Abstract
Objectives
To determine use of 2-[N-(7-nitrobenz-2-oxa-1,3-diazol-4-yl)amino]-2-deoxy-D-glucose (2-NBDG) as a tracer for detection of hypermetabolic circulating tumor cells (CTC) by fluorescence imaging.
Procedures
Human breast cancer cells were implanted in the mammary gland fat pad of athymic mice to establish orthotopic human breast cancer xenografts as a mouse model of circulating breast cancer cells. Near-infrared fluorescence imaging of the tumor-bearing mice injected with 2-DeoxyGlucosone 750 (2-DG 750) was conducted to assess glucose metabolism of xenograft tumors. Following incubation with fluorescent 2-NBDG, circulating breast cancer cells in the blood samples collected from the tumor-bearing mice were collected by magnetic separation, followed by fluorescence imaging for 2-NBDG uptake by circulating breast cancer cells, and correlation of the number of hypermetabolic circulating breast cancer cells with tumor size at the time when the blood samples were collected.
Results
Human breast cancer xenograft tumors derived from MDA-MB-231, BT474, or SKBR-3 cells were visualized on near-infrared fluorescence imaging of the tumor-bearing mice injected with 2-DG 750. Hypermetabolic circulating breast cancer cells with increased uptake of fluorescent 2-NBDG were detected in the blood samples from tumor-bearing mice and visualized by fluorescence imaging, but not in the blood samples from normal control mice. The number of hypermetabolic circulating breast cancer cells increased along with growth of xenograft tumors, with the number of hypermetabolic circulating breast cancer cells detected in the mice bearing MDA-MB231 xenografts larger than those in the mice bearing BT474 or SKBR-3 xenograft tumors.
Conclusions
Circulating breast cancer cells with increased uptake of fluorescent 2-NBDG were detected in mice bearing human breast cancer xenograft tumors by fluorescence imaging, suggesting clinical use of 2-NBDG as a tracer for fluorescence imaging of hypermetabolic circulating breast cancer cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Circulating tumor cells (CTC) have emerged as a useful prognostic biomarker for prediction of the risk of metastasis in patients diagnosed with breast cancer and many other solid tumors. Detection of CTC in patients diagnosed with breast cancer is associated with risk for development of metastasis and poor prognosis [1–3].
In addition to CTC numbers, viability, glucose metabolism, and other functional activity of CTC are important factors governing capability of CTC to survive and grow at a distant site to establish metastasis [4]. Several dyes are available for monitoring and detecting viable CTC using the CellSearch System [5, 6] or flow cytometry [7, 8]. These dyes include 7-amino-actinomycin D (7-ADD) and annexin V [9, 10], and calcein AM and ethidium homodimer −1 (Calcein/EthD-1) which are routinely used for evaluation of cell viability in flow cytometry [11, 12]. In addition, attempts were made to characterize CTC by molecular profiling of various biomarkers [13–15]. However, glucose metabolism and other metabolic activities of CTC remains poorly understood. There is a need to develop tracers, sensors, or probes for assessing glucose metabolism and other metabolic activities of CTC.
2-NBDG is a fluorescence-labeled 2-deoxy-glucose analog useful as a tracer for evaluation of cellular glucose metabolism [16, 17]. 2-NBDG was used as a tracer for assessing glucose metabolism of tumor cells and tumor cells showed increased uptake of 2-NBDG compared with cellular uptake of this tracer by nonmalignant mammalian cells [18, 19]. This study aims to determine feasibility and utility of 2-NBDG as a tracer for detecting and assessing glucose metabolism of CTC, using mouse xenograft models of circulating breast cancer cells.
Materials and Methods
Cells, Animals, and Establishment of Tumor Xenografts
Human breast cancer cell lines (MDA-MB-231, SKBR3 and BT474) with expression of epithelial cell adhesion molecule (EpCAM) were purchased from American Type Culture Collection (ATCC) and cultured under conditions suggested by ATCC. Large number of circulating breast cancer cells were detected in blood samples from the mice bearing xenograft tumors derived from MDA-MB-231 cells, compared with smaller number of circulating breast cancer cells in the mice bearing xenograft tumors derived from SKBR3 breast cancer cells [20]. Human breast cancer cells were cultured as described previously [20], using Leibovitz’s L-15 medium for MDA-MB-231 cells, McCoy’s 5A medium for SKBR3 cells, and Hybri-Care medium for BT474 cells, supplemented with 10 % fetal bovine serum. Experiments using animals were conducted in a protocol approved by the Institutional Animal Care and Use Committee at UT Southwestern Medical Center. To establish a mouse xenograft model of circulating breast cancer cells, human breast cancer cells were implanted in the mammary gland fat pads of athymic nu/nu mice (female, 5–6 week old) purchased from National Cancer Institute (Bethesda, MD), in a method described previously [20]. Tumor size was monitored in two dimensions with a caliper and tumor volume was calculated as length (mm) x width (mm) x width (mm) x 0.5.
