. 2013), such correlations and their pathways/mechanisms remain inadequately understood.
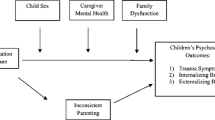
To this end, this study examined the associations between various types of ACEs (physical and psychological neglect, physical and psychological abuse, witnessing inter-parental violence, and parental substance abuse) and child bullying and the potential mediating effects of post-traumatic stress disorder (PTSD) in these associations as a pathway from victim to perpetrator and from internalizing problems to externalizing problems. The results can provide informed decision-making in targeting appropriate prevention strategies and interventions.
Child Bullying
Bullying refers to aggressive behavior with intent to harm that occurs repeatedly and encompasses an imbalance of power between the bully and the victim (Olweus 2013). Bullying can be exhibited in many forms, such as physical acts (e.g., hitting, kicking, tripping), verbal acts (e.g., teasing, name calling, making threats, making inappropriate sexual comments), and social acts (e.g., spreading rumors, being purposefully exclusive, embarrassing someone in public). Bullying is associated with numerous negative psychological and behavioral effects, such as depression, suicidal ideation and behaviors, and substance abuse (Garnefski and Kraaij 2014; Luk et al. 2010; Reed et al. 2015; Stapinski et al. 2015). In short, bullying is a significant public health problem and social issue.
A systematic review of more than 80 studies found that the prevalence of traditional bullying among adolescents (aged 12 to 18 years) was around 35% (Modecki et al. 2014). In Taiwan, 38.65% of middle-school students reported having engaged in at least one kind of physical bullying during the last semester and 53% reported verbally bullying others (Wei et al. 2010). Another study using a sample of 14,022 Taiwan students from elementary to high school (Grades 4 to 12) found an even higher prevalence of 68% for perpetrators of bullying for at least one type of violent behavior during the preceding year (Chen and Avi Astor 2010). Boys were more physical aggressive than girls, and girls were more relationally aggressive than boys (Zimmer-Gembeck et al. 2005).
Adverse Childhood Experiences and Bullying
ACEs are associated with externalizing problems in adolescents and adults (Allwood and Widom 2013; Mumford et al. 2019; Ryan et al. 2013), which suggested that bullying and aggressive behaviors can be consequences of ACEs (e.g. parental violence and neglect). Based on the spillover hypothesis, which purports that mood, affect, or behavior transfers from one setting to the next (Almeida et al. 1999), children experience and learn aggressive behaviors as well as coercive control and psychological control from their parents and exercise such behaviors in settings outside the home, such as school and become perpetrators themselves. Moreover, the emotion and stress of marital relationships and inter-parental conflict affect other relationships in the family system, such as the parent-child relationship (Erel and Burman 1995; Krishnakumar and Buehler 2000). Based on social learning theory (Bandura 1977), negative and harsh parenting behaviors are associated with children’s aggressive behaviors via observational learning, modeling, and coercive family processes (Parke et al. 1988; Patterson 1982). Thus, we hypothesized that children who experienced higher levels of physical and psychological violence and neglect as well as dysfunctional family environments (exposure to inter-parental violence and parental substance use) have higher risk of being aggressive and bullying others than children who have not had these experiences.
Psychological Problems and Bullying Perpetration
Bullying is a group phenomenon and is also influenced by peer behaviors and reactions (Swearer et al. 2010). Previous research on bullying perpetration focused more on their social experiences and shown that bully perpetrators are perceived by their peers as attractive, popular, and powerful (Graham 2010; Rodkin et al. 2006; Swearer et al. 2010; Thunfors and Cornell 2008; Vaillancourt et al. 2003) and associated with high social intelligence (Kaukiainen et al. 1999). However, although bullying perpetrators may be popular and powerful, they could also experience mental health problems and psychological symptoms. A study in Finland found that anxiety, depression and psychosomatic symptoms were most frequent among bully-victims and equally common among bullies and victims (Kaltiala-Heino et al. 2000). They suggested that bullying should be seen as an indicator of risk of mental disorders in adolescence. A study in New York found that frequent exposure to victimization or bullying others was related to high risks of depression and suicide ideation and attempts compared with adolescents not involved in bullying behaviors (Klomek et al. 2007). In a sample of Midwestern middle school students in U.S., bullies and bully-victims were more likely to be depressed than victims and no status students. And, victims and bully-victims were more likely to experience anxious symptoms than bullies and no status students (Swearer et al. 2001). Although most of the studies using screening tools (survey questions) as measures of mental health, some studies using doctors’ diagnosis for measuring mental health. A study in a large-scale national sample found that children (ages 6–17) with a diagnosis of depression and anxiety had a threefold increased odds of being a bully (Turcotte Benedict et al. 2015). Comparing to depression and anxiety, PTSD was relatively less studied for its influences on bullying perpetration among children. One study using data from a nationally-representative survey of the American adults revealed high rates of psychiatric disorders among individuals who endorsed a past-year history of bullying perpetration and found strong associations between PTSD and bullying perpetration (McMillan et al. 2016); the results indicate that adults who reported engaging in bullying behaviors were more likely than those who did not engage in bullying behaviors to experience panic disorder (odds ratio (OR) = 4.58), social phobia (OR = 3.75), and PTSD (OR = 3.72). The internalizing problems were associated with externalizing problems. A study in Italian students (ages 11–18) found that the bullies and bully-victims reported higher levels of PTSD (Baldry et al. 2019). Therefore, we hypothesize that children who have higher levels of PTSD are more likely to exhibit bullying perpetration than children who do not have high levels of PTSD.
