Abstract
Plant secondary metabolites (PSMs) are a major constraint to the ingestion of food by folivorous and browsing herbivores. Understanding the way in which mammalian detoxification pathways are adapted to deal with PSMs is crucial to understanding how PSMs influence ingestive behavior of herbivores and hence their fitness and the impact that they have on vegetation. Pharmacological concepts can provide insights into the relationship between the absorption and metabolic fate of PSMs and ingestive behavior. Lipophilic PSMs will be absorbed into the bloodstream and must be removed fast enough to prevent their accumulation to toxic levels. Elimination depends on their metabolism, usually by cytochrome P450 enzymes, to more polar metabolites that can be excreted by the kidney. The concentration of PSM in blood (C) is a better measure of exposure to a toxin compared to the amount ingested because there can be great variability in the rate and degree of absorption from the gut. C rises and falls depending on the relative rates of absorption and elimination. These rates depend in part on metabolic and transport processes that are saturable and liable to inhibition and induction by PSMs, indicating that complex interactions are likely. Herbivores can use diet choice and the rate and amount of PSM consumption to prevent C from reaching a critical level that produces significant adverse effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Herbivory is a widespread feeding habit of terrestrial vertebrates. Among the Eutherian mammals, most of the Artiodactyls and Perrisodactyls including the Bovids, Equids, and Cervids are exclusively herbivorous. The Lagomorphs and some Rodents also subsist on a diet largely composed of plants (Williams and Kay, 2001). Among the marsupials, herbivory is also widespread within the Diprotodontia, including many examples of herbivorous mammals, such as the macropods and possums (Hume, 1999). Plant material is generally a diffuse source of nutrients, and large amounts of material need to be ingested to maintain the metabolism of herbivorous mammals (Iason and Van Wieren, 1999). As a result, these mammals can consume a high proportion of plant biomass production and hence have an important influence on ecosystem function (Hester et al., 2006).
Because of plants' immobile nature and vulnerability to herbivory, strong selection pressure exists to evolve antiherbivory adaptations (Rhoades, 1979). Antiherbivory strategies diverge along the lines of the major division within the plant kingdom. Monocotyledonous plants (e.g., grasses and sedges) tolerate herbivory; their basal meristems reduce the impact of grazing on plant survival by facilitating regrowth (McNaughton, 1983). Dicotyledonous plants tend to have chemical and physical defenses that discourage herbivory (Bryant et al., 1991). Chemical defense is manifest in the evolution of a large array of phytochemicals that appear to have minimal function in the primary metabolism of plants (Rosenthal and Berenbaum, 1991). These so-called plant secondary metabolites (PSMs) include alkaloids, terpenes, phenolics, glucosinolates, and cyanogenic glycosides. Mammalian herbivores that ingest PSMs are liable to suffer a variety of adverse effects including reductions in nutrient availability and toxicity.
In this review, we consider the effects of PSMs on the ingestive behavior of herbivores, by using a pharmacological perspective. We also review the mechanisms used by herbivores to overcome plant defenses and avoid PSM toxicity, and consider how the pharmacokinetics of PSMs may influence ingestive behavior.
Plant Secondary Metabolites as Drugs
Modern pharmacology arose from the traditional use of plant products as medicines, and even today many therapeutic drugs are plant secondary metabolites (e.g., morphine, digoxin, atropine, ephedrine, artemisinin, vincristine, paclitaxel) or PSM derivatives (e.g., codeine, buprenorphine, warfarin, docetaxel). The principles surrounding the absorption, distribution, metabolism, and excretion of phytochemicals are the same, whether they are considered in the context of the delivery of drugs to target tissues in humans, or the detoxification of PSMs by mammalian herbivores. These two views of PSMs, as drugs and as chemical defenses, have been independently pursued, and we argue here that an exchange of concepts will benefit both of these disciplines. In particular, pharmacological concepts can provide insights into the relationship between ingestive behavior and the absorption and elimination of dietary PSMs. Conversely, the study of the chemical ecology of plant/herbivore interactions can provide insights to pharmacologists by considering the evolutionary context in which physiological mechanisms for metabolism of modern drugs arose.
A Note on Terminology
A drug may be broadly defined as any chemical that produces a biological effect on a human or animal, including both therapeutic and toxic effects (which are often produced by the same substance at different doses). Many PSMs are known to have drug effects as medicines, toxins, or antifeedants, but others have not had any such effects characterized. A xenobiotic is a chemical that may be present in animal tissues following absorption from the environment, but that lacks nutritional value. Xenobiotics include PSMs, synthetic drugs, and agricultural and other industrial chemicals. Where possible we have referred to literature on PSMs, but for much of the discussion on pharmacology we found no PSM data available, and we have used findings on synthetic drugs and other xenobiotics.
Effects of Plant Secondary Metabolites on Herbivores
Gastrointestinal Effects
Some PSMs remain in the gut where they may have local adverse effects. Condensed tannins, for example, are large polar molecules that cannot cross the gastrointestinal epithelium and are, therefore, not absorbed (Terrill et al., 1994). Tannins have an astringent taste and can bind and reduce the absorption of dietary proteins. Formyl phloroglucinols (e.g., jensenone, sideroxylonal) are aldehydes that react so rapidly with amine groups on proteins and other cellular constituents that they are not absorbed from the gut (McLean et al., 2004). However, these reactions result in adverse effects, mediated through serotonin release, which deter herbivory (Lawler et al., 1998; Wiggins et al., 2005). These locally acting PSMs will not be further considered in this review.