Near-Infrared Fluorescence Imaging of Tumor-Bearing Mice
XenoLight RediJect 2-DeoxyGlucosone 750 (2-DG-750), a near-infrared fluorescent probe was purchased from Caliper Life Sciences (Hopkinton, MA). Near-infrared fluorescent 2-DG-750 has a peak excitation 745 nm and peak emission 780 nm. Near-infrared fluorescence imaging of the tumor-bearing mice was conducted with an IVIS Spectrum instrument (PerkinElmer, Waltham, MA). At 3 to 4 h post injection of 70 to 100 μL of fluorescent 2-DG-750, near-infrared fluorescence images of the tumor-bearing mice were obtained with indocyanine green/indocyanine green (ICG)/ICG) filter sets at a wave length of Ex745nm/Em820nm, in a protocol from the vendor (Caliper life Sciences). Near-infrared fluorescence images were processed and analyzed with Living Image® 4.2 software (PerkinElmer).
Fluorescence Imaging of Circulating Breast Cancer Cells with Increased Uptake of Fluorescent 2-NBDG
Starting at 1 week after implantation of tumor cells, mouse blood samples (100 μL/mouse) were collected by puncturing the mouse saphenous vein. The blood samples containing circulating breast cancer cells were incubated with 2-NBDG, a fluorescent glucose analogue purchased from Invitrogen (Carlsbad, CA), at a dose of 5 μg/100 μL blood, for 30 min in a dark incubator at 37 °C. Subsequently, circulating breast cancer cells were harvested with magnetic beads conjugated with anti-epithelial cell adhesion molecule (EpCAM) IgG in a protocol from the vendor (JSR Micro, Inc, Sunnyvale, CA), followed by fluorescence imaging of circulating breast cancer cells with cellular uptake of fluorescent 2-NBDG. Briefly, 1 μL of 1 % suspension of the magnetic beads was added to 100 μL of blood samples at the end of incubation with 2-NBDG, followed by incubation at 4 °C for 30 min with gentle shaking to facilitate binding of the magnetic beads to circulating breast cancer cells. Subsequently, the circulating breast cancer cells were collected from the blood by magnetic separation with a magnetic separation rack [Cell signaling, Danvers, MA], washed 3 times with PBS, and transferred to a 96-well plate after re-suspending the circulating breast cancer cells in 100 μl PBS. Uptake of 2-NBDG by circulating breast cancer cells was examined under a fluorescent microscope equipped with a 488 nm filter (Olympus). Large cells with fluorescent signals derived from cellular uptake of fluorescent 2-NBDG were counted as hypermetabolic circulating breast cancer cells, in comparison to small size of normal mouse blood cells (lymphocytes and RBC) showing no or little fluorescence signals of 2-NBDG. Total number of hypermetabolic circulating breast cancer cells in a blood sample was obtained by visual scanning of the whole area of the well of the 96 well plate with manual cell counter. The experiments were repeated three times.
Results
Variable Growth of Xenograft Tumors Derived from Different Human Breast Cancer Cell Lines
Orthotopic human breast cancer xenografts were established in mice (N = 9), following implantation of MDA-MB231 cells (N = 3), BT474 cells (N = 3), or SKBR-3 cells (N = 3) at the mammary gland fat. A group of mice (N = 3) without implantation of breast cancer cells was used as a normal control. Large xenograft tumors were established in all of mice implanted with MDA-MB231 (N = 3) or BT474 breast cancer cells (N = 3), and tumors reached about 8 to 10 mm at 7 weeks post-implantation of the tumor cells. In contrast, the xenograft tumors derived from SKBR-3 breast cancer cells (N = 3) grew slower than those of MDA-231 or BT474 xenograft tumors. The xenograft tumor in 1 of 3 mice implanted with SKBR-3 tumor cells reached about 5 mm in largest dimension at 7 weeks post implantation of the tumor cells, while only small, barely visible tumors were established in other 2 of 3 mice implanted with SKBR-3 breast cancer cells.