The Current Study
The mechanisms involved in the linkage between child maltreatment/ACEs and externalizing behaviors are not well understood and require an explanation of such maltreatment and behavioral problem associations. Not only does the current study provide opportunities for capturing the associations among these variables but it also explores possible mechanism involved in such associations. We hypothesize that various types of child maltreatment and dysfunctional family environments (recognized as ACEs) have direct effects on adolescent bullying perpetration and PTSD symptoms, and that PTSD mediates the associations between the ACEs and bullying perpetration. In other words, children who have had adverse experiences are at greater risk for PTSD symptoms than children without ACEs, and, in turn, suffering from PTSD leads them to be at greater risk of exhibiting bullying perpetration. This study provides useful evidence-based information about the significant roles of ACEs and psychological trauma in order to highlight the importance of tackling and healing such psychological trauma to reduce bullying behavior in children.
Method
Participants
We collected data from a nation-wide, proportionately stratified, random sample of 6233 fourth-grade students (ages 10–11) in Taiwan in 2014 as part of a project of the Longitudinal Study of Children’s and Adolescents’ Family and Social Experiences (LSCAFSE). We stratified the sample by geographical location across Taiwan (19 counties or cities in total) and randomly selected districts to increase representation. The final sample of this study consisted of 6233 fourth-grade students who had parental consent for participation and whose data were valid. The participants were equally distributed by gender (50% male and 50% female).
Procedure
The present study received approval from the Research Ethics Committee of National Taiwan University Hospital prior to sampling and data collection. Informed consent was obtained from all individual participants and their parents. Confidentiality of data and voluntary participation were emphasized. Participants were also informed about their rights to withdraw at any time. Self-report questionnaires were distributed to consenting students in group sessions at schools. Finally, the research assistants gave a small gift (a set of stationeries in a pencil bag) to each student who completed the survey to express appreciation for their time and effort.
Measures
We assessed the children’s experiences of child maltreatment (physical and psychological neglect, physical and psychological abuse) and dysfunctional family environment (parental substance abuse and exposure to inter-parental violence) and children’s bullying perpetration using self-reported survey responses. The questionnaire was examined for content validity by a group of seven multidisciplinary experts (4 child development scholars, 1 sociologist, 1 clinical social worker, and 1 statistician), and was administered to 726 pilot-study participants. The LSCAFSE research team modified some of the measures according to the results of the pilot study’s internal consistency analysis and principal component analysis as well as suggestions from scholars and other experts. The psychometrics of these measures were examined again after the formal data were collected. The findings support those of previous studies that have shown that school-age children (especially ages 8 to 11) can reliably and validly report their own health status and quality of life (Riley 2004; Varni et al. 2007).
Bullying Perpetration
The bullying scale used in this study is composed of seven items to assess participants’ experiences of interacting with others in the past year, including verbal insult(s), threat(s), extortion, property damage, physical violence, and relational aggression. Sample questions are: In the past year, I spread rumor or said something bad behind someone’s back to hurt him/her; I intentionally isolated my peers and asked others not to talk/play with them; I threated my peers; I hit, kicked, pushed, pinched or strangled my peers, etc. Participants used a 5-point scale (0 = never, 1 = 1–2 times, 2 = 3–5 times, 3 = 6–10 times, and 4 = more than 10 times) to rate the frequency of bullying behaviors. The scale is based on several existing instruments with modifications, and previous studies have shown its adequate reliability (Chen and Astor 2012; Furlong et al. 2005; Wei et al. 2010). Cronbach’s alpha (α) was used to calculate the reliability of the scale. The scores were internally consistent (α = .82).
Physical and Psychological Neglect
We used the 6-item Neglect Subscale of the International Society for the Prevention of Child Abuse and Neglect (ISPCAN) Child Abuse Screening Tool Children’s Version (ICAST-C (Zolotor et al. 2009) to define psychological neglect and physical neglect in the past year. We added one more item to account for children who are left alone at home. Participants used a 5-point scale (0 = never, 1 = seldom, 2 = sometimes, 3 = very often, and 4 = always) to rate the frequency of parental psychological neglect and another 5-point scale (0 = never, 1 = 1–2 times, 2 = 3–5 times, 3 = 6–10 times, and 4 = more than 10 times) to rate the frequency of physical neglect by their parents. Higher scores indicate more severe child neglect. The scores were internal consistent for the overall neglect scale (α = .70), the psychological neglect subscale (α = .65), and the physical neglect subscale (α = .61).