Systemic Effects
Many PSMs are lipophilic in character and can pass readily through the cell membranes of the gastrointestinal epithelium and be absorbed into the bloodstream, in which they will be delivered around the body to produce effects at distant sites. For example, morphine and digoxin stimulate chemoreceptors in the area postrema of the brainstem, resulting in nausea (Saito et al., 2003). In some cases, vomiting ensues leading to removal of unabsorbed toxin. Emetic agents can also act in the gut, via the release of serotonin and substance P from enterochromaffin cells, exciting sensory neurons that project to the area postrema and other parts of the brainstem (Saito et al., 2003). Stimulation of the emetic center is also associated with the development of conditioned flavor aversions that deter herbivores from repeated ingestion of toxic plants (Zahorik et al., 1990). PSMs can target other organs with specific toxicity; for example, digoxin causes cardiac arrhythmias, pyrrolizidine alkaloids produce multiple organ toxicity and cancers (Fu et al., 2004), and terpenes cause depression of the central nervous system (Falk et al., 1991; Tibballs, 1995). PSMs can also target particular systems, such as cholinergic neurotransmission that is blocked by atropine (which occupies the muscarinic receptors of acetylcholine) and enhanced by physostigmine (which inhibits acetylcholinesterase). Sublethal toxicity can deter future feeding through learned aversions (Provenza, 1995) and taste associations (Pass and Foley, 2000).
Pharmacodynamics: How Effect Depends on Concentration of Drug
The effect of a drug generally depends on the size of the dose taken and the consequent concentration produced at site(s) of action in the body (Wilkinson, 2001). The relationship between the log concentration of drug and its effect is sigmoidal rising to an asymptote (Fig. 1; Ross and Kenakin, 2001). Note that there is a dynamic range where the effect is sensitive to changes in concentration; a characteristic maximum effect (E max); and at low concentrations the effects are minimal or zero. We hypothesize that herbivore metabolic adaptations and ingestive behavior are directed toward preventing the concentration of PSMs in the body from exceeding tolerable levels.
Potency
Drugs and other PSMs differ markedly in their potency, measured by the amount (or concentration) required to produce a particular effect. For example, digoxin and atropine act therapeutically in humans at submilligram doses, whereas the doses of salicin (once used as an analgesic) and quinine are 1000 times greater. Among antifeedant PSMs, terpenes and phenolics are present at high concentrations in Eucalyptus leaf (up to 12% and 40% dry matter, respectively; Cork and Sanson, 1991), but the major antifeedant effect against marsupial folivores is exerted by formylphloroglucinols, which are present at significantly lower concentrations (mostly below 4% dry matter; Moore et al., 2004; Moore and Foley, 2005).
Tolerance
Continued exposure to a drug can lead to tolerance: a reduced effect that is usually due to an adaptation by cells to the presence of the drug. This happens especially with drugs that act on the central nervous system, which for example becomes less sensitive to alcohol and nicotine in regular drinkers and smokers, respectively (Le Houezec, 1998; Nutt, 1999). Tolerance to alcohol can develop to such an extent that individuals can survive normally lethal blood levels (Davis and Lipson, 1986), as well as tolerance to opioids in that addicts may take 50 times the normal dose, an amount which could be lethal for an opioid-naïve person (O'Brien, 2001). However, not all drugs elicit tolerance, as for example the doses of digoxin, warfarin, and atropine-like drugs that do not need to be increased with their continued therapeutic usage (Hardman et al., 2001).
Pharmacokinetics: How the Concentration of Drug Changes with Time After Dose
Absorption of Plant Secondary Metabolites
Absorption from the gut is usually by passive diffusion down a concentration gradient (Wilkinson, 2001). The speed of membrane permeation depends on the lipid solubility of the PSM. Some PSMs are substrates for active transporters, for example, glucosides that can be absorbed by the sodium-dependent glucose transporter SGL1, whereas glycosides of other sugars (e.g., rhamnose) are not transported (Manach et al., 2004). In general, glycosides must be hydrolyzed to be absorbed as the more lipophilic aglycone.
Most active PSM transport is by less specific efflux transporters such as P-glycoprotein (P-gp), which pumps foreign molecules out of the central nervous system and out of the body and into the gut, bile, and urine (Lin and Yamazaki, 2003).
Concentration in Blood
After an oral dose of a drug, its concentration in the body, which is usually measured in the blood or plasma (C), rises to a maximum (C max) and then falls (Fig. 2). The drug is distributed by the blood around the body and enters tissues where enzymes may convert it into metabolites that diffuse back into the blood and may be excreted in urine. Some metabolites that are formed in the liver are secreted into the bile and excreted in the feces (e.g., menthol glucuronide; Yamaguchi et al., 1994).
Blood concentration of cineole after an oral dose (100 mg/kg) administered to a brushtail possum. Methods are given in Boyle et al. (2002)
For many drugs, the time course of the effects following an oral dose will be described by a combination of the curves in Figs. 1 and 2. For example, the speed of onset of effects will depend on the rate of increase in concentration, and the maximum effect will be some function of C max. Pharmacokinetic–pharmacodynamic models incorporate change in concentration with time after a dose and the concentration–effect curve, and aim to describe the time–effect relationship (Meibohm and Derendorf, 1997). The overall scheme is illustrated below
where PK is pharmacokinetics, PD is pharmacodynamics, and C is concentration.
The concentration at the tissue site of action usually cannot be directly measured, but the rise and fall in the concentration in blood plasma over time is a better measure of tissue exposure to a drug compared to the dose (which is the amount ingested over a given period of time, and gives far less data than a series of blood concentrations). Furthermore, there are many factors—such as body size and composition, and the rates of absorption and elimination—that affect the relationship between dose and concentration in the blood, which are often highly variable. Wilkinson (2001) gives a good introduction to pharmacokinetics, and there are specialist texts that give a detailed treatment (e.g., Rowland and Tozer, 1995; Shargel and Yu, 1999).
The concentration of a drug in blood relates best to its effect when it acts rapidly and reversibly. In other circumstances, there may not be a simple relationship between blood concentration and effect. For example, there can be delays if the equilibration between blood and tissue site of action is slow (as with some opioids; Lotsch et al., 2004), and the relationship between concentration and effect may be complicated if tissue sensitivity changes over time (as with levodopa; Deleu et al., 2002). Furthermore, the effects can persist after a drug has been eliminated from the blood if it is bound in tissues, or its actions are not reversible (e.g., irreversible enzyme inhibition or cell death). Sometimes the biological activity of a compound is attributable to its metabolite, as outlined below.