Visualization of Hypermetabolic Xenograft Tumors in Mice by 2-DG-750 Near-Infrared Fluorescence Imaging
Hypermetabolic xenograft tumors with increased uptake of 2-DG-750 were well visualized on near-infrared fluorescence images of the tumor-bearing mice obtained at 1 h post injection of the tracer. In the two mice with no visible tumors after implantation of SKBR-3 cells, near-infrared fluorescent signals could be detected at the mammary gland fat pad injection site, although the amount of fluorescent signals was smaller than that of larger BT474 xenograft tumors (Fig. 1). This suggested presence of small tumors or clusters of hypermetabolic SKBR-3 tumor cells at the mammary gland fat pad injection site.
Near-infrared fluorescence imaging of tumor-bearing mice. Representative Near-infrared fluorescence images of tumor-bearing mice obtained at 3 h post injection of 2-DG-750: 2-DG-750 near-infrared fluorescent signals were visualized at region of left mammary gland fat pad at 5 weeks post implantation of SKBR-3 tumor cells, indicating a small, hypermetabolic SKBR-3 xenograft tumor with uptake of 2-DG-750; b BT474 tumor with increased uptake of 2-DG-750 was visualized at region of left mammary gland fat pad, along with a small focus of 2-DG-750 fluorescent signal at right axilla, likely a lymph node metastasis. Excretory 2-DG-750 fluorescent signals were also visualized in the region of urinary bladder. EF: epi-fluorescence units
Visualization of Circulating Breast Cancer Cells with Increased Uptake of Fluorescent 2-NBDG by Fluorescence Imaging
Circulating breast cancer cells with increased uptake of 2-NBDG were detected in the blood samples of tumor-bearing mice following incubation of the blood samples with 2-NBDG and magnetic separation using magnetic beads conjugated with anti-EpCAM IgG. Circulating breast cancer cells with uptake of 2-NBDG were detected not only in the blood samples from the mice bearing visible SKBR-3 xenograft tumors, but also in the blood samples from the mice with no visible tumors after implantation of SKBR-3 tumor cells (Fig. 2a). Circulating breast cancer cells with uptake of 2-NBDG were also detected in the blood samples from the mice bearing MDA-MB-231 xenograft tumors (Fig. 2b), or BT474 xenograft tumors (Fig. 2c). No circulating breast cancer cells or epithelial cells with 2-NBDG uptake were detected in the blood samples from normal control mice (Fig. 2d). Circulating breast cancer cells with no increased uptake of 2-NBDG were noted in the blood samples from the tumor-bearing mice, which were estimated to comprise 20 % of epithelial cancer cells captured by magnetic separation and likely represent nonviable or apoptotic circulating breast cancer cells. Small numbers of mouse lymphocytes and red blood cells (RBC) were present in the suspension of circulating breast cancer cells and magnetic beads following magnetic separation. However, mouse lymphocytes and RBC could be easily differentiated from circulating breast cancer cells based on their morphological features, small size, and absence of uptake of 2-NBDG reflected by the absence of green fluorescent signals under a fluorescent microscope (Fig. 2). The size of the magnetic beads (2–4 μm) was even smaller than those of mouse lymphocytes (6–8 μm) and showed no significant non-specific binding of 2-NBDG [Fig. 2].