Physical and Psychological Abuse
First, we assessed physical abuse using seven modified Physical Assault Scale items of the Childhood Experiences of Violence Questionnaire (CEVQ) (Walsh et al. 2008) and Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) (Runyan et al. 1998). Participants used a 5-point scale (from 1 = never to 5 = more than 10 times) to rate the frequency of parental physical abuse in the past year. The physical abuse scale scores demonstrate strong internal consistency (α = .82). Second, the research team developed a 4-item psychological abuse scale based on the Child Abuse Screening Tool Children’s Version (ICAST-C) used in ISPCAN study (Zolotor et al. 2009). The sample questions include those that involve swearing at the child, threatening to kick out the child from home, and saying “I wish you were never born” or “I hope you die” to the child. Participants used a 5-point scale (from 0 = never to 4 = more than 10 times) to rate the frequency of psychological abuse in the past year. The scores were internally consistent (α = .76).
Dysfunctional Family Environment
The two variables related to dysfunctional family environment in the current study are exposure to inter-parental violence and parental substance abuse. First, we assessed exposure to and witness of inter-parental violence using two items from the CEVQ: (1) ‘How many times have you seen or heard either of your parents say hurtful or mean things to each other or to another adult in your home?’ and (2) ‘How many times have you seen or heard either of your parents hit the other or another adult in your home?’ Participants used a 5-point scale (1 = never, 2 = 1–2 times, 3 = 3–5 times, 4 = 6–10 times, 5 = more than 10 times) to rate the frequency of exposure to inter-parental violence. Test-retest reliability of the stem items exceeded .81. The kappa coefficient of agreement for the classification of domestic violence indicates excellent intra-rater reliability (Landis and Koch 1977). Second, we defined parental substance abuse by asking the question: ‘How many times have you ever felt afraid of either of your parent’s behavior after their use of alcohol or drugs?’ Children used a 5-point scale (from 1 = never to 5 = more than 10 times) to rate the frequency of exposure to a dysfunctional family environment because of parental substance abuse from their perspectives. Although there is a limitation for the single-question test, the single-question alcohol and drug-use screening test design has been validated in previous research (Smith et al. 2009, 2010).
PTSD
We assessed children’s symptoms associated with traumatic experiences using the Chinese version of the UCLA PTSD Reaction Index for DSM-IV (Chen et al. 2002; Steinberg et al. 2004). Participants used a 5-point Likert scale (from 0 = never to 4 = most of the time) to rate the frequency of experiencing each symptom during the previous month. In order to reduce the time needed to complete the questionnaire, we deleted five items (items 11, 14, 20, 21, and 22) from the original scale according to the factor analysis results from the pilot study; therefore, the current study used only 17 items. The adolescent version of the Chinese PTSD scale has been validated for children in the fourth grade (Chen et al. 2002). The PTSD score was computed using the means of all 17 responses. Higher scores reflect greater post-traumatic symptom severity. The PTSD scale scores showed strong reliability for the present sample (α = .89).
Statistical Analysis
We performed statistical analysis using SPSS for Windows, version 24. First, we employed descriptive statistics to assess the distribution of bullying, four types of child maltreatment, and exposure to inter-parental violence, parental substance abuse, and children’s PTSD symptoms. Second, we conducted correlational analysis using the Pearson coefficient to illustrate interrelationships among each of the variables. Third, we conducted hierarchical regression to examine the effects of child maltreatment, dysfunctional family environment, and PTSD symptoms on children’s bullying, after controlling for gender. Finally, we used four-step regression analysis (Baron and Kenny 1986) to examine the mediating effect of PTSD on the associations between the ACE variables and child bullying. The four-step analysis parameters for the mediating effect are: (1) significant effect of predictor(s) on the outcome variable, (2) significant effect of predictor(s) on the mediator, (3) association between the mediator and the outcome when predictor(s) are controlled, and (4) reduction in the effect of predictor(s) on the outcome when the mediator is entered into the model. A Sobel test provided support for partial mediation (Sobel 1982).
Results
Descriptive Statistics and Correlations
Overall, 6233 participants completed the research questionnaire without withdrawal; 50% were girls and 50% were boys. Table 1 presents the correlation coefficients for all the study variables and the descriptive statistics of the means and standard deviations of the variables. Considering the cut-off point of 3 times or more happened in the past year, the prevalence of bullying perpetrations was 5%. More specifically, verbal (9.9%) and relational (6.4%) aggressive bullying behaviors were found to be the most prevalent, followed by physical (4.1%) and threaten (2%) bullying behaviors. Gender differences were found in verbal, physical, and threatened bullying behaviors, but no gender difference in relational aggressive bullying behaviors. Specifically, boys had higher scores of verbal bullying behaviors (M = 1.62, SD = 1.05) than girls (M = 1.41, SD = .81), t(5848) = 9.2, p < .001. Boys had higher scores of physical bullying behaviors (M = 1.27, SD = .73) than girls (M = 1.14, SD = .52), t(5623) = 7.64, p < .001.