Elimination of Plant Secondary Metabolites
It is self-evident that herbivores must remove ingested PSMs from their body or risk their progressive accumulation to harmful levels. Metabolism and excretion are the processes used to eliminate PSMs from the body. Because the terrestrial kidney conserves water by extensively reabsorbing it from the renal tubules, lipophilic substances that can freely permeate the tubular epithelium are also extensively reabsorbed (Wilkinson, 2001). Thus, the more lipophilic a PSM, the more readily it will be absorbed from the gut and the less efficiently it will be excreted by the kidney. Animals possess a battery of enzymes that can transform lipophilic xenobiotics into water-soluble metabolites that are more readily excreted by the kidney.
Metabolism of Plant Secondary Metabolites
The enzymes that metabolize xenobiotics are considered to have evolved in herbivores in response to the formation of defensive chemicals by plants (Gonzalez and Nebert, 1990; Lewis et al., 1998). Compared to the enzymes of intermediary metabolism, they are characterized by a remarkable lack of substrate specificity, enabling them to metabolize a chemically diverse range of PSMs and, incidentally, other xenobiotics. Thus, humans use the same group of enzymes to metabolize therapeutic drugs, whether of plant origin or the newly created products of synthetic chemistry.
The major type are the cytochrome P450 enzymes (CYPs), which are responsible for most oxidative metabolism of xenobiotics (Wilkinson, 2001). P450 genes are found in virtually all organisms, and the enzymes they code for are responsible for many different reactions: some plant P450 enzymes are involved in the synthesis of the plant defense chemicals that are subsequently catabolized in the animal by other related enzymes of the same superfamily (Werck-Reichhart and Feyerreisen, 2000).
The overall pattern of P450 genes is the same in humans and the puffer fish, and has been conserved despite 420 million yr of separate development (Nelson, 2003). Despite the similarities in P450 gene families among mammals, there is variation in the individual orthologous forms of P450 enzymes, probably driven by dietary differences, giving rise to marked differences between species in xenobiotic metabolism (Shimada et al., 1997; Lewis et al., 1998; Boyle et al., 1999, 2000, 2001; Machala et al., 2003). Within species, there can also be polymorphic and sex differences in P450 activity that, combined with individual differences in diet and associated induction processes, can result in significant individual differences in xenobiotic metabolism (Lewis et al., 1998; Ayrton and Morgan, 2001; Weaver, 2001; Weinshilboum, 2003).
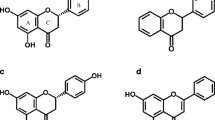
The major sites of xenobiotic metabolism are the gastrointestinal endothelium, the liver, and the kidney (Parkinson, 2001; Doherty and Charman, 2002). In the case of ruminant herbivores, which have a bacterial fermentation chamber anterior to major sites of absorption, microbial biotransformation of PSMs in the rumen is an important mechanism for PSM metabolism (Carlson and Breeze, 1984). Because lipophilic PSMs are absorbed in the small intestine, they escape contact with the colonic bacteria of hindgut fermenters. However, many PSMs are polar (e.g., glycosides) and poorly absorbed, and are subject to bacterial metabolism in the colon (Manach et al., 2004). For example, quercetin-3-rutinoside (rutin) is hydrolyzed to the flavonol quercetin, which is partly absorbed intact and partly metabolized to hydroxy acids that are then absorbed (Olthof et al., 2003; Rechner et al., 2004).
Tissue level xenobiotic metabolism is divided into two phases: functionalization (Phase 1) and conjugation (Phase 2) (for a detailed account of xenobiotic biotransformation, see Parkinson, 2001). Phase 1 reactions serve to introduce or free a functional group, such as –OH, –NH2, or –COOH. Most Phase 1 reactions involve a variety of oxidations catalyzed by P450 enzymes, but hydrolyses are also important for many PSMs such as esters, amides, and glycosides. In Phase 2, functional groups on xenobiotics or their metabolites are used to form adducts with endogenous substances, such as glucuronic acid, sulfate, glycine, or glutathione. The resulting conjugate is typically much more polar than its precursor, limiting its reabsorption from the renal tubules. Additionally, it may be a substrate for active transport into the renal tubules or bile duct, which can greatly increase the rate of elimination (Lin and Yamazaki, 2003; Lee and Kim, 2004).
Is Metabolism Detoxification?
In general, xenobiotic metabolism acts on lipophilic substrates that are converted into more polar, and, therefore, more readily excreted, metabolites. In changing the chemical structure of a xenobiotic, metabolism usually changes the biological activity, but this does not always result in detoxification because there are many examples where the metabolite is active (Zhou et al., 2004a).
For example, P450 oxidation of pyrrolizidine alkaloids generates reactive metabolites that form adducts with protein and DNA, resulting in hepatotoxicity and carcinogenicity (Fu et al., 2004). Rumen bacterial biotransformation can also lead to activation of xenobiotics. For example, S-methyl cysteine sulfoxide, found in cruciferous plants, is metabolized in the rumen to dimethyl disulfide, which causes hemolytic anemia (Smith, 1980).
Induction and Inhibition of Metabolism and Transport
Competition between substrates can result in inhibition of metabolism (Lin and Lu, 2001; Weaver, 2001), especially with low-capacity pathways such as glycine conjugation (Moriwaki et al., 2005). Mechanism-based inhibition occurs when an enzyme produces a reactive product that binds to the enzyme and inactivates it (Weaver, 2001). The furanocoumarins in grapefruit juice, for example, inactivate enterocyte CYP3A, which can result in clinically significant increases in oral absorption of drugs (e.g., cyclosporin) that are extensively metabolized by this enzyme (Dresser and Bailey, 2003). Recovery depends on enzyme regeneration and takes a few days (Greenblatt et al., 2003).