Fluorescence imaging of glucose metabolism in circulating breast cancer cells. Blood samples from tumor-bearing mice were incubated with fluorescent 2-NBDG and circulating breast cancer cells were collected by collection with magnetic beads conjugated with antibodies against EpCAM molecules on breast cancer cells, followed by fluorescent imaging with a fluorescence microscope. Representative fluorescence images show SKBR3 (a), MDA-MB-231 (b), and BT474 (c) circulating breast cancer cells with green fluorescent signals from cellular uptake of fluorescent 2-NBDG (400× magnification). No circulating breast cancer cells or epithelial cells with increased uptake of 2-NBDG were detected in the blood samples from normal control mice (d). No significant 2-NBDG fluorescent signals were observed with lymphocytes or magnetic beads present in the blood samples from tumor-bearing mice (a–c) or in the blood samples from normal control mice (d). Magnetic beads are marked by arrow head
Increase of Hypermetabolic Circulating Breast Cancer Cells along with Growth of Xenograft Tumors
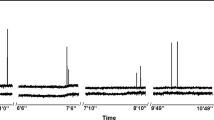
Circulating breast cancer cells with increased 2-NBDG uptake were detected in the blood samples of the tumor-bearing mice, starting at 2 weeks post implantation of the breast cancer cells. In the mice bearing xenograft tumors derived from MDA-MB-231 cells, single circulating breast cancer cell with uptake of 2-NBDG could be detected in the blood samples (100 μl blood/mouse) taken as early as 2 weeks post implantation of tumor cells, which gradually increased to 2 circulating breast cancer cells/100 μl blood at 3 weeks, 4 to 8 circulating breast cancer cells/100 μl blood at 4 weeks, 15 to 18 circulating breast cancer cells/100 μl blood at 5 weeks, 18 to 23 circulating breast cancer cells/100 μl blood at 6 weeks, and 33 to 45 circulating breast cancer cells/100 μl blood at 7 weeks post implantation of tumor cells. In the mice bearing xenograft tumors derived from BT474 cells, 2 to 3 circulating breast cancer cells with uptake of 2-NBDG were detected in 100 μl of blood samples taken at 2 weeks post implantation of tumor cells. The number of circulating breast cancer cells with uptake of 2-NBDG increased to 2 to 10 circulating breast cancer cell/100 μl blood at 3 weeks, 8 to 21 circulating breast cancer cells/100 μl blood at 4 weeks, 8 to 30 circulating breast cancer cells/100 μl blood at 5 weeks, 20 to 44 circulating breast cancer cells/100 μl blood at 6 weeks, and 44 to 70 circulating breast cancer cells/100 μl blood at 7 weeks post implantation of tumor cells. Although 1 to 2 circulating breast cancer cells/100 μl blood could also be detected at 2 weeks post implantation of tumor cells, a smaller number of circulating breast cancer cells with uptake of 2-NBDG was detected in the mice bearing small xenograft tumors derived from SKBR-3 cells, compared with the numbers of circulating breast cancer cells with uptake of 2-NBDG detected in the mice bearing larger MDA-MB-231 or BT474 tumors. At 3 weeks post implantation of SKBR-3 tumor cells, 2 to 6 circulating breast cancer cells with uptake of 2-NBDG were detected in 100 μl of blood samples, which increased to 4 to 10 circulating breast cancer cells/100 μl blood at 4 weeks, 7 to 24 circulating breast cancer cells/100 μl blood at 5 weeks, 13 to 38 circulating breast cancer cells/100 μl blood at 6 weeks, and 12 to 39 circulating breast cancer cells/100 μl blood at 7 weeks post implantation of tumor cells. The number of circulating breast cancer cells with uptake of 2-NBDG in the mouse with the largest tumor (5 × 5 mm) was highest among the circulating breast cancer cells with uptake 2-NBDG detected from 3 mice bearing SKBR-3 xenograft tumors. The number of circulating breast cancer cells with uptake of 2-NBDG increased along with increasing tumor size in the mice bearing MDA-MB-231, BT474, or SKBR-3 xenograft tumors (Fig. 3).
Correlation of number of circulating breast cancer cells with tumor growth. Increased number of MDA-MB-231 circulating breast cancer cells (a), SKBR-3 circulating breast cancer cells (b), or BT474 circulating breast cancer cells (c) with uptake of 2-NBDG were detected (graph at right), along with increase of tumor size or volume (graph at left), starting at 2 weeks post implantation of tumor cells. The size of SKBR-3 tumors and number of SKBR-3 circulating breast cancer cells with uptake of 2-NBDG were smaller than tumor size and number of circulating breast cancer cells with increased uptake of 2-NBDG derived from MDA-MB-231 or BT474 breast cancer cells
Discussion
Malignant transformation of cells is associated with increased aerobic glycolysis (Warburg effect), e.g., conversion of glucose to lactic acid in the presence of oxygen [21]. 2-deoxy-2-(18 F)fluoro-D-glucose (F-18 FDG), a glucose analogue, is widely used for quantification of glucose metabolism in vivo with positron emission tomography [22]. Positron emission tomography with F-18 FDG (F-18 FDG PET) is clinically accepted for diagnostic staging and restaging of breast cancer and many of other tumors [23–25]. However, F-18 FDG PET is limited by spatial resolution for detection and assessing glucose metabolism of small metastatic lesions in vivo or assessing glucose metabolism of circulating tumor cells in vivo at cellular level.