Effects of Adverse Childhood Experiences on Bullying
Prior to conducting hierarchical multiple regression, we tested the relevant assumptions of this statistical analysis. First, the sample size of 6233 was deemed adequate, given that eight independent variables were to be included in the analysis (Tabachnick et al. 2007). Analysis of the correlations revealed that no independent variables were highly correlated, with the exception of the correlation between physical and psychological abuse (r = .68). As the collinearity statistics (i.e., tolerance and variance inflation factor) were all within accepted limits, the results indicate that multicollinearity was not a concern (Hair et al. 1998). The value of the Durbin-Watson test statistic was 1.91, which indicates that the residuals were not correlated (Durbin and Watson 1951). Additional analysis showed no significant results for demographic variables such as family incomes, parents’ education and marital status, thus we decided to remove these sociodemographic variables from the model, except gender.
We conducted hierarchical regression analysis to examine whether the four child maltreatment factors and two family-dysfunction variables and PTSD were significant contributors to children’s bullying perpetration after controlling for child gender. Table 2 summarizes the hierarchical regression analysis results. The demographic variable (gender) was entered into the regression model of child bullying in the first step (Model 1). A set of child maltreatment variables (i.e., physical and psychological neglect, physical and psychological abuse) was entered into the regression model in the second step (Model 2). A set of dysfunctional family environment variables (parental substance abuse and witness of inter-parental violence) was entered into the regression model in the third step (Model 3). Finally, the mental health variable, PTSD, was entered in the fourth and final step (Model 4).
The results show that the child maltreatment variables significantly contributed to the regression model, F (4, 6154) = 309.1, p < .001, and accounted for 17% of the variance in child bullying (∆R2 = .17, p < .001). Then, adding the two dysfunctional family environment variables significantly explained an additional 2% of the variance in child bullying; this change in R2 was significant: F (2, 6152) = 73.26, p < .001. Finally, the addition of PTSD to the regression model explained an additional 3% of the variance in child bullying; this change in R2 also was significant: F (1, 6151) = 254.9, p < .001. Taken together, these variables in the final model significantly explained 23% of the variance in child bullying. The regression coefficients in Model 3 (before adding the mediator) indicate that physical neglect (β = .08), psychological neglect (β = .07), physical abuse (β = .20), psychological abuse (β = .08), parental substance abuse (β = .10), and witness of inter-parental violence (β = .10) are positively associated with child bullying (all p < .001). Children who had experienced child maltreatment and had a dysfunctional family environment and PTSD symptoms were more likely to exhibit bullying perpetration than children without these experiences and conditions. Child gender was positively associated with bullying (β = .06, p < .001), indicating that boys reported more bullying perpetration than girls. Among all the ACE predictors of bullying used in this study (Model 3), physical abuse played the most significant role in child bullying, followed by parental substance abuse and witness of inter-parental violence. After adding PTSD to Model 4, PTSD played the most significant role in child bullying (β = .20, p < .001), followed by physical abuse (β = .18, p < .001), and the other ACE variables. When a stepwise elimination approach was applied, the set of child maltreatment variables was the best predictor of bullying and accounted for most of the variance in bullying (∆R2 = .17, p < .001; F (4, 6154) = 309.1, p < .001), followed by PTSD (∆R2 = .03, p < .001; F (1, 6151) = 254.9, p < .001).
Mediating Effect of PTSD Between ACEs and Child Bullying
To examine the potential mediating effect of PTSD on the relationships between the ACEs and child bullying, we conducted additional four-step regression analysis as described in the previous section. In Step One, after controlling for child gender, the four types of child maltreatment and two types of dysfunctional family environment were found to have significant direct effects on child bullying. Children who experienced maltreatment and lived in a dysfunctional family environment were more likely to exhibit bullying perpetration than children who did not. In Step Two, all child maltreatment and dysfunctional family environment variables were found to have significant direct effects on PTSD. In Step Three, PTSD (the mediator) was associated with bullying (the outcome) when all predictors were controlled. In Step Four, when PTSD (the mediator) was entered into the model, the effects of the predictors on child bullying (outcome) were reduced. After PTSD was added to the model, all ACE variables predicted child bullying with a reduction in the coefficient (see Model 4), and psychological neglect even became insignificant. These results indicate that PTSD fully mediated the association between psychological neglect and child bullying and partially mediated the associations between each of the other five ACE variables and bullying. The Sobel test results also support our finding that PTSD mediated the effects of these ACE variables (physical neglect, psychological neglect, physical abuse, psychological abuse, parental substance abuse, and exposure to interparental violence) on child bullying (Z = 4.72, 15.73, 5.49, 3.14, 2.41, and 9.14, respectively, p < .001). Children who had adverse experiences in their families were more likely to have PTSD symptoms than those who did not and, in turn, their psychological trauma led to greater risk of exhibiting bullying perpetration toward others.