Some xenobiotics bind to receptors in the cell nucleus leading to increased synthesis of certain xenobiotic-metabolizing enzymes, a process called induction (Lin and Lu, 2001; Weaver, 2001). Unlike enzyme inhibition, which is almost immediate, induction takes some days or weeks while the new protein is synthesized for the full effect to be seen (Hollenberg, 2002). The increased amount of enzyme enables faster metabolism of substrates, and is clearly a useful adaptation to a diet with changing PSM content. St John's wort (Hypericum perforatum) contains hyperforin, which activates the nuclear pregnane X receptor—thereby inducing the expression of CYP3A4, an enzyme that metabolizes most drugs (Moore et al., 2000). St John's wort also induces the intestinal efflux transporter P-gp, and both mechanisms contribute to the lowered blood levels of substrate drugs (Dresser et al., 2003). The full manifestation of the effects of St John's wort and other PSMs are complex, and depend on species, tissue, dose, timing, and PSM composition (Zhou et al., 2003, 2004b). Glucosinolates found in cruciferous plants also cause the induction of P450s (Bonnesen et al., 1999) following their hydrolysis in the digestive tract to active metabolites such as isothiocyanates.
Inducers are also substrates for the enzymes they induce (Hollenberg, 2002) and can act as competitive inhibitors of other reactions while present and bound to the active site. This is demonstrated in the brushtail possum, in which pretreatment for 10 d with a mixture of dietary terpenes induced hepatic P450 enzymes, resulting in faster in vitro metabolism of both the terpenes (1,8-cineole and p-cymene) and other substrates (Pass et al., 1999, 2001, 2002). When the inducing terpenes were added to liver enzyme preparations, they potently inhibited the metabolism of 1,8-cineole (Pass and McLean, 2002).
The consequences for PSM metabolism (and P-gp transport) by herbivores that consume large amounts of PSMs in their diet may be a complex result of induction (from recent exposure to inducing PSMs) and inhibition (by competitively inhibitory PSMs currently consumed and mechanism-based inhibitors recently consumed).
Dietary exposure of ruminant herbivores to PSMs can also lead to induced adaptation of the rumen microbial population, which can result in large changes in rates of metabolism and hence bioavailability. Such adaptation is generally presumed to depend on changes to microbial population structure in response to altered substrate availability. Thus, for example, the presence of oxalate salts in the diet of ruminant herbivores leads to the proliferation of Oxalobacter formigenes, a bacterial species capable of degrading oxalates (Allison et al., 1985). Adapted animals are tolerant to dietary oxalate exposure, and rates of degradation increase with increases in dietary exposure (Duncan et al., 1997).
Pharmacokinetic Factors Influence Plant Secondary Metabolite Concentration and Effects
The ingestive behavior of a herbivore effectively determines the PSM dosage rate (amount ingested per time), but the concentration in blood will depend as well on the relative rates of absorption and elimination, which are liable to considerable variability among species and individuals.
Some xenobiotics are extensively metabolized in the gut lumen, gut wall, and liver so that only a fraction of the oral dose reaches the systemic circulation (Wilkinson, 2001; Doherty and Charman, 2002). This fraction, termed the bioavailability (F), can be calculated from the ratio of the areas under the concentration–time curve after oral and intravenous dosing. Low values are inherently variable (Hellriegel et al., 1996), and a change in F from, say, 0.03 to 0.06 effectively doubles the amount of xenobiotics that reaches most of the body.
Limits to Consumption of PSMs
Herbivorous mammals typically eat in bouts separated by periods of not eating, and the total meal may take several hours (Arnold, 1981). The presence of PSMs in food plants presents a risk of toxicity to herbivores but, in most cases, it is presumed that they are able to limit consumption of toxic plants before they cause toxicity. Cases of clinical signs of toxicity among wild herbivores in their natural range are unusual. The means by which herbivores discern the toxicity of plants and avoid overconsumption are not well known, and we have developed a model system by using 1,8-cineole and the brushtail possum to address this. The monoterpene 1,8-cineole (cineole) is present in many species of Eucalyptus leaf as well as a number of conifer species (Von Rudloff, 1975). When brushtail possums were fed an artificial diet containing 2% cineole, the size of each bout was limited by the blood cineole concentration, since feeding stopped when this reached a critical level (Fig. 3; Boyle et al., 2005). The blood concentration depends on the amount of cineole ingested (i.e., the dose), its speed of absorption, and its bioavailability. Thus, the size and frequency of bouts, and the rate of eating during a bout may be governed by a negative feedback effect from the concentration of blood cineole or its metabolites.
Blood concentrations of cineole (○) in the brushtail possum in relation to eating a diet containing 2% cineole (—). From Boyle et al. (2005)
Repeated ingestion of PSMs will lead to accumulation if some remains in the body after the previous feeding bout. The extent of accumulation depends on both the rate of ingestion (i.e., dose rate) and the rate of elimination. If an animal eats at a constant rate, the PSM will accumulate to a steady state when the (usually first-order) elimination rate equals the intake rate. This is because the first-order rate of elimination will increase with the concentration of PSM (up to a concentration that saturates the enzymes).
Because the elimination rate (k.C) changes with C, the efficiency of elimination of a xenobiotic is better expressed by using the clearance concept, borrowed from renal physiology (Wilkinson, 2001). Clearance (CL) is the volume of blood or plasma from which a drug has been completely removed per unit time, and its value remains constant for any one individual and occasion so long as first-order conditions pertain. Clearance enables the steady-state concentration (C ss) to be calculated for any constant dosing rate.
Continued accumulation of even low-potency PSMs will eventually lead to adverse effects. The consumption of PSMs on a daily basis will be limited by the capacity of the animal to eliminate them and their metabolites. This will depend on the rates of metabolism and renal excretion.
Implications of Pharmacokinetics of PSMS for Patterns of Ingestive Behavior
We have seen that, in a pharmacological context, circulating concentrations of drugs can serve as a useful approximation of drug concentrations at target tissues, and we argue that a similar approximation is useful in the context of herbivores and PSMs. Herbivores can avoid exceeding thresholds of plasma PSM concentrations by various means. First, spreading their feeding bouts on particular toxic plants throughout the day, or over longer periods, will reduce the probability of toxic thresholds being exceeded (Foley et al., 1999). There is evidence that consumption of toxic plants on 1 d influences intake rates on subsequent days, with cattle showing cyclical patterns of consumption to maintain circulating concentrations of toxins below toxic thresholds (Pfister et al., 1997). At shorter timescales, however, there is less evidence that herbivores alter patterns of ingestive behavior, including meal frequency, in response to PSM concentrations (Wiggins et al., 2003; Sorensen et al., 2005). A temporal distribution of feeding on a toxic plant species is likely to be facilitated by a dispersed spatial distribution of the plant. Large patches of toxic plants limit the potential for consuming alternative plants and may, therefore, limit intake potential. For example, extensive stands of invasive plants such as sagebrush (Artemisia spp.) are difficult to control by herbivory; smaller patches are more readily consumed presumably since alternative food sources may allow herbivores to maintain toxin concentrations below critical thresholds (Heady, 1964; Provenza et al., 2003).