Fluorescent or near-infrared fluorescent glucose analogue molecules were used for assessing glucose metabolism of tumors in vivo [26–28]. 2-NBDG is a fluorescent glucose analogue tested for molecular imaging of glucose uptake in oral neoplasia by topical application of this fluorescent tracer [29], and differential imaging of cancerous tissue and normal tissue in a pathological tissue sample using a wide-field camera and filters to create multispectral tissue images [30]. However, 2-NBDG has limited use for detection and functional imaging of tumor lesions located deep in the body due to relatively poor tissue penetration of fluorescent photons. In the current study, hypermetabolic circulating breast cancer cells was detected by fluorescence imaging using 2-NBDG as a tracer. Following incubation of blood samples from tumor-bearing mice with 2-NBDG ex vivo, circulating breast cancer cells with increased uptake of 2-NBDG were harvested by magnetic separation and visualized by fluorescence imaging with a fluorescent microscope (Fig. 2). Circulating breast cancer cells with uptake of 2-NBDG were easily differentiated from non-viable or apoptotic circulating breast cancer cells with no increased uptake of 2-NBDG, and mouse lymphocytes or RBC with no increased uptake of 2-NBDG [Fig. 2]. There is no significant nonspecific binding of 2-NBDG to free magnetic beads following magnetic separation and washing with PBS. Using easily accessible blood samples, e.g. a “liquid biopsy”, fluorescence imaging of CTC may provide an attractive, alternative approach for noninvasive assessment of glucose metabolism of tumors at the cellular level.
Epithelial cell adhesion molecule (EpCAM) is an epithelial cell-specific surface glycoprotein highly expressed in breast cancer and other epithelial-origin cancer cells [31]. Using the Cell Tack system based on enumeration of CTC positive for EpCAM, CTC could be detected in only 60 % of patients with metastatic breast cancer [5, 6, 32]. It was suggested to use a combination of cytokeratin and EpCAM antibodies for detection of circulating tumor cells in blood of metastatic breast cancer patients [33, 34]. In conjunction with use of 7-ADD [9] or other probes, quantification of 2-NBDG uptake may be used to differentiate viable, hypermetabolic CTC from other blood cells or nonviable, apoptotic CTC by multi-color flow cytometry. 2-NBDG flow cytometry may be particularly useful for detecting and assessing glucose metabolism of CTC with little or no EpCAM expression following epithelial to mesenchymal transition, and other circulating blood cancer cells in leukemia, lymphoma, or neuroblastoma. Based on previous use of 2-NBDG for monitoring therapeutic effects of anticancer drugs on cancer cells [35], quantification of 2-NBDG uptake by CTC may be used for monitoring the therapeutic effects of systemic anticancer therapy on disseminated micro-metastasis, or leukemia and other blood cancers where use of conventional imaging techniques may be limited.
There is a difference in growth of the xenograft tumors derived from three different breast cancer cells lines (MDA-MB-231, BT474, or SKBR3) tested in current study, a finding similar to that described previously [20]. MDA-MB-231 and BT474 tumors grew faster than SKBR-3 tumors after implantation of the tumor cells. Visible tumors were established in all three mice implanted with MDA-MB-231 or BT474 tumor cells, but in only one of three mice implanted with SKBR3 cells. Also, the size of the visible SKBR-3 tumor was smaller than the size of the MDA-MB-231 and BT474 tumors. Along with growth of xenograft tumors, increased number of circulating breast cancer cells with increased uptake of 2-NBDG were detected in the blood samples from the tumor-bearing mice at a weekly interval. Hypermetabolic circulating breast cancer cells could be detected in the mice with no large visible tumors, but showing 2-DG 750 signals derived from viable tumor cells at implantation site on the Near-infrared fluorescence images [Fig. 1]. This suggested that hypermetabolic circulating breast cancer cells might be present and play an role in development of metastasis in the patients with small primary tumor lesions which might not be detected by conventional imaging. Overall, the number of circulating breast cancer cells with 2-NBDG uptake in the blood samples from the mice bearing visible or nonvisible SKBR-3 xenograft tumors was lower than those detected in the blood samples of the mice bearing MDA-MB-231 or BT474 xenograft tumors. This is in agreement with the findings by Eliane et al. [20]. Molecular mechanism related to difference of xenograft tumor growth and number of circulating breast cancer cells derived from these three breast cancer cells lines remained to be elucidated. It may be related to different cell proliferation and metastatic potential among these cell lines due to different gene expression profile. A correlation of the number of hypermetabolic CTC, and tumor size with subsequent development of metastasis in the patients will help to further determine the role of hypermetabolic CTC in pathogenesis of distant metastasis and use of hypermetabolic CTC as a prognostic biomarker.