Discussion and Implications
Using hierarchical regression, we examined the effects of child maltreatment, dysfunctional family environment, and PTSD symptoms on children’s bullying after controlling for gender. We also examined the possible mediating effect of PTSD on the associations between ACE variables and child bullying to explore and understand the pathways and mechanisms that lead from adverse experiences to psychological trauma and then to externalizing problems in children in Taiwan.
Consistent with the hypotheses, we found direct effects of various types of ACEs on child bullying and PTSD symptoms. Moreover, we found evidence that PTSD mediates the relationships between six types of ACEs and child bullying perpetration in a national representative sample in Taiwan. This study provides an important extension of previous work that explored the links between ACEs and externalizing problems to explore a potential underlying mechanism, PTSD, which is a form of psychological trauma. ACEs are traumatic events that have negative and long-lasting effects on students’ health and well-being and their ability to thrive in school, at home, and throughout their life. This study’s results can inform evidence-based practices and show that children who have had ACEs, such as neglect, abuse, and family dysfunction, are at risk of exhibiting internalizing problem (PTSD) and externalizing problem (bullying) and confirm the pathway from ACEs to bullying through PTSD.
Promoting trauma-sensitive policies in schools has the greatest potential to impact all students positively. Such policies promote shared understanding among all school staff members and administrators about the impact of trauma and ACEs on students, improve access to comprehensive mental and behavioral health services to all students, and adopt positive discipline and restorative justice practices in schools (National Association of School Psychologists 2019). Restorative justice emphasizes and promotes trauma-informed and resilience-oriented practices for individuals and school/community empowerment. Children who are victims of family violence (e.g., physical and psychological abuse and witness to domestic violence) may react defensively and aggressively in response to perceived blame and attack (Lereya et al. 2013; Luke and Banerjee 2013). Thus, prevention and intervention should shift the focus from punishment to healing and recovery, and the conversation should be changed from “what’s wrong with you?” to “what happened to you?”
The results obtained in the current study demonstrate how adverse trauma and experiences can impact children’s mental health (PTSD) and then lead to behavioral problems. Trauma is an exceptional experience in which powerful and dangerous stimuli overwhelm and impair the child’s capacity to self-regulate and self-sooth (Cook et al. 2017). Therefore, developing and establishing trauma-sensitive policies within schools are critical initiatives. From the perspective of trauma-informed practice, trauma-sensitive policies in schools would allow the focus to be more on healing and growth than punishment to combat child bullying. A perpetrator of school bullying can also be a victim of family violence and neglect. When children have a trauma history of family violence and neglect or live in a dysfunctional family environment, they may be easily triggered and more likely to react intensely and negatively. They may have difficulties in self-regulation and a low ability to think through consequences before acting. Consequently, traumatized children may behave in ways that appear oppositional and volatile. Children who are victims of family violence (e.g., physical and psychological abuse and witness to domestic violence) may react defensively and aggressively in response to perceived blame and attack. Using trauma-informed strategies in schools can help to remove barriers for those students who are in need of extra support. Trauma-sensitive strategies can reveal the motivation behind students’ behaviors by using trauma-informed behavioral assessments, learning how early trauma impacts learning and behavior, and developing trauma-sensitive school-wide approaches to discipline (Attachment and Trauma Network 2019). By understanding and responding to trauma, school administrators, teachers, and staff can help reduce its negative impacts, which include bullying, and create a more positive school environment.
Limitations and Future Study
The limitations of this study need to be acknowledged. The analyses were limited by the cross-sectional nature of the current data, as longitudinal research would be more beneficial for understanding the complex and reciprocal relationships among these study variables. Second, the data were collected from a single source, namely self-reports by children for both predictors and outcome, which raises concerns of shared method variance. Thus, future research should collect data from both children and parents to reduce measurement bias and increase the validity of the findings. Third, parental substance abuse was measured by a single question: ‘How many times have you ever felt afraid of either of your parent’s behavior after their use of alcohol or drugs?’ Participants used a 5-point scale (from 1 = never to 5 = more than 10 times) to rate the frequency of exposure to a dysfunctional family environment because of parental substance abuse These data could include longitudinal data to investigate the trajectories of bullying, PTSD symptoms, and each dimension of ACEs for comparison against baseline data. In addition to parental violence and inter-parental violence as family-violence predictors in this study, future study can include sibling bullying as another form of family-violence predictor of peer bullying. Finally, the group of bully-victims was not able to be identified using the measures in this study. This subgroup of children involving in bullying can be at the worst situation in terms of their mental health (Swearer et al. 2001). Future research can account for this group of children that are considered bully-victims.