Critical thresholds for particular toxins may also be avoided through diet mixing. The toxin dilution hypothesis (Freeland and Janzen, 1974) has been around for a long time, but never adequately tested (Iason and Villalba, 2006, in this issue). It is certainly true that herbivores consume more food when offered a choice of foods containing different PSMs than when offered foods containing a single PSM (Burritt and Provenza, 2000; Wiggins et al., 2003), and Wiggins et al., 2006 (this issue) have shown that leaf consumption is greater when two chemically dissimilar plants are offered together rather than either one alone. This phenomenon, however, has not yet been linked to circulating concentrations of PSMs that would demonstrate that animals are maintaining toxins below toxic thresholds through diet mixing.
Induction and inhibition of PSM metabolism also has implications for patterns of ingestion. Ruminant herbivores are generally cautious when they encounter novel foods, and this may be an adaptive mechanism to allow time for induction of enzymes responsible for PSM metabolism. Such induction may occur at the level of the gut microflora or the liver. Adapted animals consume more toxic plants than nonadapted ones (Duncan et al., 2000). Indeed, diet mixing, or occasional sampling of novel foods, may be an adaptive strategy for maintaining enzymes in an induced state to give maximum future protection against toxicity when encountering novel plants.
Conclusion
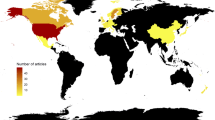
A pharmacokinetic approach to the study of PSM metabolism has much to offer in terms of quantifying the impact of PSMs on large herbivores under different feeding scenarios and to suggest explanations for observed patterns of feeding behavior. Much of the research on the pharmacokinetics of PSMs derives from the pharmacological literature, and some of the methods and understanding of drug metabolism now need to be adopted by ecologists to advance the field of plant/animal interactions. A range of factors relating to the physiology of the subject influence the fate of drugs following their ingestion (Fig. 4). These include the state of enzyme induction/inhibition (Lin and Lu, 2001), genetic factors (Weinshilboum, 2003), disease states (Rodighiero, 1999), and the age of the animal (Woodhouse, 1992; Kinirons and O'Mahony, 2004) and its nutritional status (Walter-Sack and Klotz, 1996; Ioannides, 1999). Improved understanding of how such factors influence the metabolism of plant secondary compounds in herbivores would help to improve our understanding of the influence of PSMs on ingestive behavior. Of particular interest are the questions surrounding the kinetics of toxin elimination and how this relates to the kinetics of feeding behavior at a range of temporal scales.
References
Allison, M. J., Dawson, K. A., Mayberry, W. R., and Foss, J. G. 1985. Oxalobacter formigenes gen. nov., sp. nov.: Oxalate-degrading anaerobes that inhabit the gastrointestinal tract. Arch. Microbiol. 141:1–7.
Arnold, G. W. 1981. Grazing behavior, pp. 79–104, in F. W. Morley (ed.). Grazing Animals. Elsevier, Amsterdam.
Ayrton, A. and Morgan, P. 2001. Role of transport proteins in drug absorption, distribution and excretion. Xenobiotica 31:469–497.
Bonnesen, C., Stephensen, P. U., Andersen, O., Sorensen, H., and Vang, O. 1999. Modulation of cytochrome P-450 and glutathione S-transferase isoform expression in vivo by intact and degraded indolyl glucosinolates. Nutr. Cancer 33:178–187.
Boyle, R., McLean, S., Foley, W. J., and Davies, N. W. 1999. Comparative metabolism of dietary terpene, p-cymene, in generalist and specialist folivorous marsupials. J. Chem. Ecol. 25:2109–2126.
Boyle, R., McLean, S., Foley, W. J., Moore, B. D., Davies, N. W., and Brandon, S. 2000. Fate of the dietary terpene, p-cymene, in the male koala. J. Chem. Ecol. 25:1095–1111.
Boyle, R., McLean, S., Foley, W., Davies, N. W., Peacock, E. J., and Moore, B. 2001. Metabolites of dietary 1,8-cineole in the male koala (Phascolarctos cinereus). Comp. Biochem. Physiol. C 129:385–395.
Boyle, R. R., McLean, S., Brandon, S., Pass, G. J., and Davies, N. W. 2002. Application of solid-phase microextraction to the quantitative analysis of 1,8-cineole in blood and expired air in a Eucalyptus herbivore, the brushtail possum (Trichosurus vulpecula). J. Chromatogr. B. 780:397–406.
Boyle, R. R., McLean, S., Brandon, S., and Wiggins, N. 2005. Rapid absorption of dietary 1,8-cineole results in critical blood concentration of cineole and immediate cessation of eating in the common brushtail possum (Trichosurus vulpecula). J. Chem. Ecol. 31:2775–2790.
Bryant, J. P., Provenza, F. D., Pastor, J., Reichardt, P. B., Clausen, T. P., and Dutoit, J. T. 1991. Interactions between woody-plants and browsing mammals mediated by secondary metabolites. Annu. Rev. Ecol. Syst. 22:431–446.
Burritt, E. A. and Provenza, F. D. 2000. Role of toxins in intake of varied diets by sheep. J. Chem. Ecol. 26:1991–2005.
Carlson, J. R. and Breeze, R. G. 1984. Ruminal metabolism of plant toxins with emphasis on indolic compounds. J. Anim. Sci. 58:1040–1049.
Cork, S. J. and Sanson, G. D. 1991. Digestion and nutrition in the koala: A review, pp. 129–144, in A. K. Lee, K. A. Handasyde, and G. D. Sanson (eds.). Biology of the Koala. Surrey Beatty and Sons, Chipping Norton, NSW.