In summary, hypermetabolic circulating breast cancer cells with increased uptake of 2-NBDG were detected and visualized by fluorescence imaging, using blood samples from a mouse xenograft model of breast cancer. The data from this preclinical study suggest that 2-NBDG could be used as a tracer for detection of hypermetabolic circulating breast cancer cells in patients diagnosed with breast cancer by fluorescence imaging in association with enrichment of CTC by magnetic separation or other methods of collection, or flow cytometry.
References
Cristofanilli M, Budd G, Ellis M et al (2004) Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med 351:781–791
Cristofanilli M, Hayes DF, Budd GT et al (2005) Circulating tumor cells: a novel prognostic factor for newly diagnosed metastatic breast cancer. J Clin Oncol 23:1420–1430
Pierga JY, Bidard FC, Mathiot C et al (2008) Circulating tumor cell detection predicts early metastatic relapse after neoadjuvant chemotherapy in large operable and locally advanced breast cancer in a phase II randomized trial. Clin Cancer Res 14:7004–7010
Bednarz-Knoll N, Alix-Panabières C, Pantel K (2011) Clinical relevance and biology of circulating tumor cells. Breast Cancer Res 13(6):228
Riethdorf S, Fritsche H, Muller V et al (2007) Detection of circulating tumor cells in peripheral blood of patients with metastatic breast cancer: a validation study of the cell search system. Clin Cancer Res 13:920–928
Sieuwerts AM, Kraan J, Bolt J et al (2009) Anti-epithelial cell adhesion molecule antibodies and the detection of circulating normal-like breast tumor cells. J Natl Cancer Inst 101:61–66
Wang N, Shi L, Li H et al (2012) Detection of circulating tumor cells and tumor stem cells in patients with breast cancer by using flow cytometry: a valuable tool for diagnosis and prognosis evaluation. Tumour Biol 33(2):561–569
Hristozova T, Konschak R, Budach V, Tinhofer I (2012) A simple multicolor flow cytometry protocols for detection and molecular characterization of circulating tumor cells in epithelial cancers. Cytometry A 81(6):489–495
Schmid I, Krall WJ, Uittenbogaart CH, Braun J, Giorgi JV (1992) Dead cell discrimination with 7-amino-actinomycin D in combination with dual color immunofluorescence in single laser flow cytometry. Cytometry 13(2):204–208
Zimmermann M, Meyer N (2011) Annexin V/7-AAD staining in keratinocytes. Methods Mol Biol 740:57–63
O’Brien MC, Bolton WE (1995) Comparison of cell viability probes compatible with fixation and permeabilization for combined surface and intracellular staining in flow cytometry. Cytometry 19(3):243–255
Shenkin M, Babu R, Maiese R (2007) Accurate assessment of cell count and viability with a flow cytometer. Cytometry B Clin Cytom 72(5):427–432
Powell AA, Talasaz AH, Zhang H et al (2012) Single cell profiling of circulating tumor cells: transcriptional heterogeneity and diversity from breast cancer cell lines. PLoS One 7(5):e33788
Nadal R, Fernandez A, Sanchez-Rovira P et al (2012) Biomarkers characterization of circulating tumor cells in breast cancer patients. 14(3):R71
de Albuquerque A, Kaul S, Breier G, Krabisch P, Fersis N (2012) Multimarker analysis of circulating tumor cells in peripheral blood of metastatic breast cancer patients: A stem forward in personalized medicine. Breast Care (Basel) 7(1):7–12
Yoshioka K, Takahashi H, Homma T et al (1996) A novel fluorescent derivative of glucose applicable to the assessment of glucose uptake activity of Escherichia coli. Biochim Biophys Acta 1289(1):5–9
Yoshioka K, Saito M, Oh KB et al (1996) Intracellular fate of 2-NBDG, a fluorescent probe for glucose uptake activity in Escherichia coli cells. Biosci Biotechnol Biochem 60:1899–1901
O’Neil RG, Wu L, Mullani N (2005) Uptake of a fluorescent deoxyglucose analog (2-NBDG) in tumor cells. Mol Imaging Biol 7(6):388–392