Conclusions
In this study, children with higher levels of bullying perpetration reported more family violence and neglect at home and parental substance abuse problems than children who did not self-report as engaging in bullying perpetration. Among fourth-graders in Taiwan, children who reported these ACEs were more likely to have PTSD symptoms and resultant externalizing problems that increase their risk of exhibiting bullying perpetration toward others. That is, this study found that ACEs indirectly affect child bullying through PTSD. In addition to implementing behavioral modeling and corrections to combat bullying in schools, prevention and intervention efforts should address and screen for ACEs to tackle psychological problems and their effects. In summary, the current study informs evidence-based practices and demonstrates pathways from ACEs to child bullying through PTSD in a nationally representive sample in Taiwan and has implications for promoting trauma-sensitive policies in schools.
References
Afifi, T. O., McMillan, K. A., Asmundson, G. J. G., Pietrzak, R. H., & Sareen, J. (2011). An examination of the relation between conduct disorder, childhood and adulthood traumatic events, and posttraumatic stress disorder in a nationally representative sample. Journal of Psychiatric Research, 45, 1564–1572. https://doi.org/10.1016/j.jpsychires.2011.08.005.
Allwood, M. A., & Widom, C. S. (2013). Child abuse and neglect, developmental role attainment, and adult arrests. Journal of Research in Crime and Delinquency, 50, 551–578. https://doi.org/10.1177/0022427812471177.
Almeida, D. M., Wethington, E., & Chandler, A. L. (1999). Daily transmission of tensions between marital dyads and parent–child dyads. Journal of Marriage and the Family, 61, 49–61. https://doi.org/10.2307/353882.
Attachment and Trauma Network (2019). ATN’s Trauma-Sensitive Schools. Retrieved from https://creatingtraumasensitiveschools.org/
Baldry, A. C., Sorrentino, A., & Farrington, D. P. (2019). Post-traumatic stress symptoms among Italian preadolescents involved in school and cyber bullying and victimization. Journal of Child and Family Studies, 28, 2358–2364. https://doi.org/10.1007/s10826-018-1122-4.
Balistreri, K. S., & Alvira-Hammond, M. (2016). Adverse childhood experiences, family functioning and adolescent health and emotional well-being. Public Health, 132, 72–78. https://doi.org/10.1016/j.puhe.2015.10.034.
Bandura, A. (1977). Social learning theory. Englewood Cliffs: Prentice Hall.
Barber, B. A., Kohl, K. L., Kassam-Adams, N., & Gold, J. I. (2014). Acute stress, depression, and anxiety symptoms among English and Spanish speaking children with recent trauma exposure. Journal of Clinical Psychology in Medical Settings, 21, 66–71. https://doi.org/10.1007/s10880-013-9382-z.
Baron, R. M., & Kenny, D. A. (1986). The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality & Social Psychology, 51, 1173–1182. https://doi.org/10.1037/0022-3514.51.6.1173.
Chen, J. K., & Astor, R. A. (2012). School variables as mediators of personal and family factors on school violence in Taiwanese junior high schools. Youth & Society, 44, 175–200. https://doi.org/10.1037/e633562009-001.
Chen, J. K., & Avi Astor, R. (2010). School violence in Taiwan: examining how Western risk factors predict school violence in an Asian culture. Journal of Interpersonal Violence, 25, 1388–1410. https://doi.org/10.1177/0886260509354576.
Chen, S. H., Lin, Y. H., Tseng, H. M., & Wu, Y. C. (2002). Post-traumatic stress reactions in children and adolescents one year after the 1999 Taiwan Chi-Chi earthquake. Journal of the Chinese Institute of Engineers, 25, 597–608. https://doi.org/10.1080/02533839.2002.9670734.
Cook, A., Spinazzola, J., Ford, J., Lanktree, C., Blaustein, M., Cloitre, M., et al. (2017). Complex trauma in children and adolescents. Psychiatric Annals, 35, 390–398.
Durbin, J., & Watson, G. S. (1951). Testing for serial correlation in least squares regression. II. Biometrika, 38, 159–177. https://doi.org/10.2307/2332391.
Erel, O., & Burman, B. (1995). Interrelatedness of marital relations and parent-child relations: a meta-analytic review. Psychological Bulletin, 118, 108–132. https://doi.org/10.1037/0033-2909.118.1.108.
Furlong, M. J., Greif, J. L., Bates, M. P., Whipple, A. D., Jimenez, T. C., & Morrison, R. (2005). Development of the California school climate and safety survey-short form. Psychology in the Schools, 42, 137–149. https://doi.org/10.1002/pits.20053.
Garnefski, N., & Kraaij, V. (2014). Bully victimization and emotional problems in adolescents: moderation by specific cognitive coping strategies? Journal of Adolescence, 37, 1153–1160. https://doi.org/10.1016/j.adolescence.2014.07.005.
Graham, S. (2010). What educators need to know about bullying behaviors. Phi Delta Kappan, 92, 66–69. https://doi.org/10.1177/003172171009200112.
Hair, J. F., Anderson, R. E., Tatham, R. L., & Black, W. C. (1998). Multivariate data analysis. New Jersey: Englewood Cliff.