Davis, A. R. and Lipson, A. H. 1986. Central-nervous-system tolerance to high blood-alcohol levels. Med. J. Aust. 144:9–12.
Deleu, D., Northway, M. G., and Hanssens, Y. 2002. Clinical pharmacokinetic and pharmacodynamic properties of drugs used in the treatment of Parkinson's disease. Clin. Pharmacokinet. 41:261–309.
Doherty, M. M. and Charman, W. N. 2002. The mucosa of the small intestine—how clinically relevant as an organ of drug metabolism? Clin. Pharmacokinet. 41:235–253.
Dresser, G. K. and Bailey, D. G. 2003. The effects of fruit juices on drug disposition: A new model for drug interactions. Eur. J. Clin. Invest. 33:10–16.
Dresser, G. K., Schwarz, U. I., Wilkinson, G. R., and Kim, R. B. 2003. Coordinate induction of both cytochrome P4503A and MDRI by St John's wort in healthy subjects. Clin. Pharmacol. Ther. 73:41–50.
Duncan, A. J., Frutos, P., and Young, S. A. 1997. Rates of oxalic acid degradation in the rumen of sheep and goats in response to different levels of oxalic acid administration. Anim. Sci. 65:451–455.
Duncan, A. J., Frutos, P., and Young, S. A. 2000. The effect of rumen adaptation to oxalic acid on selection of oxalic-acid-rich plants by goats. Br. J. Nutr. 83:59–65.
Falk, A., Lof, A., Hagberg, M., Hjelm, E. W., and Wang, Z. P. 1991. Human exposure to 3-carene by inhalation-toxicokinetics, effects on pulmonary-function and occurrence of irritative and CNS-symptoms. Toxicol. Appl. Pharmacol. 110:198–205.
Foley, W. J., Iason, G. R., and McArthur, C. 1999. Role of plant secondary metabolites in the nutritional ecology of mammalian herbivores: How far have we come in 25 years? pp. 130–209, in H.-J. G. Jung and G. C. Fahey (eds.). San Antonio, Texas, USA. American Society of Animal Science, Savoy, IL.
Freeland, W. J. and Janzen, D. H. 1974. Strategies in herbivory by mammals: The role of plant secondary compounds. Am. Nat. 108:268–289.
Fu, P. P., Xia, Q. S., Lin, G., and Chou, M. W. 2004. Pyrrolizidine alkaloids—genotoxicity, metabolism enzymes, metabolic activation, and mechanisms. Drug Metab. Rev. 36:1-55.
Gonzalez, F. J. and Nebert, D. W. 1990. Evolution of the P450 gene superfamily: Animal–plant “warfare”, molecular drive and human genetic differences in drug oxidation. Trends Genet. 6:182–186.
Greenblatt, D. J., von Moltke, L. L., Harmatz, J. S., Chen, G. S., Weemhoff, J. L., Jen, C., Kelley, C. J., LeDuc, B. W., and Zinny, M. A. 2003. Time course of recovery of cytochrome P450 3A function after single doses of grapefruit juice. Clin. Pharmacol. Ther. 74:121–129.
Hardman, J. G., Limbird, L. E., and Gilman, A. G. 2001. Goodman and Gilman's The Pharmacological Basis of Therapeutics. McGraw-Hill, New York.
Heady, H. F. 1964. Palatability of herbage and animal preference. J. Range Manag. 17:76–82.
Hellriegel, E. T., Bjornsson, T. D., and Hauck, W. W. 1996. Interpatient variability in bioavailability is related to the extent of absorption: Implications for bioavailability and bioequivalence studies. Clin. Pharmacol. Ther. 60:601–607.
Hester, A. J., Bergman, M., Iason, G. R., and Moen, J. 2006. Impact of large herbivores on plant community structure and dynamics, in K. Danell, R. Gergstrom, P. Duncan, and J. Pastor (eds.). Large Herbivore Ecology and Ecosystem Dynamics. Cambridge University Press, Cambridge, in press.
Hollenberg, P. F. 2002. Characteristics and common properties of inhibitors, inducers, and activators of CYP enzymes. Drug Metab. Rev. 34:17–35.
Hume, I. D. 1999. Marsupial Nutrition. Cambridge University Press, Cambridge.
Iason, G. R. and Van Wieren, S. E. 1999. Digestive and ingestive adaptations of mammalian herbivores to low-quality forage, pp. 337–369, in H. H. Olff, V. K. Brown, and R. H. Drent (eds.). Herbivores: Between Plants and Predators, 38th Symposium of the British Ecological Society. Blackwell, Oxford.
Iason, G. R. and Villalba, J. J. 2006. Behavioral strategies of mammal herbivores against plant secondary metabolites: The avoidance–tolerance continuum. J. Chem. Ecol., this issue.
Ioannides, C. 1999. Effect of diet and nutrition on the expression of cytochromes 450. Xenobiotica 29:109–154.
Kinirons, M. T. and O'Mahony, M. S. 2004. Drug metabolism and ageing. Br. J. Clin. Pharmacol. 57:540–544.
Lawler, I. R., Foley, W. J., Pass, G. J., and Eschler, B. M. 1998. Administration of a 5HT(3) receptor antagonist increases the intake of diets containing Eucalyptus secondary metabolites by marsupials. J. Comp. Physiol. B 168:611–618.
Le Houezec, J. 1998. Nicotine: Abused substance and therapeutic agent. J. Psychiatry Neurosci. 23:95–108.
Lee, W. and Kim, R. B. 2004. Transporters and renal drug elimination. Annu. Rev. Pharmacol. Toxicol. 44:137–166.
Lewis, D. F., Watson, E., and Lake, B. G. 1998. Evolution of the cytochrome P450 superfamily: Sequence alignments and pharmacogenetics. Mutat. Res. 410:245–270.
Lin, J. H. and Lu, A. Y. H. 2001. Interindividual variability in inhibition and induction of cytochrome P450 enzymes. Annu. Rev. Pharmacol. Toxicol. 41:535–567.