Zou C, Wang Y, Shen Z (2005) 2-NBDG as a fluorescent indicator for direct glucose uptake measurement. J Biochem Biophys Methods 64:207–215
Eliane JP, Repollet M, Luker KE et al (2008) Monitoring serial changes in circulating human breast cancer cells in murine xenograft models. Cancer Res 68(14):5529–5532
Warburg O, Wind F, Negelein E (1927) The metabolism of tumors in the body. J Gen Physiol 8(6):519–530
Som P, Atkins HL, Bandoypadhyay D et al (1980) A fluorinated glucose analog, 2-fluoro-2-deoxy-D-glucose [18 F]: nontoxic tracer for rapid tumor detection. J Nucl Med 21:670–675
Wahl RL, Cody RL, Hutchins GD, Mudgett EE (1991) Primary and metastatic breast carcinoma: initial clinical evaluation with PET with the radiolabeled glucose analogue 2-[F-18]-fluoro-2-deoxy-D-glucose. Radiology 179(3):765–770
Avril N, Menzel M, Dose J et al (2001) Glucose metabolism of breast cancer assessed by 18 F-FDG PET: histologic and immunohistochemical tissue analysis. J Nucl Med 42(1):9–16
Biersack HJ, Bender H, Palmedo H (2004) FDG-PET in monitoring therapy of breast cancer. Eur J Nucl Med Mol Imaging Suppl. 1:S112–S117
Yamada K, Saito M, Matsuoka H, Inagaki N (2007) A real-time method of imaging glucose uptake in single, living mammalian cells. Nat Protoc 2(3):753–762
Cheng Z, Levi J, Xiong Z et al (2006) Near-infrared fluorescent deoxyglucose analogue for tumor optical imaging in cell culture and living mice. Bioconjugate Chem 17:662–669
Kovar JL, Volcheck W, Sevick-Muraca E, SimpsonMA ODM (2009) Characterization and performance of a near-infrared 2-deoxyglucose optical imaging agent for mouse cancer models. Anal Biochem 384(2):254–262
Nitin N, Carlson AL, Muldoon T et al (2009) Molecular imaging of glucose uptake in oral neoplasia following topical application of fluorescently labeled deoxy-glucose. Int J Cancer 11:2634–2642
Langsner RJ, Middleton LP, Sun J et al (2011) Wide-field imaging of fluorescent deoxy-glucose in ex vivo malignant and normal breast tissue. Biomedical Optics Express 2(6):1514–1523
Izar M, Winter MJ, de Boer CJ, Litvinov SV (1999) The biology of the 17-1A antigen (Ep-CAM). J Mol Med (Berl) 77(10):699–712
Witzig TE, Bossy B, Kimlinger T et al (2002) Detection of circulating cytokeratin-positive cells in the blood of breast cancer patients using immunomagnetic enrichment and digital microscopy. Clin Cancer Res 8:1085–1091
Königsberg R, Obermayr E, Bises G et al (2011) Detection of EpCAM positive and negative circulating tumor cells in metastatic breast cancer patients. Acta Oncol 50(5):700–710
Weissenstein U, Schumann A, Reif M, Link S, Toffol-Schmidt UD, Heusser P (2012) Detection of circulating tumor cells in blood of metastatic breast cancer patients using a combination of cytokeratin and EpCAM antibodies. BMC Cancer 12(1):206
Millon SR, Ostrander JH, Brown JQ, Raheja A, Seewaldt VL, Ramanujam N (2011) Uptake of 2-NBDG as a method to monitor therapy response in breast cancer cell lines. Breast Cancer Res Treat 126(1):55–62
Acknowledgments
This study was supported by a grant from the Department of Defense CDMRP BCRP (W81XWH1110188) to F.P., and a faculty research start-up grant to F. P. from the Harold C. Simmons Comprehensive Cancer Center, University of Texas Southwestern Medical Center at Dallas, Texas, USA. Imaging infrastructure is provided by Southwestern Small Animal Imaging Research Program supported in part by U24 CA126608 and Simmons Cancer Center (P30 CA142543).
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cai, H., Peng, F. 2-NBDG Fluorescence Imaging of Hypermetabolic Circulating Tumor Cells in Mouse Xenograft model of Breast Cancer. J Fluoresc 23, 213–220 (2013). https://doi.org/10.1007/s10895-012-1136-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10895-012-1136-z