Harford, T. C., Yi, H.-y., & Grant, B. F. (2014). Associations between childhood abuse and interpersonal aggression and suicide attempt among U.S. adults in a national study. Child Abuse & Neglect, 38, 1389–1398. https://doi.org/10.1016/j.chiabu.2014.02.011.
Kaltiala-Heino, R., Rimpelä, M., Rantanen, P., & Rimpelä, A. (2000). Bullying at school—an indicator of adolescents at risk for mental disorders. Journal of Adolescence, 23, 661–674. https://doi.org/10.1006/jado.2000.0351.
Kaukiainen, A., Björkqvist, K., Lagerspetz, K., Österman, K., Salmivalli, C., Rothberg, S., & Ahlbom, A. (1999). The relationships between social intelligence, empathy, and three types of aggression. Aggressive Behavior, 25, 81–89.
Klomek, A. B., Marrocco, F., Kleinman, M., Schonfeld, I. S., & Gould, M. S. (2007). Bullying, depression, and suicidality in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 46, 40–49.
Krishnakumar, A., & Buehler, C. (2000). Interparental conflict and parenting behaviors: a meta-analytic review. Family Relations, 49, 24–44. https://doi.org/10.1111/j.1741-3729.2000.00025.x.
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 159–174. https://doi.org/10.2307/2529310.
Lereya, S. T., Samara, M., & Wolke, D. (2013). Parenting behavior and the risk of becoming a victim and a bully/victim: a meta-analysis study. Child Abuse & Neglect, 37, 1091–1108. https://doi.org/10.1016/j.chiabu.2013.03.001.
Luk, J. W., Wang, J., & Simons-Morton, B. G. (2010). Bullying victimization and substance use among US adolescents: mediation by depression. Prevention Science, 11, 355–359. https://doi.org/10.1007/s11121-010-0179-0.
Luke, N., & Banerjee, R. (2013). Differentiated associations between childhood maltreatment experiences and social understanding: a meta-analysis and systematic review. Developmental Review, 33, 1–28. https://doi.org/10.1016/j.dr.2012.10.001.
McMillan, K. A., Thorisdottir, A. S., & Asmundson, G. J. (2016). Psychiatric correlates of past year adult bullying behaviors: findings from the National Epidemiology Survey of Alcohol and Related Conditions. Psychiatry Research, 246, 745–749. https://doi.org/10.1016/j.psychres.2016.07.065.
Modecki, K. L., Minchin, J., Harbaugh, A. G., Guerra, N. G., & Runions, K. C. (2014). Bullying prevalence across contexts: a meta-analysis measuring cyber and traditional bullying. The Journal of Adolescent Health, 55, 602–611. https://doi.org/10.1016/j.jadohealth.2014.06.007.
Mumford, E. A., Taylor, B. G., Berg, M., Liu, W., & Miesfeld, N. (2019). The social anatomy of adverse childhood experiences and aggression in a representative sample of young adults in the US. Child Abuse & Neglect, 88, 15–27. https://doi.org/10.1016/j.chiabu.2018.10.016.
National Association of School Psychologists (2019). Trauma-sensitive schools. Retrieved from https://www.nasponline.org/resources-and-publications/resources-and-podcasts/mental-health/trauma-sensitive-schools
Olweus, D. (2013). School bullying: development and some important challenges. Annual Review of Clinical Psychology, 9, 751–780. https://doi.org/10.1146/annurev-clinpsy-050212-185516.
Parke, R. D., MacDonald, K. B., Beitel, A., & Bhavnagri, N. (1988). The role of the family in the development of peer relationships. In R. D. Peters & R. J. McMahon (Eds.), Social learning and systems approaches to marriage and the family (pp. 17–44). Philadelphia: Brunner/Mazel.
Patterson, G. R. (1982). Coercive family process: A social learning approach (Vol.3). Eugene: Castalia.
Perez, N. M., Jennings, W. G., & Baglivio, M. T. (2018). A path to serious, violent, chronic delinquency: the harmful aftermath of adverse childhood experiences. Crime & Delinquency, 64, 3–25. https://doi.org/10.1177/0011128716684806.
Reed, K. P., Nugent, W., & Cooper, R. L. (2015). Testing a path model of relationships between gender, age, and bullying victimization and violent behavior, substance abuse, depression, suicidal ideation, and suicide attempts in adolescents. Children and Youth Services Review, 55, 128–137. https://doi.org/10.1016/j.childyouth.2015.05.016.
Riley, A. W. (2004). Evidence that school-age children can self-report on their health. Ambulatory Pediatrics, 4, 371–376. https://doi.org/10.1367/A03-178R.1.
Rodkin, P. C., Farmer, T. W., Pearl, R., & Acker, R. V. (2006). They’re cool: Social status and peer group supports for aggressive boys and girls. Social Development, 15, 175–204.