Lin, J. H. and Yamazaki, M. 2003. Role of P-glycoprotein in pharmacokinetics—clinical implications. Clin. Pharmacokinet. 42:59–98.
Lotsch, J., Skarke, C., Liefhold, J., and Geisslinger, G. 2004. Genetic predictors of the clinical response to opioid analgesics: Clinical utility and future perspectives. Clin. Pharmacokinet. 43:983–1013.
Machala, M., Soucek, P., Neca, J., Ulrich, R., Lamka, J., Szotakova, B., and Skalova, L. 2003. Inter-species comparisons of hepatic cytochrome P450 enzyme levels in male ruminants. Arch. Toxicol. 77:555–560.
Manach, C., Scalbert, A., Morand, C., Remesy, C., and Jimenez, L. 2004. Polyphenols: Food sources and bioavailability. Am. J. Clin. Nutr. 79:727–747.
McLean, S., Brandon, S., Davies, N. W., Foley, W. J., and Muller, H. K. 2004. Jensenone: Biological reactivity of a marsupial antifeedant from Eucalyptus. J. Chem. Ecol. 30:19–36.
McNaughton, S. J. 1983. Compensatory plant growth as a response to herbivory. Oikos 40:329–336.
Meibohm, B. and Derendorf, H. 1997. Basic concepts of pharmacokinetic/pharmacodynamic (PK/PD) modelling. Int. J. Clin. Pharmacol. Ther. 35:401–413.
Moore, B. D. and Foley, W. J. 2005. Tree use by koalas in a chemically complex landscape. Nature 435:488–490.
Moore, B. D., Wallis, I. R., Pala-Paul, J., Brophy, J. J., Willis, R. H., and Foley, W. J. 2004. Antiherbivore chemistry of Eucalyptus—cues and deterrents for marsupial folivores. J. Chem. Ecol. 30:1743–1769.
Moore, L. B., Goodwin, B., Jones, S. A., Wisely, G. B., Serabjit-Singh, C. J., Willson, T. M., Collins, J. L., and Kliewer, S. A. 2000. St. John's wort induces hepatic drug metabolism through activation of the pregnane X receptor. Proc. Natl. Acad. Sci. U. S. A. 97:7500–7502.
Moriwaki, H., Tsujimoto, Y., Shimizu, M., Noda, T., Warashina, M., and Tanaka, M. 2005. Influence of sodium benzoate on the metabolism of o-xylene in the rat. Xenobiotica 35:487–497.
Nelson, D. R. 2003. Comparison of P450s from human and fugu: 420 million years of vertebrate P450 evolution. Arch. Biochem. Biophys. 409:18–24.
Nutt, D. 1999. Alcohol and the brain—pharmacological insights for psychiatrists. Br. J. Psychiatry 175:114–119.
O'Brien, C. P. 2001. Drug addiction and drug abuse, pp. 621–642, in J. G. Hardman, L. E. Limbird, and A. G. Gilman (eds.). Goodman and Gilman's The Pharmacological Basis of Therapeutics. 10th ed. McGraw-Hill, New York.
Olthof, M. R., Hollman, P. C. H., Buijsman, M., van Amelsvoort, J. M. M., and Katan, M. B. 2003. Chlorogenic acid, quercetin-3-rutinoside and black tea phenols are extensively metabolized in humans. J. Nutr. 133:1806–1814.
Parkinson, A. 2001. Biotransformation of xenobiotics, pp. 133–224, in C. D. Klaasen (ed.). Casarett and Doull's Toxicology: The Basic Science of Poisons. 6th ed. McGraw-Hill, New York.
Pass, G. J. and Foley, W. J. 2000. Plant secondary metabolites as mammalian feeding deterrents: Separating the effects of the taste of salicin from its post-ingestive consequences in the common brushtail possum (Trichosurus vulpecula). J. Comp. Biochem. Physiol. 170.
Pass, G. J. and McLean, S. 2002. Inhibition of the microsomal metabolism of 1,8-cineole in the common brushtail possum (Trichosurus vulpecula) by terpenes and other chemicals. Xenobiotica 32:1109–1126.
Pass, G. J., McLean, S., and Stupans, I. 1999. Induction of xenobiotic metabolising enzymes in the common brushtail possum, Trichosurus vulpecula, by Eucalyptus terpenes. J. Comp. Biochem. Physiol. 124:239–246.
Pass, G. J., McLean, S., Stupans, I., and Davies, N. 2001. Microsomal metabolism of the terpene 1,8-cineole in the common brushtail possum (Trichosurus vulpecula), koala (Phascolarctos cinereus), rat and human. Xenobiotica 31:205–221.
Pass, G. J., McLean, S., Stupans, I., and Davies, N. W. 2002. Microsomal metabolism and enzyme kinetics of the terpene p-cymene in the common brushtail possum (Trichosurus vulpecula), koala (Phascolarctos cinereus) and rat. Xenobiotica 32:383–397.
Pfister, J. A., Provenza, F. D., Manners, G. D., Gardner, D. R., and Ralphs, M. H. 1997. Tall larkspur ingestion: Can cattle regulate intake below toxic levels? J. Chem. Ecol. 23:759–777.
Provenza, F. D. 1995. Postingestive feedback as an elementary determinant of food preference and intake in ruminants. J. Range Manag. 48:2–17.
Provenza, F. D., Villalba, J. J., and Bryant, B. P. 2003. Foraging by herbivores: Linking the biochemical diversity of plants to herbivore culture and landscape diversity, pp.387–421, in J. A. Bissonette and I. Staoch (eds.). Landscape Ecology and Resource Management. Linking Theory with Practice. Island Press, Washington.
Rechner, A. R., Smith, M. A., Kuhnle, G., Gibson, G. R., Debnam, E. S., Srai, S. K. S., Moore, K. P., and Rice-Evans, C. A. 2004. Colonic metabolism of dietary polyphenols: Influence of structure on microbial fermentation products. Free Radic. Biol. Med. 36:212–225.
Rhoades, D. F. 1979. Evolution of plant chemical defence against herbivores, pp. 3–54, in G. A. Rosenthal and D. H. Janzen (eds.). Herbivores. Their Interaction with Secondary Plant Metabolites. Academic Press, New York.