Runyan, D. K., Curtis, P., Hunter, W., Black, M. M., Kotch, J. B., Bangdiwala, S., et al. (1998). LONGSCAN: a consortium for longitudinal studies of maltreatment and the life course of children. Aggression and Violent Behavior, 3, 275–285.
Ryan, J. P., Williams, A. B., & Courtney, M. E. (2013). Adolescent neglect, juvenile delinquency and the risk of recidivism. Journal of Youth and Adolescence, 42, 454–465. https://doi.org/10.1007/s10964-013-9906-8.
Smith, P. C., Schmidt, S. M., Allensworth-Davies, D., & Saitz, R. (2009). Primary care validation of a single-question alcohol screening test. Journal of General Internal Medicine, 24, 783–788. https://doi.org/10.1007/s11606-009-0928-6.
Smith, P. C., Schmidt, S. M., Allensworth-Davies, D., & Saitz, R. (2010). A single-question screening test for drug use in primary care. Archives of Internal Medicine, 170, 1155–1160. https://doi.org/10.1001/archinternmed.2010.140.
Sobel, M. E. (1982). Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology, 13, 290–312.
Stapinski, L. A., Araya, R., Heron, J., Montgomery, A. A., & Stallard, P. (2015). Peer victimization during adolescence: concurrent and prospective impact on symptoms of depression and anxiety. Anxiety, Stress, & Coping, 28, 105–120. https://doi.org/10.1080/10615806.2014.962023.
Steinberg, A. M., Brymer, M. J., Decker, K. B., & Pynoos, R. S. (2004). The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports, 6, 96–100. https://doi.org/10.1007/s11920-004-0048-2.
Swearer, S. M., Song, S. Y., Cary, P. T., Eagle, J. W., & Mickelson, W. T. (2001). Psychosocial correlates in bullying and victimization: the relationship between depression, anxiety, and bully/victim status. Journal of Emotional Abuse, 2, 95–121. https://doi.org/10.1300/j135v02n02_07.
Swearer, S. M., Espelage, D. L., Vaillancourt, T., & Hymel, S. (2010). What can be done about school bullying? Linking research to educational practice. Educational Researcher, 39, 38–34. https://doi.org/10.3102/0013189x09357622.
Tabachnick, B. G., Fidell, L. S., & Ullman, J. B. (2007). Using multivariate statistics (Vol. 5). Boston: Pearson.
Thunfors, P., & Cornell, D. (2008). The popularity of middle school bullies. Journal of School Violence, 7, 65–82.
Turcotte Benedict, F., Vivier, P. M., & Gjelsvik, A. (2015). Mental health and bullying in the United States among children aged 6 to 17 years. Journal of Interpersonal Violence, 30, 782–795. https://doi.org/10.1177/0886260514536279.
Vaillancourt, T., Hymel, S., & McDougall, P. (2003). Bullying is power: Implications for school-based intervention strategies. Journal of Applied School Psychology, 19, 157–176.
Varni, J. W., Limbers, C. A., & Burwinkle, T. M. (2007). How young can children reliably and validly self-report their health-related quality of life? An analysis of 8,591 children across age subgroups with the PedsQL™ 4.0 Generic Core Scales. Health and Quality of Life Outcomes, 5, 1. https://doi.org/10.1186/1477-7525-5-1.
Walsh, C. A., MacMillan, H. L., Trocmé, N., Jamieson, E., & Boyle, M. H. (2008). Measurement of victimization in adolescence: development and validation of the childhood experiences of violence questionnaire. Child Abuse & Neglect, 32, 1037–1057. https://doi.org/10.1016/j.chiabu.2008.05.003.
Wei, H. S., Williams, J. H., Chen, J. K., & Chang, H. Y. (2010). The effects of individual characteristics, teacher practice, and school organizational factors on students’ bullying: a multilevel analysis of public middle schools in Taiwan. Children and Youth Services Review, 32, 137–143. https://doi.org/10.1016/j.childyouth.2009.08.004.
Zimmer-Gembeck, M. J., Geiger, T. C., & Crick, N. R. (2005). Relational and physical aggression, prosocial behavior, and peer relations: gender moderation and bidirectional associations. The Journal of Early Adolescence, 25, 421–452.
Zolotor, A. J., Runyan, D. K., Dunne, M. P., Jain, D., Peturs, H. P., Ramirez, C., et al. (2009). ISPCAN child abuse screening tool children’s version (ICAST-C): Instrument development and multi-national pilot testing. Child Abuse & Neglect, 33, 833–841. https://doi.org/10.1037/t27249-000.
Funding
This work was supported by the National Taiwan University (NTU) Children and Family Research Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hsieh, YP., Shen, A.CT., Hwa, HL. et al. Associations Between Child Maltreatment, Dysfunctional Family Environment, Post-Traumatic Stress Disorder and Children’s Bullying Perpetration in a National Representative Sample in Taiwan. J Fam Viol 36, 27–36 (2021). https://doi.org/10.1007/s10896-020-00144-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10896-020-00144-6