Rodighiero, V. 1999. Effects of liver disease on pharmacokinetics. An update. Clin. Pharmacokinet. 37:399–431.
Rosenthal, G. A. and Berenbaum, M. R. 1991. Herbivores. Their interactions with Secondary Plant Metabolites. Harcourt Brace Jovanovich, Illinois.
Ross, E. M. and Kenakin, T. P. 2001. Pharmacodynamics: Mechanisms of drug action and the relationship between drug concentration and effect, pp. 31–42, in J. G. Hardman, L. E. Limbird, and A. G. Gilman (eds.). Goodman and Gilman's The Pharmacological Basis of Therapeutics. 10th ed. McGraw-Hill, New York.
Rowland, M. and Tozer, T. N. 1995. Clinical Pharmacokinetics—Concepts and Applications. Lea & Febiger, Philadelphia, p. 601.
Saito, R., Takano, Y., and Kamiya, H. O. 2003. Roles of substance P and NK(1) receptor in the brainstem in the development of emesis. J. Pharmacol. Sci. 91:87–94.
Shargel, L. and Yu, A. 1999. Applied Biopharmaceutics & Pharmacokinetics. McGraw-Hill, New York.
Shimada, T., Mimura, M., Inoue, K., Nakamura, S., Oda, H., Ohmori, S., and Yamazaki, H. 1997. Cytochrome P450-dependent drug oxidation activities in liver microsomes of various animal species including rats, guinea pigs, dogs, monkeys, and humans. Arch. Toxicol. 71:401–408.
Smith, R. H. 1980. Kale poisoning: The brassica anaemia factor. Vet. Rec. 107:12–15.
Sorensen, J. S., Heward, E., and Dearing, M. D. 2005. Plant secondary metabolites alter the feeding patterns of a mammalian herbivore (Neotoma lepida). Oecologia 146:415–422.
Terrill, T. H., Waghorn, G. C., Woolley, D. J., McNabb, W. C., and Barry, T. N. 1994. Assay and digestion of C-14-labeled condensed tannins in the gastrointestinal-tract of sheep. Br. J. Nutr. 72:467–477.
Tibballs, J. 1995. Clinical effects and management of eucalyptus oil ingestion in infants and young children. Med. J. Aust. 163:177–180.
Von Rudloff, E. 1975. Volatile leaf oil analysis in chemosystematic studies of North American conifers. Biochem. Syst. Ecol. 2:131–167.
Walter-Sack, I. and Klotz, U. 1996. Influence of diet and nutritional status on drug metabolism. Clin. Pharmacokinet. 31:47–64.
Weaver, R. J. 2001. Assessment of drug–drug interactions: Concepts and approaches. Xenobiotica 31:499–538.
Weinshilboum, R. 2003. Genomic medicine—inheritance and drug response. N. Engl. J. Med. 348:529–537.
Werck-Reichhart, D. and Feyerreisen, R. 2000. Cytochromes P450: A success story. Genome Biol. 1:3002.9–3003.1.
Wiggins, N. L., McArthur, C., McLean, S., and Boyle, R. 2003. Effects of two plant secondary metabolites, cineole and gallic acid, on nightly feeding patterns of the common brushtail possum. J. Chem. Ecol. 29:1447–1464.
Wiggins, N. L., Marsh, K. J., Wallis, I. R., Foley, W. J., and McArthur, C. 2005. Sideroxylonal in Eucalyptus foliage influences foraging behavior of an arboreal folivore. Oecologia http://www.springerlink.com/link.asp?id=32tj3775u2341578.
Wiggins, N. L., McArthur, C., Davies, N. W., and McLean, S. 2006. Behavioral responses of a generalist mammalian folivore to the physiological constraints of a chemically defended diets. J. Chem. Ecol., in this issue.
Wilkinson, G. R. 2001. Pharmacokinetics: The dynamics of drug absorption, distribution, and elimination, pp. 3–29, in J. G. Hardman, L. E. Limbird, and A. G. Gilman (eds.). Goodman and Gilman's The Pharmacological Basis of Therapeutics. 10th ed. McGraw-Hill, New York.
Williams, S. H. and Kay, R. F. 2001. A comparative test of adaptive explanations for hypsodonty in ungulates and rodents. J. Mammal. Evol. 8:207–229.
Woodhouse, K. 1992. Drugs and the liver. Part III. Ageing of the liver and the metabolism of drugs. Biopharm. Drug Dispos. 13:311–320.
Yamaguchi, T., Caldwell, J., and Farmer, P. B. 1994. Metabolic fate of [H-3]-l-menthol in the rat. Drug Metab. Dispos. 22:616–624.
Zahorik, D. M., Houpt, K. A., and Swartzmanandert, J. 1990. Taste-aversion learning in 3 species of ruminants. Appl. Animal Behav. Sci. 26:27–39.
Zhou, S. F., Gao, Y. H., Jiang, W. Q., Huang, M., Xu, A. L., and Paxton, J. W. 2003. Interactions of herbs with cytochrome P450. Drug Metab. Rev. 35:35–98.
Zhou, S. F., Koh, H. L., Gao, Y. H., Gong, Z. Y., and Lee, E. J. D. 2004a. Herbal bioactivation: The good, the bad and the ugly. Life Sci. 74:935–968.
Zhou, S. F., Lim, L. Y., and Chowbay, B. 2004b. Herbal modulation of P-glycoprotein. Drug Metab. Rev. 36:57–104.
Acknowledgments
Our thanks to Takuya Shimada and Bill Foley for convening the symposium and stimulating the writing of this review, and to Glenn Iason for useful commments on a draft manuscript. We are also grateful to our coworkers, in particular, Rebecca Boyle and Sue Brandon. This work has in part been supported by the Australian Research Council.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McLean, S., Duncan, A.J. Pharmacological Perspectives on the Detoxification of Plant Secondary Metabolites: Implications for Ingestive Behavior of Herbivores. J Chem Ecol 32, 1213–1228 (2006). https://doi.org/10.1007/s10886-006-9081-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10886-006-9081-4